Abstract
Aims
Gemcitabine has been associated with an increased risk of arterial and venous thromboembolic events (ATEs and VTEs), although the overall risk remains unclear. As indications for its use in oncology are expanding, a comprehensive characterization of these complications becomes imperative.
Methods
Pubmed was searched for articles published from 1 January 1990 to 31 December 2012. Eligible studies included prospective randomized controlled phase II and III trials evaluating gemcitabine based vs. non-gemcitabine based chemotherapy in patients with solid tumours. Data on VTEs and ATEs were extracted. Overall incidence rates, odds ratio (OR), and 95% confidence intervals (CIs) were calculated employing fixed or random effects models depending on the heterogeneity of included trials.
Results
A total of 4845 patients from 19 trials were included. Among patients treated with gemcitabine based chemotherapy, the overall incidence of VTEs (13 studies comprising 3823 patients) and ATEs (eight studies consisting of 2431 patients) was 2.1% (95% CI 1.2%, 3.8%) and 2.2% (95% CI 1.4%, 3.2%). The associated ORs of VTEs and ATEs were 1.56 (95% CI 0.86, 2.83, P = 0.15) and 1.82 (95% CI 0.89, 3.75, P = 0.10) compared with non-gemcitabine based therapy. A tendency to increase the risk of ATE and VTEs was also detected in any prespecified subgroup.
Conclusion
The use of gemcitabine does not significantly increase the risk of VTEs and ATEs in patients with solid tumours when compared with non-gemcitabine based chemotherapy.
Keywords: cancer, gemcitabine, meta-analysis, thromboembolic events
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Gemcitabine has been associated with an increased risk of arterial and venous thromboembolic events (ATEs and VTEs), but the overall incidence and risk of developing thromboembolic events is still unknown.
WHAT THIS STUDY ADDS
Our study for the first time demonstrates that the use of gemcitabine has a tendency to increase the risk of VTEs and ATEs in patients with solid tumours when compared with non-gemcitabine based chemotherapy.
Introduction
Venous and arterial thromboembolic events (VTEs and ATEs) are a major source of morbidity and mortality for cancer patients [1–3]. The importance of cancer-associated thrombosis comes from the fact that it is exceedingly common in cancer patients. It is reported that appropriately one fifth of all VTEs occur in cancer patients and the ones who develop thromboembolic events have a worse prognosis and an increased risk of death [1, 4]. Several clinical characteristics have been associated with increased risk of developing thromboembolic events in patients with cancer, including more advanced disease, systematic chemotherapy, anti-angiogenic therapy, multiple comorbidities and concomitant medications [5–9].
Among chemotherapeutic agents, gemcitabine based regimens particularly have been associated with a wide range of thromboembolic complications [10]. However, this association is mostly based on case reports, single arm prospective studies and retrospective analyses [11–17]. For example, in one prospective study of 108 patients with advanced non-small-cell lung cancer (NSCLC) who underwent chemotherapy with gemcitabine and cisplatin, 22 thromboembolic events occurred in 19 patients (17.6%, 95% CI 10.3, 24.8%), including 10 ATEs (two myocardial infarctions, seven lower limb arterial thrombosis and one ischaemic stroke) and 12 VTEs (three catheter-related upper limb venous thromboembolic events, six venous thrombosis of the lower limb and three pulmonary embolic episodes) [13]. As gemcitabine represents an important contemporary chemotherapeutic agent and the indications for its use in oncology have been expanding, a comprehensive characterization of these complications becomes imperative. Therefore, we performed a systematic review and meta-analysis of randomized controlled trials to evaluate the incidence and odds ratio (OR) of VTEs and ATEs in cancer patients receiving gemcitabine based vs. non-gemcitabine based chemotherapy.
Methods
Data source
The selection and systematic review of trials was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [18]. Trials were selected from those published in PubMed between 1 January 1990, and 31 December 2012, with ‘gemcitabine,’ ‘cancer,’ ‘carcinoma’ and ‘randomized clinical trial’ as keywords. Only trials published in peer-reviewed publications in full manuscript form in English were eligible. Only the most recent publication was included when duplicates were identified. We also reviewed the reference lists of the original and review articles to identify relevant studies.
Study selection
Our primary objective was to evaluate the association between treatment with gemcitabine based therapy and risk of VTEs and ATEs in patients with cancer. Clinical trials meeting the following criteria were included in the meta-analysis: 1) prospective randomized controlled phase II or III trial of cancer patients, 2) random assignment of participants to treatment with gemcitabine or non-gemcitabine containing therapy and 3) available data on all grade VTEs or ATEs. The quality of reports of clinical trials was assessed and calculated using the five item Jadad scale including randomization, double-blinding and withdrawals as previously described [19].
Data extraction and clinical end point
Data extraction was conducted independently by two investigators (WXQ and ZS) and any discrepancy between the reviewers was resolved by consensus. For each study, the following information was extracted: author, publication year, trial phase, treatment arms, number of patients enrolled, number evaluable for toxicity, underlying malignancy, median age, median treatment duration, median progression free survival, adverse outcomes of interest (VTEs and ATEs), gemcitabine dosage (mg m−2) and schedules used. The following adverse outcomes were considered as VTEs/ATEs and included in the main analysis: thrombosis/thrombus/embolism (excluded vascular access related-thrombosis if reported separately), arterial thrombosis, cerebral infarct, cerebral ischaemia, cerebrovascular accident, myocardial infarction and myocardial ischaemia. Phlebitis (including superficial thrombosis) was initially included and subsequently extracted from analysis to observe if it led to different results of the main comparisons. We assessed and recorded adverse events according to the National Cancer Institute's common toxicity criteria (version 2 or 3), which has been adopted widely in cancer clinical trials [20].
Statistical analysis
All analyses were performed using Stata version 12.0 software (Stata Corporation, College Station, TX, USA) and Open Meta-Analyst software version 4.16.12 (Tufts University). For the calculation of incidence, the number of patients with ATEs/VTEs and the number of patients receiving gemcitabine were extracted from the selected clinical trials. The proportion of patients with ATEs/VTEs and 95% confidence interval (CI) were derived for each study. For the calculation of the OR, patients assigned to gemcitabine based therapy were compared only with those assigned to control treatment in the same trial. We used the Peto method to calculate ORs and 95% CIs because this method provides the best confidence interval coverage and is more powerful and relatively less biased than the fixed or random effects analysis when dealing with low event rates [21]. Between study heterogeneity was estimated using the χ2-based Q test and I2 statistic [22]. Heterogeneity was considered statistically significant when Pheterogeneity < 0.1 or I2 > 50%. If heterogeneity existed, data were analyzed using a random effects model (DerSimonian Larid method). In the absence of heterogeneity, a fixed effects model was used. A two-sided P value less than 0.05 was considered significant. Prespecified subgroup analyses were performed according to tumour type, phase of trials, publication year or ethnicity. The presence of publication bias was evaluated by using the Begg and Egger tests [23, 24]. The trim and fill method was also used to explore potential biases.
Results
Our search yielded 1457 publications describing the use of gemcitabine, and 19 RCTs were finally included in the meta-analysis. The selection process is summarized in Figure 1. In total, 4845 patients were investigated in these trials and they had a variety of cancers: NSCLC (13 trials) [25–37], breast cancer (three trials) [38–40], pancreatic cancer (two trials) [41, 42] and head and neck cancer (one trial) [43]. Sample sizes were in the range of 52 to 620 patients, with five trials including >400 patients each. According to the inclusion criteria of each trial, patients were required to have adequate renal, hepatic and haematologic function. The median age of study participants was in the range of 54–77 years (some studies only reported the mean age). The quality of 19 included trials was moderate and the median Jadad score was 2 (range = 2–3). None of the included trials was a double-blind randomized placebo controlled trial. Six trials did not mention the blinding of allocation clearly in the randomization process and thus had Jadad scores of 3. Thirteen trials did not mention the blinding of allocation clearly in the randomization process, and did not mention the concealment of allocation and thus had Jadad scores of 2. Table 1 reports the study and patient characteristics for the included trials.
Figure 1.
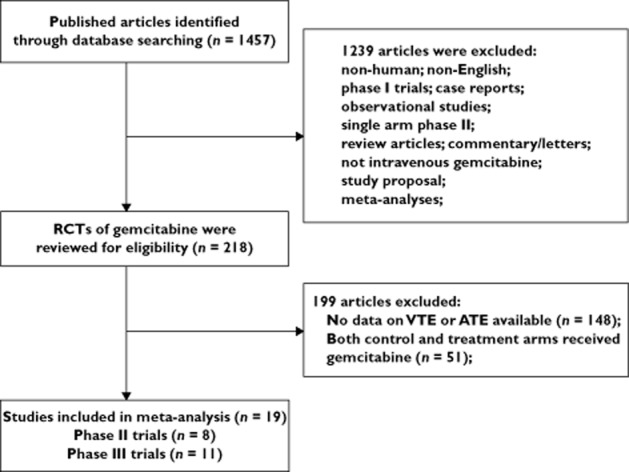
Selection process for randomized controlled trials included in the meta-analysis
Table 1.
Characteristics of 19 randomized controlled clinical trials included in the meta-analysis
| Author/year | Phase | Underlying malignancies | Patients enrolled | Treatment arm | Median age (years) | Median treatment duration (months/cycles) | Median PFS/TTF (months) | Number of patients for analysis | Number of VTEs | Number of ATEs | Jadad score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sandler et al. 2000 [25] | III | NSCLC | 522 | GEM 1000 mg m−2 + CDDP q.4.w. | 62 | 4 cycles | 5.6 | 260 | NR | 4 | 2 |
| CDDP q.4.w. | 63 | 4 cycles | 3.7 | 262 | NR | 1 | |||||
| Scagliotti et al. 2002 [26] | III | NSCLC | 620 | GEM 1000 mg m−2 + CDDP q.4.w. | 63 | 9.4 | 4.6 | 197 | 1 | 4 | 2 |
| PTX+CBP q.4.w. | 62 | 8.7 | 4.6 | 194 | 2 | 1 | |||||
| NVB+CDDP q.4.w. | 63 | 8.2 | 3.8 | 198 | 2 | 1 | |||||
| Sculier et al. 2002 [24] | III | NSCLC | 284 | GEM 1000 mg m−2 + CDDP+CBP q.4.w. | NR | NR | 86 days | 92 | NR | 4 | 2 |
| IFO+GEM q.4.w. | NR | NR | 84 days | 94 | NR | 0 | |||||
| CDDP+IFO+CBP q.4.w. | NR | NR | 84 days | 94 | NR | 3 | |||||
| Comella et al. 2004 [28] | II | NSCLC | 264 | GEM 1200 mg m−2 q.4.w. | 75 | 3 cycles | 3.3 | 68 | NR | 2 | 3 |
| PTX q.4.w. | 72 | 3 cycles | 3.7 | 63 | NR | 3 | |||||
| GEM 1000 mg m−2 + NVB q.3.w. | 72 | 3 cycles | 4.1 | 68 | NR | 1 | |||||
| GEM+PTX q.3.w. | 73 | 3 cycles | 4.5 | 65 | NR | 3 | |||||
| Georgoulias et al. 2005 [29] | III | NSCLC | 413 | GEM 1000 mg m−2 + DOC q.3.w. | 63 | 4 cycles | NR | 197 | NR | 1 | 2 |
| NVB+DDP q.3.w. | 64 | 4 cycles | NR | 192 | NR | 0 | |||||
| Lutz et al. 2005 [41] | II | Pancreatic cancer | 96 | GEM 800 mg m−2 + DOC q.3.w. | 58 | 4 cycles | 3.9 | 45 | 1 | NR | 2 |
| TXT+DDP q.3.w. | 59 | 4 cycles | 2.8 | 44 | 0 | NR | |||||
| Tan et al. 2005 [30] | III | NSCLC | 316 | GEM 1000 mg m−2 + NVB q.3.w. | 59 | 4 cycles | 3.9 | 154 | 5 | NR | 2 |
| NVB+CBP q.3.w. | 60 | 4 cycles | 4.4 | 155 | 1 | NR | |||||
| Fountzilas et al. 2006 [43] | II | Head and neck cancer | 166 | GEM 1000 mg m−2 + PTX q.3.w. | 63 | NR | 4.4 | 85 | NR | 3 | 2 |
| PTX+PLD q.3.w. | 65 | NR | 6.0 | 81 | NR | 1 | |||||
| Leong et al. 2007 [31] | II | NSCLC | 135 | GEM 800 mg m−2 q.4.w. | 72 | 2 cycles | 3.42 | 43 | 1 | NR | 2 |
| NVB q.4.w. | 73 | 2 cycles | 2.99 | 45 | 0 | NR | |||||
| TXT q.4.w. | 72 | 2 cycles | 2.78 | 46 | 1 | NR | |||||
| Martin et al. 2007 [38] | III | MBC | 252 | GEM 1200 mg m−2 + NVB q.3.w. | 58 | 6 cycles | 6.0 | 123 | 1 | NR | 3 |
| NVB q.3.w. | 57 | 4 cycles | 4.0 | 125 | 2 | NR | |||||
| Ohe et al. 2007 [32] | III | NSCLC | 602 | GEM 1000 mg m−2 + CDDP q.3.w. | 61 | NR | 3.2 | 151 | 0 | NR | 2 |
| PTX+CBP q.3.w. | 63 | NR | 3.2 | 148 | 0 | NR | |||||
| CPT-11 + CDDP q.4.w. | 62 | NR | 3.3 | 147 | 0 | NR | |||||
| NVB+CDDP q.3.w. | 61 | NR | 3.0 | 146 | 1 | NR | |||||
| Brufsky et al. 2011 [39] | II | MBC | 191 | GEM 1500 mg m−2 + PTX+BEV q.4.w. | 55.2 | 6 cycles | 11.3 | 93 | 5 | NR | 3 |
| PTX+BEV q.4.w. | 57.5 | 6 cycles | 8.8 | 94 | 3 | NR | |||||
| Kosmidis et al. 2011 [33] | III | NSCLC | 398 | GEM 1000 mg m−2 + PTX q.3.w. | 59 | 4 cycles | 5.0 | 185 | 1 | NR | 3 |
| PTX+NVB q.4.w. | 62 | 3 cycles | 4.4 | 185 | 1 | NR | |||||
| Seidman et al. 2011 [40] | III | MBC | 475 | GEM 1000 mg m−2 + DOC q.3.w. | 57 | 6 cycles | 6.7 | 237 | 4 | NR | 2 |
| CAP+DOC q.3.w. | 54 | 6 cycles | 5.1 | 226 | 1 | NR | |||||
| Weissman et al. 2011 [34] | III | NSCLC | 383 | GEM 1000 mg m−2 + L-OHP q.3.w. | 63 | 4 cycles | 4.44 | 184 | 0 | NR | 3 |
| CBP+PTX q.3.w. | 64 | 4 cycles | 4.67 | 187 | 1 | NR | |||||
| EI-Khoueiry et al. 2012 [42] | II | Pancreatic cancer | 52 | GEM 1000 mg m−2 + SOR q.4.w. | 65 | 2 cycles | 2.3 | 37 | 3 | NR | 2 |
| SOR qd. | 66 | 2 cycles | 2.9 | 15 | 0 | NR | |||||
| Han et al. 2012 [35] | III | NSCLC | 313 | GEM 1250 mg m−2 + DDP q.3.w. | 56.5 | 6 cycles | 6.4 | 150 | 1 | NR | 3 |
| Gefitinib qd. | 57 | 163 days | 5.8 | 159 | 0 | NR | |||||
| Spigel et al. 2012 [37] | II | NSCLC | 110 | GEM 1500 mg m−2 + PEM+BEV q.4.w. | 76 | 2.5 cycles | 4.7 | 55 | 4 | 1 | 2 |
| PEM+CBP+BEV q.3.w. | 77 | 6 cycles | 10.2 | 55 | 4 | 0 | |||||
| Price et al. 2012 [36] | II | NSCLC | 111 | GEM 100 mg m−2 + Radiotherapy | 74 | NR | NR | 55 | NR | 1 | 2 |
| Radiotherapy | 75 | NR | NR | 56 | NR | 0 |
ATE, arterial thromboembolic event; BEV, bevacizumab; CBP, carboplatin; CDDP, cisplatin; CPT-11, irinotecan; DOC, docetaxel; GEM, gemcitabine; IFO, ifosfamide; L-OHP, oxaliplatin; MBC; metastatic breast cancer; NR, not reported; NSCLC, non-small-cell lung cancer; NVB, vinorelbine; PEM, pemetrexed; PFS, progression-free survival; PLD, pegylated liposomal doxorubicin; PTX, paclitaxel; q.4.w., every 4 weeks; q.3.w., every 3 weeks; qd, every day; SOR, sorafenib; TTF, time-to-treatment failure; VTE, venous thromboembolic event.
Incidence of VTEs and ATEs
A total of 3823 patients (13 trials) were considered for the incidence analysis of VTEs. In the gemcitabine group, 27 patients experienced VTEs compared with 19 patients in the non-gemcitabine group. The highest incidence (8.1%; 95% CI 2.6%, 22.3%) was observed in a phase II pancreatic cancer trial [42] and the lowest incidence was observed in two trials in which no VTEs occurred [32, 34]. Using a random effects model (heterogeneity test: Q = 25.164, P = 0.014, I2 = 52%), the summary incidence of VTEs in patients receiving gemcitabine based therapy was 2.1% (95% CI 1.2%, 3.8%, Figure 2).
Figure 2.
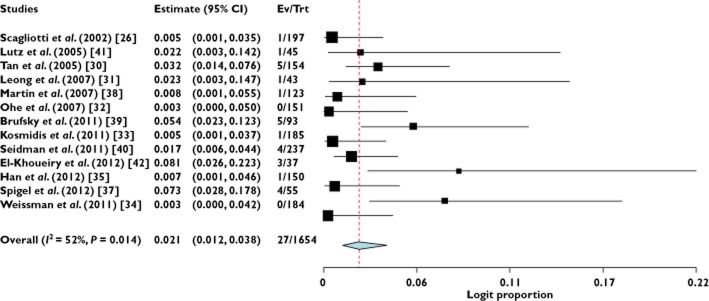
Incidence of venous thromboembolic events associated with gemcitabine
A total of 2431 patients (eight trials) were considered for the incidence analysis of ATEs. 24 patients experienced ATEs compared with 19 patients in the non-gemcitabine group. The highest incidence (3.5%; 95% CI, 1.1%–10.4%) was observed in a phase II head and neck cancer trial [43], and the lowest incidence (0.5%; 95%CI: 0.1%–3.5%) was observed in a phase III NSCLC trial [29]. Using a fixed-effects model (heterogeneity test: Q = 4.062; P = 0.773; I2 = 0%), the summary incidence of ATEs in patients receiving gemcitabine based therapy was 2.2% (95% CI, 1.4%–3.2%, Figure 3).
Figure 3.
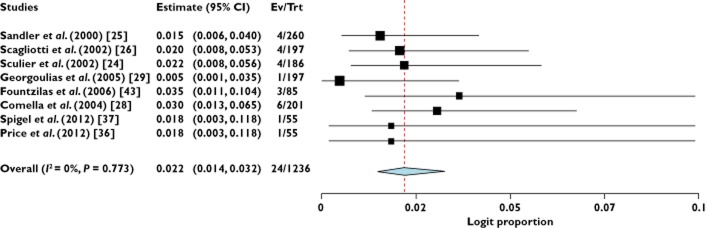
Incidence of arterial thromboembolic events associated with gemcitabine
Odds ratio of VTEs and ATEs
To investigate the specific contribution of gemcitabine to the development of ATEs/VTEs and exclude the influence of confounding factors such as underlying malignancy, and other therapeutic interventions, we determined the OR of gemcitabine associated VTEs and ATEs. The combined results demonstrated that the use of gemcitabine did not significantly increase the risk of developing VTEs (Peto OR 1.56, 95% CI 0.86, 2.83, P = 0.15, Figure 4) using a fixed effect model (I2 = 0%, P = 0.91). Similar results in the risk of VTEs were also detected in subgroup analysis according to tumour type, phase of trials, publication year or ethnicity. In addition, the highest OR of VTEs was observed in pancreatic cancer patients with OR of 5.03 (95% CI 0.59, 42.62, P = 0.138), but the differences among tumour types were not statistically significant (Table 2).
Figure 4.
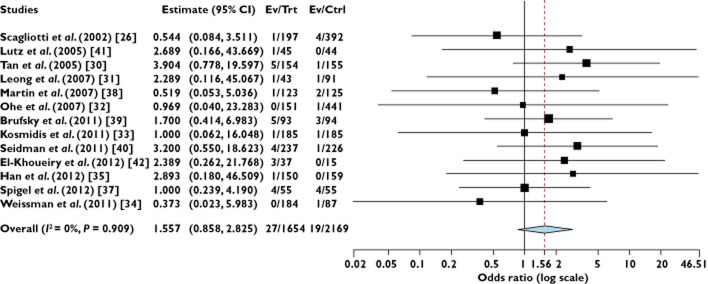
Relative risk of venous thromboembolic events associated with gemcitabine based vs. non-gemcitabine based therapy
Table 2.
Odds ratio of VTEs based on prespecified subgroups
| VTEs, Number/total number | ||||||||
|---|---|---|---|---|---|---|---|---|
| Group | Subgroup | Number of trials | Gemcitabine | Non-gemcitabine | I2(%) | Odds ratio (95% CI) | P for odds ratio | P for group difference |
| Overall | 13 | 27/1654 | 19/2169 | 0 | 1.56 (0.86, 2.83) | 0.145 | NA | |
| Tumour type | NSCLC | 8 | 13/1119 | 13/1665 | 0 | 1.27 (0.57–2.82) | 0.554 | 0.895 |
| Pancreas | 2 | 4/82 | 0/59 | 0 | 5.03 (0.59, 42.62) | 0.138 | ||
| MBC | 3 | 10/453 | 6/445 | 0 | 1.66 (0.62, 4.47) | 0.318 | ||
| Phase of trials | Phase II | 5 | 14/273 | 8/299 | 0 | 1.72 (0.72, 4.10) | 0.224 | 0.790 |
| Phase III | 8 | 13/1381 | 11/1870 | 0 | 1.43 (0.63, 3.24) | 0.392 | ||
| Publication year | 2000–2005 | 3 | 7/396 | 5/591 | 0 | 1.91 (0.60, 6.12) | 0.276 | 0.761 |
| 2006–2012 | 10 | 20/1258 | 14/1578 | 0 | 1.45 (0.72, 2.90) | 0.295 | ||
| Ethnics | Asian | 3 | 6/455 | 2/755 | 0 | 3.27 (0.79, 13.48) | 0.101 | 0.553 |
| Non-Asian | 10 | 21/1199 | 17/1414 | 0 | 1.33 (0.69, 2.56) | 0.398 | ||
MBC, metastatic breast cancer; NA, not available; NSCLC, non-small-cell lung cancer.
Eight randomized trials were available to calculate the OR of ATEs. The meta-analysis showed that the summary OR of ATEs in gemcitabine based vs. non-gemcitabine based therapy was a non-significant 1.82 (95% CI 0.89, 3.75, P = 0.10, Figure 5). The test for heterogeneity was not significant (I2 = 0%, P = 0.59). Additionally, a tendency to increase the risk of ATE was also detected in prespecified subgroups according to tumour type, phase of trials or publication year (Table 3).
Figure 5.

Relative risk of arterial thromboembolic events associated with gemcitabine based vs. non-gemcitabine based therapy
Table 3.
Odds ratio of ATEs based on prespecified subgroups
| ATEs, Number/total number | ||||||||
|---|---|---|---|---|---|---|---|---|
| Group | Subgroup | Number of trials | Gemcitabine | Non-gemcitabine | I2(%) | Odds ratio (95% CI) | P for odds ratio | P for group difference |
| Overall | 8 | 24/1236 | 10/1195 | 0 | 1.82 (0.89, 3.75) | 0.102 | NA | |
| Tumour type | NSCLC | 7 | 21/1151 | 9/1114 | 0 | 1.72 (0.80, 3.73) | 0.168 | 0.868 |
| Head and neck cancer | 1 | 3/85 | 1/81 | 0 | 2.93 (0.30, 28.73) | 0.326 | ||
| Phase of trials | Phase II | 4 | 11/396 | 4/255 | 0 | 1.43 (0.47, 4.39) | 0.528 | 0.640 |
| Phase III | 4 | 13/840 | 6/940 | 5 | 2.16 (0.84, 5.54) | 0.108 | ||
| Publication year | 2000–2005 | 5 | 19/1041 | 9/1003 | 21 | 1.52 (0.68, 3.41) | 0.306 | 0.631 |
| 2006–2012 | 3 | 5/195 | 1/192 | 0 | 3.75 (0.75, 18.75) | 0.108 | ||
ATE, arterial thrombosis events; NA, not available; NSCLC, non-small-cell lung cancer.
Sensitivity analysis
Sensitivity analyses using an empirical continuity correction [21] (fixed Mantel-Haenszel OR for VTEs: 1.62, 95% CI 0.94, 2.78; OR for ATEs: 1.60, 95% CI 0.83, 3.08), with a continuity of 0.5 correction (fixed Mantel-Haenszel OR for VTEs: 1.50, 95% CI 0.84, 2.69; OR for ATEs: 1.67, 95% CI 0.84, 3.35), or without a continuity correction (fixed Mantel-Haenszel OR of VTEs: 1.59, 95% CI 0.86, 2.95; OR for ATEs: 1.77, 95% CI 0.85, 3.68) showed results similar to those of the primary analysis (Table 4).
Table 4.
Sensitivity analyses for the outcome of VTEs and ATEs
| Factors | Sensitivity analysis | Statistical model | OR (95% CI) |
|---|---|---|---|
| VTEs | Empirical continuity correction | Fixed (MH) | 1.62 (0.94, 2.78) |
| No continuity correction | Fixed (MH) | 1.59 (0.86, 2.95) | |
| A continuity correction of 0.5 | Fixed (MH) | 1.50 (0.84, 2.69) | |
| ATEs | Empirical continuity correction | Fixed (MH) | 1.60 (0.83, 3.08) |
| No continuity correction | Fixed (MH) | 1.77 (0.85, 3.68) | |
| A continuity correction of 0.5 | Fixed (MH) | 1.67 (0.84, 3.35) |
ATEs, arterial thrombosis events; CI, confidence interval; MH, Mantel-Haenszel test; VTEs, venous thrombosis events.
Publication bias
No evidence of publication bias was detected for the OR of VTEs and ATEs in this study by either Begg or Egger's test (OR of VTEs: Begg's test P = 0.542; Egger's test P = 0.568; OR of ATEs: Begg's test P = 0.142; Egger's test P = 0.256). Analogously, the trim and fill analysis did not show a publication bias for VTE and ATE events.
Discussion
Our meta-analysis is the first, to the best of our knowledge, to explore the risk of thromboembolic events associated with gemcitabine. The combined analysis of data from randomized controlled trials shows that the use of gemcitabine has a tendency to increase the risk of VTEs and ATEs in cancer patients when compared with non-gemcitabine based therapy. Additionally, the overall incidence of gemcitabine associated VTEs and ATEs is 2.1% (95% CI 1.2%, 3.8%) and 2.2% (95% CI 1.4%, 3.2%), respectively. A tendency to increase the risk of ATE and VTEs was also detected in any prespecified subgroup.
One possible explanation for this finding is the under-reporting of VTEs and ATEs. Because clinical trials with gemcitabine are usually not designed specifically to address toxic events, the number of cancer trials reporting these vascular events is very low. In our search, 88.4% of prospective clinical trials were excluded because data on thromboembolic events was unavailable. In addition, thromboembolic events are usually under-diagnosed because they are asymptomatic at presentation and therefore, often diagnosed incidentally. Another possible explanation for this finding is that a relatively small number of patients were included in our study and thus there is lack of statistical power to demonstrate a significant difference. As a result, more high quality randomized controlled trials are still needed to investigate whether gemcitabine is associated with VTEs and ATEs.
The pathogenesis of gemcitabine-induced thrombogenicity remains unclear, although several studies have suggested potential mechanisms. Gemcitabine-induced thrombocytopenia and thrombocytosis may be directly related to the increased risk of thromboembolic events, because either one of these adverse events may be important in overwhelming the regulatory mechanisms and overturning the balance towards thrombophilia [10]. Gemcitabine may also be capable of coagulation cascade activation and possibly endothelial damage [17]. However, the precise mechanism by which gemcitabine induces a shift towards the procoagulant state remains to be clarified.
Currently, the international guidelines do not recommend routine VTE prophylaxis during chemotherapy in outpatient settings 44. Some recent data suggest that low molecular weight heparin prophylaxis can reduce the risk of VTE in patients with certain types of cancer [45]. Our data of a non-significantly increased risk of VTEs with gemcitabine used in solid tumours could be used as the basis for testing thromboprophylaxis in an appropriate clinical trial setting.
Our meta-analysis has several limitations. First, this meta-analysis is not based on individual patient data and meta-analyses based on published data tend to overestimate treatment effects compared with individual patient data analyses. In addition, it precludes a more comprehensive analysis such as adjusting for baseline factors and other differences that exist between the trials from which the data are pooled. Secondly, there are potentially important differences among the included studies, including differing dosage, administration schedule and infusion duration of gemcitabine, periods of study conduct and study investigators. All of these could possibly impact on gemcitabine-related thrombosis events and increase the clinical heterogeneity among included trials. Additionally, our study includes a mixed population of patients treated with a gemcitabine based combination (including platinum, capecitabine, paclitaxel, docetaxel, irinotecan, bevacizumab, pemetrexed and vinorebline) therapy or gemcitabine alone, It is possible that the concomitant administration of other drugs (such as the combination with bevacizumab or platinum) in a few of the trials may have contributed to a higher risk of VTEs and ATEs. Indeed, previous meta-analyses have demonstrated that the use of bevacizumab or platinum in cancer patients is associated with an increased risk of thrombotic events [9, 46]. Therefore, all of these would increase the heterogeneity and make the interpretation of the results more problematic. Thirdly, these studies were conducted at various international institutions by different investigators and may have potential bias in reporting the types of adverse events. In particular, the frequency of VTEs is under-reported in clinical trials. Trials which reported zero VTEs and ATEs in one or both arms were also included for analysis. In this setting, using fixed effects models and continuity corrections would bias the results towards null. However we feel that including trials reporting zero VTEs and ATEs would provide the most conservative estimate. Finally, the included studies were conducted at major academic institutions among patients with adequate major organ function and may not reflect the general patient population in the community or patients with organ dysfunction. It could be that thrombosis is more frequent in a ‘real-life’ setting, as a retrospective cohort analysis showed [47].
Conclusion
In conclusion, with the present evidence, the use of gemcitabine does not increase the risk of VTEs and ATEs in patients with solid tumours when compared with non-gemcitabine based chemotherapy.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
References
- 1.Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5:632–634. doi: 10.1111/j.1538-7836.2007.02374.x. [DOI] [PubMed] [Google Scholar]
- 2.Lyman GH, Khorana AA, Falanga A, Clarke-Pearson D, Flowers C, Jahanzeb M, Kakkar A, Kuderer NM, Levine MN, Liebman H, Mendelson D, Raskob G, Somerfield MR, Thodiyil P, Trent D, Francis CW. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25:5490–5505. doi: 10.1200/JCO.2007.14.1283. [DOI] [PubMed] [Google Scholar]
- 3.Lyman GH, Khorana AA. Cancer, clots and consensus: new understanding of an old problem. J Clin Oncol. 2009;27:4821–4826. doi: 10.1200/JCO.2009.22.3032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heit JA. Cancer and venous thromboembolism: scope of the problem. Cancer Control. 2005;12(Suppl. 1):5–10. doi: 10.1177/1073274805012003S02. [DOI] [PubMed] [Google Scholar]
- 5.Khorana AA, Connolly GC. Assessing risk of venous thromboembolism in the patient with cancer. J Clin Oncol. 2009;27:4839–4847. doi: 10.1200/JCO.2009.22.3271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choueiri TK, Schutz FA, Je Y, Rosenberg JE, Bellmunt J. Risk of arterial thromboembolic events with sunitinib and sorafenib: a systematic review and meta-analysis of clinical trials. J Clin Oncol. 2010;28:2280–2285. doi: 10.1200/JCO.2009.27.2757. [DOI] [PubMed] [Google Scholar]
- 7.Ranpura V, Hapani S, Chuang J, Wu S. Risk of cardiac ischemia and arterial thromboembolic events with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis of randomized controlled trials. Acta Oncol. 2010;49:287–297. doi: 10.3109/02841860903524396. [DOI] [PubMed] [Google Scholar]
- 8.Proverbs-Singh T, Chiu SK, Liu Z, Seng S, Sonpavde G, Choueiri TK, Tsao CK, Yu M, Hahn NM, Oh WK, Galsky MD. Arterial thromboembolism in cancer patients treated with cisplatin: a systematic review and meta-analysis. J Natl Cancer Inst. 2012;104:1837–1840. doi: 10.1093/jnci/djs435. [DOI] [PubMed] [Google Scholar]
- 9.Seng S, Liu Z, Chiu SK, Proverbs-Singh T, Sonpavde G, Choueiri TK, Tsao CK, Yu M, Hahn NM, Oh WK, Galsky MD. Risk of venous thromboembolism in patients with cancer treated with cisplatin: a systematic review and meta-analysis. J Clin Oncol. 2012;30:4416–4426. doi: 10.1200/JCO.2012.42.4358. [DOI] [PubMed] [Google Scholar]
- 10.Dasanu CA. Gemcitabine: vascular toxicity and prothrombotic potential. Expert Opin Drug Saf. 2008;7:703–716. doi: 10.1517/14740330802374262. [DOI] [PubMed] [Google Scholar]
- 11.Desai AA, Vogelzang NJ, Rini BI, Ansari R, Krauss S, Stadler WM. A high rate of venous thromboembolism in a multi-institutional phase II trial of weekly intravenous gemcitabine with continuous infusion fluorouracil and daily thalidomide in patients with metastatic renal cell carcinoma. Cancer. 2002;95:1629–1636. doi: 10.1002/cncr.10847. [DOI] [PubMed] [Google Scholar]
- 12.D'Epiro S, Salvi M, Mattozzi C, Giancristoforo S, Campoli M, Zanniello R, Luci C, Macaluso L, Giovannoni S, Iacovelli R, Calvieri S, Richetta AG. Gemcitabine-induced extensive skin necrosis. Case Rep Med. 2012;2012:831616. doi: 10.1155/2012/831616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Numico G, Garrone O, Dongiovanni V, Silvestris N, Colantonio I, Di Costanzo G, Granetto C, Occelli M, Fea E, Heouaine A, Gasco M, Merlano M. Prospective evaluation of major vascular events in patients with nonsmall cell lung carcinoma treated with cisplatin and gemcitabine. Cancer. 2005;103:994–999. doi: 10.1002/cncr.20893. [DOI] [PubMed] [Google Scholar]
- 14.Kucukates E. Antimicrobial resistance among Gram-negative bacteria isolated from intensive care units in a Cardiology Institute in Istanbul, Turkey. Jpn J Infect Dis. 2005;58:228–231. [PubMed] [Google Scholar]
- 15.Zupancic M, Shah PC, Shah-Khan F. Gemcitabine-associated thrombotic thrombocytopenic purpura. Lancet Oncol. 2007;8:634–641. doi: 10.1016/S1470-2045(07)70203-6. [DOI] [PubMed] [Google Scholar]
- 16.Kalapura T, Krishnamurthy M, Reddy CV. Acute myocardial infarction following gemcitabine therapy - a case report. Angiology. 1999;50:1021–1025. doi: 10.1177/000331979905001208. [DOI] [PubMed] [Google Scholar]
- 17.Duvic M, Talpur R, Wen S, Kurzrock R, David CL, Apisarnthanarax N. Phase II evaluation of gemcitabine monotherapy for cutaneous T-cell lymphoma. Clin Lymphoma Myeloma. 2006;7:51–58. doi: 10.3816/CLM.2006.n.039. [DOI] [PubMed] [Google Scholar]
- 18.Moher DLA, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, Tugwell P, Klassen TP. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet. 1998;352:609–613. doi: 10.1016/S0140-6736(98)01085-X. [DOI] [PubMed] [Google Scholar]
- 20.NCI, Cancer Therapy Evaluation Program. CTC v 2.0 and common terminology criteria for adverse events criteria V3.0 (CTCAE). Available at: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm (last accessed 27 January 2013)
- 21.Sweeting MJ, Sutton AJ, Lambert PC. What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med. 2004;23:1351–1375. doi: 10.1002/sim.1761. [DOI] [PubMed] [Google Scholar]
- 22.Zintzaras E, Ioannidis JP. Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol. 2005;28:123–137. doi: 10.1002/gepi.20048. [DOI] [PubMed] [Google Scholar]
- 23.Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985;27:335–371. doi: 10.1016/s0033-0620(85)80003-7. [DOI] [PubMed] [Google Scholar]
- 24.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 25.Sandler AB, Nemunaitis J, Denham C, von Pawel J, Cormier Y, Gatzemeier U, Mattson K, Manegold C, Palmer MC, Gregor A, Nguyen B, Niyikiza C, Einhorn LH. Phase III trial of gemcitabine plus cisplatin vs. cisplatin alone in patients with locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol. 2000;18:122–130. doi: 10.1200/JCO.2000.18.1.122. [DOI] [PubMed] [Google Scholar]
- 26.Scagliotti GV, De Marinis F, Rinaldi M, Crino L, Gridelli C, Ricci S, Matano E, Boni C, Marangolo M, Failla G, Altavilla G, Adamo V, Ceribelli A, Clerici M, Di Costanzo F, Frontini L, Tonato M. Phase III randomized trial comparing three platinum-based doublets in advanced non-small-cell lung cancer. J Clin Oncol. 2002;20:4285–4291. doi: 10.1200/JCO.2002.02.068. [DOI] [PubMed] [Google Scholar]
- 27.Sculier JP, Lafitte JJ, Lecomte J, Berghmans T, Thiriaux J, Florin MC, Efremidis A, Alexopoulos CG, Recloux P, Ninane V, Mommen P, Paesmans M, Klastersky J. A three-arm phase III randomised trial comparing combinations of platinum derivatives, ifosfamide and/or gemcitabine in stage IV non-small-cell lung cancer. Ann Oncol. 2002;13:874–882. doi: 10.1093/annonc/mdf154. [DOI] [PubMed] [Google Scholar]
- 28.Comella P, Frasci G, Carnicelli P, Massidda B, Buzzi F, Filippelli G, Maiorino L, Guida M, Panza N, Mancarella S, Cioffi R. Gemcitabine with either paclitaxel or vinorelbine vs. paclitaxel or gemcitabine alone for elderly or unfit advanced non-small-cell lung cancer patients. Br J Cancer. 2004;91:489–497. doi: 10.1038/sj.bjc.6602011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Georgoulias V, Ardavanis A, Tsiafaki X, Agelidou A, Mixalopoulou P, Anagnostopoulou O, Ziotopoulos P, Toubis M, Syrigos K, Samaras N, Polyzos A, Christou A, Kakolyris S, Kouroussis C, Androulakis N, Samonis G, Chatzidaki D. Vinorelbine plus cisplatin vs. docetaxel plus gemcitabine in advanced non-small-cell lung cancer: a phase III randomized trial. J Clin Oncol. 2005;23:2937–2945. doi: 10.1200/JCO.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 30.Tan EH, Szczesna A, Krzakowski M, Macha HN, Gatzemeier U, Mattson K, Wernli M, Reiterer P, Hui R, Pawel JV, Bertetto O, Pouget JC, Burillon JP, Parlier Y, Abratt R. Randomized study of vinorelbine – gemcitabine vs. vinorelbine – carboplatin in patients with advanced non-small cell lung cancer. Lung Cancer. 2005;49:233–240. doi: 10.1016/j.lungcan.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 31.Leong SS, Toh CK, Lim WT, Lin X, Tan SB, Poon D, Tay MH, Foo KF, Ho J, Tan EH. A randomized phase II trial of single-agent gemcitabine, vinorelbine, or docetaxel in patients with advanced non-small cell lung cancer who have poor performance status and/or are elderly. J Thorac Oncol. 2007;2:230–236. doi: 10.1097/JTO.0b013e318031d06f. [DOI] [PubMed] [Google Scholar]
- 32.Ohe Y, Ohashi Y, Kubota K, Tamura T, Nakagawa K, Negoro S, Nishiwaki Y, Saijo N, Ariyoshi Y, Fukuoka M. Randomized phase III study of cisplatin plus irinotecan vs. carboplatin plus paclitaxel, cisplatin plus gemcitabine, and cisplatin plus vinorelbine for advanced non-small-cell lung cancer: Four-Arm Cooperative Study in Japan. Ann Oncol. 2007;18:317–323. doi: 10.1093/annonc/mdl377. [DOI] [PubMed] [Google Scholar]
- 33.Kosmidis PA, Fountzilas G, Eleftheraki AG, Kalofonos HP, Pentheroudakis G, Skarlos D, Dimopoulos MA, Bafaloukos D, Pectasides D, Samantas E, Boukovinas J, Lambaki S, Katirtzoglou N, Bakogiannis C, Syrigos KN. Paclitaxel and gemcitabine vs. paclitaxel and vinorelbine in patients with advanced non-small-cell lung cancer. A phase III study of the Hellenic Cooperative Oncology Group (HeCOG) Ann Oncol. 2011;22:827–834. doi: 10.1093/annonc/mdq445. [DOI] [PubMed] [Google Scholar]
- 34.Weissman CH, Reynolds CH, Neubauer MA, Pritchard S, Kobina S, Asmar L. A phase III randomized trial of gemcitabine-oxaliplatin vs. carboplatin-paclitaxel as first-line therapy in patients with advanced non-small cell lung cancer. J Thorac Oncol. 2011;6:358–364. doi: 10.1097/JTO.0b013e3181ffe8ef. [DOI] [PubMed] [Google Scholar]
- 35.Han JY, Park K, Kim SW, Lee DH, Kim HY, Kim HT, Ahn MJ, Yun T, Ahn JS, Suh C, Lee JS, Yoon SJ, Han JH, Lee JW, Jo SJ. First-SIGNAL: first-line single-agent iressa vs. gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. J Clin Oncol. 2012;30:1122–1128. doi: 10.1200/JCO.2011.36.8456. [DOI] [PubMed] [Google Scholar]
- 36.Price A, Yellowlees A, Keerie C, Russell S, Faivre-Finn C, Gilligan D, Snee M, Skailes G, Hatton M, Erridge S, Mohammed N. Radical radiotherapy with or without gemcitabine in patients with early stage medically inoperable non-small cell lung cancer. Lung Cancer. 2012;77:532–536. doi: 10.1016/j.lungcan.2012.05.089. [DOI] [PubMed] [Google Scholar]
- 37.Spigel DR, Hainsworth JD, Shipley DL, Ervin TJ, Kohler PC, Lubiner ET, Peyton JD, Waterhouse DM, Burris HA, 3rd, Greco FA. A randomized phase II trial of pemetrexed/gemcitabine/bevacizumab or pemetrexed/carboplatin/bevacizumab in the first-line treatment of elderly patients with advanced non-small cell lung cancer. J Thorac Oncol. 2012;7:196–202. doi: 10.1097/JTO.0b013e3182307efe. [DOI] [PubMed] [Google Scholar]
- 38.Martin M, Ruiz A, Munoz M, Balil A, Garcia-Mata J, Calvo L, Carrasco E, Mahillo E, Casado A, Garcia-Saenz JA, Escudero MJ, Guillem V, Jara C, Ribelles N, Salas F, Soto C, Morales-Vasquez F, Rodriguez CA, Adrover E, Mel JR. Gemcitabine plus vinorelbine vs. vinorelbine monotherapy in patients with metastatic breast cancer previously treated with anthracyclines and taxanes: final results of the phase III Spanish Breast Cancer Research Group (GEICAM) trial. Lancet Oncol. 2007;8:219–225. doi: 10.1016/S1470-2045(07)70041-4. [DOI] [PubMed] [Google Scholar]
- 39.Brufsky A, Hoelzer K, Beck T, Whorf R, Keaton M, Nadella P, Krill-Jackson E, Kroener J, Middleman E, Frontiera M, Paul D, Panella T, Bromund J, Zhao L, Orlando M, Tai F, Marciniak MD, Obasaju C, Hainsworth J. A randomized phase II study of paclitaxel and bevacizumab with and without gemcitabine as first-line treatment for metastatic breast cancer. Clin Breast Cancer. 2011;11:211–220. doi: 10.1016/j.clbc.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 40.Seidman AD, Brufsky A, Ansari RH, Hart LL, Stein RS, Schwartzberg LS, Stewart JF, Russell CA, Chen SC, Fein LE, De La Cruz Vargas JA, Kim SB, Cavalheiro J, Zhao L, Gill JF, Obasaju CK, Orlando M, Tai DF. Phase III trial of gemcitabine plus docetaxel vs. capecitabine plus docetaxel with planned crossover to the alternate single agent in metastatic breast cancer. Ann Oncol. 2011;22:1094–1101. doi: 10.1093/annonc/mdq578. [DOI] [PubMed] [Google Scholar]
- 41.Lutz MP, Van Cutsem E, Wagener T, Van Laethem JL, Vanhoefer U, Wils JA, Gamelin E, Koehne CH, Arnaud JP, Mitry E, Husseini F, Reichardt P, El-Serafi M, Etienne PL, Lingenfelser T, Praet M, Genicot B, Debois M, Nordlinger B, Ducreux MP. Docetaxel plus gemcitabine or docetaxel plus cisplatin in advanced pancreatic carcinoma: randomized phase II study 40984 of the European Organisation for Research and Treatment of Cancer Gastrointestinal Group. J Clin Oncol. 2005;23:9250–9256. doi: 10.1200/JCO.2005.02.1980. [DOI] [PubMed] [Google Scholar]
- 42.El-Khoueiry AB, Ramanathan RK, Yang DY, Zhang W, Shibata S, Wright JJ, Gandara D, Lenz HJ. A randomized phase II of gemcitabine and sorafenib vs sorafenib alone in patients with metastatic pancreatic cancer. Invest New Drugs. 2012;30:1175–1183. doi: 10.1007/s10637-011-9658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fountzilas G, Papakostas P, Dafni U, Makatsoris T, Karina M, Kalogera-Fountzila A, Maniadakis N, Aravantinos G, Syrigos K, Bamias A, Christodoulou C, Economopoulos T, Kalofonos H, Nikolaou A, Angouridakis N, Stathopoulos G, Bafaloukos D, Pavlidis N, Daniilidis J. Paclitaxel and gemcitabine vs. paclitaxel and pegylated liposomal doxorubicin in advanced non-nasopharyngeal head and neck cancer. An efficacy and cost analysis randomized study conducted by the Hellenic Cooperative Oncology Group. Ann Oncol. 2006;17:1560–1567. doi: 10.1093/annonc/mdl151. [DOI] [PubMed] [Google Scholar]
- 44.NCCN. Clinical Practice Guidelines in Oncology. Venous Thromboembolic Disease V.1.2010. Available at: http://www.nccn.org (last accessed 1 January 2013)
- 45.Agnelli G, Gussoni G, Bianchini C, Verso M, Mandala M, Cavanna L, Barni S, Labianca R, Buzzi F, Scambia G, Passalacqua R, Ricci S, Gasparini G, Lorusso V, Bonizzoni E, Tonato M. Nadroparin for the prevention of thromboembolic events in ambulatory patients with metastatic or locally advanced solid cancer receiving chemotherapy: a randomised, placebo-controlled, double-blind study. Lancet Oncol. 2009;10:943–949. doi: 10.1016/S1470-2045(09)70232-3. [DOI] [PubMed] [Google Scholar]
- 46.Nalluri SR, Chu D, Keresztes R, Zhu X, Wu S. Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis. JAMA. 2008;300:2277–2285. doi: 10.1001/jama.2008.656. [DOI] [PubMed] [Google Scholar]
- 47.Khorana AA, Dalal M, Lin J, Connolly GC. Incidence and predictors of venous thromboembolism (VTE) among ambulatory high-risk cancer patients undergoing chemotherapy in the United States. Cancer. 2013;119:648–655. doi: 10.1002/cncr.27772. [DOI] [PubMed] [Google Scholar]


