Abstract
Marked increases in the awareness, treatment and control of high LDL-cholesterol occurred among US adults between 1988–1994 and 1999–2004. An update to the ATP-III guidelines was published in 2004 and it is unknown if these improvements have continued following publication of these revised treatment recommendations. We determined trends in the awareness, treatment and control of high LDL-cholesterol among US adults from 1999– 2000 through 2009–2010 using nationally representative samples of US adults ≥ 20 years of age from six consecutive National Health and Nutrition Examination Surveys (NHANES) in 1999–2000 (n=1,659), 2001–2002 (n=1,897), 2003–2004 (n=1,698), 2005–2006 (n=1,692), 2007–2008 (n=2,044) and 2009–2010 (n=2,318). LDL-cholesterol was measured after an overnight fast and high LDL-cholesterol and controlled LDL-cholesterol were defined using the 2004 updated ATP-III guidelines. Awareness and treatment of high cholesterol were defined using self-report. Among US adults, the prevalence of high LDL-cholesterol did not change from 1999–2000 (37.2%) through 2009–2010 (37.8%). Awareness of high LDLcholesterol increased from 48.9% in 1999–2000 to 62.8% in 2003–2004 but did not increase further through 2009–2010 (61.5%). Among those aware of having high LDL-cholesterol, treatment increased from 41.3% in 1999–2000 to 72.6% in 2007–2008 and was 70.0% in 2009–2010. Among US adults receiving treatment for high LDL-cholesterol, the percentage with controlled LDL-cholesterolincreased from 45.0% in 1999–2000 to 65.3% in 2005–2006 and decreased slightly by 2009–2010 (63.6%). High LDL-cholesterol remains common among US adults. Additional efforts are needed to prevent high LDL-cholesterol and increase the awareness, treatment and control of high LDL-cholesterol among US adults.
Keywords: LDL-cholesterol, statins, treatment, awareness, risk factors
Analyses have showed that marked increases in the awareness, treatment and control of high LDL-cholesterol among US adults occurred after the publication of the Third Adult Treatment Panel (ATP-III) cholesterol guidelines in 2001.1,2 However, in 2003–2004, less than 50% of US adults with high LDL-cholesterol were receiving lipid-lowering treatment and less than 25% had controlled their LDL-cholesterol to the levels recommended by the ATP-III guidelines.2 Several randomized trials have been published since the release of ATP-III and an update to the ATP-III with revised treatment recommendations was published in 2004.3A recent analysis of National Health and Nutrition Examination Survey (NHANES) data found the mean LDL-cholesterol has among US adults declined from 1988 through 2010.4 However, this report did not evaluate the prevalence and trends of high LDL-cholesterol and awareness, treatment and control among US adults. Documenting these trends may provide a useful benchmark given the forthcoming update to the ATP cholesterol guidelines.The main goal of our study was to document trends in high LDL-cholesterol prevalence, awareness, treatment and control among US adults from 1999– 2000 through 2009–2010. To achieve this goal, we analyzed data from six serial population-based NHANES.
METHODS
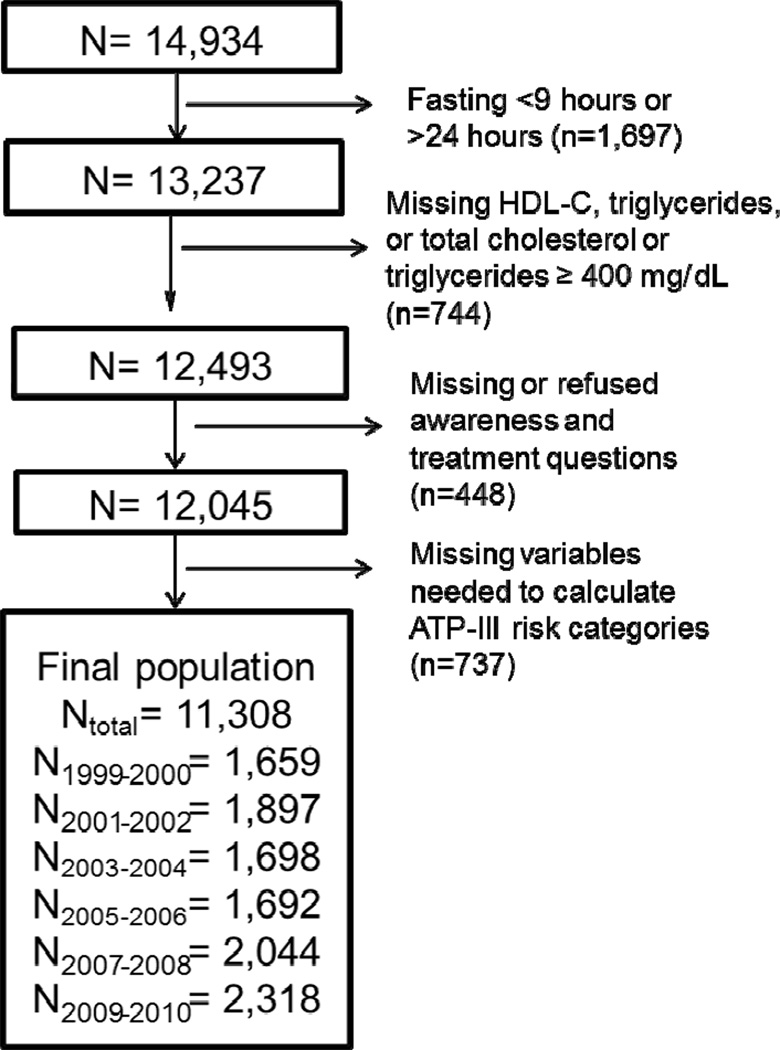
NHANES 1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, and 2009– 2010 were conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. Each two year period included a sample of the non-institutionalized civilian US population identified through a stratified, multistage probability sampling design. This approach allows nationally representative prevalence estimates to be generated. The current analysis was limited to adult participants, 20 years of age and older who were assigned to attend a morning study visit (n=14,934). Participants are assigned for a morning study visit such that national estimates can be generated from this sample. After excluding individuals who did not fast or were missing data, there were 11,308 participants included in these analyses (Figure 1). The protocol for each NHANES was approved by the National Center for Health Statistics of the Centers for Disease Control and Prevention Institutional Review Board. Informed consent was obtained from each participant.
Figure 1.
Selection of participants for the current analysis of LDL-cholesterol among participants in NHANES 1999–2000 through NHANES 2009–2010.
Data for the current analysis were collected through standardized procedures that included questionnaires, a medical examination, and phlebotomy. Participant awareness of the presence of high LDL-cholesterol was defined by an affirmative response to the question “Have you ever been told by a doctor or other health professional that your blood cholesterol was high”. Use of lipid-lowering treatment was defined by affirmative responses to the following two questions “To lower your cholesterol, have you ever been told by a doctor or other health professional to take prescribed medicine?” and “Are you now following this advice to take prescribed medicine?” Based on the average of three blood pressure measurements taken during the study visit, hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg or self-reported use of antihypertensive medication. Waist circumference was measured to the nearest 0.1 cm at the level of the iliac crest at the end of normal respiration.
Blood collection and processing are detailed in the NHANES Laboratory/Medical Technicians Procedures Manuals.5 Diabetes mellitus was defined as a fasting plasma glucose ≥ 126 mg/dL or self-report of a history of diabetes with concurrent antidiabetes medication use. Total- and HDL-cholesterol and triglycerides were measured using the Hitachi 704 Analyzer and reagents purchased from Roche/Boehringer Mannheim Diagnostics, Indianapolis, IN. LDL-cholesterol was calculated using the Friedewald equation.6 Using measurement of glucose, blood pressure, waist circumference, HDL-cholesterol and triglycerides from the in-home study visit, the metabolic syndrome was defined using the harmonized definition.7
For the purpose of diagnosis, treatment and control of LDL-cholesterol, the 2004 updated ATP-III guidelines classify individualsbased on their global CHD riskinto one of fourmutually exclusive CHD risk categories: (1) no CHD or CHD risk equivalents and 0–1 major CHD risk factors (0–1 risk factors), (2) no CHD or CHD risk equivalents and two or more major CHD risk factors (2+ risk factors), (3) CHD not at very high risk and/or CHD risk equivalents (CHD or risk equivalent), and (4) CHD at very high risk (CHD at very high risk). CHD risk factors include older age (≥55 years for women and ≥45 years for men), current cigarette smoking, hypertension, family history of CHD (history of myocardial infarction or angina before age 50 years among first-degree relatives), and low HDL-cholesterol (<40 mg/dL). HDL cholesterol ≥ 60 mg/dL is considered protective and offsets the presence of one these risk factors. Participants who reported a prior diagnosis of CHD or myocardial infarction were defined as having a history of CHD. Risk equivalents included a 10-year risk for CHD > 20% estimated by the Framingham equation in the ATP-III report or history of stroke or diabetes mellitus. Data on other ATP-III risk equivalents (e.g., peripheral arterial disease, aortic aneurysm) were not routinely collected in NHANES and not used in the current analyses. Among people with CHD, current smoking, diabetes mellitus and metabolic syndrome place them in the very high risk category. High LDL-cholesterol and LDL-cholesterol control were defined using the 2004 update of the ATP-III treatment guidelines (Table 1).3
Table 1.
Definitions of high low-density lipoprotein cholesterol and control in the updated (2004) Adult Treatment Panel (ATP)-III guidelines.
| High LDL-C | Control | |
|---|---|---|
| History of coronary heart disease at very high risk* | LDL-C ≥ 70 mg/dL or use of lipid-lowering therapy | LDL-C < 70 mg/dL |
| History of coronary heart disease† or risk equivalent | LDL-C ≥ 100 mg/dL or use of lipid-lowering therapy | LDL-C < 100 mg/dL |
| 2+ coronary heart disease risk factors and 10 year Framingham risk of 10 – 20% | LDL-C ≥ 100 mg/dL or use of lipid-lowering therapy | LDL-C < 100 mg/dL |
| 10 year Framingham risk < 10% | LDL-C ≥ 130 mg/dL or use of lipid-lowering therapy | LDL-C < 130 mg/dL |
| 0–1 coronary heart disease risk factors | LDL-C ≥ 160 mg/dL or use of lipid-lowering therapy | LDL-C < 160 mg/dL |
LDL-C: low-density lipoprotein cholesterol; CHD: coronary heart disease
Very high risk defined by having a history of CHD and diabetes mellitus, cigarette smoking and/or the metabolic syndrome
Not including individuals at very high risk
Coronary heart disease risk equivalents included diabetes mellitus and stroke
Coronary heart disease risk factors include older age (≥55 years for women and ≥45 years for men), current cigarette smoking, hypertension, family history of coronary heart disease (history of myocardial infarction or angina before age 50 years among first-degree relatives), and low HDL-cholesterol. HDL cholesterol ≥ 60 mg/dL is considered protective and offsets the presence of one these risk factors.
Participant characteristics and the prevalence of high LDL-cholesterol were calculated for each 2 year NHANES period. Among those with high LDL-cholesterol, we calculated the percent who were aware of their diagnosis. Prevalence of treatment was calculated for all people with high LDL-cholesterol and those aware of their diagnosis. The proportion of US adults with controlled LDL-cholesterolwas calculated for all people with high LDL-cholesterol and for those receiving treatment. Trends over time were calculated using logistic regression with calendar period as an ordinal independent variable. Deviations from linearity were assessed by modeling calendar period as a quadratic term. Trends were calculated overall and for sub-groups defined by age, race-ethnicity, gender, and CHD risk categories.We calculated the number of US adults in 2007–2010 with high LDL-cholesterol, overall and by CHD risk categories. To identify reasons people did not have controlled LDL-cholesterol, we calculated the number and percent of US adults with high LDL-cholesterol: (1) not aware of their diagnosis of high LDL-cholesterol, (2) aware but not treated, (3) treated but not controlled, and (4) with controlled LDL-cholesterol. Many people with uncontrolled LDL-cholesterol may be close to achieving their goal. Therefore, for US adults with uncontrolled high LDL-cholesterol, we calculated the percentage whose LDL-cholesterol was ≥ 30 mg/dL above their goal. Next, we used Poisson regression models to calculate the multivariable adjusted prevalence ratios for having high LDL cholesterol and awareness, treatment and control of this condition associated with CHD risk categories (0–1 risk factors [referent],2+ risk factors, CHD or risk equivalents, and CHD at very high risk) in the two most contemporary NHANES pooled together (NHANES 2007– 2010). We pooled NHANES 2007–2008 and 2009–2010 to achieve more reliable estimates (n>50 participants in every sub-population).Prevalence ratios included adjustment for age, gender, race-ethnicity, income, education and health insurance status.
All analyses were performed using SUDAAN 10.1 (Research Triangle Institute, Research Triangle Park, NC) accounting for the NHANES sampling design. To obtain US nationally representative prevalence estimates, morning fasting sampling weights were applied to all calculations. NHANES sampling weights were recalibrated based on the proportion of participants missing data by 10-year age group, sex, and race-ethnicity. Recalibration of the sampling weights corrects for differences in missing data across age, sex, and race-ethnicity strata, and assumes that data within strata are missing randomly.8
RESULTS
Characteristics of participants are presented by 2-year period (1999–2000 through 2009–2010) in Table 2. In more recent time periods, the population on average was older, less likely to have an annual household income <$20,000, more likely to have graduated high school, and less likely to be current versus never smokers. Also, in the more recent time periods, a higher percentage of participants had government or no health insurance. Body mass index was higher and the prevalence of diabetes increased while the prevalence of 2+ versus 0–1 CHD risk factors decreased over time. Mean LDL-cholesterol decreased from 125.6 mg/dL to 116.9 mg/dL between 1999–2000 and 2009–2010.
Table 2.
Characteristics of NHANES participants by 2-year survey period, 1999–2000 through 2009–2010
| Calendar period | Linear p-value |
Quadratic p-value |
||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | 1999–2000 (n=1659) |
2001–2002 (n=1897) |
2003–2004 (n=1697) |
2005–2006 (n=1692) |
2007–2008 (n=2041) |
2009–2010 (n=2316) |
||
| Age (years) | ||||||||
| < 50 | 64.6% | 63.0% | 60.9% | 60.0% | 58.2% | 56.9% | Ref | Ref |
| 50–64 | 20.6% | 22.8% | 23.6% | 22.8% | 24.9% | 25.0% | 0.012 | 0.753 |
| ≥ 65 | 14.8% | 14.2% | 15.6% | 17.2% | 16.9% | 18.1% | <0.001 | 0.978 |
| Male Gender | 48.0% | 48.0% | 48.0% | 47.6% | 48.4% | 48.3% | 0.812 | 0.822 |
| Race/Ethnicity | ||||||||
| Non-Hispanic White | 70.8% | 72.3% | 71.8% | 71.7% | 69.9% | 68.0% | Ref | Ref |
| Non-Hispanic Black | 10.2% | 10.8% | 11.5% | 11.1% | 11.0% | 11.2% | 0.574 | 0.918 |
| Hispanic | 15.0% | 12.2% | 10.9% | 11.5% | 13.3% | 13.8% | 0.912 | 0.270 |
| Other | 4.0% | 4.8% | 5.8% | 5.6% | 5.8% | 7.0% | 0.054 | 0.937 |
| Household Income < $20K | 18.0% | 16.8% | 16.8% | 12.1% | 14.2% | 14.8% | 0.020 | 0.172 |
| High School Graduate | 76.9% | 81.2% | 82.3% | 82.6% | 81.5% | 81.9% | 0.026 | 0.048 |
| Health Insurance | ||||||||
| Private | 63.7% | 61.6% | 55.8% | 57.1% | 58.6% | 53.2% | Ref | Ref |
| Government | 19.6% | 22.1% | 25.7% | 24.3% | 24.1% | 25.7% | <0.001 | 0.205 |
| None | 16.7% | 16.4% | 18.6% | 18.5% | 17.3% | 21.1% | 0.007 | 0.861 |
| Smoking Status | ||||||||
| Never | 49.4% | 50.0% | 51.8% | 50.6% | 54.7% | 56.0% | Ref | Ref |
| Current | 23.2% | 25.0% | 24.1% | 24.4% | 20.2% | 18.4% | 0.002 | 0.096 |
| Former | 27.5% | 25.0% | 24.1% | 25.1% | 25.1% | 25.7% | 0.179 | 0.583 |
| Body Mass Index (kg/m2) | ||||||||
| < 25 | 40.3 (1.9) | 34.4 (1.4) | 33.6 (1.3) | 33.6 (1.7) | 33.1 (1.1) | 31.3 (1.7) | Ref | Ref |
| 25 – 30 | 31.2 (0.9) | 37.1 (1.9) | 34.6 (2.0) | 31.9 (1.5) | 34.5 (1.0) | 32.7 (1.4) | 0.042 | 0.139 |
| ≥ 30 | 28.6 (1.8) | 28.5 (1.4) | 31.8 (1.5) | 34.6 (1.8) | 32.4 (1.4) | 36.0 (1.5) | <0.001 | 0.378 |
| Hypertension | 26.7% | 28.6% | 30.4% | 28.9% | 30.1% | 29.5% | 0.289 | 0.369 |
| Diabetes mellitus | 6.6% | 8.4% | 8.5% | 9.2% | 10.7% | 10.6% | <0.001 | 0.517 |
| CHD at very high risk† | 67.7% | 64.5% | 70.3% | 73.8% | 78.3% | 68.9% | 0.202 | 0.436 |
| CHD Risk category | ||||||||
| 0–1 risk factors | 62.9% | 61.6% | 62.8% | 66.1% | 62.1% | 63.9% | Ref | Ref |
| 2+ risk factors | 23.9% | 23.7% | 22.5% | 18.0% | 20.9% | 20.0% | 0.008 | 0.380 |
| CHD or risk equivalent | 10.6% | 11.6% | 11.3% | 12.2% | 12.8% | 12.9% | 0.174 | 0.995 |
| CHD at very high risk | 2.7% | 3.0% | 3.4% | 3.7% | 4.2% | 3.1% | 0.158 | 0.168 |
| Ever had cholesterol checked | 70.4% | 67.9% | 70.8% | 76.1% | 74.5% | 73.9% | 0.005 | 0.559 |
| LDL-cholesterol (mg/dL) | 125.6 (1.1) | 120.9 (1.6) | 116.8 (1.2) | 115.0 (1.3) | 116.0 (1.0) | 116.9 (1.1) | <0.001 | <0.001 |
Numbers in table are mean (standard error) or percent
CHD= Coronary Heart Disease
CHD risk categories were defined by (1) 0 – 1 risk factors - no CHD or CHD risk equivalents and 0–1 major CHD risk factors, (2) 2+ risk factors - no CHD or CHD risk equivalents and two or more major CHD risk factors, (3) CHD or risk equivalent - CHD not at very high risk and/or CHD risk equivalents and (4) CHD at very high risk - CHD with cigarette smoking, diabetes mellitus, or metabolic syndrome. See Table 1 for definitions of CHD risk factors and CHD risk equivalents.
Percentage of individuals with CHD who are cigarette smokers or have diabetes mellitus or metabolic syndrome
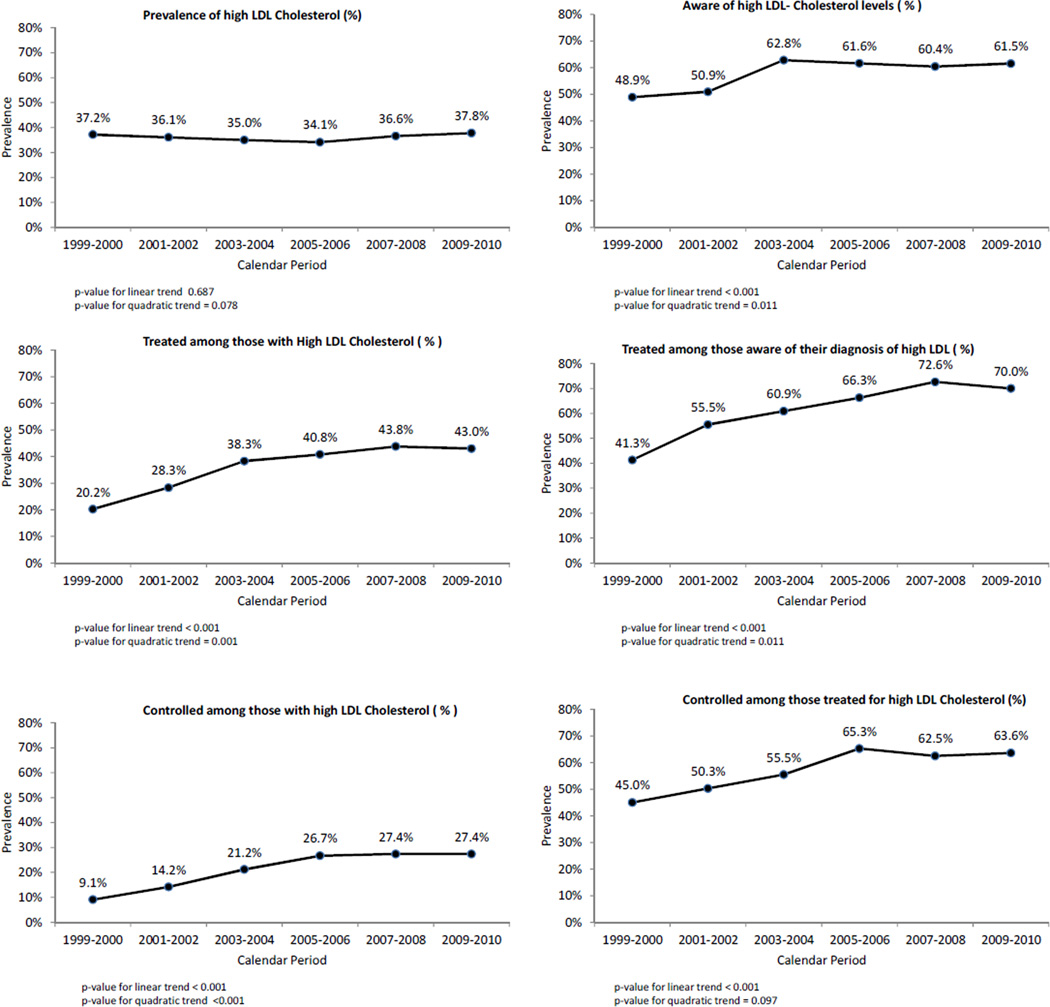
The prevalence of high LDL-cholesterol remained stable from 1999–2000 through 2009–2010 (Figure 2). Among those with high LDL-cholesterol, awareness of this condition increased from 1999–2000 to 2003–2004 but did not increase further through 2009–2010. Among those aware of having high LDL-cholesterol, the prevalence of treatment increased through 2007–2008 but did not increase further in 2009–2010. Among all US adults with high LDL-cholesterol and those receiving treatment, the prevalence of control increased from 1999–2000 to 2005–2006 but did not increase further by 2009–2010. Trends in the prevalenceof high LDL-cholesterol and awareness, treatment and control of this condition were consistent across age, race-ethnicity and gender sub-groups (Supplemental Table 1).
Figure 2.
Prevalence of high LDL-cholesterol and high cholesterol awareness, treatment and control of among US adults from 1999–2000 through 2009–2010.
Trends in the prevalence, awareness, and treatment of high LDL-cholesterol were consistent across CHD risk categories (Supplemental Table 2). LDL-cholesterol control improved in high risk groups, but in 2009–2010, only 58.3% of individuals with CHD or risk equivalents had controlled LDL-cholesterol and the proportion controlled among those with CHD at very high risk was even lower. In 2007–2010, higher CHD risk categories were associated with increased prevalence ratios for having high LDL-cholesterol (Table 3). Among those with high LDL-cholesterol, US adults with 2+ CHD risk factors and CHD or risk equivalents were less likely that those with 0–1 CHD risk factors to be aware of their high LDL-cholesterol diagnosis. Among those aware of their high LDL-cholesterol, treatment was more common among individuals with CHD or risk equivalents. Compared to individuals with 0 –1 CHD risk factors, people with 2+ CHD risk factors, CHD or risk equivalents and CHD at very high risk were less likely to have controlled LDL-cholesterol.
Table 3.
Adjusted* prevalence ratios (95% confidence intervals) for high low density lipoprotein cholesterol and for high cholesterol awareness, treatment, and control in NHANES 2007–2010.
| Prevalence ratio (95% confidence interval) | |||||
|---|---|---|---|---|---|
| Variable | High low-density lipoprotein-cholesterol‡ |
Aware† | Treated† † | Controlled††† | |
| CHD Risk Category | |||||
| 0–1 risk factors | 1 (ref) | 1 (ref) | 1(ref) | 1(ref) | |
| 2+ risk factors | 3.04 (2.65–3.49) | 0.76 (0.66–0.87) | 0.93 (0.77–1.13) | 0.63 (0.51–0.78) | |
| CHD or risk equivalent | 3.47 (3.01–3.99) | 0.86 (0.77–0.96) | 1.20 (1.03–1.41) | 0.71 (0.62–0.82) | |
| CHD at very high risk | 3.89 (3.37–4.50) | 0.96(0.86–1.07) | 1.21 (1.00–1.47) | 0.27 (0.18–0.41) | |
Adjusted for age, gender, race/ethnicity, income, education, and insurance status CHD - coronary heart disease
Among all individuals
Among all individuals with high LDL-cholesterol
Among individuals aware of their diagnosis of high LDL-cholesterol
Among those treated for high LDL-cholesterol
Very high risk defined by having a history of coronary heart and diabetes mellitus, cigarette smoking and/or the metabolic syndrome
Coronary heart disease risk equivalents included diabetes mellitus and stroke
Coronary heart disease risk factors include older age (≥55 years for women and ≥45 years for men), current cigarette smoking, hypertension, family history of coronary heart disease (history of myocardialinfarction or angina before age 50 years among first-degree relatives), and low HDL-cholesterol. HDL cholesterol ≥ 60 mg/dL is considered protective and offsets the presence of one these risk factors.
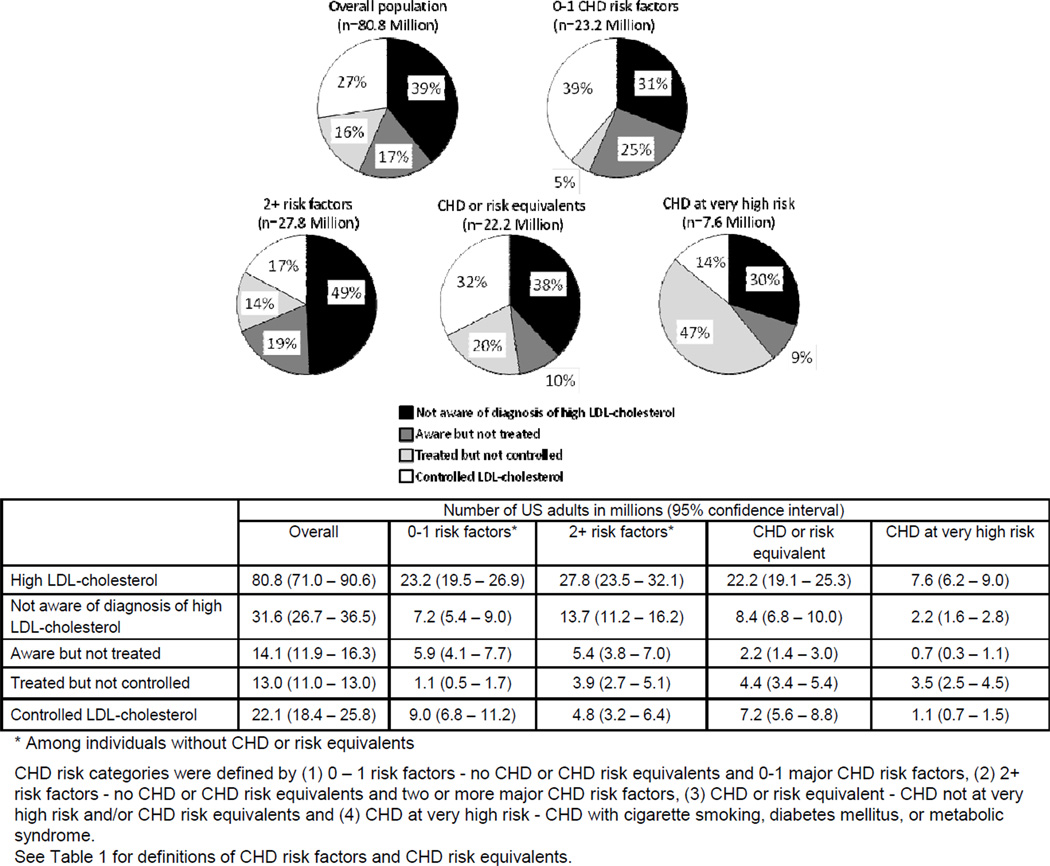
Among the US population in 2007–2010, 80.8 million adults had high LDL-cholesterol (Figure 3). Of those with high LDL-cholesterol, 39% were not aware of their diagnosis of high LDL-cholesterol, 17% were aware but not treated, 16% were treated and not controlled and 27% had controlled their LDL-cholesterol. The majority of the 23.2 million US adults withhigh LDL-cholesterol and 0–1 risk factors and 27.8 million US adults with 2+ risk factors were either not aware of this diagnosisor were aware but not treated. Only 5%and 14% of those with 0–1 and 2+ risk factors were treated but did not achieve their LDL-cholesterol goal, respectively. Among the 22.2 million US adults with CHD or risk equivalents, 20% were treated but did not have controlledLDL-cholesterol. Of the 7.6 million US adults with CHD at very high risk, 47% were treated but did not have controlled LDL-cholesterol and only 14% had controlled LDL-cholesterol.
Figure 3.
Number of US adults in 2007–2010 with high LDL-cholesterol by awareness, treatment and control status, overall and by coronary heart disease risk category.
For US adults with uncontrolled high LDL-cholesterol in 2007–2010, LDL-cholesterol was, on average, 32.0 (standard error = 1.1) mg/dL above goal. Additionally, 42.7% of participants with uncontrolled high LDL-cholesterol had an LDL-cholesterol ≥ 30 mg/dL above their goal (32.9%, 39.5%, 54.4% and 48.4% for those with 0–1 risk factors, 2+ risk factors, CHD or risk equivalents, and CHD at very high risk, respectively).
DISCUSSION
The current study has several important findings. First, high LDL-cholesterol is common, its prevalence has remained stable over the past 12 years and 80.8 million US adults had high LDL-cholesterol in 2007–2010. Second, the rapid increase in awareness of high LDL-cholesterol between 1999–2000 and 2003–2004 has not continued and only 61.5% of US adults with high LDL-cholesterol were aware of having this condition in 2009– 2010. Third, both among all individuals with high LDL-cholesterol and among those treated with pharmacological lipid-lowering therapy, the prevalence of controlled LDL-cholesterol did not increase between 2005–2006 and 2009–2010. Furthermore, in 2009–2010, only 27.4% of US adults with high LDL-cholesterol had controlled their LDL-cholesterol to guideline recommended levels and almost half of people with uncontrolled LDL-cholesterol were 30 mg/dL or more above their guideline recommended goal. Finally, US adults with CHD at very high risk for subsequent events were substantially less likely than their lower risk counterparts to achieve their LDL-cholesterol goal.
Prior analyses of earlier NHANES have found marked increases in the awareness, treatment and control of high LDL-cholesterol among US adults. Hyre and colleagues reported awareness of high LDL-cholesterol increased by more than 50% between 1988– 1994 and 1999–2004 and lipid-lowering therapy usage increased almost four-fold (from 11.7% to 40.8%) over this time period.1 Additionally, Mann and colleagues reported an increase in statin use from 19.6% to 35.9% among US adults with high LDL-cholesterol between 1999–2000 and 2003–2004.2 These prior studies overlap with the publication of the ATP-III guidelines in 2001. Using data from the National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey, Moser found an increased use of statins from 2002 through 2004 among individuals with diabetes.9While an update to ATP-III was published in 2004, our results indicate that control of high LDL-cholesterol has not continued to increase through 2009–2010.
A recent analysis of NHANES data from 1988 through 2010 found a marked decline in mean LDL-cholesterol levels among US adults.4 In this study, the mean LDL-cholesterol among US adults ≥ 20 years of age was 129, 123 and 116 mg/dL in 1988–1994, 1999– 2002, and 2007–2010, respectively. The authors hypothesized that the improvements in LDL-cholesterol may be due to decreased consumption of trans-fatty acids, other healthy lifestyle changes, or increased lipid-lowering medication use. They also reported a greater than a 4-fold increase in lipid-lowering medication use between 1988–1994 and 2007–2010. The current study extends this prior NHANES analysis to report the awareness, treatment and control of LDL-cholesterol among US adults and, despite improvements in the average LDL-cholesterol level among US adults, highlights the continued efforts needed to improve LDL-cholesterol control among individuals diagnosed with high cholesterol, especially among those at highest risk for future CHD events.
A limitation of our study is the reliance ona single measurement of LDL-cholesterol. Variation in LDL-cholesterol measurement may have resulted in the misclassification of some participants. However,this threat may be minimal as the mean LDL-cholesterol was 32.0 mg/dL above goal for individuals with uncontrolled LDL-cholesterol. The presence of CHD was based on self-report and medical record review was not feasible. The exact criteria for defining CHD at very high risk was not available and had to modified for our analysis. Despite these limitations, the current study has several strengths. These include its complex sampling design which permitted us to generate nationally representative estimates, the large sample size of participants who fasted overnight prior to their study visit, and broad data collection which allowed us to calculate participants’ CHD risk.
Supplementary Material
Acknowledgments
This research, including design and conduct of the study, analysis and interpretation of the data, and preparation of the manuscript, was supported by Amgen, Inc.The academic authors conducted all analyses and maintained the rights to publish this manuscript. Dr. Muntner has served as a consultant to Amgen Inc. Dr. Woolley is employed by Amgen, Inc.Dr. Rosenson serves a consultant to Amgen, Inc, and the Mount Sinai School of Medicine receives research support from Amgen, Inc.
This work was supported by a grant from Amgen, Inc. Thousand Oaks, CA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors have no other disclosures.
References
- 1.Hyre AD, Muntner P, Menke A, Raggi P, He J. Trends in ATP-III-defined high blood cholesterol prevalence, awareness, treatment and control among U.S. adults. Ann Epidemiol. 2007;17:548–555. doi: 10.1016/j.annepidem.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 2.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42:1208–1215. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 3.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 4.Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, –2010. JAMA. 2012;308:1545–1554. doi: 10.1001/jama.2012.13260. [DOI] [PubMed] [Google Scholar]
- 5. [Accessed November 14, 2007];National Center for Health Statistics: National Health and Nutrition Examination Survey Laboratory Procedures Manual. 2007 http://wwwcdcgov/nchs/data/nhanes/lab1-6pdf.
- 6.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of lowdensity lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 7.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC, Jr International Diabetes Federation Task Force on E, Prevention, Hational Heart L, Blood I, American Heart A, World Heart F, International Atherosclerosis S, International Association for the Study of O. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 8.Coresh J, Astor BC, McQuillan G, Kusek J, Greene T, Van Lente F, Levey AS. Calibration and random variation of the serum creatinine assay as critical elements of using equations to estimate glomerular filtration rate. Am J Kidney Dis. 2002;39:920–929. doi: 10.1053/ajkd.2002.32765. [DOI] [PubMed] [Google Scholar]
- 9.Moser A, Segars LW. Assessment of antihyperlipidemic therapy in US patients with coronary heart disease. J Am Osteopathic Assoc. 2010;110:331–339. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.