Abstract
Purpose
Diabetes and periodontal disease are two common diseases with high prevalence rates. Recent evidence has shown a bidirectional relationship between diabetes and periodontitis. The aim of this study was to investigate the effects of nonsurgical periodontal therapy on glycemic control in type 2 diabetes mellitus patients.
Methods
Sixty subjects aged 35-45 years with blood sugar controlled by oral hypoglycaemic agents were randomly divided equally among 3 groups: group A (scaling, mouthwash, and brushing), group B (mouthwash and brushing), and group C (brushing only). Glycated haemoglobin (HbA1c), fasting blood sugar (FBS), probing pocket depth (PPD), gingival index (GI), plaque index (PI), and the relevant drug history were recorded at baseline and after 3 months of intervention. Comparison of the mean difference among the variables was performed by parametric and nonparametric tests, which were further evaluated using multiple regression analysis.
Results
The mean differences between the PPD, FBS, HbA1c, GI, and PI in groups A and B were found to be statistically significant (P<0.001). Multiple regression analysis in group A showed that out of all the independent variables, GI and frequency of drug administration independently (b=0.3761 and b=0.598) showed a significantly greater impact on HbA1c (R2=0.832, P<0.05).
Conclusions
Nonsurgical periodontal therapy can effectively decrease HbA1c levels in type 2 diabetes mellitus patients on medication.
Keywords: Glycosylated hemoglobin A, Periodontal debridement, Type II diabetes mellitus
INTRODUCTION
Diabetes mellitus (DM) is a chronic, noncommunicable disease and also one of the major global public health issues. It is defined as a clinical syndrome characterized by hyperglycemia; due to a defect in insulin secretion by pancreatic β cells, a decrease in insulin sensitivity, or a combination of both. The most common form of DM is type 2 diabetes mellitus (DM2), which accounts for 85% of all diabetes patients [1]. DM currently is the twelfth leading cause of death in the world. The prevalence of DM has risen dramatically in recent years [2]. Asia, in particular, has the highest prevalence of diabetes in the world. Countries exhibiting a high rate in growth of the diabetic population include India and China, among many other developing countries [3]. DM2, the most common type of diabetes, is characterized by hyperglycemia, hyperlipidemia, and associated complications. Clinical and epidemiological evidence demonstrates that individuals with diabetes tend to have a higher prevalence of and more severe periodontitis than nondiabetics [4]. Periodontal disease is the most prevalent oral complication in patients with DM2. It is characterized by gingival inflammation, periodontal pocket formation, loss of connective tissue attachment, and alveolar bone resorption, ultimately resulting in tooth loss.
Furthermore, patients with poor control of diabetes experience more periodontitis than well-controlled diabetics [4,5]. Direct and indirect evidence supports the concept that periodontal infection adversely affects glycemic control in people with diabetes. Southerland et al. [6] proposed a common pathogenesis involving an increased inflammatory response for periodontitis and diabetes. Patients with periodontitis have increased serum levels of inflammatory cytokines, while diabetic patients have hyper-inflammatory immune cells that can aggravate production of inflammatory cytokines [7]. This exacerbation can increase insulin resistance, that is, a physiological condition in which cells fail to respond to the normal actions of the hormone insulin and make it more difficult for patients to control their diabetes [7,8].
In a review article by Mealey [8], he cited a number of established mechanisms by which diabetes can influence the periodontium, which include the following: alteration in the host immune-inflammatory response, altered wound healing, accumulation of advanced glycation end products, and elevated proinflammatory cytokines. When oral hygiene is compromised, oral bacteria may form a plaque biofilm that is resistant to chemicals and immune cells [6,7]. Without mechanical debridement, the plaque biofilm matures and causes gingivitis in a few days. The infection then leads to formation of pockets between the teeth and gums, signalling a break-down of the periodontal apparatus and bone. The observation that periodontal therapy appears to reduce periodontal infection and inflammation suggests that periodontal therapy may facilitate metabolic control of diabetes, improving insulin sensitivity by reducing peripheral inflammatory cytokine levels [7]. Therefore, we put forward the hypothesis that if periodontitis is causally related to worsening of parameters of diabetic patients, then periodontal treatment should improve glycemic control.
Therefore, the present study was performed to investigate the effects of nonsurgical periodontal therapy on glycemic control in DM2 patients.
MATERIALS AND METHODS
Based on a pilot study, a sample size of 15 patients in each group was estimated considering (α=0.05 [95% confidence interval] and β=0.2 [80% power]). The mean difference between the glycated hemoglobin (HbA1c) levels of the untreated group and treated group was observed to be 1.08±0.93. On the basis of this difference, to be clinically significant, the necessary sample size was estimated using sample size and power calculations developed by William D. Dupont and licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 United States License. for a 5% type I error and 20% type II error, and it was found to be 15 subjects. Due to the longitudinal nature of the study, anticipating the attrition of some participants, a sample size of 20 patients in each group was recruited. Patients who visited the Diabetic Centre in Moradabad (India) for their routine check-up and investigation were screened for DM2 and periodontitis. The inclusion criteria were as follows: patients with DM2, blood sugar controlled only with oral hypoglycemic agents, mild to moderate periodontitis (pocket depth of 4-5 mm), presence of a minimum of 28 teeth, and no systemic antibiotic administration and no periodontal treatment in last six months. The exclusion criteria were the following: patients with systemic diseases other than DM2, tobacco and alcohol users, and patients suffering from oral disease who needed emergency treatment.
Before starting the study, the examiner was calibrated so as to achieve a minimum kappa value of 0.80. In order to ensure intraexaminer consistency, a randomly selected group of 6 patients was examined and re-examined for the plaque index (PI) score, gingival index (GI) score, and probing pocket depth (PPD) in mm. The scores were assessed for reliability by applying the kappa statistic. The kappa value for intraexaminer reliability ranged from 0.89 to 0.92.
A total of 60 patients aged 35-45 years who fulfilled the eligibility criteria and signed the informed consent were recruited to the study. The study protocol was reviewed and approved by the Institutional Ethics Review Committee, Moradabad. In this study, the examiner and participants were both blinded.
All of the 60 patients were randomly divided into 3 equal groups:
Group A (n=20): patients, who had undergone scaling, were advised to regularly use 0.12% mouthwash (once daily) and brush (twice daily)
Group B (n=20): patients who were advised to regularly use 0.12% chlorhexidine mouthwash (once daily) and brush (twice daily)
Group C (control) (n=20): patients who were advised to brush (twice daily)
The participants were reinstructed on the use of mouth-wash and brushing and regular performance was reinforced every month through telephone calls to ensure compliance. The oral examination was conducted in the dental clinic wing of the Diabetic Centre. The examination included assessing periodontal pocket depth in mm, gingival status, plaque accumulation, and glycemic status (HbA1c in % and fasting blood sugar in mg/dL) of each individual patient at baseline and after 3 months of the intervention. Periodontal pocket depth was assessed by measuring the PPD with a UNC-15 probe at six points for each tooth and the arithmetic mean value of all the teeth was considered.
The gingival status was assessed by the GI of Loe and Silness [9], and dental plaque by the PI of Silness and Loe [10]. The participants were interviewed for demographic data, and the duration and frequency of drug usage, which was later cross-verified with their hospital records.
Statistical analysis was carried out using SPSS ver. 16.0 (SPSS, Inc., Chicago, IL, USA). Levene's test for homogeneity of variance (P<0.05) was performed, as we assumed equity of variance was more important than an assumption of normality. A comparison of the mean differences of the PPD, HbA1c, and fasting blood sugar level was analyzed by a paired t-test and between the groups by one-way analysis of variance (ANOVA), while the mean differences in the GI and PI scores were analyzed by the Wilcoxon signed rank test and between the groups by Kruskal-Wallis ANOVA. Statistical significance was considered to be when P≤0.05 (95% confidence interval). The associations between glycemic control and potential predicting factors were evaluated with multiple linear regression analysis using HbA1c as a dependent variable. Variables that were found to have a greater impact were included in stepwise regression analysis.
RESULTS
All of the 60 participants completed the study. It was found that the mean changes in the PPD, fasting blood sugar, and HbA1c after intervention in groups A and B were statistically significant (P<0.001), while in group C, they were statistically non significant (P=0.078). On comparison between the groups, the mean PPD and fasting blood sugar level did not show any statistically significant differences. It was found that the HbA1c level (P=0.004), GI score (P=0.001), and PI score (P=0.001) showed a statistically significant difference after 3 months of the treatment regime. A greater reduction in the mean±standard deviation HbA1c level could be seen in group A (0.58±0.27), followed by group B (0.25±0.14) and group C (0.004±0.12). A statistically significant difference was seen in the comparison between the groups, with the significant pair being groups A and C. A marked statistically significant difference in the GI and PI scores was seen (P<0.001) after 3 months of intervention. A statistically significant difference was seen on comparing among the groups, with the significant pairs being groups A and B, and groups A and C for the GI scores; and groups A and C, and groups B and C for the PI scores (Table 1).
Table 1.
Comparison of mean changes of PPD, GI, PI, HbA1c, frequency of drug and fasting blood sugar level among all the three groups.
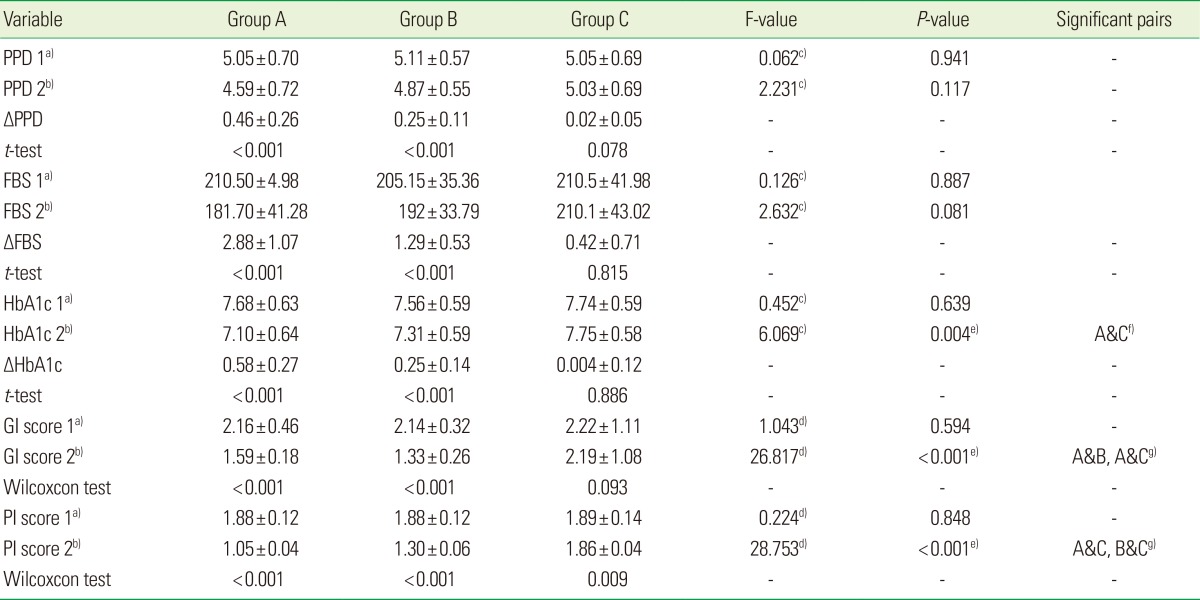
Values are presented as mean±standard deviation.
PPD: probing pocket depth, GI: gingival index, PI: plaque index; HbA1c: glycated haemoglobin, FBS: fasting blood sugar, Group A: scaling, Group B: mouthwash, Group C: control.
a)1, at baseline. b)2, after 3-month intervention. c)Analysis of variance. d)Kruskall Wallis test. e)Significance. f)Bonferroni test. g)Mann-Whitney test.
Table 2 depicts the association of all of the independent variables with HbA1c in group A through a simple linear regression model. The simple linear regression model showed that out of all of the independent variables, the GI score and frequency of drug use independently (b=0.911 and b=0.493) showed a strong relationship with the HbA1c. On stepwise regression analysis, both the GI score and frequency of drug usage showed statistical significance (R2=0.832) at P<0.05. The B value reflected that with an increase in 1.23 units in the GI score, there would be an increase in 1 unit of the HbA1c level (Table 3).
Table 2.
Simple linear regression analysis showing the association between independent variables and HbA1c in group A subjects.
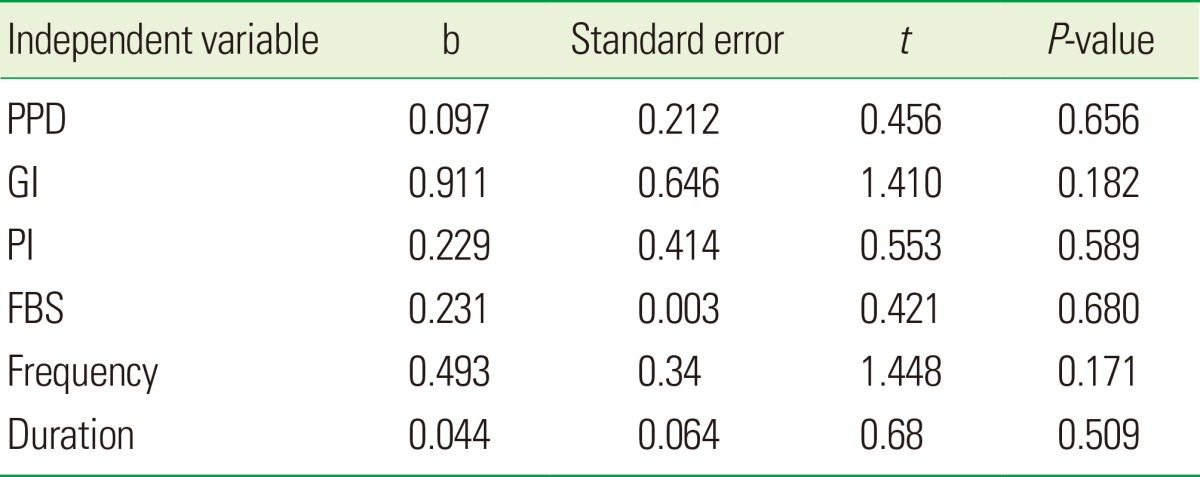
P<0.05, significant.
HbA1c: glycated haemoglobin, PPD: probing pocket depth, GI: gingival index, PI: plaque index; FBS: fasting blood sugar, Group A: scaling, Group B: mouthwash, Group C: control.
Table 3.
Multiple linear regression analysis showing the influence of the two most independent variables with glycated haemoglobin.
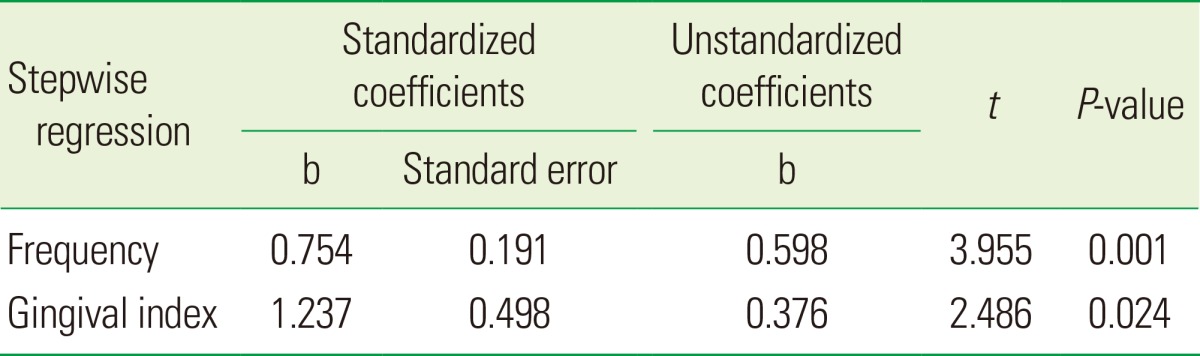
R2=0.832. P<0.05, significant.
DISCUSSION
The influence of diabetes on periodontal health has been discussed widely in the dental literature [11]. Periodontal disease has been reported to be the sixth complication of diabetes [12].
There is substantial evidence to support considering diabetes as a risk factor for poor periodontal health; there is also evidence that periodontal infection adversely affects glycemic control in diabetes. This study assessed the effect of nonsurgical periodontal therapy on glycemic control in DM2 patients on oral medication by comparing treatment groups (A, B) with a control group (C). The control group was choosen so as to overcome the Hawthorne effect [13]. Although the subjects in group C were given no treatment except brushing and oral hygiene instructions, after the completion of study, these subjects were given full non-surgical periodontal treatment and supportive treatment if needed. The periodontal parameters measured were PI, GI, and PPD, and were correlated with fasting blood sugar and HbA1c. The HbA1c was taken because HbA1c is a reflection of the mean blood glucose concentration over the preceeding 1-3 months, while fasting blood sugar reflects differences over a short period of time, which is clinically less relevant.
The healing results of nonsurgical periodontal therapy were assessed after 3 months. Opinions differ in the literature concerning the appropriate time for assessing the healing response to nonsurgical therapy. Studies done by various authors have shown that in periodontal pockets of 4-7 mm depth, most changes occur in the first 3-5 months, while in deep pockets up to 12 mm, a gradual improvement takes place over a period of 12 months [14]. In our study, the response to nonsurgical periodontal therapy was evaluated after 3 months, as the majority of the examined sites had a PPD up to 3-6 mm only.
The outcome of this study corroborates prior evidence supporting an interaction between periodontal status and diabetic metabolic control [15], and supports the hypothesis that successful periodontal treatment can improve glucose metabolism. These findings document a direct interrelationship between periodontal conditions and metabolic parameters in DM2 patients, extending earlier studies reporting a similar relationship that did not consider DM2 specifically [16].
Periodontal disease may affect insulin signalling through proinflammatory mediators. The highly vascularised inflamed periodontium can be a source of inflammatory mediators, such as tumor necrosis factor (TNF), which can affect glucose and fat metabolism [17]. The proinflammatory cytokine TNF impairs insulin signalling by increasing the adipose secretion of free fatty acids. There is a consensus that this process weakens glycemic control in diabetic patients by raising insulin resistance. Accordingly, periodontal therapy might improve glycemic control by decreasing proinflammatory mediators.
Indirect and direct evidence supports the concept that periodontal infection adversely affects glycemic control in people with diabetes [18]. Indirect evidence supporting the biological plausibility of this link is derived from studies of the relationship between insulin resistance and the response to inflammation. Insulin resistance has been observed in active inflammatory connective tissue diseases [19], other clinical diseases [20], and acute infection [21].
The inflamed periodontium is highly vascular, and the ulcerated pocket epithelium may serve as a portal to the systemic circulation for bacterial products and locally produced inflammatory mediators. Hence, chronic periodontitis, a predominantly gram-negative infection, may serve as a focal source for sustained entry of bacterially derived lipopolysaccharides and host-produced inflammatory mediators into the systemic circulation [22]. Among the inflammatory mediators produced in response to the bacterial challenge in chronic periodontitis are interleukin (IL)-1β, IL-6, and TNF-α. These mediators have been shown to influence glucose metabolism [23], while TNF-α has also been reported to cause insulin resistance [24]. IL-1β and IL-6 have been reported to antagonize insulin action [25].
The results of this study showed that, following professional scaling, there was marked improvement in the HbA1c level by 0.58%, which was similar to the result of a meta-analysis of 0.40% [11]. Moreover, our findings are consistent with prior positive responses to nonsurgical periodontal therapy in persons with DM2 reported by Westfelt et al. [26]. On the other hand, studies involving systemic antibiotics accompanying mechanical therapy reported an improvement in both periodontal status and glycemic control [27], whereas studies including periodontal treatment alone reported improvement in periodontal status only [4]. In this study, group A, following periodontal therapy (i.e., scaling), a marked significant reduction in HbA1c was observed along with decreased plaque scores, decreased GI scores, and lower PPD values. The results showed that the frequency of drug use and gingival inflammation had a greater impact on HbA1c than the other independent variables, which was in agreement with the study done by Kiran et al. [28]. The reduced plaque levels, in turn, would reduce the gram-negative bacteria in plaque. This decreased plaque level would decrease gingival inflammation, which had an effect on reducing insulin resistance. In group B, with the use of 0.12% chlorhexidine, there was a significant reduction in HbA1c, but it was comparatively less than that of group A. This might be because using mouthwash does not itself completely eliminate the etiological factors like plaque responsible for inducing gingivitis.
It was found that providing professional scaling to the diabetic patient, as an adjunct to oral hypoglycemic drugs, provided an additive effect in reducing HbA1c levels and thus contributing to the good general health of the patient. Thus, dental professionals, along with physicians, can lend a helpful hand in improving the glycemic level by controlling the inflammatory cytokines in DM2 patients.
The limitations of this study included the following: The sample size was not large enough to analyze patients with moderate and severe periodontitis separately, the plasma marker of systemic inflammation was not considered and correlated, the long-term effect of periodontal therapy for at least 6 months should have been considered, and the dosage of the drug was also not recorded.
The present study concludes that nonsurgical periodontal therapy can effectively decrease fasting blood sugar and HbA1c levels in diabetic patients on medication. Preventive periodontal regimens for diabetic patients should be sufficiently intense and sustained so as to eliminate periodontal inflammation and should be closely coordinated with the patient's overall clinical diabetic management.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Mealy B. Diabetes Mellitus. In: Greenberg MS, Glick M, editors. Burket's oral medicine diagnosis and treatment. 10th ed. New York: B.C. Decker; 2003. pp. 563–577. [Google Scholar]
- 2.Taylor GW. The effects of periodontal treatment on diabetes. J Am Dent Assoc. 2003;134 Spec No:41S–48S. doi: 10.14219/jada.archive.2003.0371. [DOI] [PubMed] [Google Scholar]
- 3.Chinese Diabetes Society. China guideline for type 2 diabetes. Chin J Diabetes Mellitus. 2010;2(Suppl 2):6–56. [Google Scholar]
- 4.Seppälä B, Ainamo J. A site-by-site follow-up study on the effect of controlled versus poorly controlled insulin-dependent diabetes mellitus. J Clin Periodontol. 1994;21:161–165. doi: 10.1111/j.1600-051x.1994.tb00297.x. [DOI] [PubMed] [Google Scholar]
- 5.Tervonen T, Knuuttila M. Relation of diabetes control to periodontal pocketing and alveolar bone level. Oral Surg Oral Med Oral Pathol. 1986;61:346–349. doi: 10.1016/0030-4220(86)90417-2. [DOI] [PubMed] [Google Scholar]
- 6.Southerland JH, Taylor GW, Offenbacher S. Diabetes and periodontal infection: making the connection. Clin Diabetes. 2005;23:171–178. [Google Scholar]
- 7.Dağ A, Firat ET, Arikan S, Kadiroglu AK, Kaplan A. The effect of periodontal therapy on serum TNF-alpha and HbA1c levels in type 2 diabetic patients. Aust Dent J. 2009;54:17–22. doi: 10.1111/j.1834-7819.2008.01083.x. [DOI] [PubMed] [Google Scholar]
- 8.Mealey BL. Periodontal disease and diabetes: a two-way street. J Am Dent Assoc. 2006;137:26S–31S. doi: 10.14219/jada.archive.2006.0404. [DOI] [PubMed] [Google Scholar]
- 9.Loe H, Silness J. Periodontal disease in pregnancy: I. prevalence and severity. Acta Odontol Scand. 1963;21:533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 10.Silness J, Loe H. Periodontal disease in pregnancy: II. correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 11.Cohen DW, Friedman LA, Shapiro J, Kyle GC, Franklin S. Diabetes mellitus and periodontal disease: two-year longitudinal observations. I. J Periodontol. 1970;41:709–712. doi: 10.1902/jop.1970.41.12.709. [DOI] [PubMed] [Google Scholar]
- 12.Lowe GD. The relationship between infection, inflammation, and cardiovascular disease: an overview. Ann Periodontol. 2001;6:1–8. doi: 10.1902/annals.2001.6.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Moeintaghavi A, Arab HR, Bozorgnia Y, Kianoush K, Alizadeh M. Non-surgical periodontal therapy affects metabolic control in diabetics: a randomized controlled clinical trial. Aust Dent J. 2012;57:31–37. doi: 10.1111/j.1834-7819.2011.01652.x. [DOI] [PubMed] [Google Scholar]
- 14.Lowenguth RA, Greenstein G. Clinical and microbiological response to nonsurgical mechanical periodontal therapy. Periodontol 2000. 1995;9:14–22. doi: 10.1111/j.1600-0757.1995.tb00052.x. [DOI] [PubMed] [Google Scholar]
- 15.da Cruz GA, de Toledo S, Sallum EA, Sallum AW, Ambrosano GM, de Cassia Orlandi Sardi J, et al. Clinical and laboratory evaluations of non-surgical periodontal treatment in subjects with diabetes mellitus. J Periodontol. 2008;79:1150–1157. doi: 10.1902/jop.2008.070503. [DOI] [PubMed] [Google Scholar]
- 16.Tervonen T, Karjalainen K, Knuuttila M, Huumonen S. Alveolar bone loss in type 1 diabetic subjects. J Clin Periodontol. 2000;27:567–571. doi: 10.1034/j.1600-051x.2000.027008567.x. [DOI] [PubMed] [Google Scholar]
- 17.Lösche W, Karapetow F, Pohl A, Pohl C, Kocher T. Plasma lipid and blood glucose levels in patients with destructive periodontal disease. J Clin Periodontol. 2000;27:537–541. doi: 10.1034/j.1600-051x.2000.027008537.x. [DOI] [PubMed] [Google Scholar]
- 18.Teeuw WJ, Gerdes VE, Loos BG. Effect of periodontal treatment on glycemic control of diabetic patients: a systematic review and meta-analysis. Diabetes Care. 2010;33:421–427. doi: 10.2337/dc09-1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Svenson KL, Lundqvist G, Wide L, Hallgren R. Impaired glucose handling in active rheumatoid arthritis: relationship to the secretion of insulin and counter-regulatory hormones. Metabolism. 1987;36:940–943. doi: 10.1016/0026-0495(87)90128-4. [DOI] [PubMed] [Google Scholar]
- 20.Beck-Nielsen H. Clinical Disorders of Insulin Resistance. In: Alberti KG, Viberti G, editors. International textbook of diabetes mellitus. New York: Wiley; 1992. pp. 531–568. [Google Scholar]
- 21.Sammalkorpi K. Glucose intolerance in acute infections. J Intern Med. 1989;225:15–19. doi: 10.1111/j.1365-2796.1989.tb00030.x. [DOI] [PubMed] [Google Scholar]
- 22.Grossi SG, Genco RJ. Periodontal disease and diabetes mellitus: a two-way relationship. Ann Periodontol. 1998;3:51–61. doi: 10.1902/annals.1998.3.1.51. [DOI] [PubMed] [Google Scholar]
- 23.Iwamoto Y, Nishimura F, Nakagawa M, Sugimoto H, Shikata K, Makino H, et al. The effect of antimicrobial periodontal treatment on circulating tumor necrosis factor-alpha and glycated hemoglobin level in patients with type 2 diabetes. J Periodontol. 2001;72:774–778. doi: 10.1902/jop.2001.72.6.774. [DOI] [PubMed] [Google Scholar]
- 24.Feingold KR, Grunfeld C. Role of cytokines in inducing hyperlipidemia. Diabetes. 1992;41(Suppl 2):97–101. doi: 10.2337/diab.41.2.s97. [DOI] [PubMed] [Google Scholar]
- 25.Ling PR, Istfan NW, Colon E, Bistrian BR. Differential effects of interleukin-1 receptor antagonist in cytokine- and endotoxin-treated rats. Am J Physiol. 1995;268(2 Pt 1):E255–E261. doi: 10.1152/ajpendo.1995.268.2.E255. [DOI] [PubMed] [Google Scholar]
- 26.Westfelt E, Rylander H, Blohme G, Jonasson P, Lindhe J. The effect of periodontal therapy in diabetics: results after 5 years. J Clin Periodontol. 1996;23:92–100. doi: 10.1111/j.1600-051x.1996.tb00540.x. [DOI] [PubMed] [Google Scholar]
- 27.Alpagot T, Wolff LF, Smith QT, Tran SD. Risk indicators for periodontal disease in a racially diverse urban population. J Clin Periodontol. 1996;23:982–988. doi: 10.1111/j.1600-051x.1996.tb00524.x. [DOI] [PubMed] [Google Scholar]
- 28.Kiran M, Arpak N, Unsal E, Erdogan MF. The effect of improved periodontal health on metabolic control in type 2 diabetes mellitus. J Clin Periodontol. 2005;32:266–272. doi: 10.1111/j.1600-051X.2005.00658.x. [DOI] [PubMed] [Google Scholar]


