Abstract
BACKGROUND
Long-term adhesion-related complications and incisional hernias after abdominal surgery are common and costly. There are few data on the risk of these complications after different abdominal operations.
STUDY DESIGN
We identified Medicare beneficiaries who underwent endovascular repair of an abdominal aortic aneurysm from 2001–2008 who presumably are not at risk for laparotomy-related complications. We identified all laparoscopic and open operations involving the abdomen, pelvis, or retroperitoneum and categorized them into 5 groups according to invasiveness. We then identified laparotomy-related complications for up to 5 years after the index operation and compared these with the baseline rate of complications in a control group of patients who did not undergo an abdominal operation.
RESULTS
We studied 85,663 patients, 7,513 (8.8%) of which underwent a laparotomy, including 2,783 major abdominal operations, 709 minor abdominal operations, 963 ventral hernia repairs, 493 retroperitoneal/pelvic operations, and 2,565 laparoscopic operations. Mean age was 76.7 years and 82.0% were male. Major abdominal operations carried the highest risk for adhesion-related complications (14.3% and 25.0% at 2 and 5 years compared with 4.0% and 7.8% for the control group; p < 0.001) and incisional hernias (7.8% and 12.0% compared with 0.6% and 1.2% for the control group; p < 0.001). Laparoscopic operations (4.6% and 10.7% for adhesions, 1.9% and 3.2% for incisional hernias) carried the lowest risk.
CONCLUSIONS
Late-onset laparotomy-related complications are frequent and their risk extends through 5 years beyond the perioperative period. With the advancement and expansion of laparoscopic techniques and its attendant lower risk for long-term complications, these results can alter the risk-to-benefit profile of various types of abdominal operations and can also strengthen the rationale for additional development of laparoscopic approaches to abdominal operations.
Long-term complications after abdominal surgery, including adhesion-related complications and incisional hernia repairs, are common and costly, but the risks for these complications have been poorly characterized. Although rarely fatal, both of these complications can have substantial clinical and cost implications because they frequently require additional hospitalizations and/or surgical procedures. These longer-term complications must be considered when counseling patients about the risks and benefits of surgery and different surgical approaches.
After undergoing laparotomy, 93% of patients have been shown to have adhesions at a subsequent operation1 and the risk of bowel enterotomy during reoperations complicated by adhesions is as high as 19%.2 Although many adhesions are asymptomatic, others cause serious complications, such as bowel obstruction and ischemia. The prevalence of incisional hernia after laparotomy is reported to be between 11% and 20%,3,4 and incisional hernia recurrence after surgical repair is as high as 45%.5,6 Incisional hernias cause pain and other more serious problems, such as bowel obstruction, incarceration, and strangulation. Surgeons are aware of these complications, but few studies have examined the risk of such complications for different types of abdominal procedures.7
Few data that we are aware of have examined the risks of laparotomy-related complications after various types of abdominal operations. Previously, we showed high rates of laparotomy-related complications after open abdominal aortic aneurysm (AAA) repair, but also noted a baseline rate of such complications after endovascular repair (EVAR).8,9 Because uncomplicated EVAR is confined to the arterial system, there should be no risk of laparotomy-related complications, so observed complications in the EVAR group were likely influenced by earlier abdominal surgery. We therefore studied the risks of late-onset laparotomy-related complications in a large cohort of patients undergoing EVAR to estimate the rates of laparotomy-related complications in a general elderly population.
METHODS
Patient selection
We used a previously identified cohort of all traditional Medicare beneficiaries with a diagnosis of AAA who underwent endovascular repair during the period 2001–2008 as our study group. We identified all traditional Medicare beneficiaries age 67 or older with at least 2 years of earlier Medicare claims who had a diagnosis of AAA (ICD-9-CM code 441.4) and underwent EVAR (code 39.71 endovascular implantation of graft). Benefi-ciaries enrolled in health maintenance organizations at any time during the study period and those not enrolled in both Medicare Parts A and B were excluded.
Identifying laparotomy/laparoscopic operations
We used Current Procedural Terminology codes to identify laparoscopic and open operations involving the abdomen, pelvis, or retroperitoneum (RP). We categorized these into 5 distinct laparotomy (LAP) groups based on the level of invasiveness and direct entry into the peritoneal space (see Appendix; online only): those who underwent major abdominal operations (eg, esophagectomy, colectomy, hepatectomy, pancreatectomy), minor abdominal operations (eg, open appendectomy, gastrostomy, cecostomy, ileostomy), abdominal wall hernia operations (inguinal hernias were excluded), RP/pelvic operations (eg, total abdominal hysterectomy, nephrectomy, cystectomy), and all laparoscopic operations. Those who underwent 2 operations more than 30 days apart where the second operation was not a study result were categorized according to their first operation. As a sensitivity analysis, we categorized them according to their most invasive operation, but this did not substantively affect our results.
Identifying late-onset laparotomy-related complications
We identified late-onset laparotomy-related complications using both ICD-9-CM diagnosis codes and CPT procedure codes (Table 1). Complications were categorized as hernia-related or adhesion-related. Hernia-related complications included ventral incisional hernia repairs. Adhesion-related complications were characterized as operative (lysis of adhesions, small bowel resection, and large bowel resection) and nonoperative (admission for bowel obstruction without an operation). To ensure that small and large bowel resections were performed for adhesions or obstructions rather than diverticular disease or carcinoma, we required all bowel resection procedure codes to be accompanied by a diagnosis code for bowel obstruction.
Table 1.
ICD-9 Diagnosis Codes and CPT Procedure Codes Used to Identify Laparotomy-Related Complications
| Code | Description |
|---|---|
| Bowel obstruction* | |
| 560.1 | Paralytic ileus |
| 560.8 | Intestinal obstruction without mention of hernia |
| 560.81 | Intestinal or peritoneal adhesions with obstruction |
| 560.89 | Pseudo-obstruction or mural thickening causing obstruction |
| 560.9 | Unspecified intestinal obstruction |
| 552.21 | Incisional hernia with obstruction |
| Incisional hernia repairs† | |
| 49560 | Repair initial incisional or ventral hernia; reducible |
| 49561 | Incarcerated or strangulated |
| 49565 | Repair recurrent incisional or ventral hernia; reducible |
| 49566 | Incarcerated or strangulated |
| 49568 | Implantation of mesh for incisional or ventral hernia |
| 49654 | Laparoscopy, surgical, repair, incisional hernia; reducible |
| 49655 | Incarcerated or strangulated |
| 49656 | Laparoscopy, surgical, repair, recurrent incisional hernia; reducible |
| 49657 | Incarcerated or strangulated |
| Lysis of adhesions† | |
| 44005 | Enterolysis (freeing of intestinal adhesion) |
| 44180 | Laparoscopy, surgical, enterolysis (freeing of intestinal adhesion) |
| Small bowel resection† | |
| 44202 | Laparoscopy, surgical; enterectomy; resection of small intestine |
| 44203 | Each additional small intestine resection |
| 44120 | Enterectomy, resection of small intestine; single resection |
| 44130 | Enteroenterostomy, anastomosis of intestine |
| 44186 | Laparoscopy, surgical; jejunostomy (eg, for decompression or feeding) |
| 44187 | Ileostomy or jejunostomy, non-tube |
| Large bowel resection† | |
| 44140 | Colectomy, partial; with anastomosis |
| 44141 | With skin-level cecostomy or colostomy |
| 44143 | With end colostomy and closure of distal segment |
| 44144 | With resection, with colostomy or ileostomy and creation of mucofistula |
| 44160 | Colectomy, partial, with removal of terminal ileum with ileocolostomy |
| 44204 | Laparoscopy, surgical; colectomy, partial, with anastomosis |
| 44205 | With removal of terminal ileum with ileocolostomy |
| 44206 | With end colostomy and closure of distal segment |
| 44213 | Laparoscopy, surgical; mobilization of splenic flexure with partial colectomy |
| 44188 | Laparoscopy, surgical, colostomy or skin level cecostomy |
ICD-9 codes.
Current Procedural Terminology codes.
To be considered a late-onset laparotomy complication, the event had to occur at least 30 days after the initial operation. Complications that occurred within 30 days of the operation were excluded. Because all of the operative complications (lysis of adhesions, small bowel resection, large bowel resection) could have also qualified as an initial LAP operation, these were only counted as a complication if they were preceded by an earlier operation.
Control group
We included as a control population all patients who did not undergo a designated LAP operation for the 2-year period before their EVAR. We imposed this 2-year “clean” period to limit the potential impact of any pre-existing adhesions resulting from an earlier operation that occurred before enrollment in Medicare. The date of their EVAR then became their index date to determine rates of subsequent complications. We chose a 2-year period because in a previous study we found that most laparotomy-related complications after open AAA repair occurred within 2 years of the operation.8 In addition, previous studies have shown that most incisional hernias occur within 12 months of the laparotomy,10,11 and the greatest percentage of readmissions due to adhesion-related complications occurs in the first year after laparotomy.7
If the first episode after the clean period is a nonoperative admission for a bowel obstruction, they are counted as part of the baseline complication rate in the control population for nonoperative admissions due to adhesions, but continue to be followed until an operative complication is encountered. If the first episode after the clean period is an operative complication, they are counted as part of the baseline complication rate in the control population. See Figure 1 for a flowchart demonstrating the creation of the 5 LAP groups and the control group.
Figure 1.
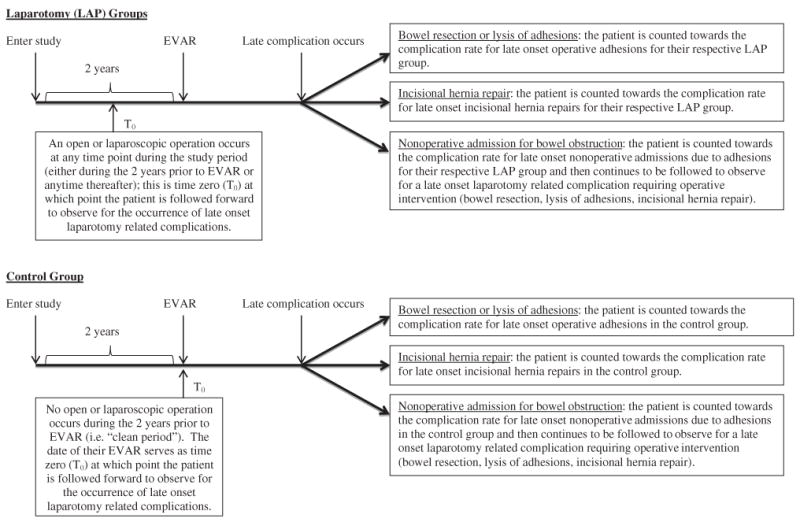
Flow chart demonstrating the creation of the 5 laparotomy (LAP) groups and the control group. All patients enter the study 2 years before the date of their endovascular aneurysm repair (EVAR).
Statistical analysis
We calculated the total number of patients who underwent an operation in each of the 5 LAP groups and in the control group and then calculated the number of those patients with a laparotomy-related complication 30 days or more after the index operation (or index date for the control group). Freedom from late-onset laparotomy-related complications at 2 and 5 years was estimated with the use of Kaplan-Meier life-table methods. We tested for differences in time to a complication between the control group and each of the 5 LAP groups by deriving approximate z-tests from the fitted confidence limits at 2 and 5 years and evaluating a p value for the difference.
Categorical variables were compared with chi-square tests and continuous variables were compared with Student’s t-test or Wilcoxon rank sum test, where appropriate. All statistical analyses were performed using SAS 9.1.3 statistical software (SAS Institute). This study was approved by the Institutional Review Board at Harvard Medical School.
RESULTS
We studied 85,663 patients who underwent EVAR between 2001 and 2008 and who had at least 2 years of Medicare enrollment before their EVAR procedure. Of these, 7,513 patients (8.8%) underwent one of the predefined LAP operations during the study period: 2,783 (37.0%) had a major abdominal operation, 709 (9.4%) had a minor abdominal operation, 963 (12.8%) had a ventral hernia repair without any record of an earlier LAP operation, 493 (6.6%) had an RP/pelvic operation, and 2,565 (34.1%) had a laparoscopic operation. The control group consisted of 78,150 patients who had a 2-year “clean” period during which there were no LAP operations.
Mean age of the control group and all patients in the 5 LAP groups were similar (76.8 vs 76.5 years). Eighty-two percent of the study group patients were male (Table 2). Patients in all 5 LAP groups had a higher incidence of comorbid conditions when compared with the control group. Those who underwent abdominal wall hernia operations were younger. Patients undergoing RP/pelvic operations were more likely to be women.
Table 2.
Demographic and Comorbidities of the Patients Undergoing an Operation in Each of the 5 Laparotomy Groups and the Control Group
| Variable | Control group (n = 78,150) |
Major open abdominal (n = 2,783) |
Minor open abdominal (n = 709) |
Abdominal wall hernia (n = 963) |
RP/pelvic (n = 493) |
Laparoscopic (n = 2,565) |
|---|---|---|---|---|---|---|
| Male, % | 82.2 | 80.1* | 88. 2† | 81.9 | 72.2† | 80.4‡ |
| Age, y, mean | 76.8 | 76.8 | 76.0 | 75.7 | 76.4 | 76.7 |
| 67–69, % | 12.0 | 10.9 | 14.0† | 12.6† | 11.0† | 11.9† |
| 70–74, % | 26.0 | 26.1 | 30.0‡ | 33. 0† | 27.4 | 25.8 |
| 75–79, % | 34.6 | 35.5 | 30.9‡ | 34.9 | 37.5 | 36.3 |
| 80–84, % | 16.6 | 17.8 | 17.5 | 13.9‡ | 16.8 | 16.7 |
| 85 or older, % | 10.8 | 9.7 | 7.6* | 5.6† | 7.3‡ | 9.3‡ |
| Race/ethnicity, % | ||||||
| White | 95.2 | 94.6 | 94.5 | 95.3 | 96.2 | 95.3 |
| Black | 2.9 | 3.7‡ | 2.7 | 2.6 | 2.2 | 2.5 |
| Other | 1.9 | 1.7 | 2.8 | 2.1 | 1.6 | 2.2 |
| Comorbidities, % | ||||||
| MI within 6 mo | 1.5 | 1.8 | 3.1† | 1.3 | 1.0 | 1.2 |
| MI 7–24 mo | 7.8 | 11.8† | 16.4† | 9.7‡ | 12.0† | 11.2† |
| Valvular heart disease | 11.6 | 14.7† | 18.2† | 13.9‡ | 11.6 | 14.5† |
| CHF | 14.0 | 20.9† | 28.2† | 19.1† | 18.1* | 19.5† |
| PVD | 20.0 | 24.4† | 31.3† | 24.0* | 28.6† | 23.1† |
| CVD | 15.7 | 16.4 | 29.3† | 17.3 | 15.4 | 16.2 |
| Hypertension | 65.7 | 77.9† | 76.7† | 74.7† | 77.9† | 75.7† |
| Diabetes | 19.0 | 22.2† | 24.7† | 23.3† | 19.5 | 21.7† |
| COPD | 28.2 | 42.6† | 47.4† | 38.0† | 34.7* | 35.4† |
| Renal insufficiency | 6.7 | 9.6† | 17.1† | 9.8† | 13.8† | 10.1† |
| ESRD | 0.5 | 0.7 | 6.8† | 0.8 | 4.9† | 1.0* |
| Cancer | 19.6 | 51.1† | 34.0† | 24.0† | 63.1† | 25.2† |
| Obesity | 2.6 | 3.4‡ | 3.0 | 6.3† | 3.0 | 4.1† |
Comparisons are made between each laparotomy group and the control group.
p < 0.01 when compared with the control group.
p < 0.001 when compared with the control group.
p < 0.05 when compared with the control group.
CHF, congestive heart failure; CVD, cerebral vascular disease; ESRD, end-stage renal disease, PVD, peripheral vascular disease.
Late-onset laparotomy-related complications
Risk for late-onset laparotomy-related complications extended well out to 5 years for all 5 LAP groups (Table 3). Major abdominal operations had the highest risk of complications compared with the control group: 4.8% and 8.8% (p < 0.001, at 2 and 5 years) for operative adhesion complications and 14.3% and 25.0% (p < 0.001, at 2 and 5 years) for any adhesion complications (both operative and nonoperative). For operative adhesion complications at 5 years, major abdominal operations conveyed the most risk (p < 0.001), followed by abdominal wall hernia operations and laparoscopic operations (both p < 0.05). Among the 5 LAP groups, RP/pelvic and laparoscopic operations had the lowest risk for any adhesion complications compared with the control group (5.1% and 10.6% at 2 and 5 years for RP/pelvic [p = NS for both] and 4.6% [p = NS] and 10.7% [p < 0.001] at 2 and 5 years for laparoscopic). Abdominal wall hernia operations and minor abdominal operations had significantly higher rates of any adhesion complications compared with the control group, although the risk was not as high as with major abdominal operations.
Table 3.
Probability of Late-Onset Laparotomy-Related Complications at 2 and 5 Years after the Index Operation (or Index Date for the Control Population)
| Complication/index operation | Probability of complications, % | |
|---|---|---|
| 2 y | 5 y | |
| Operative adhesions: admission for bowel resection or lysis of adhesions | ||
| Major abdominal (n = 2,783) | 4.8* | 8.8* |
| Minor abdominal (n = 709) | 1.5 NS | 3.3 NS |
| Hernia (n = 963) | 1.2 NS | 3.2† |
| RP/pelvic (n = 493) | 1.4 NS | 3.1 NS |
| Laparoscopic (n = 2,565) | 1.2† | 2.6† |
| Control group (n = 78,150) | 0.8 | 1.7 |
| Nonoperative adhesions: admission for bowel obstruction without surgery | ||
| Major abdominal (n = 2,783) | 11.7* | 20.9* |
| Minor abdominal (n = 709) | 7.1* | 16.2* |
| Hernia (n = 963) | 5.2‡ | 11.7* |
| RP/pelvic (n = 493) | 4.4 NS | 8.7 NS |
| Laparoscopic (n = 2,565) | 3.6 NS | 8.7* |
| Control group (n = 78,150) | 3.2 | 6.2 |
| Any adhesions: admission for bowel obstruction with or without surgery | ||
| Major abdominal (n = 2,783) | 14.3* | 25.0* |
| Minor abdominal (n = 709) | 8.0* | 18.3* |
| Hernia (n = 963) | 6.2‡ | 13.6* |
| RP/pelvic (n = 493) | 5.1 NS | 10.6 NS |
| Laparoscopic (n = 2,565) | 4.6 NS | 10.7* |
| Control group (n = 78,150) | 4.0 | 7.8 |
| Incisional hernia repair | ||
| Major abdominal (n = 2,783) | 7.8* | 12.0* |
| Minor abdominal (n = 709) | 3.0* | 5.6* |
| Hernia (n = 963) | 3.6* | 7.4* |
| RP/pelvic (n = 493) | 2.5† | 4.6‡ |
| Laparoscopic (n = 2,565) | 1.9* | 3.2* |
| Control group (n = 78,150) | 0.6 | 1.2 |
| Any surgery: incisional hernia repair, bowel resection, or lysis of adhesions | ||
| Major abdominal (n = 2,783) | 11.1* | 18.1* |
| Minor abdominal (n = 709) | 4.3* | 8.3* |
| Hernia (n = 963) | 4.7* | 9.6* |
| RP/pelvic (n = 493) | 3.8† | 7.3‡ |
| Laparoscopic (n = 2,565) | 2.9* | 5.4* |
| Control group (n = 78,150) | 1.4 | 2.8 |
p < 0.001 when compared with the control group.
p < 0.05 when compared with the control group.
p < 0.01 when compared with the control group.
NS, nonsignificant values; RP, retroperitoneum.
All 5 LAP groups had an increased risk for incisional hernia repairs at both 2 and 5 years compared with the control group (all p < 0.001 except RP/pelvic p < 0.05 at 2 years). Major abdominal operations conveyed the highest risk (7.8% and 12.0%, at 2 and 5 years), followed by abdominal wall hernia repairs (3.6% and 7.4%). Retroperitoneum/pelvic (2.5% and 4.6%) and laparoscopic operations (1.9% and 3.2%) conveyed the lowest risk, although still significantly higher than the control group. When examining any surgical complication (incisional hernia repair, bowel resection, or lysis of adhesions), major abdominal operations conveyed the highest risk at 2 and 5 years (11.1% and 18.1%; p < 0.001). The 4 other LAP groups had higher rates of any surgical complication as well, but these were less than half the risk associated with major abdominal operations.
The control group had low rates of de novo operative adhesion complications (0.8% and 1.7%, at 2 and 5 years) and incisional hernia repairs (0.6% and 1.2%). However, they did have a 3.2% and 6.2% risk for nonoperative adhesion complications at 2 and 5 years, which likely represent bowel obstructions that arise for other reasons or from operations that occurred before the 2-year “clean” window.
Freedom from operative, nonoperative, and any adhesion-related complications are shown in Figures 2A, 2B, and 2C, respectively. Freedom from incisional hernia complications and any surgical complication (incisional hernia repair, bowel resection, or lysis of adhesions) are shown in Figures 2D and 2E. These results mirror those reported for the discrete 2-and 5-year follow-up periods.
Figure 2.
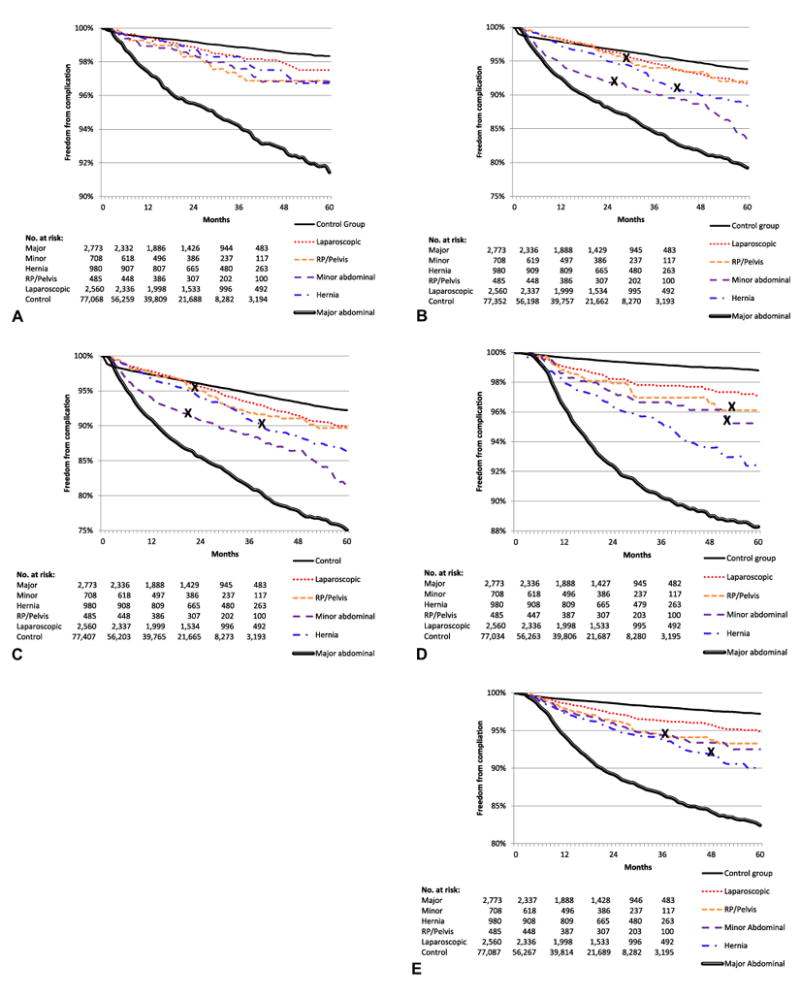
(A) Freedom from operative late-onset laparotomy-related adhesion complications (bowel resection or lysis of adhesions) in each of the 5 laparotomy (LAP) groups and the control group. Standard error does not exceed 10% for all survival curves. (B) Freedom from nonoperative late-onset laparotomy-related adhesion complications in each of the 5 LAP groups and the control group. X denotes where the standard error exceeds 10%, otherwise the standard error does not exceed 10% for all other survival curves. (C) Freedom from any late-onset laparotomy-related adhesion complications in each of the 5 LAP groups and the control group. X denotes where the standard error exceeds 10%, otherwise the standard error does not exceed 10% for all other survival curves. (D) Freedom from late-onset laparotomy-related incisional hernia repairs in each of the 5 LAP groups and the control group. X denotes where the standard error exceeds 10%, otherwise the standard error does not exceed 10% for all other survival curves. (E) Freedom from any surgery (bowel resection, lysis of adhesions, and incisional hernia repair) for late-onset laparotomy-related complications in each of the 5 LAP groups and the control group. X denotes where the standard error exceeds 10%, otherwise the standard error does not exceed 10% for all other survival curves. RP, retroperitoneum.
DISCUSSION
With the growth of minimally invasive techniques, the risk of laparotomy-related complications after abdominal operations might be changing. Even for major abdominal operations, however, these risks have been poorly defined previously. In addition, few earlier studies have examined the risk of such complications for different types of abdominal operations. In this study, we used a cohort of Medicare patients who underwent EVAR to study the risk of late-onset laparotomy-related complications for open and laparoscopic operations involving entry into the abdomen.
We found that major abdominal operations have the highest risk for late-onset laparotomy-related complications at 2 and 5 years post surgery. At 5 years, one fourth of all elderly patients who have undergone a major abdominal operation are readmitted for an adhesion-related complication (operative and nonoperative) and 12.0% have undergone repair of an incisional hernia. In contrast, laparoscopic procedures carry the lowest risk for late-onset laparotomy-related complications so the widespread adoption of laparoscopic techniques has likely led to a marked decrease in these types of complications. Finally, procedures performed outside of the peritoneum (RP/pelvic) also have little risk of obstruction.
Our findings provide estimates for a broader range of operations than previously reported in the literature. The Surgical and Clinical Adhesions Research Study, a large retrospective study using the Scottish National Health Service Database, found that during a 10-year period, 5.7% of all readmissions in patients who underwent open abdominal and pelvic operations were “directly” related to postoperative adhesions and that 38.6% of all readmissions were “possibly” related to postoperative adhesions.7 These findings suggest that our overall complication rate of 25.0% for major procedures might be an underestimate, as some patients admitted with diagnoses of abdominal pain, nausea, and vomiting without a diagnosis code for obstruction might have postoperative adhesions as the cause of their symptoms. In contrast, however, we found that operative intervention to relieve an obstruction due to adhesions at 5 years was required in 8.8% of patients undergoing a major abdominal operation, which is more than double the 10-year rate of 3.8% seen in the Surgical and Clinical Adhesions Research study and the 3.3% rate reported by Menzies and Ellis during a 25-year follow-up period.1 However, these studies included patients undergoing minor abdominal operations and pelvic operations, limiting direct comparison with our results and highlighting the importance of examining operations by their degree of invasiveness.
Persons undergoing laparascopic operations were found to have a low risk for late-onset laparotomy-related complications in our study. Previous studies examining the risk of complications after laparoscopic surgery have been limited to comparisons with their open counterpart and have produced mixed results. Some suggest that the laparoscopic approach is associated with a lower risk of complications and others have shown no difference.12,13 For instance, the CLASICC (Conventional versus Laparoscopic-Assisted Surgery in Colorectal Cancer) trial,14 comparing laparoscopically assisted with open colorectal surgery, found no difference in intestinal obstruction (2.0% vs 2.3%) or incisional hernia (7.4% vs 8.6%) at 3 years. In contrast, Rosin and colleagues,15 in a study of 306 laparoscopic colon and rectal procedures (there was no open surgical cohort), found a 1.3% rate of postoperative bowel obstruction during 8 years, which is much less than the 5-year rate of 10.7% after laparoscopic operations in our study. Our study examined all laparoscopic procedures and shows that when compared with major abdominal operations, laparoscopic procedures have a substantially lower risk for postoperative adhesion and incisional hernia-related complications. As laparoscopic techniques continue to evolve, this can affect the decision-making process of surgeons.
We also found a high rate of incisional hernia repairs after major abdominal operations at 5 years (12.0%), consistent with earlier studies that have shown the development of incisional hernias after abdominal operations to be between 11% and 20%.3,4 Mudge and Hughes, during a 10-year period, found that incisional hernias developed in 11% (62 of 564) of patients undergoing major abdominal operations and that 1.8% (10 of 564) underwent incisional hernia repair. Our results are likely indicative of the most clinically significant hernias because we only identified patients who underwent repair of their incisional hernias. Many ventral incisional hernias go unrepaired because they are asymptomatic and/or the risks of repair outweigh the benefits. One potential confounder that can affect our incisional hernia results is that patients with AAA might be at an increased risk for postoperative incisional hernias when compared with patients without AAA,16 although the low rate of incisional hernias in our control group argues against this.
The strengths of the 100% Medicare sample are its large size, longitudinal design, and broad representation of the elderly US population. However, there are several limitations to our study. First, administrative data are subject to coding errors. We attempted to limit the effect of these problems by using physician and hospital codes rather than hospital codes only. Second, several of the hernia repair codes are stated to be for “incisional or ventral” hernias and are not specific. We chose to treat the code as a complication for incisional hernia repair if it occurred during the follow-up period. Third, we required a 2-year clean period to limit the impact of pre-existing adhesions for the control group, but we lacked data on operations that occurred before this period. The rate of complications we observe in the control population likely reflects some operations that happened before the clean period. Finally, we studied a pre-existing cohort of patients who had undergone EVAR. Because EVAR is confined to the vascular system, there is no reason to expect that these would result in any increased risk of the complications we studied. As stated earlier, patients with AAA might be at an increased risk for developing incisional hernias after surgery, potentially limiting generalizability of our results to the general elderly population.
CONCLUSIONS
Late-onset laparotomy-related complications are frequent and their risk extends well beyond the perioperative period. The risk of late-onset complications is highest in patients undergoing major abdominal operations, and laparoscopic operations have the lowest risk of complications. These late risks need to be discussed with the patient to truly achieve informed consent. In addition, with the advancement and expansion of laparoscopic techniques and their attendant lower risk for long-term complications, these results might alter the risk-to-benefit profile of various types of abdominal operations and also strengthen the rationale for additional development of laparoscopic approaches to abdominal operations.
Acknowledgments
This work was supported by the NIH T32 Harvard-Longwood Research Training in Vascular Surgery grant HL007734 and NIH grant 1RC4MH092717-01 for comparative effectiveness research.
Abbreviations and Acronyms
- AAA
abdominal aortic aneurysm
- EVAR
endovascular repair
- LAP
laparotomy
- RP
retroperitoneum
Appendix
The Current Procedural Terminology codes used to identify all laparoscopic and open operations involving the abdomen, pelvis, and retroperitoneum and the 5 laparotomy groups they were categorized into: major abdominal operations, minor abdominal operations, abdominal wall hernia repairs, retroperitoneal/pelvic operations, and laparoscopic operations
| CPT | Description of procedure |
|---|---|
| Major abdominal operations | |
| 20102 | Exploration of penetrating wound; abdomen/flank/back |
| 43107 | Total esophagectomy; with pharyngogastrostomy or cervical esophagogastrostomy (transhiatal) |
| 43108 | with colon interposition or small intestine reconstruction |
| 43112 | Total esophagectomy, with thoracotomy; with pharyngogastrostomy or cervical esophagogastrostomy |
| 43113 | with colon interposition or small intestine reconstruction |
| 43116 | Partial esophagectomy, cervical, with free intestinal graft, microvascular anastomosis and intestinal reconstruction |
| 43117 | Partial esophagectomy, distal two thirds, with or without proximal gastrectomy (Ivor Lewis) |
| 43118 | with colon interposition or small intestine reconstruction |
| 43121 | Partial esophagectomy, distal two thirds, with thoracotomy only |
| 43122 | Partial esophagectomy, thoracoabdominal or abdominal approach |
| 43123 | with colon interposition or small intestine reconstruction |
| 43320 | Esophagogastrostomy (cardioplasty), with or without vagotomy and pyloroplasty |
| 43324 | Esophagogastric fundoplasty (eg, Nissen, Belsey IV, Hill procedures) |
| 43325 | Esophagogastric fundoplasty; with fundic patch (Thal-Nissen procedure) |
| 43326 | with gastroplasty (eg, Collis) |
| 43340 | Esophagojejunostomy (without total gastrectomy); abdominal approach |
| 43360 | Gastrointestinal reconstruction for previous esophagectomy; with stomach, with or without pyloroplasty |
| 43361 | with colon interposition or small intestine reconstruction |
| 43400 | Ligation, direct, esophageal varices |
| 43401 | Transection of esophagus with repair, for esophageal varices |
| 43405 | Ligation or stapling at gastroesophageal junction for pre-existing esophageal perforation |
| 43415 | Suture of esophageal wound or injury; transthoracic or transabdominal approach |
| 43425 | Closure of esophagostomy or fistula; transthoracic or transabdominal approach |
| 43496 | Free jejunum transfer with microvascular anastomosis |
| 43620 | Gastrectomy, total; with esophagogastrostomy |
| 43621 | with Roux-en-Y reconstruction |
| 43622 | with formation of intestinal pouch, any type |
| 43631 | Gastrectomy, partial, distal; with gastroduodenostomy |
| 43632 | with gastrojejunostomy |
| 43633 | with Roux-en-Y reconstruction |
| 43634 | with formation of intestinal pouch |
| 43635 | Vagotomy when performed with partial distal gastrectomy |
| 43640 | Vagotomy including pyloroplasty, with or without gastrostomy; truncal or selective |
| 43641 | parietal cell (highly selective) |
| 43810 | Gastroduodenostomy |
| 43820 | Gastrojejunostomy; without vagotomy |
| 43825 | with vagotomy, any type |
| 43842 | Gastric restrictive procedure, without gastric bypass, for morbid obesity; vertical banded gastroplasty |
| 43843 | other than vertical-bounded gastroplasty |
| 43845 | Gastric restrictive procedure with partial gastrectomy, pylorus-preserving duodenoileostomy and ileoileostomy |
| 43846 | Gastric restrictive procedure, with gastric bypass for morbid obesity; with short limb Roux-en-Y gastroenterostomy |
| 43847 | with small intestine reconstruction to limit absorption |
| 43848 | Revision, open, of gastric restrictive procedure for morbid obesity, other than adjustable gastric restrictive device |
| 43850 | Revision of gastroduodenal anastomosis (gastrojejunostomy) with reconstruction; without vagotomy |
| 43855 | with vagotomy |
| 43860 | Revision of gastrojejunal anastomosis, with or without partial gastrectomy or intestine resection; without vagotomy |
| 43865 | with vagotomy |
| 43880 | Closure of gastrocolic fistula |
| 44005 | Enterolysis (freeing of intestinal adhesion) |
| 44010 | Duodenotomy, for exploration, biopsy(s), or foreign body removal |
| 44015 | Tube or needle catheter jejunostomy for enteral alimentation, intraoperative, any method |
| 44020 | Enterotomy, small intestine, other than duodenum; for exploration, biopsy(s), or foreign body removal |
| 44021 | for decompression (eg, Baker tube) |
| 44025 | Colotomy, for exploration, biopsy(s), or foreign body removal |
| 44050 | Reduction of volvulus, intussusception, internal hernia, by laparotomy |
| 44055 | Correction of malrotation by lysis of duodenal bands and/or reduction of midget volvulus (eg, Ladd procedure) |
| 44110 | Excision of one or more lesions of small or large intestine not requiring anastomosis; single enterotomy |
| 44111 | multiple enterotomies |
| 44120 | Enterectomy, resection of small intestine; single resection and anastomosis |
| 44121 | each additional resection and anastomosis |
| 44125 | with enterostomy |
| 44126 | Enterectomy, resection of small intestine for congenital atresia, single resection and anastomosis; without tapering |
| 44127 | with tapering |
| 44128 | each additional resection and anastomosis |
| 44130 | Enteroenterostomy, anastomosis of intestine, with or without cutaneous enterostomy |
| 44133 | Donor enterectomy, open; partial, from living donor |
| 44135 | Intestinal allotransplantation; from a cadaver donor |
| 44136 | from living donor |
| 44137 | Removal of transplanted intestinal allograft, complete |
| 44139 | Mobilization (take-down) of splenic flexure performed in conjunction with partial colectomy |
| 44140 | Colectomy, partial; with anastomosis |
| 44141 | with skin-level cecostomy or colostomy |
| 44143 | with end colostomy and closure of distal segment (Hartmann-type procedure) |
| 44144 | with resection, with colostomy or ileostomy and creation of mucofistula |
| 44145 | with coloproctostomy (low pelvic anastomosis) |
| 44146 | with coloproctostomy (low pelvic anastomosis); with colostomy |
| 44147 | abdominal and transanal approach |
| 44150 | Colectomy, total, abdominal, without proctectomy; with ileostomy or ileoproctostomy |
| 44151 | with continent ileostomy |
| 44155 | Colectomy, total, abdominal, with proctectomy; with ileostomy |
| 44156 | with continent ileostomy |
| 44157 | with ileoanal anastomosis, includes loop ileostomy, and rectal mucosectomy, when performed |
| 44158 | with ileoanal anastomosis, creation of ileal reservoir (S or J), includes loop ileostomy, and rectal mucosectomy |
| 44160 | Colectomy, partial, with removal or terminal ileum with ileocolostomy |
| 44314 | Revision of ileostomy; complicated (reconstruction in-depth) |
| 44345 | Revision of colostomy; complicated (reconstruction in-depth) |
| 44602 | Suture of small intestine (enterorrhaphy) for perforated ulcer, diverticulum, wound, injury or rupture; single perforation |
| 44603 | multiple perforations |
| 44604 | Suture of large intestine (colorrhaphy) for perforated ulcer, diverticulum, wound, injury or rupture; without colostomy |
| 44605 | with colostomy |
| 44615 | Intestinal stricturoplasty (enterotomy and enterorrhaphy) with or without dilation, for intestinal obstruction |
| 44620 | Closure of enterostomy, large or small intestine |
| 44625 | with resection and anastomosis other than colorectal |
| 44626 | with resection and colorectal anastomosis (eg, closure of Hartmann-type procedure) |
| 44640 | Closure of intestinal cutaneous fistula |
| 44650 | Closure of enteroenteric or enterocolic fistula |
| 44660 | Closure of enterovesical fistula; without intestinal or bladder resection |
| 44661 | with intestine and/or bladder resection |
| 44680 | Intestinal plication |
| 44700 | Exclusion of small intestine from pelvis by mesh or other prosthesis, or native tissue (eg, bladder or omentum) |
| 44701 | Intraoperative colonic lavage |
| 44799 | Unlisted procedure, intestine |
| 45110 | Proctectomy; complete, combined abdominoperineal, with colostomy |
| 45111 | Proctectomy; partial resection of rectum, transabdominal approach |
| 45112 | Proctectomy, combined abdominoperineal pull-through procedure (eg, colo-anal anastomosis) |
| 45113 | Proctectomy, partial, with rectal mucosectomy, ileoanal anastomosis, creation of ileal reservoir (S or J) |
| 45114 | Proctectomy, partial, with anastomosis; abdominal and transsacral approach |
| 45119 | Proctectomy, combined abdominoperineal pull-through procedure, with creation of colonic reservoir (eg, J pouch) |
| 45120 | Proctectomy, complete, abdominal and perineal approach; with pull through procedure and anastomosis |
| 45121 | with subtotal or total colectomy, with multiple biopsies |
| 45123 | Proctectomy, partial, without anastomosis, perineal approach |
| 45126 | Pelvic exenteration for colorectal malignancy, with proctectomy (with or without colostomy) |
| 45135 | Excision of rectal procidentia, with anastomosis; abdominal and perineal approach |
| 45136 | Excision of ileoanal reservoir with ileostomy |
| 45540 | Proctopexy (eg, for prolapse); abdominal approach |
| 45550 | with sigmoid resection, abdominal approach |
| 45560 | Repair of rectocele |
| 45562 | Exploration, repair, and presacral drainage for rectal injury |
| 45563 | with colostomy |
| 45800 | Closure of rectovesical fistula |
| 45805 | with colostomy |
| 45820 | Closure of rectourethral fistula |
| 45825 | with colostomy |
| 46712 | Repair of ileoanal pouch fistula/sinus, pouch advancement; combined transperineal and transabdominal approach |
| 46735 | Repair of high imperforate anus without fistula; combined transabdominal and sacroperineal approaches |
| 46742 | Repair of high imperforate anus with rectourethral or rectovaginal fistula; combined transabdominal and sacroperineal |
| 46746 | Repair of cloacal anomaly by anorectovaginoplasty and urethroplasty, combined abdominal and sacroperineal |
| 46748 | with vaginal lengthening by intestinal graft or pedicle flaps |
| 47010 | Hepatotomy; open for drainage of abscess or cyst, 1 or 2 stages |
| 47011 | for percutaneous drainage of abscess or cyst, 1 or 2 stages |
| 47015 | Laparotomy, with aspiration and/or injection of hepatic parasitic (eg, amoebic or echinococcal) cyst(s) or abscess(es) |
| 47120 | Hepatectomy, resection of liver, partial lobectomy |
| 47122 | trisegmentectomy |
| 47125 | total left lobectomy |
| 47130 | total right lobectomy |
| 47135 | Live allotransplantation; orthotopic, partial or whole, from cadaver or living donor, any age |
| 47136 | heterotopic, partial or whole, from cadaver or living donor, any age |
| 47140 | Donor hepatectomy (including cold preservation), from living donor; left lateral segment only (segments II and III) |
| 47141 | total left lobectomy (segments II, II, and IV) |
| 47142 | total right lobectomy (segments V, VI, VII, and VIII) |
| 47300 | Marsupialization of cyst or abscess of liver |
| 47350 | Management of liver hemorrhage; simple suture of liver wound or injury |
| 47360 | complex suture of liver wound or injury, with or without hepatic artery ligation |
| 47361 | exploration of hepatic wound, extensive debridement, coagulation and/or suture, with or without packing of liver |
| 47362 | re-exploration of hepatic wound for removal of packing |
| 47400 | Hepaticotomy or hepaticostomy with exploration, drainage or removal of calculus |
| 47420 | Choledochotomy or choledochostomy with exploration, drainage, or removal or calculus |
| 47425 | with transduodenal sphincterotomy or sphincteroplasty |
| 47460 | Transduodenal sphincterotomy or sphincteroplasty, with or without transduodenal extraction of calculus |
| 47480 | Cholecystotomy or cholecystostomy with exploration, drainage, or removal of calculus |
| 47600 | Percutaneous cholecystostomy |
| 47605 | Cholecystectomy; with cholangiography |
| 47610 | Cholecystectomy with exploration of common duct |
| 47612 | with choledochoenterostomy |
| 47620 | with transduodenal sphincterotomy or sphincteroplasty, with or without cholangiography |
| 47700 | Exploration for congenital atresia of bile ducts, without repair, with or without liver biopsy |
| 47701 | Portoenterostomy (eg, Kasai procedure) |
| 47711 | Excision of bile duct tumor, with or without primary repair of bile duct; extrahepatic |
| 47712 | intrahepatic |
| 47715 | Excision of choledochal cyst |
| 47720 | Cholecystoenterostomy; direct |
| 47721 | with gastroenterostomy |
| 47740 | Roux-en-Y |
| 47741 | Roux-en-Y with gastroenterostomy |
| 47760 | Anastomosis, of extrahepatic biliary ducts and gastrointestinal tract |
| 47765 | Anastomosis, on intrahepatic ducts and gastrointestinal tract |
| 47780 | Anastomosis, Roux-en-Y, of extrahepatic biliary ducts and gastrointestinal tract |
| 47785 | Anastomosis, Roux-en-Y, of intrahepatic biliary ducts and gastrointestinal tract |
| 47800 | Reconstruction, plastic, of extrahepatic biliary ducts with end-to-end anastomosis |
| 47801 | Placement of choledochal stent |
| 47802 | U-tube hepaticoenterostomy |
| 47900 | Suture of extrahepatic biliary duct for pre-existing injury |
| 48000 | Placement of drains, peripancreatic, for acute pancreatitis |
| 48001 | with cholecystostomy, gastrostomy and jejunostomy |
| 48020 | Removal of pancreatic calculus |
| 48100 | Biopsy of pancreas, open (eg, fine-needle aspiration, needle core biopsy, wedge biopsy) |
| 48105 | Resection or debridement of pancreas and peripancreatic tissue for acute necrotizing pancreatitis |
| 48120 | Excision of lesion of pancreas (eg, cyst, adenoma) |
| 48140 | Pancreatectomy, distal subtotal, with or without splenectomy; without pancreaticojejunostomy |
| 48145 | with pancreaticojejunostomy |
| 48146 | Pancreatectomy, distal, near-total with preservation of duodenum (Child-type procedure) |
| 48148 | Excision of ampulla of Vater |
| 48150 | Pancreatectomy (Whipple-type procedure); with pancreatojejunostomy |
| 48152 | without pancreatojejunostomy |
| 48153 | Pancreatectomy (pylorus-spearing, Whipple-type procedure); with pancreatojejunostomy |
| 48154 | without pancreatojejunostomy |
| 48155 | Pancreatectomy, total |
| 48160 | Pancreatectomy, total or subtotal, with autologous transplantation of pancreas or pancreatic islet cells |
| 48500 | Marsupialization of pancreatic cyst |
| 48510 | External drainage, pseudocyst of pancreas; open |
| 48520 | Internal anastomosis of pancreatic cyst to gastrointestinal tract; direct |
| 48540 | Roux-en-Y |
| 48545 | Pancreatorrhaphy for injury |
| 48547 | Duodenal exclusion with gastrojejunostomy for pancreatic injury |
| 48548 | Pancreaticojejunostomy, side to side anastomosis (Puestow-type operation) |
| 48554 | Transplantation of pancreatic allograft |
| 48556 | Removal of transplanted pancreatic allograft |
| 48999 | Unlisted procedure, pancreas |
| 49000 | Exploratory laparotomy, with or without biopsy(s) |
| 49002 | Reopening of recent laparotomy |
| 49010 | Exploration, retroperitoneal area with or without biopsy(s) |
| 49020 | Drainage of peritoneal abscess or localized peritonitis, exclusive of appendiceal abscess; open |
| 49040 | Drainage of subdiaphragmatic or subphrenic abscess; open |
| 49060 | Drainage of retroperitoneal abscess; open |
| 49062 | Drainage of extraperitoneal lymphocele to peritoneal cavity; open |
| 49203 | Excision or destruction, open, intra-abdominal tumors; largest tumor 5 cm diameter |
| 49204 | largest tumor 5.1 to 10.0 cm diameter |
| 49205 | largest tumor >10.0 cm diameter |
| 49220 | Staging laparotomy for Hodgkins disease or lymphoma |
| 49402 | Removal or peritoneal foreign body from peritoneal cavity |
| 50660 | Ureterectomy, total, ectopic ureter, combination abdominal, vaginal, and/or perineal approach |
| 50800 | Ureteroenterostomy, direct anastomosis of ureter to intestine |
| 50810 | Ureterosigmoidostomy, with creation of sigmoid bladder and establishment of abdominal or perineal colostomy |
| 50815 | Uretercolon conduit, including intestine anastomosis |
| 50820 | Ureteroileal conduit (ileal bladder), including intestine anastomosis (Bricker operation) |
| 50825 | Continent diversion, including intestine anastomosis using any segment of small and/or large intestine |
| 50830 | Urinary diversion (eg, taking down of ureteroileal conduit, ureterosigmoidostomy or ureteroneocystostomy) |
| 50840 | Replacement of all or part of ureter by intestine segment, including intestine anastomosis |
| 50860 | Ureterostomy, transplantation of ureter to skin |
| 50900 | Ureterohhaphy, suture of ureter |
| 50920 | Closure of ureterocutaneous fistula |
| 50930 | Closure of ureterovisceral fistula (including visceral repair) |
| 50940 | Delegation of ureter |
| 51570 | Cystectomy, complete |
| 51575 | with bilateral pelvic lymphadenectomy, including external iliac, hypogastric, and obturator nodes |
| 51580 | Cystectomy, complete, with ureterosigmoidostomy or ureterocutaneous transplantations |
| 51585 | with bilateral pelvic lymphadenectomy, including external iliac, hypogastric, and obturator nodes |
| 51590 | Cystectomy, complete, with ureteroileal conduit or sigmoid bladder, including intestine anastomosis |
| 51595 | with bilateral pelvic lymphadenectomy, including external iliac, hypogastric, and obturator nodes |
| 51596 | Cystectomy, complete, with continent diversion, using segment of small and/or large intestine to construct neobladder |
| 51597 | Pelvic exenteration, complete, for vesical, prostatic or urethral malignancy |
| 54535 | Orchiectomy, radical, for tumor; with abdominal exploration |
| 54560 | Exploration for undescended testis with abdominal exploration |
| 55535 | Excision of varicocele or ligation of spermatic veins for varicocele; abdominal approach |
| 55540 | with hernia repair |
| 57305 | Closure of rectovaginal fistula; abdominal approach |
| 57307 | abdominal approach, with concomitant colostomy |
| 58240 | Pelvic exenteration for gynecologic malignancy |
| 58960 | Laparotomy, for staging or restaging of ovarian, tubal, or primary peritoneal malignancy (second look) |
| Minor abdominal operations | |
| 43101 | Excision of lesion, esophagus; thoracic or abdominal approach |
| 43246 | Upper gastrointestinal endoscopy with directional placement of percutaneous gastrostomy tube |
| 43330 | Esophagomyotomy (Heller-type); abdominal approach |
| 43350 | Esophagomyotomy, fistulization of esophagus, external; abdominal approach |
| 43500 | Gastrostomy; with exploration or foreign body removal |
| 43501 | Gastrostomy; with suture repair of bleeding ulcer |
| 43502 | Gastrostomy; with suture repair of pre-existing esophagogastric laceration (eg, Mallory-Weiss) |
| 43510 | Gastrostomy; with esophageal dilation and insertion of permanent intraluminal tube |
| 43520 | Pyloromyotomy, cutting of pyloric muscle (Fredet-Ramstedtetype operation) |
| 43605 | Biopsy of stomach; by laparotomy |
| 43610 | Excision, local; ulcer or benign tumor of stomach |
| 43611 | Excision, local; malignant tumor of stomach |
| 43800 | Pyloroplasty |
| 43830 | Gastrostomy, open; without construction of gastric tube (eg, Stamm procedure) |
| 43832 | Gastrostomy, open; with constriction of gastric tube (eg, Janeway procedure) |
| 43840 | Gastrorrhaphy, suture of perforated duodenal or gastric ulcer, wound, or injury |
| 43870 | Closure of gastrostomy, surgical |
| 43881 | Implantation or replacement of gastric neurostimulator electrodes, antrum, open |
| 43882 | Revision or removal of gastric neurostimulator electrodes, antrum, open |
| 44300 | Placement, enterostomy or cecostomy, tube open (eg, for feeding or decompression) |
| 44310 | Ileostomy or jejunostomy, non-tube |
| 44312 | Revision of ileostomy; simple (release of superficial scar) |
| 44316 | Continent ileostomy (Kock procedure) |
| 44320 | Colostomy or skin level cecostomy |
| 44322 | Colostomy or skin level cecostomy; with multiple biopsies (eg, for congenital megacolon) |
| 44340 | Revision of colostomy; simple (release of superficial scar) |
| 44346 | Revision of colostomy; with repair of paracolostomy hernia |
| 44800 | Excision of Meckel’s diverticulum (diverticulectomy) or omphalomesenteric duct |
| 44820 | Excision of lesion of mesentery |
| 44850 | Suture of mesentery |
| 44899 | Unlisted procedure, Meckel’s diverticulum and the mesentery |
| 44900 | Incision and drainage of appendiceal abscess; open |
| 44950 | Appendectomy |
| 44955 | Appendectomy; when done for indicated purpose at time of other major procedure |
| 44960 | Appendectomy; for ruptured appendix with abscess or generalized peritonitis |
| 47100 | Biopsy of liver, wedge |
| 47380 | Ablation, open, of one or more liver tumor(s); radiofrequency |
| 47381 | Ablation, open, of one or more liver tumor(s); cryosurgical |
| 47382 | Ablation, one or more liver tumor(s), percutaneous, radiofrequency |
| 49250 | Umbilectomy, omphalectomy, excision of umbilicus |
| 49255 | Omentectomy, epiploectomy, resection of omentum |
| 49419 | Insertion of intraperitoneal cannula or catheter, with subcutaneous reservoir, permanent |
| 49420 | Insertion of intraperitoneal cannula or catheter for drainage or dialysis; temporary |
| 49421 | Insertion of intraperitoneal cannula or catheter for drainage or dialysis; permanent |
| 49422 | Removal of permanent intraperitoneal cannula or catheter |
| 49423 | Exchange of previously placed abscess or cyst drainage catheter under radiological guidance |
| 49425 | Insertion of peritoneal-venous shunt |
| 49426 | Revision of peritoneal-venous shunt |
| 49428 | Ligation of peritoneal-venous shunt |
| 49429 | Removal of peritoneal-venous shunt |
| 49435 | Insertion of subcutaneous extension to intraperitoneal cannula or catheter with remote chest exit site |
| 49436 | Delayed creation of exit site from embedded subcutaneous segment of intraperitoneal cannula or catheter |
| 49440 | Insertion of gastrostomy tube, percutaneous, under fluoroscopic guidance |
| 49441 | Insertion of duodenostomy or jejunostomy tube, percutaneous, under fluoroscopic guidance |
| 49442 | Insertion of cecostomy or other colonic tube, percutaneous, under fluoroscopic guidance |
| 50845 | Cutaneous appendico-vesicostomy |
| 62223 | Creation of shunt; ventriculo-peritoneal, -pleural, other terminus |
| 62258 | Removal of complete cerebrospinal fluid shunt system; with replacement |
| 63303 | Vertebral corpectomy; extradural, lumbar or sacral by transperitoneal or retroperitoneal approach |
| 63307 | Vertebral corpectomy; intradural, lumbar or sacral by transperitoneal or retroperitoneal approach |
| 63740 | Creation of shunt, lumbar, subarachnoid-peritoneal, -pleural, or other, including laminectomy |
| Abdominal wall hernia operations | |
| 49560 | Repair initial incisional or ventral hernia; reducible |
| 49561 | Repair initial incisional or ventral hernia; incarcerated or strangulated |
| 49565 | Repair recurrent incisional or ventral hernia; reducible |
| 49566 | Repair recurrent incisional or ventral hernia; incarcerated or strangulated |
| 49568 | Implantation of mesh for incisional or ventral hernia repair or for closure of debridement for necrotizing tissue infection |
| 49570 | Repair epigastric hernia; reducible |
| 49572 | Repair epigastric hernia; incarcerated or strangulated |
| 49580 | Repair umbilical hernia, younger than 5 years; reducible |
| 49582 | Repair umbilical hernia, younger than 5 years; incarcerated or strangulated |
| 49585 | Repair umbilical hernia, age 5 years or older; reducible |
| 49587 | Repair umbilical hernia, age 5 years or older; incarcerated or strangulated |
| 49590 | Repair spigelian hernia |
| 49600 | Repair of small omphalocele, with primary closure |
| 49605 | Repair of large omphalocele or gastroschisis; with or without prosthesis |
| 49606 | Repair of large omphalocele or gastroschisis; with removal of prosthesis, final reduction and closure |
| 49610 | Repair of omphalocele (Gross-type operation); first stage |
| 49611 | Repair of omphalocele (Gross-type operation); second stage |
| 49900 | Suture, secondary, of abdominal wall for evisceration or dehiscence |
| 49904 | Omental flap, extra-abdominal (eg, for reconstruction of sternal and chest wall defects) |
| 49905 | Omental flap, intra-abdominal |
| 49906 | Free omental flap with microvascular anastomosis |
| 49999 | Unlisted procedure, abdomen, peritoneum and omentum |
| Retroperitoneal/pelvic operations | |
| 50010 | Renal exploration, not necessitating other specific procedures |
| 50020 | Drainage of perirenal or renal abscess; open |
| 50040 | Nephrostomy, nephrotomy with drainage |
| 50045 | Nephrotomy, with exploration |
| 50060 | Nephrolithotomy; removal of calculus |
| 50065 | Nephrolithotomy; secondary surgical operation for calculus |
| 50070 | Nephrolithotomy; complicated by congenital kidney abnormality |
| 50075 | Nephrolithotomy; removal of large staghorn calculus filling renal pelvis and calyces |
| 50100 | Transection of repositioning of aberrant renal vessels |
| 50120 | Pyelotomy; with exploration |
| 50125 | Pyelotomy; with drainage, pyelostomy |
| 50130 | Pyelotomy; with removal of calculus (pyelolithotomy, pelviolithotomy, including coagulum pyelolithotomy) |
| 50135 | Pyelotomy; complicated (eg, secondary operation, congenital kidney abnormality) |
| 50205 | Renal biopsy by surgical exposure of kidney |
| 50220 | Nephrectomy; including partial ureterectomy, any open approach including rib resection |
| 50225 | Nephrectomy; complicated because of previous surgery on same kidney |
| 50230 | Nephrectomy; radical, with regional lymphadenectomy and/or vena cava thrombectomy |
| 50234 | Nephrectomy with total ureterectomy and bladder cuff; through same incision |
| 50236 | Nephrectomy with total ureterectomy and bladder cuff; through separate incision |
| 50240 | Nephrectomy, partial |
| 50250 | Ablation, open, one or more renal mass lesion(s), cryosurgical, including intraoperative ultrasound |
| 50280 | Excision or unroofing of cyst(s) of kidney |
| 50290 | Excision of perinephric cyst |
| 50320 | Donor nephrectomy; open, from liver donor |
| 50340 | Recipient nephrectomy |
| 50360 | Renal allotransplantation, implantation of graft; without recipient nephrectomy |
| 50365 | Renal allotransplantation, implantation of graft; with recipient nephrectomy |
| 50370 | Removal of transplanted renal allograft |
| 50380 | Renal autotransplantation, reimplantation of kidney |
| 50400 | Pyeloplasty (Foley Y-pyeloplasty), plastic operation on renal pelvis; simple |
| 50405 | Pyeloplasty (Foley Y-pyeloplasty), plastic operation on renal pelvis; complicated |
| 50500 | Nephrorrhaphy, suture of kidney wound or injury |
| 50520 | Closure of nephrocutaneous or pyelocutaneous fistula |
| 50525 | Closure of nephrovisceral fistula (eg, renocolic), including visceral repair; abdominal approach |
| 50540 | Symphysiotomy for horseshoe kidney with or without pyeloplasty, unilateral or bilateral (one operation) |
| 50600 | Ureterotomy with exploration or drainage |
| 50605 | Ureterotomy for insertion of indwelling stent, all types |
| 50650 | Ureterectomy, with bladder cuff |
| 50700 | Ureteroplasty, plastic operation on ureter (eg, stricture) |
| 50715 | Ureterolysis, with or without repositioning of ureter for retroperitoneal fibrosis |
| 50722 | Ureterolysis for ovarian vein syndrome |
| 50725 | Ureterolysis for retrocaval ureter, with reanastomosis of upper urinary tract or vena cava |
| 50727 | Revision of urinary-cutaneous anastomosis (any type urostomy); |
| 50728 | Revision of urinary-cutaneous anastomosis (any type urostomy); with repair of fascial defect and hernia |
| 50740 | Ureteropyelostomy, anastomosis of ureter and renal pelvis |
| 50750 | Ureterocalycostomy, anastomosis of ureter to renal calyx |
| 50760 | Ureteroureterostomy |
| 50770 | Transureteroureterostomy, anastomosis of ureter to contralateral ureter |
| 50780 | Ureteroneocystostomy; anastomosis of single ureter to bladder |
| 50782 | Ureteroneocystostomy; anastomosis of duplicated ureter to bladder |
| 50783 | Ureteroneocystostomy; with extensive ureteral tailoring |
| 50785 | Ureteroneocystostomy; with vesico-psoas hitch or bladder flap |
| 51020 | Cystotomy or cystostomy; with fulguration and/or insertion of radioactive material |
| 51030 | Cystotomy or cystostomy; with cryosurgical destruction of intravesical lesion |
| 51040 | Cystostomy, cystotomy with drainage |
| 51045 | Cystotomy, with intersection of ureteral catheter or stent |
| 51050 | Cystolithotomy, cystotomy with removal of calculus, without vesical neck resection |
| 51060 | Transvesical ureterolithotomy |
| 51065 | Cystotomy, with calculus basket extraction and/or ultrasonic or electrohydraulic fragmentation of ureteral calculus |
| 51080 | Drainage of perivesical or prevesical space abscess |
| 51500 | Excision of urachal cyst or sinus, with or without umbilical hernia repair |
| 51520 | Cystotomy; for simple excision of vesical neck |
| 51525 | Cystotomy; for excision of bladder diverticulum, single or multiple |
| 51530 | Cystotomy; for excision of bladder tumor |
| 51535 | Cystotomy for excision, incision, or repair of ureterocele |
| 51550 | Cystectomy, partial; simple |
| 51555 | Cystectomy, partial; complicated (eg, postradiation, previous surgery, difficult location) |
| 51565 | Cystectomy, partial, with reimplantation of ureter(s) into bladder (ureteroneocystostomy) |
| 51800 | Cystoplasty or cystourethroplasty, plastic operation on bladder and/or vesicle neck, any procedure vesical neck |
| 51820 | Cystourethroplasty with unilateral or bilateral ureteroneocystostomy |
| 51840 | Anterior vesicourethropexy, or urethropexy; simple |
| 51841 | Anterior vesicourethropexy, or urethropexy; complicated (eg, secondary repair) |
| 51845 | Abdomino-vaginal vesical neck suspension, with or without endoscopic control (eg, Stamey, Raz, modified Pereyra) |
| 51860 | Cystorrhaphy, suture of bladder wound, injury or rupture; simple |
| 51865 | Cystorrhaphy, suture of bladder wound, injury or rupture; complicated |
| 51880 | Closure of cystostomy |
| 51900 | Closure of vesicovaginal fistula, abdominal approach |
| 51920 | Closure of vesicouterine fistula |
| 51925 | Closure of vesicouterine fistula with hysterectomy |
| 51940 | Closure, exstrophy of bladder |
| 51960 | Enterocystoplasty, including intestinal anastomosis |
| 51980 | Cutaneous vesicostomy |
| 55821 | Prostatectomy; suprapubic, subtotal, 1 or 2 stages |
| 57540 | Excision of cervical stump, abdominal approach |
| 57545 | Excision of cervical stump, abdominal approach with pelvic floor repair |
| 58140 | Myomectomy, excision of fibroid tumor(s), 1 to 4 intramural myoma(s) with total weight 250 g |
| 58146 | Myomectomy, excision of fibroid tumor(s), 5 or more intramural myomas with total weight >250 g |
| 58150 | Total abdominal hysterectomy, with or without removal of tube(s), with or without removal of ovary(s) |
| 58152 | Total abdominal hysterectomy with colpo-urethrocystopexy (eg, Marshall-Marchetti, Krantz, Burch) |
| 58180 | Supracervical abdominal hysterectomy (subtotal), with or without removal tube(s), with or without removal of ovary(s) |
| 58200 | Total abdominal hysterectomy, including partial vaginectomy, with para-aortic and pelvic lymph node sampling |
| 58210 | Radical abdominal hysterectomy, with bilateral total pelvic lymphadenectomy and para-aortic lymph node sampling |
| 58400 | Uterine suspension, with or without shortening of round ligaments or sacrouterine ligaments |
| 58410 | Uterine suspension, with presacral sympathectomy |
| 58520 | Hysterorrhapy, repair of ruptured uterus (nonobstetrical) |
| 58540 | Hysteroplasty, repair of uterine anomaly (Strassman-type) |
| 58600 | Ligation or transection of fallopian tube(s), abdominal or vaginal approach, unilateral or bilateral |
| 58605 | Ligation or transection of fallopian tube(s), abdominal or vaginal approach, postpartum, unilateral or bilateral |
| 58611 | Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery |
| 58700 | Salpingectomy, complete or partial, unilateral or bilateral |
| 58720 | Salpingo-oophorectomy, complete or partial, unilateral or bilateral |
| 58740 | Lysis of adhesions (salpingolysis, ovariolysis) |
| 58750 | Tubotubal anastomosis |
| 58752 | Tubouterine implantation |
| 58760 | Fimbrioplasty |
| 58770 | Salpingostomy (salpingoneostomy) |
| 58805 | Drainage of ovarian cyst(s), unilateral or bilateral; abdominal approach |
| 58822 | Drainage of ovarian abscess; abdominal approach |
| 58825 | Transposition, ovary(s) |
| 58900 | Biopsy of ovary, unilateral or bilateral |
| 58920 | Wedge resection or bisection of ovary, unilateral or bilateral |
| 58925 | Ovarian cystectomy, unilateral or bilateral |
| 58940 | Oophorectomy, partial or total, unilateral or bilateral |
| 58943 | Oophorectomy, partial or total, unilateral or bilateral for ovarian, tubal or primary peritoneal malignancy |
| 58950 | Resection of ovarian, tubal or primary peritoneal malignancy with bilateral salpingo-oophorectomy and omentectomy |
| 58951 | with total abdominal hysterectomy |
| 58952 | with radical dissection for debulking |
| 58953 | Bilateral salpingo-oophorectomy with omentectomy, total abdominal hysterectomy and radical dissection for debulking |
| 58954 | with pelvic lymphadenectomy |
| 58956 | Bilateral salpingo-oophorectomy with total omentectomy, total abdominal hysterectomy for malignancy |
| 58957 | Resection (tumor debulking) of recurrent ovarian, tubal, primary peritoneal, uterine malignancy, with omentectomy |
| 58958 | with pelvic lyphadenectomy and limited para-aortic lyphadenectomy |
| 59100 | Hysterotomy, abdominal (eg, for hydatidiform mole, abortion) |
| 59120 | Surgical treatment of ectopic pregnancy; tubal or ovarian, requiring salpingectomy and/or oophorectomy |
| 59121 | Surgical treatment of ectopic pregnancy; tubal or ovarian, without salpingectomy and/or oophorectomy |
| 59130 | Surgical treatment of ectopic pregnancy; abdominal pregnancy |
| 59135 | Surgical treatment of ectopic pregnancy; interstitial, uterine pregnancy requiring total hysterectomy |
| 59136 | Surgical treatment of ectopic pregnancy; interstitial, uterine pregnancy with partial resection of uterus |
| 59325 | Cerclage of cervix, during pregnancy; abdominal |
| 59350 | Hysterorrhaphy of ruptured uterus |
| 59510 | Routine obstetric care including antepartum care, cesarean delivery, and postpartum care |
| 59514 | Cesarean delivery only |
| 59515 | Cesarean delivery only including postpartum care |
| 59525 | Subtotal or total hysterectomy after cesarean delivery |
| 59618 | Routine obstetric care including antepartum care and cesarean delivery after attempted vaginal delivery |
| 59620 | Cesarean delivery only, after attempted vaginal delivery after previous cesarean |
| 59622 | Cesarean delivery only, after attempted vaginal delivery after previous cesarean including postpartum care |
| 60540 | Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal |
| 60545 | with excision of adjacent retroperitoneal tumor |
| Laparoscopic operations | |
| 43280 | Esophagogastric fundoplasty (Nissen, Toupet) |
| 43289 | Unlisted procedure, esophagus |
| 43644 | Gastric restrictive procedure; with gastric bypass and Roux-en-Y gastroenterostomy |
| 43645 | Gastric restrictive procedure; with gastric bypass and small intestine reconstruction |
| 43647 | Implantation or replacement of gastric neurostimulator electrodes, antrum |
| 43648 | Revision or removal of gastric neurostimulator electrodes, antrum |
| 43651 | Transection of vagus nerves, truncal |
| 43652 | Transection of vagus nerves, selective or highly selective |
| 43653 | Gastrostomy, without construction of gastric tube (Stamm procedure) |
| 43659 | Unlisted procedure, stomach |
| 43770 | Gastric restrictive procedure; placement of adjustable gastric restrictive device |
| 43771 | Revision of adjustable gastric restrictive device component only |
| 43772 | Removal of adjustable gastric restrictive device component only |
| 43773 | Removal and replacement of adjustable gastric restrictive device component only |
| 43774 | Removal of adjustable gastric restrictive device and subcutaneous port components |
| 43775 | Gastric restrictive procedure; longitudinal gastrectomy (sleeve) |
| 44186 | Jejunostomy |
| 44187 | Ileostomy or jejunostomy, non-tube |
| 44188 | Colostomy or skin level cecostomy |
| 44202 | Enterectomy, resection of small intestine, single resection and anastomosis |
| 44203 | Each additional small intestine resection and anastomosis |
| 44204 | Colectomy, partial, with anastomosis |
| 44205 | Colectomy, partial, with removal of terminal ileum with ileocolostomy |
| 44206 | Colectomy, partial, with end colostomy and closure of distal segment (Hartmann) |
| 44207 | Colectomy, partial, with anastomosis, with coloproctostomy |
| 44208 | Colectomy, partial, with anastomosis, with coloproctostomy with colostomy |
| 44210 | Colectomy, total, abdominal, without proctectomy, with ileostomy or ileoproctostomy |
| 44211 | Colectomy, total, abdominal, with proctectomy, with ileoanal anastomosis, creation of ileal reservoir |
| 44212 | Colectomy, total, abdominal, with proctectomy, with ileostomy |
| 44213 | Mobilization of splenic flexure performed in conjunction with partial colectomy |
| 44227 | Closure of enterostomy, large or small intestine, with resection and anastomosis |
| 44238 | Unlisted procedure, intestine |
| 44970 | Appendectomy |
| 44979 | Unlisted procedure, appendix |
| 45395 | Proctectomy, complete, combined abdominoperineal, with colostomy |
| 45397 | Proctectomy, combined abdominoperineal pull-through procedure with creation of colonic reservoir |
| 45400 | Proctopexy |
| 45402 | Proctopexy, with sigmoid resection |
| 45499 | Unlisted procedure, rectum |
| 47370 | Ablation of one or more liver tumors; radiofrequency |
| 47371 | Cryosurgical |
| 47379 | Unlisted procedure, liver |
| 47562 | Cholecystectomy |
| 47563 | Cholecystectomy with cholangiography |
| 47564 | Cholecystectomy with exploration of common duct |
| 47570 | Cholecystoenterostomy |
| 47579 | Unlisted procedure, biliary tract |
| 49320 | Diagnostic, with or without collection of specimens by brushing or washing |
| 49321 | with biopsy |
| 49322 | with aspiration of cavity or cyst |
| 49323 | with drainage of lymphocele to peritoneal cavity |
| 49324 | with insertion of intraperitoneal cannula or catheter, permanent |
| 49325 | with revision of previously placed intraperitoneal cannula or catheter |
| 49326 | with omentopexy |
| 49329 | Unlisted procedure, abdomen, peritoneum, and omentum |
| 49650 | Repair initial inguinal hernia |
| 49651 | Repair recurrent inguinal hernia |
| 49652 | Repair ventral, umbilical, spigelian or epigastric hernia; reducible |
| 49653 | Repair ventral, umbilical, spigelian or epigastric hernia; incarcerated or strangulated |
| 49659 | Unlisted procedure, hernioplasty, herniorrhaphy, herniotomy |
| 50541 | Ablation of renal cysts |
| 50542 | Ablation of renal mass lesion |
| 50543 | Partial nephrectomy |
| 50544 | Pyeloplasty |
| 50545 | Radical nephrectomy |
| 50546 | Nephrectomy, including partial ureterectomy |
| 50547 | Donor nephrectomy, from living donor |
| 50548 | Nephrectomy with total ureterectomy |
| 50549 | Unlisted procedure, renal |
| 51990 | Urethral suspension for stress incontinence |
| 51992 | Sling operation for stress incontinence |
| 51999 | Unlisted procedure, bladder |
| 54692 | Orchiopexy for intra-abdominal testis |
| 55550 | Ligation of spermatic veins for varicocele |
| 55559 | Unlisted procedure, spermatic cord |
| 58541 | Supracervical hysterectomy |
| 58542 | with removal of tubes and/or ovary |
| 58543 | Supracervical hysterectomy |
| 58544 | with removal of tubes and/or ovary |
| 58545 | Myomectomy; 1 to 4 intramural myomas |
| 58546 | 5 or more intramural myomas |
| 58548 | Radical hysterectomy, with bilateral total pelvic lymphadenectomy and para-aortic lymph node sampling |
| 58550 | with vaginal hysterectomy |
| 58552 | with removal of tubes and/or ovary |
| 58553 | with vaginal hysterectomy |
| 58554 | with removal of tubes and/or ovary |
| 58570 | Total hysterectomy |
| 58571 | with removal of tubes and/or ovary |
| 58572 | Total hysterectomy |
| 58573 | with removal of tubes and/or ovary |
| 58578 | Unlisted procedure, uterus |
| 58660 | Lysis of adhesions (salpingolysis, ovariolysis) |
| 58661 | with removal of adnexal structures |
| 58662 | with fulguration or excision of lesions of the ovary, pelvic viscera, or peritoneal surface |
| 58670 | with fulguration of oviducts |
| 58671 | with occlusion of oviducts by device |
| 58672 | with fimbrioplasty |
| 58673 | with salpingostomy |
| 58679 | Unlisted procedure, oviduct, ovary |
| 59150 | Treatment of ectopic pregnancy; without salpingectomy and/or oophorectomy |
| 59151 | with salpingectomy and/or oophorectomy |
| 60650 | Adrenalectomy, partial or complete, or exploration of adrenal gland |
Footnotes
Disclosure Information: Marc L Schermerhorn is a consultant for Boston Scientific, Endologix, and Medtronic. All other authors have nothing to disclose.
The opinions expressed do not necessarily represent the views or policy positions of the Centers for Medicare and Medicaid Services.
Author Contributions
Study conception and design: Bensley, Schermerhorn, O’Malley, Cotterill, Landon
Acquisition of data: Cotterill
Analysis and interpretation of data: Bensley, Schermerhorn, Hurks, Sachs, Boyd, O’Malley, Cotterill, Landon
Drafting of manuscript: Bensley, Schermerhorn, Hurks, Sachs, Boyd, O’Malley, Cotterill, Landon
Critical revision: Bensley, Schermerhorn, Hurks, Sachs, Boyd, O’Malley, Cotterill, Landon
Contributor Information
Rodney P Bensley, Department of Surgery, Beth Israel Deaconess Medical Center, Boston, MA.
Marc L Schermerhorn, Department of Surgery, Beth Israel Deaconess Medical Center, Boston, MA.
Rob Hurks, Department of Surgery, Beth Israel Deaconess Medical Center, Boston, MA.
Teviah Sachs, Department of Surgery, Beth Israel Deaconess Medical Center, Boston, MA.
Christopher A Boyd, Department of Surgery, Beth Israel Deaconess Medical Center, Boston, MA.
A James O’Malley, Department of Health Care Policy, Harvard Medical School, Boston, MA.
Philip Cotterill, Centers for Medicare and Medicaid Services, Baltimore, MD.
Bruce E Landon, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, MA; Department of Health Care Policy, Harvard Medical School, Boston, MA.
References
- 1.Menzies D, Ellis H. Intestinal obstruction from adhesions— how big is the problem? Ann R Coll Surg Engl. 1990;72:60–63. [PMC free article] [PubMed] [Google Scholar]
- 2.Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, et al. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg. 2000;87:467–471. doi: 10.1046/j.1365-2168.2000.01394.x. [DOI] [PubMed] [Google Scholar]
- 3.Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72:70–71. doi: 10.1002/bjs.1800720127. [DOI] [PubMed] [Google Scholar]
- 4.Sugerman HJ, Kellum JM, Reines HD, et al. Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg. 1996;171:80–84. doi: 10.1016/S0002-9610(99)80078-6. [DOI] [PubMed] [Google Scholar]
- 5.Anthony T, Bergen PC, Kim LT, et al. Factors affecting recurrence following incisional herniorrhaphy. World J Surg. 2000;24:95–100. doi: 10.1007/s002689910018. [DOI] [PubMed] [Google Scholar]
- 6.Flum DR, Horvath K, Koepsell T. Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg. 2003;237:129–135. doi: 10.1097/00000658-200301000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353:1476–1480. doi: 10.1016/S0140-6736(98)09337-4. [DOI] [PubMed] [Google Scholar]
- 8.Giles KA, Landon BE, Cotterill P, et al. Thirty-day mortality and late survival with reinterventions and readmissions after open and endovascular aortic aneurysm repair in Medicare beneficiaries. J Vasc Surg. 2011;53:6–12. doi: 10.1016/j.jvs.2010.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schermerhorn ML, O’Malley AJ, Jhaveri A, et al. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008;358:464–474. doi: 10.1056/NEJMoa0707348. [DOI] [PubMed] [Google Scholar]
- 10.Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J (Clin Res Ed) 1982;284:931–933. doi: 10.1136/bmj.284.6320.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollock AV, Evans M. Early prediction of late incisional hernias. Br J Surg. 1989;76:953–954. doi: 10.1002/bjs.1800760926. [DOI] [PubMed] [Google Scholar]
- 12.Scholin J, Buunen M, Hop W, et al. Bowel obstruction after laparoscopic and open colon resection for cancer: results of 5 years of follow-up in a randomized trial. Surg Endosc. 2011;25:3755–3760. doi: 10.1007/s00464-011-1782-2. [DOI] [PubMed] [Google Scholar]
- 13.Andersen LP, Klein M, Gogenur I, et al. Incisional hernia after open versus laparoscopic sigmoid resection. Surg Endosc. 2008;22:2026–2029. doi: 10.1007/s00464-008-9924-x. [DOI] [PubMed] [Google Scholar]
- 14.Taylor GW, Jayne DG, Brown SR, et al. Adhesions and incisional hernias following laparoscopic versus open surgery for colorectal cancer in the CLASICC trial. Br J Surg. 2010;97:70–78. doi: 10.1002/bjs.6742. [DOI] [PubMed] [Google Scholar]
- 15.Rosin D, Zmora O, Hoffman A, et al. Low incidence of adhesion-related bowel obstruction after laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech A. 2007;17:604–607. doi: 10.1089/lap.2006.0002. [DOI] [PubMed] [Google Scholar]
- 16.Takagi H, Sugimoto M, Kato T, et al. Postoperative incision hernia in patients with abdominal aortic aneurysm and aortoiliac occlusive disease: a systematic review. Eur J Vasc Endovasc Surg. 2007;33:177–181. doi: 10.1016/j.ejvs.2006.07.009. [DOI] [PubMed] [Google Scholar]


