Abstract
Objective
The objective of this study was to evaluate the feasibility, acceptability, and accuracy of having emergency department (ED) patients perform a rapid, point-of-care (POC) self-test for HIV before routine HIV testing.
Methods
Patients aged 18 to 65 years were recruited to perform a rapid POC HIV oral fluid at The Johns Hopkins ED in conjunction with the standard-of-care HIV POC test. Acceptability and ease of use were assessed by a questionnaire.
Results
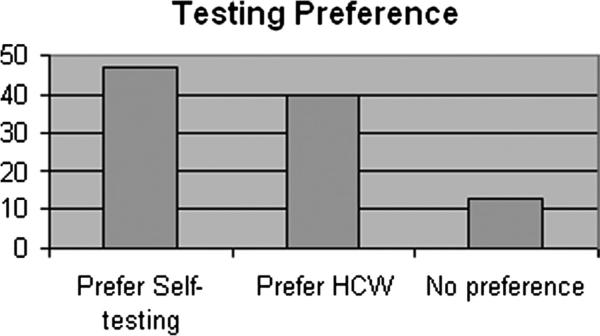
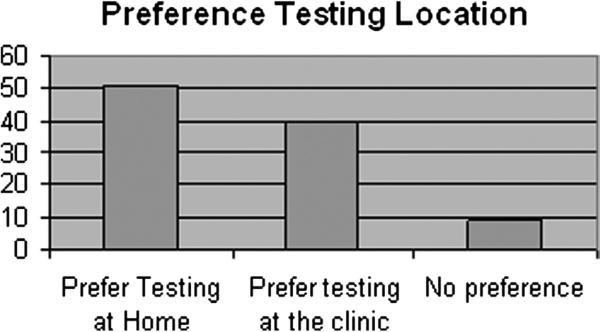
A total of 259 patients were approached for testing, and 249 (96.1%) consented to perform a self POC HIV test. Of patients performing a self-test, 100% had concordant results with those obtained by the health care worker. Four females (1.6%) were newly identified as HIV positive. Median participant age was 41 years, and 58% of patients were female; 83% were African American, and 16% were white. Overall, greater than 90% of patients reported trust of the test results, ease of testing, and willingness to test again. Approximately 35% of patients indicated they would pay up to a maximum price of $30 for testing. Overall, 46.9% of patients preferred self-testing, and 39.5% preferred health care professional testing. Regarding preferred location for testing, 51.0% preferred home self-testing, 39.5% preferred clinic/ED self-testing (P > 0.05), and 9.5% had no preference.
Conclusions
A significant proportion of patients offered POC testing in the ED agreed to perform a self–HIV test. Patients’ results were concordant with those obtained by the health care worker; 1.6% were HIV positive. The majority of participants believed the veracity of their results. A greater number of patients preferred self-testing.
Keywords: HIV, point-of-care test, oral fluid HIV test, self-testing, emergency department
The Centers for Disease Control and Prevention (CDC) calculates that an estimated 1.2 million individuals 13 years or older were living with HIV infection in the United States at the end of 2008, of which 20% were undiagnosed.1,2 In 2009, there were an estimated 48,000 new HIV infections.1 African American men and women are disproportionately affected and are estimated to have an incidence rate 7.7 times as high as the incidence rate among whites. Of the approximately 112,000 female adults and adolescents living with HIV/AIDS, 66% were exposed through heterosexual contact.1
The 2006 CDC guidelines, which advocate routine HIV testing in all health care settings, provide explicit recognition of the importance of emergency department (ED) as one of the most common sites of missed opportunity for identification of patients with unrecognized HIV.3 Two large survey studies have attempted to study the implementation of these guidelines4,5 but have fallen short. Developing approaches for breaking this barrier are critical but have failed, to date, in part because of lack of innovative approaches for streamlining testing that are customized to busy and ED care settings.
We hypothesized that allowing patients to perform their own HIV test could provide a practical mechanism to streamline the HIV testing process in the ED and thus could contribute to increasing rates of HIV testing uptake in this setting. As a first step toward testing this hypothesis, we previously conducted a study in which patients were offered the option to self-test after having undergone routine HIV testing by a health care worker (HCW) and found that HIV self-testing was both feasible to implement and highly acceptable to patients in the ED.6 We aimed to determine whether having patients perform their own HIV test in the ED before being tested by an HCW would be feasible and acceptable and yield accurate test results.
METHODS
Setting
The Johns Hopkins Hospital is an inner-city ED, with 60,000 visits per year, population of which is socioeconomically disadvantaged, composed of more than 75% African Americans, 15% current or previous injection-drug users, and an ~11% to 12% HIV seroprevalence,7 with a rate of newly recognized HIV infection of ~0.5% to 1%.8
Study Design and Participants
From July 2010 to March 2011, all patients aged 18 to 64 years who met the inclusion criteria of not having a previous HIV diagnosis or not having been tested for HIV in the previous 6 months where eligible for the self-testing study. The institutional review board of Johns Hopkins University approved the study, and written informed consent was obtained. Consented patients were asked to perform their own HIV point-of-care (POC) test using the oral fluid OraQuick Advance HIV1/2 test (OraSure, Bethlehem, Pa). Patients were given large plasticized instruction templates to use as visual aids for the sample collection and the testing procedure. Patients were asked to collect the oral fluid, add the swab to the test vial, and wait 20 minutes to read and interpret the test result without assistance from the HCW. The HCW then performed the same standard-of-care POC test by collecting the sample and performing the assay.
Methods of Measurement, Test Performance, and Data Collection
The primary outcome was patient's acceptability of the HIV self-testing process as assessed by a questionnaire administered by an HCW. Questions were asked in a Likert scale format and included confidence of the patients in the sample collection process and results they reported, patients’ overall satisfaction with performing their own test, and patients’ willingness to pay based on the possibility the test might be available for purchase over-the-counter in the future. Secondary outcomes were agreement of the self-test result compared with the HCW-performed, standard-of-care oral fluid test result and feasibility as determined by HCW direct observation and recording of any difficulties that were encountered by the patients during self-testing (eg, opening the test package).
Primary Data Analysis
Standard HIV results were immediately (within 20 minutes) made available to patients after the performance and interpretation of their self-test. Questionnaire results and observational information were recorded in an SPSS database. Data analysis was performed by SAS version 9.1 (SAS Institute Inc, Cary, NC).
RESULTS
A total of 259 patients were approached for testing, and 249 (96.1%) consented to perform a self–POC HIV test. Of patients performing a self-test, 100% had concordant results with those obtained by the health care professional. The median age was 41 years, and 58% of patients were female; 83% were African American, and 16% were white. Six patients did not complete questionnaires, and 95.1% of patients believed the rapid POC self-test was “definitely correct,” 4.5% believed the results were “probably correct,” and 91.7% of patients “trusted the results” of the self-test “very much” (Table 1). Interestingly, 98.4% reported that “overall” performing their own test was “easy,” and 1.3% indicated that performing their own test was “somewhat easy.” When asked, “Do you think you would recommend to a friend that he/she test himself/herself for HIV?” 96.2% reported they would “definitely recommend,” and 1.5% would “probably” recommend self-testing. Of patients, most would “definitely” (95.0%) or “probably” (2.9%) test themselves at home if the rapid HIV test were available over-the-counter for purchase. Approximately 35% of patients stated they were willing to pay a maximum of only $10 for the test, whereas 35.4% would pay up to a maximum price of $30 (Table 1). Almost 47% of patients preferred self-testing, and 39.5% preferred health care professional testing (Table 2, Fig. 1). Regarding preferred location for testing, 51% preferred home self-testing, and 39.5% preferred clinic/ED testing (P > 0.05) (Table 2, Fig. 2). Four female patients (1.6% of total tested), who were previously not known to be HIV positive, tested positive for HIV, and their results agreed with the tests performed by the HCW.
TABLE 1.
Acceptability and Feasibility of Self-testing Among Participants Recruited at The Johns Hopkins Emergency Room Between July 2010 to March 2011 (n = 243*)
| Characteristic | n (%) |
|---|---|
| Do you believe that the rapid HIV test result was correct for the sample that you collected? | |
| Definitely correct | 231 (95.1) |
| Probably correct | 11 (4.5) |
| Not correct | 1 (0.4) |
| How much do you trust the result of the rapid HIV test that you collected? | |
| Trust very much | 223 (91.7) |
| Trust somewhat | 18 (7.4) |
| Not trust at all | 2 (0.8) |
| How easy was it for you to follow the instruction placard? | |
| Easy to follow | 235 (96.7) |
| Somewhat easy to follow | 6 (2.5) |
| Not easy to follow | 3 (1.2) |
| How easy was it for you to open the test kit? | |
| East to open | 210 (86.4) |
| Somewhat easy to open | 29 (9.5) |
| Not easy to open | 4 (1.6) |
| How easy was it for you to collect the specimen correctly? | |
| Easy to collect | 242 (99.6) |
| Somewhat easy to collect | 1 (0.4) |
| How easy was it for you to read the result and tell the result? | |
| Easy to read and tell | 225 (92.6) |
| Somewhat easy | 16 (6.7) |
| Not easy | 2 (0.8) |
| Overall, how easy was it for you to perform the test? | |
| Easy to perform | 239 (98.4) |
| Somewhat easy to perform | 3 (1.3) |
| Not easy to perform | 1 (0.4) |
| Do you think you would recommend to a friend that he/she test himself/herself for HIV? | |
| Definitely recommend | 236 (96.2) |
| Probably recommend | 4 (1.5) |
| Would not recommend | 3 (2.3) |
| Would you test yourself at home for HIV if the rapid HIV test were available over-the-counter? | |
| Definitely test myself at home | 231 (95.0) |
| Probably test myself at home | 7 (2.9) |
| Would not test myself at home | 5 (2.1) |
| What is the maximum price you would pay to purchase a rapid HIV test over-the-counter, if available? | |
| $10 | 84 (34.6) |
| $20 | 45 (18.5) |
| $25 | 28 (11.5) |
| $30 | 86 (35.4) |
There were 243 patients who completed the questionnaire.
TABLE 2.
Preference of Self-Testing Versus Standard-of-Care Testing Among Persons Who Performed a Self-test for HIV
| n (%) | |
|---|---|
| Based on your experience today, would you prefer to test yourself for HIV, or would you prefer a health care professional to test you? | |
| Prefer self-testing | 114 (46.9) |
| Prefer health care professional | 96 (39.5) |
| No preference | 33 (13.6) |
| Based on your experience today, would you prefer to test yourself for HIV at home if available or to have a test when you come to clinics or ED? | |
| Prefer testing at home | 124 (51.0) |
| Prefer testing in clinic/ED | 96 (39.5) |
| No preference | 23 (9.5) |
FIGURE 1.
Preference of 249 persons for self-testing versus testing by an HCW.
FIGURE 2.
Preference of 249 persons for location of HIV self-testing.
DISCUSSION
Given that approximately 20% of HIV-positive persons in the United States do not currently know their status, and current data support early detection and diagnosis as a means to expedite linkage to care, treatment, and behavioral modification of risk behaviors, new and innovative methods for testing individuals for HIV are needed. In this study, we assessed the acceptability and feasibility of HIV self-testing in the ED setting, and our findings are consistent with those reported from a previous self-testing pilot study conducted in our ED.6 We find that 96% of patients who consent for HIV testing in the ED setting agree to perform self-testing before their standard-of-care HIV test and that the majority of patients (92%–96%) reported trusting the test, finding it easy to perform and interpret. The testing process did not affect the overall uptake rates of standard-of- care testing (data not shown), which currently occurs in the ED. Taken together, these data suggest high acceptability and feasibility and accuracy of HIV self-testing in the ED setting and offer a potential method to get more persons tested, with less ED staff time required.
Rapid HIV testing plays a key role in the new CDC strategy since 2006 and averts several of the previously reported challenges associated with HIV testing in busy episodic health care settings.9,10 Given that patients who opt to undergo self-testing for HIV may be motivated to improve their health, these patients might be more willing to actively seek treatment and therefore have higher rate of linkage to care as well as retention to care.
One of the potential barriers to uptake of self-testing may be cost. In our study, about 35% of patients stated they were willing to pay a maximum of $10 for a test, and approximately 18% of patients were willing to pay as much as $20, whereas only 35% were willing to pay $30. The currently advertised charge for the OraSure HIV test is $35.00 (http://www.oraquickhivtestkit.com/order.php). Accordingly, results from this study demonstrate that patients’ willingness to pay may fall short of the eventual commercial costs should the HIV self-test ever become available over-the-counter. It is important to note, however, that this study was conducted in an economically disadvantaged area and may not reflect the general population's willingness to pay.
Interestingly, even though the majority of patients trusted the results and would be willing to perform self-testing at home, 39.5% still indicated that they would prefer to have self-testing done in the clinic/ED setting (Fig. 2), and 40% of patients indicated that they would prefer to be tested by a health care professional (Fig. 1), rather than perform their own test (51%) (P > 0.05). Some of the reasons for these preferences may be related to access to counseling should the patient have a positive result and that these patients indicated that they would be “more comfortable” if testing were done by a health care professional. However, patients may prefer the confidentiality offered with the ability to self-perform and read their own results. Self-sampling at home has been reported to be preferred by women undergoing repeat follow-up screening for Chlamydia and gonorrhea.11
One limitation of our study is that these ED findings regarding self-testing feasibility and preference may not be generalizable to other settings. Our ED population is typically composed of minority populations that are socioeconomically disadvantaged and may be more likely to consent to HIV testing (and self-testing) given the higher prevalence in our area and the population's recognition and overall acceptance of the importance of HIV testing. Another limitation of our study is related to reproducibility of interpreting results and test concordance because the vast majority of test results (and thus patient experience with self-interpretation of test results) came from those who were HIV negative. A final limitation is that these findings, which were derived in an artificial study setting where patients were still tested by an HCW after their self-test was performed, may not hold true when patients perform their own self-test without a follow-up HCW-performed HIV test. Accordingly, these results may also not directly translate to willingness to perform the test at home in a setting without access to HCWs for counseling and confirmatory testing.
In conclusion, our study demonstrated that more than 95% of patients in the ED agreed to perform a self–HIV test in the ED. The patients’ results were concordant with those obtained by HCWs in all 249 patients. Four female patients received their first-time diagnosis of HIV. The majority of participants believed and trusted their results and would recommend POC testing to a friend. A greater number of patients preferred self-testing, and there was no significant difference (P > 0.05) regarding venue for self-testing. Thus, self-testing for HIVappears to be feasible in the ED setting. Further studies are required to determine whether full integration of self-testing in the ED will improve overall rates of testing uptake and completion in the ED, relative to traditional HCW-only approaches for providing testing in this setting.
Acknowledgments
This work was supported by the National Institutes of Health (NIH)/National Institutes of Biomedical Imaging and Biotechnology grant U54 EB007958 and by NIH HPTN U-01 AI068613 and an unrestricted grant from Gilead Sciences, HIV Focus Program.
Footnotes
The authors decalre no conflict of interest.
REFERENCES
- 1.Centers for Disease Control and Prevention . HIV Surveillance Report, 2008. Vol. 20. US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2010. http://www.cdc.gov/hiv/surveillance/resources/reports/2008report/index.htm. Accessed March 10, 2012. [Google Scholar]
- 2.Prejean J, Song R, Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Branson B, Handsfield H, Lampe H, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Morb Mortal Wkly Rep. 2006;55(RR-14) [PubMed] [Google Scholar]
- 4.Ehrenkranz PD, Ahn CJ, Metlay JP, et al. Availability of rapid human immunodeficiency virus testing in academic emergency departments. Acad Emerg Med. 2008;15(2):144–150. doi: 10.1111/j.1553-2712.2008.00028.x. [DOI] [PubMed] [Google Scholar]
- 5.Rothman RE, Hsieh Y-H, Harvey L, et al. 2009 US emergency department HIV testing practices. Ann Emerg Med. 2011;58(1 suppl 1):S3–S9. doi: 10.1016/j.annemergmed.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 6.Gaydos CA, Hsieh YH, Harvey L, et al. Will patients “opt-in” to perform their own rapid HIV test in the emergency department? Ann Emerg Med. 2011;58(suppl 1):S74–S78. doi: 10.1016/j.annemergmed.2011.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clark SJ, Kelen GD, Henrard DR, et al. Unsuspected primary human immunodeficiency virus type 1 infection in seronegative emergency department patients. J Infect Dis. 1994;170(1):194–197. doi: 10.1093/infdis/170.1.194. [DOI] [PubMed] [Google Scholar]
- 8.Laeyendecker O, Rothman RE, Henson C, et al. The effect of viral suppression on cross-sectional incidence testing in The Johns Hopkins Hospital Emergency Department. J Acquir Immune Defic Syndr. 2008;48:211–215. doi: 10.1097/QAI.0b013e3181743980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kecojevic A, Lindsell CJ, Lyons MS, et al. Public health and clinical impact of increasing emergency department-based HIV testing: perspectives from the 2007 conference of the National Emergency Department HIV Testing Consortium. Ann Emerg Med. 2011;58(1 suppl 1):S151–S159. doi: 10.1016/j.annemergmed.2011.03.040. [DOI] [PubMed] [Google Scholar]
- 10.Burke R, Sepkowitz KA, Bernstein K, et al. Why don't physicians test for HIV? A review of the US literature. AIDS. 2007;21(12):1617–1624. doi: 10.1097/QAD.0b013e32823f91ff. [DOI] [PubMed] [Google Scholar]
- 11.Graseck AS, Secura GM, Allsworth JE, et al. Home compared with clinic-based screening for sexually transmitted infections: a randomized controlled trial. Obstet Gynecol. 2010;116(6):1311–1318. doi: 10.1097/AOG.0b013e3181fae60d. [DOI] [PMC free article] [PubMed] [Google Scholar]