Abstract
Conflict of interest: none declared.
Goals
The goals of this research are: a) to determine the number, gender and age representation of patients with a working diagnosis of acute stroke referred by the Institute for Emergency Medical Care (IEMC) in the Clinical Center of Sarajevo University (CCSU); b) determine the incidence of patients that have been or have not been hospitalized and why; c) determine the time and procedure for emergency medical care; d) to determine the characteristics and outcomes of patients hospitalized with ischemic stroke at the Neurology Clinic CCUS.
Material and methods
The study was retrospective and included time period from 1st June 2010 to 30th November 2010. The study included patients of both sexes, older than 18 years of age.
Results
The study included a total of 233 patients. Of these, 65% are female, while 35% of patients were male. Of 82 patients who were admitted to hospital treatment at the Neurology Clinic, 55% of the patients were male and 45% female. The largest number of patients is older than 70 years (71%). Minimum time for emergency medical team arrival was 6 minutes and maximum 70 minutes (mean 35, SD 11.989). Motor weakness was noted in 31% of patients – left sided motor weakness was significantly more represented. In 73% of patients the diagnosis was confirmed. In 5% of patients thrombolytic therapy was administered, while 95% of patients were treated conservatively. Lethal outcome occurred in 30% of hospitalized patients, 37% were discharged as recovered, 30% were discharged as unaltered state, while 3% were discharged with worsening symptoms. Among risk factors, hypertension is the leading one, followed by an earlier stroke, diabetes mellitus, and cardiac arrhythmias.
Conclusions
In 91% of patients consciousness was preserved. In 73% of transported patients has been confirmed the diagnosis of ischemic stroke. Of the patients with confirmed diagnosis 59% were hospitalized. A significant number of strokes occur for the first time in relation to relapse. 5% of patients were treated with thrombolysis, while others were treated with conservative therapy. Recurrent stroke and patient confusion have significant impact on the outcome.
Key words: stroke, emergency medical care, hospitalization, triage, risk factors, neurology
1. INTRODUCTION
Stroke is a clinical term for acute loss of perfusion in vascular territory of the brain, resulting in ischemia and corresponding loss of neurological functions (1, 2, 3, 4). A stroke occurs due to ruptured cerebral artery or occlusion by thrombus or embolus of any kind. The result is a focal cerebral dysfunction, which is manifested by a sudden onset of symptoms such as a sudden focal neurological deficit, weakness, sensory deficits or difficulties with speech (5, 6). Stroke remains the third leading cause of death and the leading cause of long term disability despite advances in prevention, diagnosis, treatment and rehabilitation. Social and economic consequences of stroke are burden to patients, society in terms of premature death, long-term disability, restrictions in social functions, the cost of care and loss of productivity.
It is assumed that each year in the European Union occurs around 1 million first ischemic strokes, affecting population of 450 million (1). In the United States approximately 700 000 individuals suffer a stroke each year, of which 200 000 of them are people with recurrent stroke. The number of people with TIA and thus an increased risk of stroke are estimated to be much higher (2).
Developments in the last decade in the field of acute stroke care have emphasized the critical role of emergency medical services in optimizing the care for stroke patients (3). Recent data show that 29% to 65% of patients with signs of acute stroke access initial medical care through the local emergency medical services. While this is slightly more than half of patients, those who report to emergency medical services represent the majority of patients who come to adequate health facilities in the threehour window (7, 8, 9, 10). Because the rapid evaluation and diagnosis is very significant, all patients with suspected acute stroke should be evaluated with the same priority as patients with acute myocardial infarction or serious trauma, regardless of the severity of the deficit. General supportive care should be provided and treat acute complications (4). Patients who have had TIA or who have had a stroke are at increased risk of stroke relapse, which is a huge source of increased mortality and morbidity. Long-term care and a review of risk factors is of great importance in patients who are at high risk but did not develop a stroke, and in patients who had previous stroke or TIA (11, 12, 13).
Prehospital care of patients includes all the services that are needed in the management of patients with stroke, starting with a call to the dispatch center number 124, which activates an emergency medical response, triage and stabilization of the patient on site, to transport of the patient either by land or air to an appropriate medical facility or between the institutions (3). The most important goal of prehospital care of stroke patients include the identification of patients on site, providing adequate prehospital care and transport of the patient to an appropriate medical facility, which preferably has a unit for acute stroke.
In the prehospital environment, general supportive care and early initiation of treatment for stroke risk factors significantly affects the final outcome of the patient. Maintaining adequate tissue oxygenation is of great importance in acute cerebral ischemia. The underlying idea is to prevent hypoxia and potential further deterioration of brain injury. Patients with disorders of consciousness are those who are at most risk for compromised airway due to loss of protective reflexes. Such patients require endotracheal intubation, and generally their prognosis is poor, so about 50% of these patients dies within 30 days after stroke. Most patients with stroke do not need supplementary oxygen, except in cases where the oxygen saturation on atmosphere pressure is below 94% (4). Raised and lowered blood pressure is associated with a worse stroke outcome.
Blood pressure is usually elevated during the first 24 hours after stroke onset. Due to impairment of cerebrovascular auto regulation after acute stroke, it is believed that the cerebral blood flow is very sensitive to changes in blood pressure. High blood pressure after acute stroke increases cerebral blood flow in the ischemic area of the brain. However, elevated blood pressure increases the risk of cerebral edema and hemorrhagic transformation of the infarction. Clinical studies has been found that it is safe to start again the administration of antihypertensive therapy, about 24 hours after stroke in patients with pre-existing hypertension, which are neurologically stable and in which there are no contraindications (4, 6). Persistent hypotension is rare in patients with acute ischemic stroke and is associated with an increased probability of poor outcome. Neurological deterioration, poor neurological outcome and mortality increases in case of systolic blood pressure <100 mmHg and diastolic blood pressure <70 mm Hg. It is necessary to start early correction of hypovolemia with physiological infusion and optimize cardiac output, with adequate treatment of arrhythmias.
Hyperglycemia is detected in about one third of patients with stroke. The presence of hyperglycemia is associated with a worse outcome, as well as prior history of diabetes mellitus. However, there are doubts about at which level of glucose in the blood the treatment should start. American and European guidelines on this issue are somewhat different. By EUSI (European Stroke Initiative) glucose level >10 mmol/l requires insulin treatment, but by ASA (American Stroke Association) value > 11 mmol/l indicate requirement for insulin treatment. Topic of many discussions is that insulin therapy should be initiated at lower blood glucose levels if the level is above 7 mmol/l (4, 9). Hypoglycemia can cause focal neurological injuries that can mimic a stroke, can cause brain injury, which is why it is very important to timely determine blood glucose levels and correct low value (4).
In patients with stroke, there is a potential risk of myocardial ischemia and the occurrence of arrhythmias, which probably arises from damage to a secondary function of the autonomic nervous system. From all the cardiac arrhythmias that occur in stroke most often seen is atrial fibrillation. In patients with stroke treatment is usually limited to the regulation of heart rate. The reason why cardio conversion is attempted is that in the atrium thrombus may occur which would be released after the conversion as an embolus, further complicating the patient’s condition (4, 5).
2. GOALS
The goals of this study are: Determine the number, gender and age representation of patients with a working diagnosis of acute stroke referred by the Institute for Emergency Medical Care (IEMC) to the Neurology Clinic, Clinical Center University of Sarajevo. Determine the prevalence of patients that have been hospitalized, and the reasons why the patients are not hospitalized. Determine the time and procedures of emergency medical care. Identify the characteristics and outcomes of patients hospitalized with ischemic stroke in the Neurology Clinic, CCUS.
3. MATERIAL AND METHODS
The study was retrospective and the total sample included patients who were referred to the Neurology Clinic by IEMC over the period from June 2010 by the end of November 2010, in which was recognized the risk factors and those who received treatment before or during transport to the Neurology Clinic, regardless of whether they are hospitalized. The study included patients of both sexes, older than 18 years of age.
This study did not include patients which had other somatic diseases and disorders (cancer, hematological diseases, terminal retention of urine, hemodialysis patients, etc.) that can cause dominant lethal outcome or contribute to disability. The study was conducted based on the usual methods of access to the primary examination, a short neurological examination, medical history, establishing the status of consciousness and measuring vital signs.
4. RESULTS
Of the total of 233 patients, 152 patients are female (65%) while 81 patients are male (35%). Of the total number of patients, 166 of them were aged over 70 years, representing 71% of total sample. Of the total number of respondents 211 had a preserved state of consciousness, which represents 91%. From the baseline sample 231 patients were examined on presence of confusion. It was found that in 138 patients there were no signs of confusion (60%), while in 93 patients (40%) were signs of confusion. Patients who are admitted to the hospital treatment were 5.8 times less confused than those who were not admitted to hospital. In 232 patients was examined orientation in space and time and to third parties. 150 patients (65%) were oriented and the other 82 (35%) had loss of orientation.
Patients admitted to hospital treatment were 1.7 times more frequently disoriented than patients who were not admitted to hospital treatment. In all 233 patients was examined response to verbal stimuli. In 210 cases (90%) there was a response to verbal stimuli, whereas in 23 cases (10%) there was no response to verbal stimuli. In all 233 patients were examined responses to a painful stimulus. 217 (93%) cases had the response to a painful stimulus, while in 16 (7%) cases there was no response. In 230 patients anisocoria was tested which was determined in 9 patients (4%). In 218 patients breathing was examined breathing. Normal breathing was found in 205 (94%), while in 13 cases was identified shallow respiration (6%). 197 patients underwent cardiac monitoring. In 124 patients (53%) was recorded sinus rhythm, while arrhythmias were recorded in 49 patients (21%). Motor weakness was observed in 72 patients (31%).
On admission to hospital treatment have a significant influence patient’s gender, motor weakness and confusion. Patients who were admitted to hospital treatment 14 times more had motor weakness of those who are not admitted to hospital treatment. There was no correlation between motor weakness and the hospital treatment outcome.
Motor weakness was observed in 72 patients, in 45 cases (62%) it was left-sided weakness, whereas 27 patients (38%) suffered from right-sided weakness. There was no correlation between left-sided motor weakness and admission to hospital treatment. Of the total number of patients 16 (7%) had associated injuries.
Of the total number of patients 213 were transported to hospital, while 20 patients were not transported mainly because of the refusal of the patient or family (Table 1).
Table 1.
Treatment procedure
| TREATMENT PROCEDURE | |
|---|---|
| IV access | 160 |
| O2 | 81 |
| Infusion | 11 |
| Digoxin | 11 |
| Catheter | 0 |
| Glucose | 6 |
| Metamizole sodium | 1 |
| Diclofenac sodium | 1 |
| Diazepam | 5 |
| Phenothiazine | 4 |
| Metoclopramide | 4 |
| Ranitidine | 1 |
| Hydrocortisone | 2 |
| Dexamethasone | 0 |
| Oral antihypertensive | 2 |
| Aspirin | 0 |
| Transported | 213 |
| Not transported | 20 |
Hospitalized patients who had an unfavorable (deteriorated, lethal) treatment outcome had 0.29 times less IV access than patients who had a favorable outcome. The use of oxygen in the prehospital treatment showed no significant difference between patients who had a favorable outcome and patients who have had an adverse (deteriorated, lethal) outcome.
The time of IEMC team represents a period from receiving a call to a dispatch center, team’s referral, team arrival on site, review of patient care and treatment of the patient, patient transportation and handing over the patient to hospital team. If the patient is not transported, the time ends with the departure of the team from the site. Minimum time of IEMC team was 6 minutes, while the maximum time was 70 minutes. Consideration that should be taken into account are distance (time required to reach the patient), the severity of the patient state and the time needed for patient transport.
Of the total number of transported patients in 155 was confirmed the working diagnosis, which represents 73% of transported patients under the working diagnosis of acute stroke.
Of the total number of patients with confirmed diagnosis of acute stroke, 82 patients (53%) were admitted to hospital treatment at the Neurology Clinic, 9 patients (6%) were admitted to hospital treatment at other clinics, while 64 patients (41%) were not hospitalized.
Of 9 patients with confirmed diagnosis and which are not admitted to the Neurology Clinic, two were admitted at IICU (internist intensive care unit), 5 were admitted to the Clinic of Neurosurgery, while one patient was admitted to the Clinic of Endocrinology and one of Cardiology.
Of the total number of patients with confirmed the diagnosis (155 patients), there were 64 who are not admitted to hospital treatment. As a reason, withdrawal of symptoms (TIA) and the lack of the capacity were equally represented by 28%. In six cases, the patient refused hospitalization or the patient’s family, while lethal outcome had six patients at the Center for emergency medicine of CCUS. Of 58 patients in whom the diagnosis of acute stroke was not confirmed, 11 patients were admitted to hospital for the treatment of other medical conditions which required hospital treatment in other clinics (Table 2).
Table 2.
patients in whom the diagnosis was not confirmed and were admitted to one of the other clinics
| OTHER DIAGNOSIS – ADMISSION TO APPROPRIATE CLINICS | |
|---|---|
| Cardiology | 4 |
| Vascular surgery | 1 |
| Endocrinology | 2 |
| Neurosurgery | 2 |
| Angiology | 1 |
| ICU | 1 |
| Total | 11 |
Of 82 patients who were hospitalized at the Neurology Clinic 55% (46) patients were male, while 45% (36) were female.
On admission to hospital treatment significant influence have patients gender, motor weakness and confusion. Of the total number of patients admitted to hospital treatment at the Neurology Clinic 58 patients (71%) were aged over 70 years. Eight patients were in the age group below 40 years, which represents 10% of the total number of hospitalized patients. Of 82 patients who were hospitalized at the Neurology Clinic in 55 patients (67%) stroke occurred for the first time. In 27 cases was recurrent stroke (33%). Of 82 patients who were admitted to hospital treatment at the Neurology Clinic, 78 patients were treated using a conservative method, while 4 patients (5%) were treated with thrombolysis. In consideration should be taken strict criteria for thrombolytic therapy.
In 25 patients (30%) the outcome was lethal, in 24 patients the outcome was unchanged, 31 patients (37%) was released from the Neurology Clinic as recovered, while for two patients condition was exacerbated in relation to the admission. Patients who had unchanged or unfavorable (aggravated, lethal) outcome were 2.8 times more likely to have a recurrent stroke than patients who had a favorable outcome, or patients with recurrent stroke had worse outcomes than those in which the stroke occurred for the first time. Comparative values of risk factors (hypertension, heart rate, glucose level) in patients who were admitted to hospital treatment, as well as those who are not admitted to the hospital treatment, are shown in Figures 1, 2 and 3.
DISCUSSION
The study included a total of 233 patients of whom 152 are women (65%) and 81 (35%) men. Of 82 patients who were admitted to hospital treatment at the Neurology Clinic 46 patients (55%) were male, while the remaining 36 (45%) are female. Although the incidence and mortality rate are higher in men, women experience a greater number of strokes a year because they live longer (> 85 years) women have a higher mortality rate than men. These differences in the incidence, prevalence and prognosis of stroke outcomes in women will become more significant (4, 17, 18). The largest number of patients, 177 of them (71%) was at age older than 70 years. Age of the patient is one of the most significant independent predictors of stroke. It was expected that the number of patients increase with age. Frequency of ischemic stroke rises sharply at the age of 40 years old, when patients have multiple risk factors.
Minimum time for emergency medical team was 6 minutes while the maximum was 70 minutes, on average 35 min (SD 11.9). Such rapid transport leaves enough space to perform additional diagnostic methods to confirm acute ischemic stroke, the patient examination by a neurologist and that adequate therapy. According to research conducted in America about the time of pre-hospital treatment and transport before and after implementation of the guidelines of American Coalition for stroke, it was found that the total time, before arrival of the emergency team to the handing over the patient to the hospital was on average 42.2 minutes (3, 4, 7, 8). Of 233 patients in whom the diagnosis of stroke, 20 patients were not transported because of the refusal of the patient or family. In 91% of patients consciousness was preserved, 60% of patients was not confusing, 65% of patients were oriented in time and space, 90% of patients have a response to verbal stimuli, while 93% had a reaction to a painful stimulus, in 4% of patients were found anisocoria. Motor weakness was present in 31% of patients, left-sided motor weakness was significantly more prevalent, 62% compared to the right-sided weakness. Of 213 patients who were transported in 160 was established IV access, 81 patients received oxygen therapy. Monitoring has found that in 53% of patients had sinus rhythm and 21% patients had arrhythmia, 6% of tachycardia, bradycardia in about 3%, while in the 1% was implanted permanent pacemaker. In all patients in whom the arrhythmia was registered, it was a case of atrial fibrillation. According to research, one of the six ischemic strokes is associated with atrial fibrillation. Of 213 patients who were transported to the hospital under the working diagnosis of stroke in 155 patients (73%) the diagnosis was confirmed. Of 58 patients in whom the diagnosis was not confirmed, 11 patients were admitted to hospital for treatment of other health conditions that have required hospitalization. Of 155 patients who had confirmed the diagnosis of acute ischemic stroke, 53% were admitted to hospital treatment at Neurology Clinic, 6% were admitted to another hospital, while 41% of patients were not hospitalized. According to research conducted in Germany, nearly 95% of all stroke patients are hospitalized for acute treatment. Even in older patients (>75 years) the admission rate was 90% (15).
From 64 patients who were not admitted to hospital treatment in 28% occurred symptoms withdrawal (TIA), 28% were not admitted because of the lack of capacity, 10% of patients died in Center for emergency medicine, while 9% of patients or family members refused hospitalization, while for 17% is not known why they were not admitted to hospital treatment. Of the 82 patients admitted to the Neurology Clinic stroke occurred for the first time in 67% of patients, while relapse was recorded in 33%. By gender, 45% of the patients were female, 55% were male. Mostly these were elderly patients, 71% at >70 years of age, 14% at age 60-70, 5% at age 50-60 and 10% <40 years of age.
Our research has shown that 95% of patients admitted to the Neurology Clinic were treated conservatively, while 5% were treated with thrombolysis. Our research has shown that 30% of admitted patients had lethal outcome, 37% were discharged as recovered, 30% were discharged in unaltered state, while 3% of patients were discharged with worsening symptoms. The outcome of hospital treatment is significantly influenced by stroke relapse (recurrence), patient confusion and established IV access during the pre-hospital care.
Our research has given information that among risk factors, the leading is hypertension, followed by an earlier stroke, diabetes mellitus and cardiac arrhythmias. In 40% of patients was found more than one risk factor. According to a study conducted in Germany, with all subtypes of ischemic stroke the leading risk factor was hypertension with 66.6%, previous stroke in 22.8%, earlier TIA in 12.7%, diabetes mellitus in 28.5% and heart arrhythmias in 26.1% of cases (12, 15).
Ischemic stroke is polyetiologic disease, in which the influence of risk factors is evident. It can be concluded that the risk factors (glycaemia, hypertension, heart rhythm disorders) significantly influence the occurrence of first and repeated stroke, the stroke severity, the choice of treatment, occurrence of complications, degree of disability and mortality (21, 22). Early detection and early initiation of treatment with rapid transport of patient to an adequate medical facility is of outmost importance for the better outcome.
5. CONCLUSIONS
There was a larger number of female patients (65%) in whom the working diagnosis of stroke was set (IEMC), but the larger was the number of male patients (55%) who were admitted to hospital treatment at the Neurology Clinic.
Most patients were older than 70 years (71%). Mean time of emergency medical team was 33 minutes and the maximum time was 70 minutes. In 91% of patients consciousness was preserved. Motor weakness was present in 31% of patients, with higher representation of left-sided weakness (62%). In 73% of transported patients has been confirmed the working diagnosis of ischemic stroke. Of patients who had confirmed the diagnosis 53% were admitted to hospital treatment at the Neurology Clinic, 6% were admitted to another hospital, while 41% of patients were not admitted to hospital treatment.
There were a significantly larger number of strokes that occur for the first time in respect of recurrent stroke. By thrombolysis were treated 5% of patients, while other patients were treated with conservative therapy. For 30% of admitted patients the outcome was lethal, 37% were discharged as recovered, 30% were discharged with unaltered state, while 3% of patients were discharged with worsening symptoms. Recurrent stroke and patient confusion have significant impact on the outcome. Among risk factors, leading is hypertension, followed by an earlier stroke, diabetes mellitus and cardiac arrhythmias.
Figure 1.
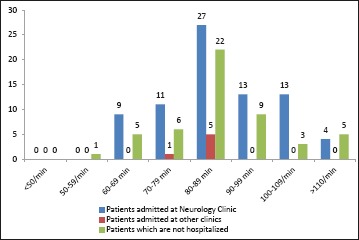
Comparison of heart rate values
Figure 2.
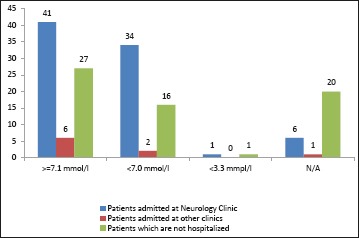
Comparison of blood glucose values
Figure 3.
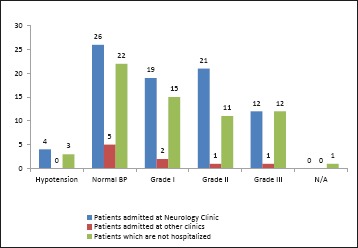
Comparison of blood pressure values
REFERENCES
- 1.Ralph L., et al. Transient Ischemic Attack: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association Council on Stroke. Stroke. 2006; 37; 577-617 [DOI] [PubMed] [Google Scholar]
- 2.Joe E., et al. Implementation Strategies for Emergency Medical Services Within Stroke Systems of Care: A Policy Statement From the American Heart Association/American Stroke Association Expert Panel on Emergency Medical Services Systems and the Stroke Council. Stroke. 2007; 38; 3097-3115; [DOI] [PubMed] [Google Scholar]
- 3.Harold P., et al. Guidelines for the Early Management of Adults With Ischemic Stroke: A Guideline From the American Heart Association/ American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Stroke. 2007; 38; 1655-1711; originally published online Apr 12, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Vrhovec B., et al. Interna medicina, treće promijenjeno i dopunjeno izdanje, Naklada Ljevak Zagreb, 2003. godine. 1616-1618, 488-490 [Google Scholar]
- 5.Jauch EC.Acute Stroke Management. Updated: Jun 8, 2009 [Google Scholar]
- 6.Sacco RL., et al. Guidelines for Prevention of Stroke in Patients With Ischemic Stroke or Transient Ischemic Attack: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association Council on Stroke. Stroke. 2006; 37; 577-561 [DOI] [PubMed] [Google Scholar]
- 7.Ohira T., et al. Risk Factors for Ischemic Stroke Subtypes: The Atherosclerosis Risk in Communities Study. Stroke. 2006; 37; 2493-2498; originally published online Aug 24, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Blaser T., et al. Risk of Stroke, Transient Ischemic Attack, and Vessel Occlusion Before Endarterectomy in Patients With Symptomatic Severe Carotid Stenosis. Stroke. 2002; 33; 1057-1062 [DOI] [PubMed] [Google Scholar]
- 9.Grau AJ., et al. Risk Factors, Outcome, and Treatment in Subtypes of Ischemic Stroke: The German Stroke Data Bank. Stroke. 2001; 32; 2559-2566 [DOI] [PubMed] [Google Scholar]
- 10.Gargano JW., et al. Sex Differences in Acute Stroke Care in a Statewide Stroke Registry. Stroke. 2008; 39; 24-29; originally published online Nov 29, 2007 [DOI] [PubMed] [Google Scholar]
- 11.Lichtman JH., et al. Elderly Women Have Lower Rates of Stroke, Cardiovascular Events, and Mortality After Hospitalization for Transient Ischemic Attack. Stroke. 2009; 40; 2116-2122; originally published online Feb 19, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tadros A., et al. Emergency Medical Services-Based Community Stroke Education: Pilot Results From a Novel Approach. Stroke. 2009; 40; 2134-2142; originally published online Apr 9, 2009. [DOI] [PubMed] [Google Scholar]
- 13.Schroeder EB., et al. Determinants of Use of Emergency Medical Services in a Population With Stroke Symptoms: The Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000; 31; 2591-2596 [DOI] [PubMed] [Google Scholar]
- 14.Adams HP., et al. Guidelines for the Early Management of Patients With Ischemic Stroke: A Scientific Statement From the Stroke Council of the American Stroke Association. Stroke. 2003; 34; 1056-1083 [DOI] [PubMed] [Google Scholar]
- 15.Aslanyan S., et al. Effect of Blood Pressure During the Acute Period of Ischemic Stroke on Stroke Outcome: A Tertiary Analysis of the GAIN International Trial. Stroke. 2003; 34; 2420-2425; originally published online Sep 18, 2003. [DOI] [PubMed] [Google Scholar]
- 16.McCormick MT., et al. Management of Hyperglycemia in Acute Stroke: How, When, and for Whom? Stroke. 2008; 39; 2177-2185; originally published online Apr 24, 2008 [DOI] [PubMed] [Google Scholar]
- 17.Gene JS., et al. Effective Glycemic Control With Aggressive Hyperglycemia Management Is Associated With Improved Outcome in Aneurysmal Subarachnoid Hemorrhage. Stroke. 2009; 40; 1644-1652; originally published online Mar 12, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyvärinen M., et al. Hyperglycemia and Incidence of Ischemic and Hemorrhagic Stroke-Comparison Between Fasting and 2-Hour Glucose Criteria. Stroke. 2009; 40; 1633-1637; originally published online Mar 12, 2009 [DOI] [PubMed] [Google Scholar]
- 19.Gray LJ., et al. Sex Differences in Quality of Life in Stroke Survivors: Data From the Tinzaparinin Acute Ischaemic Stroke Trial (TAIST). Stroke. 2007; 38; 2960-2964; [DOI] [PubMed] [Google Scholar]
- 20.Sappok T., et al. Compliance With Secondary Prevention of Ischemic Stroke: A Prospective Evaluation. Stroke. 2001; 32; 1884-1889 [DOI] [PubMed] [Google Scholar]
- 21.Muhhamed Amin OS.Left Ventricular Hypertrophy: a Comparison Among Kurdish Patients with First-ever Ishchemic Versus First-ever Hemorrhagic Stroke. Med Arh. 2013. Apr; 67(2): 101-103 doi: 10.5455/ medarh.2013.67.101-103 [DOI] [PubMed] [Google Scholar]
- 22.Suljic E, Kulasin I, Alibegovic V.Assessment of Diabetic Dysfunction in Asymptomatic Type 2 Diabetic Patients: Detection and Evaluation by issue Doppler Imaging. Acta Inform Med. 2013. Mar; 21(2): 123-126 [DOI] [PMC free article] [PubMed] [Google Scholar]


