Medical conditions that run in a family are inherited or genetic—caused by changes in genes that are passed from generation to generation. Many different types of heart disease can be inherited. Some conditions, like high blood pressure or coronary artery disease (blockages in the arteries that supply the heart with blood), run in families but probably result from a number of different genetic changes that individually have a subtle effect, but work collectively in a complex manner to cause disease. In these situations, genetic testing is not yet available. There are other less common inherited heart diseases that are caused by just one or very few genetic changes that have a very strong effect in causing disease. In this Cardiology Patient Page, we describe our approach to this type of inherited heart conditions and genetic testing. Examples include conditions that affect the heart muscle, called inherited cardiomyopathies, such as hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), and arrhythmogenic right ventricular cardiomyopathy (ARVC). There are also inherited heart conditions that affect the electrical system of the heart, causing abnormal heart rhythms called arrhythmias. Examples of inherited arrhythmias include Long QT syndrome and Brugada syndrome. Some of these conditions may require changes in lifestyle or medical therapy. All inherited heart diseases require special attention not only for the individual patient, but also for their family to see if other relatives are in need of medical care.
How does inheritance work?
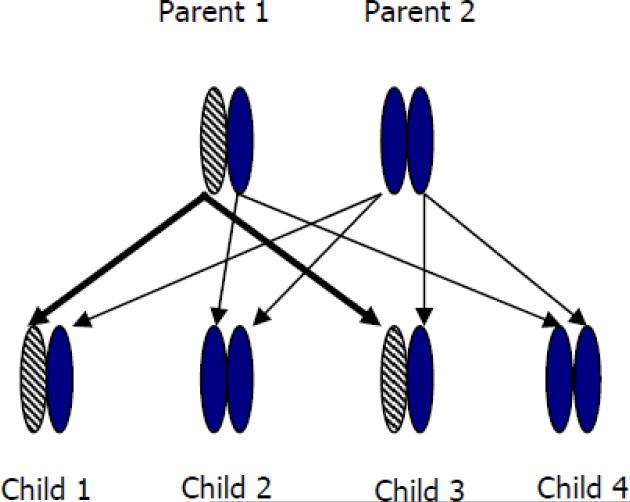
Genes are the basic units of inheritance and are made up of chemicals called DNA. Genes provide instructions for cells to make proteins that carry out all body functions and form our physical characteristics. We each have more than 20,000 genes, and each gene is present in two copies. One copy is inherited from your mother and one copy is inherited from your father. Genetic conditions are caused by a change (or mutation) in one or more genes passed from generation to generation. Most genetic heart conditions are inherited in an autosomal dominant pattern. Autosomal means that both men and women are equally affected. Dominant means that although there are two copies of each gene, a mutation in just one copy is enough to cause disease. Therefore, a person with an autosomal dominant condition has one normal copy of the gene and one copy with a mutation. The chance of passing the abnormal copy of the gene to a child is 1 out of 2, or 50%. By the same token, each child has a 50% chance of inheriting the normal copy of the gene and have no risk for developing the condition (Figure 1). On average, half of the members of a family with an autosomal dominant heart condition will develop the disease.
Figure 1. Autosomal dominant inheritance.
Parent 1 has an autosomal dominant condition. The patterned shape represents the copy of the gene with the disease-causing mutation. There is a 50% chance that each child will inherit this copy of the gene. In this example, Child 1 and Child 3 both inherited the copy with the mutation from Parent 1 and are therefore at risk for developing the condition.
Does my family have an inherited heart disease?
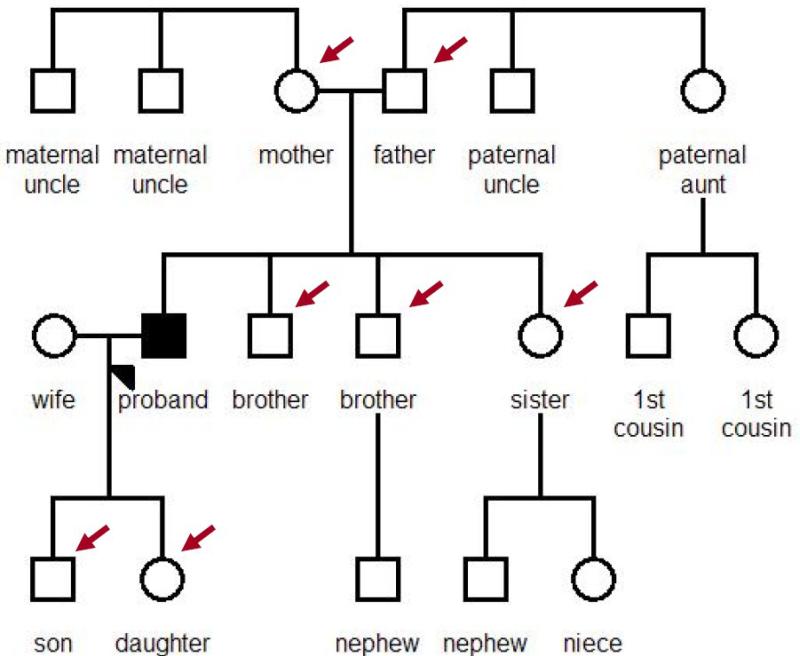
The first step in trying to determine if heart disease runs in your family is to draw a pedigree. A pedigree (Figure 2) is a family tree that shows who has and who doesn’t have the condition of interest. It is drawn to organize information about the medical history of family members, illustrate who is affected, identify the pattern of inheritance, and identify who is at risk for disease. In drawing the pedigree, it is important to know whether your relatives have been diagnosed with any heart problems, died suddenly or unexpectedly, or have other major medical problems. Sometimes people may not be aware that they have a heart condition because their findings are so mild, they haven’t seen a doctor recently, or they haven’t had the appropriate tests performed. Knowing as many details as possible is important because sudden death can be mistakenly labeled as heart attacks, drowning, or car accidents. The sudden death of a previously healthy young person should be closely examined.
Figure 2. Pedigree.
A pedigree is a family tree. Squares indicate males and circles indicate females. Darkened symbols indicate people who have the family's disease. The arrowhead indicates the proband-- the person who is being evaluated for an inherited heart disease. His family members are also at risk to develop the condition. The arrows point to his first-degree family members (children, siblings, parents) who need periodic clinical evaluation.
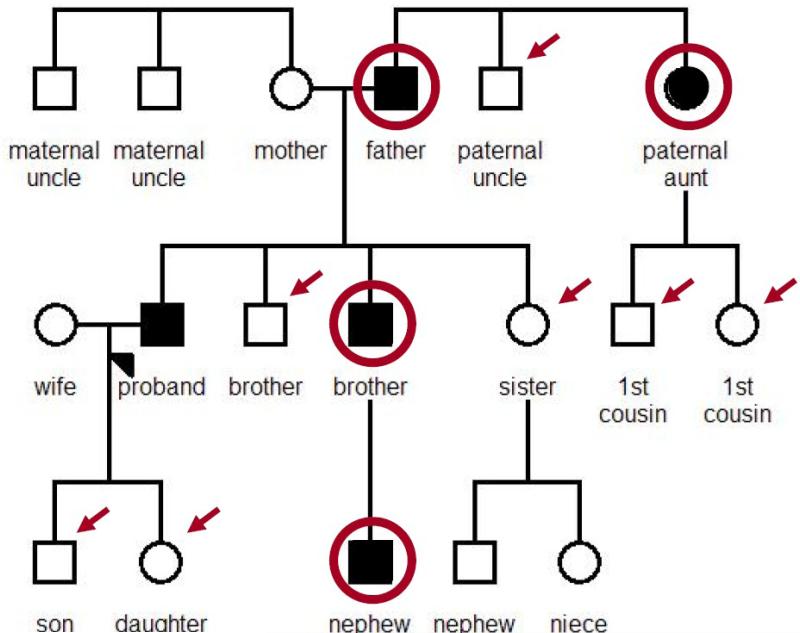
Because immediate, or first-degree, family members of a person with an autosomal dominant condition each have a 50% risk of inheriting the gene mutation that causes the family's condition, they should be evaluated by an experienced cardiologist to see if they are affected. If a person is diagnosed with the condition, the first-degree relatives of that person should then be evaluated—a process called cascade screening (Figure 3).
Figure 3. Cascade Family Screening.
The circled shapes show family members from Figure 2 whose symbols are now darkened because they were diagnosed with heart disease in the process of family screening. The arrows point to the first-degree family members of all affected individuals. These immediate family members need to be examined periodically since they are at risk for developing the family's heart condition.
What is genetic testing and what can it tell me?
Genetic testing is the process of taking a sample of a person's DNA to look for changes that could cause inherited heart disease. Important changes in genes are called pathogenic mutations. The term “pathogenic” means disease-causing.
Genetic testing can be used to:
Clarify the diagnosis in a person who has, or is suspected to have, inherited heart disease
Identify the cause of heart disease in a family
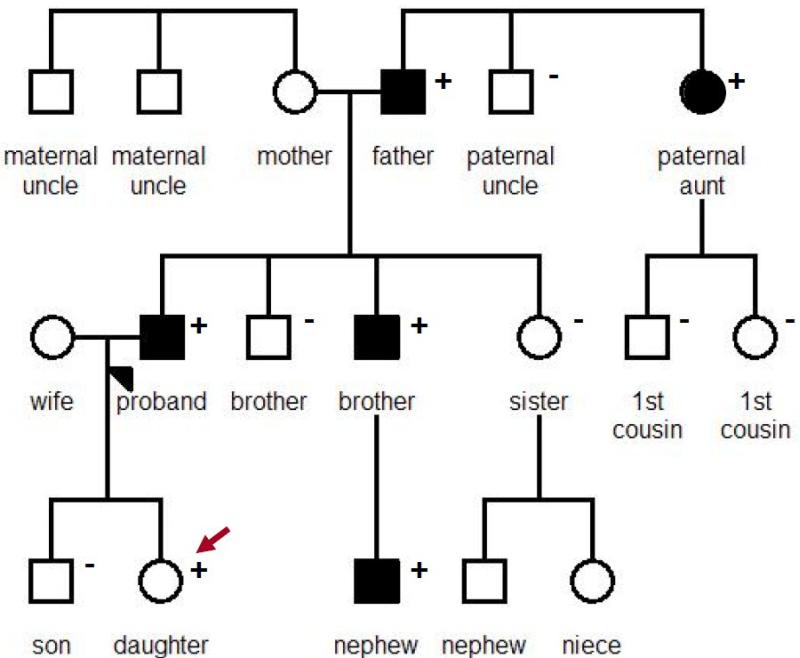
Predict which family members are at-risk to develop the family's heart condition (see section on Predictive Genetic Testing and figure 4, below)
Provide options for family planning, including preimplantation genetic diagnosis to try to avoid passing a disease-causing mutation to offspring
Figure 4. Predictive genetic testing.
This figure shows the genetic testing results for this family. The proband (arrowhead) was found to have a disease-causing mutation and many of his at-risk family members underwent predictive genetic testing. Plus signs show family members who tested positive for the pathogenic mutation and minus signs show family members who tested negative for the pathogenic mutation. In this family the mutation segregates as expected with disease, meaning that all individuals with a diagnosis of heart disease also have the mutation. The proband's daughter is an example of someone who has inherited the risk to develop heart disease but currently appears healthy and cannot yet be diagnosed with the condition.
Genetic testing for inherited heart disease can identify the cause of a family's heart disease. Testing can also help determine which specific relatives are at risk for developing it, beyond the general assumption that 50% of the family will develop the condition. It is important to recognize that results cannot predict when the condition will develop or how severe it may be. Inheriting the mutation is not a guarantee that disease will develop, although it will cause the disease in many people. Furthermore, there are typically no treatments that can prevent or change the course of disease, however we hope that such preventive treatments will be developed in the future.
Predictive genetic testing is a streamlined type of testing that can be performed once comprehensive (diagnostic) genetic testing identifies a disease-causing mutation in a relative who has the family's heart condition. Predictive genetic testing involves determining whether the family's gene mutation is present or absent in a family member who is at risk for developing the family's heart disease, but currently appears healthy. If the mutation is present, that person is at risk for developing the family's heart condition and should have regular examinations to look for evidence that disease is developing. If the mutation is absent, that individual is unlikely to develop disease but should be thoroughly evaluated if there is any change in how they feel or if their doctors have any concerns.
How does the genetic testing process work?
Genetic testing should be thought of as a family test rather than a test on an isolated individual. Although the testing process may start by taking a blood sample from one person, the results are best understood when the family is evaluated as a unit. This way, both the genetic test results and medical test results are available, providing the most accurate picture of how the disease and the gene mutations may act in that particular family. Such comprehensive information not only helps to identify specific patterns in the family, but also plays an important role in confirming that the gene mutation is truly an accurate marker of the family's heart disease.
Carefully reviewing the family history helps to identify the best person in the family to be tested first to try to initially find the gene mutation that causes the family's heart disease. To increase the chances of getting useful results, this person should be someone who has a clear diagnosis of the inherited heart condition; ideally the most severely affected family member. A sample of this person's blood will be sent to a genetic testing laboratory to undergo genetic testing for his/her condition.
Genetic testing usually examines a panel of multiple genes known to cause the specific inherited condition of interest, and other conditions that have a similar appearance. The DNA sequence in the patient's DNA is compared to the normal reference sequence. A single change in one gene is sufficient to cause disease. In some cases, two or more mutations may be responsible for causing disease in the family.
If possible, genetic testing should be performed in conjunction with a healthcare team that has the experience and resources to study the family and to provide important counseling before and after testing. This counseling helps individuals make an informed decision about whether pursuing genetic testing is right for them. It also helps to ensure that the individual and their family are appropriately cared for and understand what the results mean.
It can take a few weeks to a few months to get results depending on the genetic test ordered. There are three potential test results for the initial person being tested: positive, negative, and inconclusive. Only positive testing results are helpful. The likelihood of getting a positive result varies by the condition and the exact test performed.
A positive result means the laboratory is reasonably confident it identified a gene mutation that can cause the family's heart disease. A positive result allows at-risk family members to do predictive genetic testing. Family members who carry the same gene mutation are at risk to develop the heart condition and should be followed by a cardiologist. These individuals are also at risk to pass the mutation on to their children and these children should be examined. Relatives who do not have the family's disease-causing gene mutation are very unlikely to develop the family's heart condition and cannot pass the family's mutation on to their children. However, because our understanding of the genetics of heart disease is not perfect, it is important to carefully examine these individuals if they develop any symptoms or other changes.
A negative result means that the laboratory was unable to find a mutation capable of causing disease in any of the genes they evaluated. This result is considered unhelpful because it is still possible that there is genetic cause for a person's heart disease that was simply not detected by the technology used, or is present in a gene that was not evaluated. In this case it is not possible to offer predictive genetic testing to at-risk family members to determine their risk of developing heart disease. Therefore, all first degree family members should continue to undergo the screening recommended for the family's heart condition. Genetic testing may be reconsidered in the future if there is new information available about the potential genetic causes of the condition.
Lastly, it is also possible that the lab will find a change in a gene, but be uncertain about whether the change is capable of causing a heart condition, whether the change can modify disease severity, or whether the DNA change they found simply reflects harmless DNA variation that occurs in the general population. This type of inconclusive result is often referred to as a variant of unknown significance, or VUS. A VUS does not provide any additional information for the family. Testing other affected family members may help to better understand the significance of a VUS. If it is present in all other affected family members, as would be expected if it is responsible for causing the family's heart condition, that finding provides additional support that the VUS causes disease. This is particularly the case if there are many (more than 5) affected relatives. On the other hand, if the VUS is absent from even a single affected relative, that suggests it is not the cause of the family's heart disease. Testing unaffected family members to see if they have the VUS is generally not recommended because it is unlikely to provide helpful information about whether the VUS can cause heart disease. As with a negative result, there is still the possibility of an inherited heart condition in the family and the recommended screening of at-risk family members should be followed.
Over time, new information may become available about whether a particular gene change can cause heart disease. In some cases this information may cause the laboratory to revise the results previously reported for that gene change. For example, a DNA change previously thought to cause disease may ultimately turn out to be harmless if it is found in enough healthy people. On the other hand, a DNA change that was previously of unknown significance could later be determined to be disease-causing if it is found to track with, or segregate, with enough patients with heart disease. Therefore, it is important to remain in contact with the health care provider who ordered your genetic testing in the event that new information comes to light that changes the recommendations made to you and your family. Important points about genetic testing are summarized in the Table.
Table.
| Important things to remember about genetic testing: |
| • Genetic testing can be a helpful tool when approached and interpreted properly. |
| • Genetic testing should be considered a family test rather than a test that is relevant or accurately interpreted on only a single individual. |
| • It is not always possible to find a disease-causing gene mutation. Heart disease may still be inherited even if the genetic test result is negative. |
| • Not all changes in the DNA are harmful or capable of causing disease |
| • It may take time to determine whether a DNA change is harmful or not. Reviewing both medical and genetic information from family members can provide important insights, particularly if relatives that have the heart disease can be evaluated. |
| • Our understanding about gene mutations is likely to change over time and test results may be updated. |
| • Each individual should make a personal decision about whether to pursue genetic testing after carefully considering how they feel about the potential value and the limitations of the information. |
| • Understanding your family history is important. Talk to your relatives to try to develop a good knowledge of the family's medical history. |
What are potential consequences of genetic testing that I should be aware of?
Determining that you, or a close relative, have or are at risk for inherited disease can cause a wide range of emotional reactions including anger, guilt, grief, sadness, fear and anxiety. Some people may feel a sense of relief from removing the uncertainty about whether they or their children inherited the mutation. Others may feel disappointment or worry to learn that they or their children have inherited the mutation and are definitely at risk for developing heart disease, particularly since there are currently no treatments to change how, when, and if disease may develop. Learning that you do not carry the family's mutation will often be a relief, but may also cause feelings of guilt. It is important to consider how you might react to both positive and negative results before pursuing genetic testing. Also, since genetic testing often involves multiple members of a family, there can be an impact on family relationships. Some family members may not want to know or may not want to share their genetic status. Having periodic examinations by an experienced cardiologist is an alternative approach for family members who do not wish to pursue genetic testing.
At this time genetic testing is still quite expensive, particularly for the comprehensive testing obtained on the first family member to be tested (typically ranging from $1000-$5000). Predictive genetic testing currently costs around $400-$900. Insurance coverage for genetic testing is variable. Individuals concerned about the financial aspects of genetic testing should check with their insurance company about coverage before testing and should be familiar with the billing policies of the genetic testing laboratory.
For some, there is concern about how genetic test results may potentially be used against them by insurance companies. The Genetic Information Nondiscrimination Act (GINA) was signed into law in 2008 and provides federal legal protection from the misuse of predictive genetic information in the areas of health insurance and employment. GINA does not cover the areas of life insurance and long-term care/disability insurance. However, some states do have restrictions about how genetic information can be used in these areas. Individuals may also consider securing life insurance for themselves or their children prior to genetic testing.
Resources
GeneReviews: http://www.ncbi.nlm.nih.gov/sites/GeneTests/
National Society of Genetic Counselors: www.nsgc.org
Genetic Alliance: www.geneticalliance.org
National Human Genome Research Institute: www.genome.gov
Genetics Home Reference: http://ghr.nlm.nih.gov/
Footnotes
Disclosures: Both authors receive funding from NIH to pursue research in cardiovascular genetics. There was no specific funding for this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.