Abstract
AIM: To evaluate changes in the fatty acid composition of erythrocyte membrane phospholipids during severe and mild acute pancreatitis (AP) of alcoholic and nonalcoholic etiology.
METHODS: All consecutive patients with a diagnosis of AP and onset of the disease within the last 72 h admitted to the Hospital of Lithuanian University of Health Sciences between June and December 2007 were included. According to the Acute Physiology and Chronic Health Evaluation (APACHE II) scale, the patients were subdivided into the mild (APACHE II score < 7, n = 22) and severe (APACHE II score ≥ 7, n = 17) AP groups. Healthy individuals (n = 26) were enrolled as controls. Blood samples were collected from patients on admission to the hospital. Fatty acids (FAs) were extracted from erythrocyte phospholipids and expressed as percentages of the total FAs present in the chromatogram. The concentrations of superoxide dismutase and glutathione peroxidase were measured in erythrocytes.
RESULTS: We found an increase in the percentages of saturated and monounsaturated FAs, a decrease in the percentages of total polyunsaturated FAs (PUFAs) and n-3 PUFAs in erythrocyte membrane phospholipids of AP patients compared with healthy controls. Palmitic (C16:0), palmitoleic (C16:1n7cis), arachidonic (C20:4n6), docosahexaenoic (DHA, C22:6n3), and docosapentaenoic (DPA, C22:5n3) acids were the major contributing factors. A decrease in the peroxidation and unsaturation indexes in AP patients as well as the severe and mild AP groups as compared with controls was observed. The concentrations of antioxidant enzymes in the mild AP group were lower than in the control group. In severe AP of nonalcoholic etiology, the percentages of arachidic (C20:0) and arachidonic (C20:4n6) acids were decreased as compared with the control group. The patients with mild AP of nonalcoholic etiology had the increased percentages of total saturated FAs and gama linoleic acid (C18:3n6) and the decreased percentages of elaidic (C18:1n9t), eicosapentaenoic acid (EPA, C20:5n3), DPA (C22:5n3), DHA (C22:6n3) as well as total and n-3 PUFAs in erythrocyte membrane phospholipids.
CONCLUSION: The composition of FAs in erythrocyte membranes is altered during AP. These changes are likely to be associated with alcohol consumption, inflammatory processes, and oxidative stress.
Keywords: Acute pancreatitis, Alcohol, Fatty acids, Oxidative stress, Systemic inflammatory response syndrome
Core tip: The manuscript by Kuliaviene et al elucidates the changes of fatty acids in erythrocyte membrane phospholipids during acute pancreatitis. Alcohol may influence the increased percentage of saturated and monounsaturated fatty acids of erythrocyte membrane. Fatty acids that are linked with inflammatory processes change differently during severe and mild nonalcoholic acute pancreatitis. The decrease of pro-inflammatory acids is seen in severe acute pancreatitis while anti-inflammatory players decrease during mild acute pancreatitis. The antioxidant enzymes of erythrocytes change in mild but not severe pancreatitis group. Thus the erythrocyte membranes can reflect the inflammatory and oxidative processes of acute pancreatitis.
INTRODUCTION
Acute pancreatitis (AP) is a sudden inflammation of pancreas. About 20%-30% of patients develop severe forms of the disease manifesting with local and systemic complications. Acute pancreatitis carries an overall mortality rate of 10%-15%[1,2]. The main causes of death are associated with multiple organ failure and pancreatic infection[3,4]. The initial process of inflammation starts in the pancreas, but no strict correlation between pancreatic necrosis and organ failure has been reported[5]. Systemic inflammatory response is responsible for multiple organ failure and has the most considerable impact on the severity of acute pancreatitis and mortality from this disease[6].
The role of fatty acids (FAs) in the pathogenesis of AP is important but far from being clear. An increase the total serum free FA level is observed during AP[7]. Unsaturated FAs, especially polyunsaturated FAs (PUFAs), are liberated from pancreatic necrotic tissues and are responsible for the disturbance of FA profile in the serum of patients with AP[7,8]. The increased amount of unsaturated FAs in the necrotic pancreatic tissue and serum during AP is associated with multisystem organ failure and worse outcomes of patients[9]. Moreover, alcohol, an important etiological factor for pancreatitis, has an impact on the FA composition of serum and erythrocyte membranes[10-13]. Surprisingly, during alcohol-induced pancreatitis, the percentage of PUFAs is decreased in the serum FA profile in mild and moderate AP as well as chronic pancreatitis[14,15]. These data suggest that alcohol could play a specific role in the pathogenesis of pancreatitis.
FAs of cell membranes are precursors for lipid mediators and play an important role in the process of inflammation and oxidant status[16]. Experimental findings show that n-3 PUFAs may be beneficial in the prevention of oxidative stress-induced inflammation in pancreatitis[17]. Moreover, it influences the histological severity of AP[18-21]. Human studies also indicate likely clinical benefits of enteral feeding rich in n-3 PUFAs in patients with AP[22].
The aim of our study was to evaluate changes in the FA profile of erythrocyte membrane phospholipids and antioxidant enzymes of erythrocytes in patients with severe and mild AP, also of nonalcoholic etiology separately, in comparison with healthy individuals. We believe that erythrocyte membrane phospholipids can better reflect systemic changes caused by oxidative stress and inflammatory response in patients with AP comparing with FAs in serum, which are greatly influenced by necrotic changes in the pancreas and peripancreatic tissues. To our knowledge, no studies examining the FA composition of erythrocyte membrane phospholipids during AP have been carried out.
MATERIALS AND METHODS
Patients
All consecutive patients with a diagnosis of AP and onset of the disease within the last 72 h admitted to the Departments of Surgery and Gastroenterology at the Hospital of Lithuanian University of Health Sciences between June and December 2007 were included in this study. The diagnosis was established based on acute abdominal pain, at least 3-fold elevated levels of serum amylase, and typical radiological findings. According to the Acute Physiology and Chronic Health Evaluation (APACHE II) scale, the patients were subdivided into the mild (APACHE II score < 7, n = 22) and severe (APACHE II score ≥ 7, n = 17) AP groups. Healthy subjects (n = 26) without a past history of pancreatic diseases were enrolled as controls.
Fatty acid and antioxidant analysis
Peripheral blood samples were drawn from patients on admission to the hospital. Plasma and leukocytes were removed after centrifugation. Erythrocytes were washed and centrifuged twice. The samples were stored at -80 °C until analysis. The blood samples of the control group were subjected to the same procedure.
FA analysis was performed in the Laboratory for Health Protection Research, National Institute for Public Health and the Environment (The Netherlands), as described previously[23]. Briefly, 200 μL of erythrocytes was taken, and phospholipids were washed with distilled water and extracted with chloroform/methanol (1:1). The chloroform layer was evaporated, and the phospholipids were hydrolyzed and methylated simultaneously with BF3/MeOH for 60 min at 100 °C. After extraction with hexane, the methylated FAs (FAME) were separated on a fused silica capillary column using a GC-3900 gas chromatograph with FID detection (Varian Assoc). The baseline separation of more than 50 FAME peaks was accomplished using FAME standards (Sigma) within 57 min. Individual FAs were expressed as percentages of the total FAs present in the chromatogram.
The concentrations of superoxide dismutase (SOD) and glutathione peroxidase (GPx) were measured in erythrocytes on an auto analyzer (LX-20 Pro, Beckman-Coulter, Woerden, Netherlands) with kits from Randox (Ransod and Ransel, Crumlin, United Kingdom).
Peroxidation and unsaturation index
The indexes were calculated according to the formulas used by Viviani et al[24]. The peroxidation index (PI) was determined from the percentages of monoenoic, dienoic, trienoic, tetraenoic, pentaenoic and hexanoic FAs according to the following formula: PI = [(%monoenoic × 0.025) + (%dienoic × 1) + (%trienoic × 2) + (%tetraenoic × 4) + (%pentaenoic × 6) + (%hexanoic × 8)].
The unsaturation index (UI) is also known as the index of hydrogen deficiency. It was calculated from the number of unsaturated double bonds of each FA: UI = [(%monoenoic × 1) + (%dienoic × 2) + (%trienoic × 3) + (%tetraenoic × 4) + (%pentaenoic × 5) + (%hexanoic × 6)].
Ethics
The study was approved by Kaunas Regional Ethics Committee for Biomedical Research (BE-2-47). All patients and healthy subjects provided written informed consent.
Statistical analysis
Statistical analysis was performed using SPSS® for Windows release 14.0 (SPSS, Chicago, IL, United States). The data are presented as mean ± SD. The Mann-Whitney test and one-way and two-way ANOVA tests were applied for analysis of variables. All statistical tests were two sided, and P < 0.05 was considered statistically significant.
RESULTS
The demographic characteristics of patients and controls are presented in Table 1. There was no difference in the FA composition of membrane phospholipids between men and women in the control group (data not shown).
Table 1.
Demographic and clinical data of patients and controls
| AP | Severe AP | Mild AP | Control | |
| Age, mean ± SD, yr | 48.1 ± 15.5 | 50.2 ± 13.7 | 46.7 ± 16.8 | 42.07 ± 16.6 |
| Men | 68% | 64% | 70% | 33% |
| AP etiology | ||||
| Alcoholic | 35% | 36% | 35% | NA |
| Nonalcoholic | 65% | 64% | 65% | NA |
| Death | 6% | 7% | 5% | NA |
Values are percentage unless otherwise stated. NA: Not applicable; AP: Acute pancreatitis.
As shown in Table 2, the percentage of saturated FAs in erythrocyte membrane phospholipids was greater in the patients with AP than the control group. Palmitic acid (C16:0) had a major impact on the increase. The percentages of monounsaturated FAs were also increased, and cis-isomers, especially palmitoleic (C16:1n7cis) and erucic (C22:1n9cis) acids, mostly contributed to the change. We found a decreased percentage of some trans monounsaturated FAs in erythrocyte membrane phospholipids. Those were elaidic (C8:1n9trans) and vaccenic (C18:1n7 trans) acids (Table 2).
Table 2.
Percentages of saturated, monounsaturated and polyunsaturated fatty acids in erythrocyte membrane phospholipids
| AP | Alcoholic AP | Nonalcoholic AP | Control | |
| Saturated fatty acid | ||||
| C14:0 | 0.26 ± 0.06 | 0.26 ± 0.06 | 0.26 ± 0.07 | 0.27 ± 0.06 |
| C15:0 | 0.29 ± 0.05 | 0.27 ± 0.04 | 0.30 ± 0.06 | 0.30 ± 0.05 |
| C16:0 | 23.43 ± 1.12b | 23.80 ± 1.20b | 23.22 ± 1.06b | 22.17 ± 0.85 |
| C17:0 | 0.27 ± 0.06b | 0.23 ± 0.03b | 0.29 ± 0.06 | 0.31 ± 0.03 |
| C18:0 | 13.49 ± 0.70a | 13.40 ± 0.54 | 13.54 ± 0.78 | 13.95 ± 0.70 |
| C20:0 | 0.33 ± 0.10b | 0.28 ± 0.06b | 0.36 ± 0.09 | 0.40 ± 0.06 |
| C21:0 | 0.04 ± 0.04 | 0.04 ± 0.06 | 0.04 ± 0.04 | 0.03 ± 0.03 |
| C22:0 | 1.39 ± 0.33 | 1.15 ± 0.23b | 1.47 ± 0.34 | 1.44 ± 0.26 |
| C23:0 | 0.21 ± 0.06a | 0.17 ± 0.04b | 0.23 ± 0.06 | 0.24 ± 0.04 |
| C24:0 | 4.44 ± 0.80 | 4.30 ± 0.77 | 4.41 ± 0.97 | 4.10 ± 0.73 |
| Total | 44.05 ± 1.47a | 43.90 ± 1.00 | 44.13 ± 1.70 | 43.34 ± 0.90 |
| Monounsaturated fatty acid | ||||
| C16:1n7trans | 0.13 ± 0.02 | 0.12 ± 0.02 | 0.13 ± 0.02 | 0.14 ± 0.02 |
| C16:1n9c | 0.09 ± 0.06b | 0.09 ± 0.03 | 0.09 ± 0.07 | 0.06 ± 0.03 |
| C16:1n7c | 0.56 ± 0.19b | 0.68 ± 0.17b | 0.49 ± 0.17b | 0.33 ± 0.06 |
| C18:1n9trans | 0.11 ± 0.05b | 0.10 ± 0.02b | 0.12 ± 0.06a | 0.16 ± 0.04 |
| C18:1n7trans | 0.28 ± 0.09a | 0.23 ± 0.07b | 0.30 ± 0.09 | 0.33 ± 0.09 |
| C18:1n9c | 13.02 ± 1.49 | 13.53 ± 1.05a | 12.85 ± 1.88 | 12.42 ± 1.12 |
| C18:1n7c | 1.08 ± 0.17 | 1.09 ± 0.15 | 1.07 ± 0.20 | 1.03 ± 0.13 |
| C22:1n9c | 0.22 ± 0.05a | 0.23 ± 0.06a | 0.22 ± 0.05a | 0.18 ± 0.05 |
| C24:1 | 4.98 ± 0.69 | 4.86 ± 0.63 | 4.87 ± 0.86 | 4.58 ± 0.67 |
| Total | 20.49 ± 1.98a | 20.9 3± 1.13a | 20.16 ± 2.29 | 19.31 ± 1.02 |
| PUFA | ||||
| Omega 3 PUFA | 7.84 ± 1.71b | 7.92 ± 1.74a | 7.80 ± 1.74b | 9.45 ± 1.30 |
| C18:3n3 | 0.16 ± 0.05 | 0.18 ± 0.06 | 0.14 ± 0.04 | 0.15 ± 0.03 |
| C20:5n3 | 0.91 ± 0.46 | 0.94 ± 0.46 | 0.82 ± 0.42 | 1.02 ± 0.4 |
| C22:5n3 | 2.21 ± 0.33a | 2.29 ± 0.36 | 2.17 ± 0.32a | 2.39 ± 0.29 |
| C22:6n3 | 4.61 ± 1.12b | 4.50 ± 1.12b | 4.67 ± 1.14b | 5.89 ± 0.81 |
| Omega 6 PUFA | 26.99 ± 1.99 | 26.89 ± 1.40 | 27.51 ± 2.17 | 27.93 ± 1.58 |
| C18:2n6c | 10.16 ± 1.24 | 10.07 ± 1.01 | 10.43 ± 1.43 | 10.18 ± 1.27 |
| C18:3n6 | 0.05 ± 0.02b | 0.05 ± 0.02b | 0.04 ± 0.02a | 0.03 ± 0.01 |
| C20:3n6 | 1.44 ± 0.26a | 1.49 ± 0.27 | 1.41 ± 0.25 | 1.32 ± 0.34 |
| C20:4n6 | 12.94 ± 1.06a | 12.82 ± 0.82a | 13.01 ± 1.18a | 13.64 ± 0.99 |
| C22:4n6 | 2.48 ± 0.58 | 2.46 ± 0.35 | 2.62 ± 0.60 | 2.63 ± 0.50 |
| C16:3n4 | 0.05 ± 0.02a | 0.04 ± 0.02b | 0.06 ± 0.02 | 0.06 ± 0.02 |
| C20:2 | 0.28 ± 0.06a | 0.27 ± 0.05 | 0.29 ± 0.06a | 0.25 ± 0.03 |
| C22:2 | 0.05 ± 0.02 | 0.05 ± 0.01 | 0.06 ± 0.02 | 0.05 ± 0.02 |
| Total PUFA | 35.51 ± 1.95b | 35.17 ± 1.37b | 35.71 ± 2.21b | 37.34 ± 1.30 |
Results are presented as mean ± SD. Percentages of saturated, monounsaturated and polyunsaturated fatty acids (PUFA) in erythrocyte membrane phospholipids in patients with acute pancreatitis (AP) of alcoholic and nonalcoholic etiology.
P < 0.05,
P < 0.01 vs control group.
The percentages of total and n-3 PUFAs were decreased in erythrocyte membrane phospholipids of AP patients. This was particularly caused by the decreased percentages of docosahexaenoic (DHA C22:6n3) and docosapentaenoic (DPA C22:5n3) acids. The percentage of arachidonic acid (AA, C20:4n6) was decreased in the patients with AP comparing with the controls, though the percentages of gama-linoleic (C18:3n6) and dihomo gama linoleic (C20:3n6) acids were increased (Table 2).
A decrease of PI and UI in AP patients as well as the severe and mild AP groups compared with the controls was observed. The extent of change in the indexes in the mild AP group was greater than in the severe AP group compared with controls (Figure 1). The concentrations of SOD and GPx in the mild AP group were lower comparing with the control group (321.55 ± 75.19 μmol/mL and 10059.21 ± 2666.96 U/L vs 384.88 ± 42.21 μmol/mL and 11649.09 ± 1844.75 U/L, P < 0.001 and P < 0.05, respectively). To rule out the impact of alcohol in the changes of FAs in erythrocyte membrane phospholipids of AP patients, we analyzed AP of non-alcoholic etiology (Table 3). In the severe AP group, the percentages of arachidic acid (C20:0) and AA (C20:4n6) were decreased as compared with the control group. In the mild AP group, an increase in the percentages of total saturated FAs and gama linoleic acid (C18:3n6) and a decrease in the percentages of elaidic (C18:1n9t), EPA (C20:5n3), DPA (C22:5n3), DHA (C22:6n3), total PUFAs, and omega 3 PUFAs in erythrocyte membrane phospholipids were recorded. The change in the concentrations of antioxidant enzymes showed the same pattern: they were decreased in patients with mild AP and showed no change in the severe AP group. The changes in the PI and the UI appeared to be greater in the mild AP than severe AP group as compared with the control group.
Figure 1.
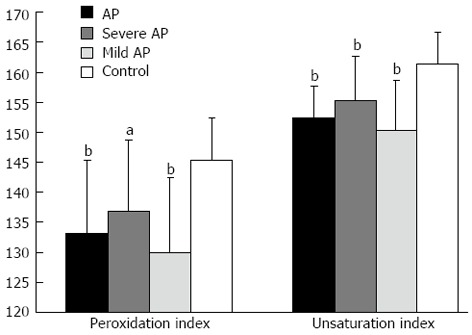
Peroxidation and unsaturation indexes of fatty acids of erythrocyte membrane phospholipids in the acute pancreatitis, severe acute pancreatitis, mild acute pancreatitis, and control groups. A significant decrease of peroxidation index and unsaturation index in acute pancreatitis (AP) patients compared with controls was observed. Bars represent mean values with standard deviation. The extent of change in the indexes in mild AP was greater than in severe AP patients comparing with controls (aP < 0.05, bP < 0.01 vs control group).
Table 3.
Percentages of fatty acids
|
Nonalcoholic |
Control | ||
| Severe AP | Mild AP | ||
| C20:0 | 0.32 ± 0.09d | 0.39 ± 0.09 | 0.40 ± 0.06 |
| C20:4n6 | 12.89 ± 0.83c | 13.09 ± 1.40 | 13.64 ± 0.99 |
| SFA | 43.53 ± 1.29 | 44.54 ± 1.86c | 43.34 ± 0.90 |
| C18:3n6 | 0.04 ± 0.02 | 0.05 ± 0.02c | 0.03 ± 0.01 |
| C18:1n9t | 0.13 ± 0.04 | 0.12 ± 0.07d | 0.16 ± 0.04 |
| C20:5n3 | 1.03 ± 0.56 | 0.67 ± 0.18d | 1.02 ± 0.4 |
| C22:5n3 | 2.28 ± 0.22 | 2.10 ± 0.36c | 2.39 ± 0.29 |
| C22:6n3 | 5.29 ± 1.02 | 4.24 ± 1.05d | 5.89 ± 0.81 |
| n-3 PUFA | 8.76 ± 1.73a | 7.14 ± 1.45d | 9.45 ± 1.30 |
| Total PUFA | 36.87 ± 1.62a | 34.91 ± 2.26d | 37.34 ± 1.30 |
| SOD | 385.37 ± 21.37a | 314.90 ± 86.04d | 384.88 ± 42.21 |
| GPx | 12557.07 ± 2836.06a | 9370.85 ± 2196.13d | 11649.09 ± 1844.75 |
| PI | 138.49 ± 10.34ac | 128.14 ± 10.74d | 146.19 ± 7.08 |
| UI | 156.67 ± 7.28ac | 148.99 ± 8.04d | 161.70 ± 4.90 |
Results are presented as mean ± SD. Percentages of fatty acids in erythrocyte membrane phospholipids, peroxidation and unsaturation indexes, and concentrations of superoxide dismutase (SOD, μmol/mL) and glutathione peroxidase (GPx, U/L) in patients with acute pancreatitis (AP) of nonalcoholic etiology.
P < 0.05 comparing mild and severe AP;
P < 0.05,
P < 0.01 vs control group. PUFA: Polyunsaturated fatty acids; SFA: Saturated fatty acids.
DISCUSSION
This study has analyzed the impact of systemic inflammatory response and oxidative stress on the FA composition of erythrocyte membranes and the concentrations of enzymes in patients with AP. The initial generation of ROS and inflammatory events occur in the pancreas, but systemic changes have a crucial impact on the severity and fatal outcomes of AP[6]. A better understanding of these systemic processes occurring during AP could help identifying new therapeutic treatment options and escaping undesirable complications or fatal outcomes.
In our study, we found that the FA composition of erythrocyte membrane phospholipids was significantly altered during AP compared with controls mainly because of the increased percentages of saturated and monounsaturated acids, namely palmitic and palmitoleic, and a decreased percentage of PUFAs. Contrary, Sztefko et al[7] found that the proportion of saturated and monounsaturated acids was decreased and the proportion of PUFAs was increased in the serum levels of free FAs in patients with AP. An increase in the percentage of PUFAs in the necrotic pancreatic tissue has also been reported[8]. On the other hand, in severe sepsis, a similar pathology with systemic inflammatory response syndrome, the lower proportions of PUFAs and the greater proportions of monounsaturated FAs in erythrocyte phospholipids have been documented[25]. These findings suggest that the FA composition of erythrocyte membrane phospholipids may reflect not only the direct events in the pancreas, but also the systemic response syndrome during AP.
Alcohol consumption can be associated with the higher percentages of saturated and monounsaturated FAs, such as palmitic and oleic acids, and the lower percentages of PUFAs, especially DHAs and arachidonic acid, in serum and membranes[10-13]. Alcoholics have also been show to have a disturbed oxidant status of plasma and erythrocyte enzymes[26-28]. In the study by Khan et al[14], the authors showed the increased percentages of saturated palmitic and monounsaturated FAs as well as the decreased percentages of some PUFAs in serum of patients with alcohol-induced AP comparing with alcoholic controls. Moreover, Gabianelli et al[29] reported that ethanol can have a direct toxic effect on erythrocyte membranes and antioxidant systems of the cells. These findings indicate that alcohol may have an impact on the FA composition of erythrocyte membrane phospholipids. Thus, the increased percentages of saturated and monounsaturated FAs in our study could partly be explained by etiological factors, most probably alcohol.
To rule out the impact of alcohol and to study the influence of inflammatory and oxidative processes during AP on the phospholipid composition of erythrocyte membranes, we analyzed patients with AP of nonalcoholic etiology. The PUFAs of cell membranes are precursors for prostaglandins and other lipid mediators of inflammatory process[16]. Arachidonic acid is the main proinflammatory actor. Meanwhile, EPA, DHA, and possibly DPA are precursors for products with anti-inflammatory and proresolving functions[30,31]. We found that in the severe AP group, the percentage of proinflammatory arachidonic acid was significantly decreased, and in the mild AP group, a decrease in the percentages of anti-inflammatory players (EPA, DHA, and DPA) was seen as compared with controls. It is now thought that saturated FAs could also be involved in the inflammatory process[32,33]. We also found a significant increase in the percentage of total saturated FAs in the mild but not severe AP group. Erythrocytes are not usually considered to be active players in the inflammatory process, but our study showed that the changes in the percentage of FAs in erythrocyte membrane phospholipids were different during mild and severe AP, therefore, we hypothesize that the composition of erythrocyte membrane phospholipids may reflect the inflammatory processes and the severity of the disease.
Oxidative stress plays a central role in the development of pancreatic inflammation and extra pancreatic complications[34-36]. The changes of the FA composition of erythrocyte membrane phospholipids could be affected from “the outside” as PUFAs of erythrocyte membrane phospholipids are extremely sensitive to oxidation[37]. SOD and GPx are important components of enzymatic antioxidant defense[37]. We found that the levels of antioxidant enzymes in erythrocytes were also altered significantly in the mild but not severe AP group comparing with controls. There were significant differences in the PI and the UI mainly because of the different percentage of PUFAs in erythrocyte membrane phospholipids in the severe and mild AP groups comparing with controls. Moreover, there was a significant difference between the severe and mild AP groups. This suggests that oxidative stress might be involved in the changes of the FA composition of erythrocyte membrane phospholipids and systemic inflammatory response.
It was unexpected to find the changes of PI and UI to be more apparent in the mild AP than severe AP group comparing with controls. It is known that systemic response followed by organ failure influences the severity and outcome of AP more than the events in the pancreas itself[5]. The similar phenomenon was also noticed in cytokine expression during mild and severe AP[38]. We hypothesize that these findings could reflect the disproportion of pro- and anti-inflammatory processes during severe AP possibly associated with oxidative stress. The mechanisms of these processes are still not clear and remain to be elucidated.
The composition of FAs in erythrocyte membranes is altered during AP. These changes are likely to be associated with alcohol intake as an etiological factor for AP, and systemic inflammatory processes and oxidative stress after the onset of the disease could influence the changes.
COMMENTS
Background
Acute pancreatitis carries an overall mortality rate of 10%-15%. Systemic inflammatory response has the most considerable impact on the severity of acute pancreatitis and mortality from this disease. Fatty acids of cell membranes are precursors for lipid mediators and play an important role in the process of inflammation and oxidant status. Erythrocyte membrane phospholipids can reflect systemic changes caused by oxidative stress and inflammatory response in patients with acute pancreatitis.
Research frontiers
The role of fatty acids in the pathogenesis of acute pancreatitis is important but far from being clear. Fatty acids are the components of membrane phospholipids. They are responsible for inflammatory and oxidative processes. Free fatty acids in serum are associated with necrotic lesions in the pancreas and peripancreatic tissues. Moreover, alcohol, an important etiological factor for pancreatitis, has an impact on the fatty acid composition of serum and erythrocyte membranes.
Innovations and breakthroughs
The earlier studies of alterations in the fatty acid composition during acute pancreatitis mainly investigated the fatty acid composition in serum that is greatly influenced by necrotic changes in the pancreas and peripancreatic tissues. Authors believe that erythrocyte membrane phospholipids can better reflect systemic changes caused by oxidative stress and inflammatory response as well as alcohol impact in patients with acute pancreatitis. To the knowledge, no studies examining the fatty acid composition of membranes during acute pancreatitis have bee carried out.
Applications
This study elucidates the pathogenesis of acute pancreatitis, especially the systemic and oxidative processes that are of high importance in the severity of acute pancreatitis and mortality from this disease.
Terminology
Fatty acids are the components of phospholipids that form the lipid bilayers of cell membranes. Fatty acids of membranes are precursors for lipid mediators of inflammatory response syndrome. Oxidative stress is a disturbance of the pro-oxidant-antioxidant balance in favor of the former, leading to potential damage, and is associated with many chronic and acute inflammatory conditions.
Peer review
This study evaluates changes in fatty acids of erythrocyte membrane phospholipids during mild and severe acute pancreatitis, of alcohol and non-alcohol etiology. The study is a prospective one and Acute Physiology and Chronic Health Evaluation II score was used to classify patients into mild (n = 22 patients) and severe (n = 17 patients). Some 26 healthy individuals were enrolled as control. This is a well conducted prospective study, and to my knowledge this is the first study that examines the fatty acid profile of the erythrocyte membrane in acute pancreatitis.
Footnotes
P- Reviewers Abdul-Wahed M, Bramhall SR, Naoaki S S- Editor Gou SX L- Editor A E- Editor Zhang DN
References
- 1.Yousaf M, McCallion K, Diamond T. Management of severe acute pancreatitis. Br J Surg. 2003;90:407–420. doi: 10.1002/bjs.4179. [DOI] [PubMed] [Google Scholar]
- 2.Toouli J, Brooke-Smith M, Bassi C, Carr-Locke D, Telford J, Freeny P, Imrie C, Tandon R. Guidelines for the management of acute pancreatitis. J Gastroenterol Hepatol. 2002;17 Suppl:S15–S39. doi: 10.1046/j.1440-1746.17.s1.2.x. [DOI] [PubMed] [Google Scholar]
- 3.Petrov MS, Shanbhag S, Chakraborty M, Phillips AR, Windsor JA. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology. 2010;139:813–820. doi: 10.1053/j.gastro.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Rau BM, Bothe A, Kron M, Beger HG. Role of early multisystem organ failure as major risk factor for pancreatic infections and death in severe acute pancreatitis. Clin Gastroenterol Hepatol. 2006;4:1053–1061. doi: 10.1016/j.cgh.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 5.Lankisch PG, Pflichthofer D, Lehnick D. No strict correlation between necrosis and organ failure in acute pancreatitis. Pancreas. 2000;20:319–322. doi: 10.1097/00006676-200004000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Kylänpää ML, Repo H, Puolakkainen PA. Inflammation and immunosuppression in severe acute pancreatitis. World J Gastroenterol. 2010;16:2867–2872. doi: 10.3748/wjg.v16.i23.2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sztefko K, Panek J. Serum free fatty acid concentration in patients with acute pancreatitis. Pancreatology. 2001;1:230–236. doi: 10.1159/000055816. [DOI] [PubMed] [Google Scholar]
- 8.Panek J, Sztefko K, Drozdz W. Composition of free fatty acid and triglyceride fractions in human necrotic pancreatic tissue. Med Sci Monit. 2001;7:894–898. [PubMed] [Google Scholar]
- 9.Navina S, Acharya C, DeLany JP, Orlichenko LS, Baty CJ, Shiva SS, Durgampudi C, Karlsson JM, Lee K, Bae KT, et al. Lipotoxicity causes multisystem organ failure and exacerbates acute pancreatitis in obesity. Sci Transl Med. 2011;3:107ra110. doi: 10.1126/scitranslmed.3002573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stark KD, Beblo S, Murthy M, Whitty JE, Buda-Abela M, Janisse J, Rockett H, Martier SS, Sokol RJ, Hannigan JH, et al. Alcohol consumption in pregnant, black women is associated with decreased plasma and erythrocyte docosahexaenoic acid. Alcohol Clin Exp Res. 2005;29:130–140. doi: 10.1097/01.alc.0000150013.65416.06. [DOI] [PubMed] [Google Scholar]
- 11.Simon JA, Fong J, Bernert JT, Browner WS. Relation of smoking and alcohol consumption to serum fatty acids. Am J Epidemiol. 1996;144:325–334. doi: 10.1093/oxfordjournals.aje.a008933. [DOI] [PubMed] [Google Scholar]
- 12.Maturu P, Varadacharyulu N. Adaptive changes in fatty acid profile of erythrocyte membrane in relation to plasma and red cell metabolic changes in chronic alcoholic men. Hum Exp Toxicol. 2012;31:652–661. doi: 10.1177/0960327111432504. [DOI] [PubMed] [Google Scholar]
- 13.di Giuseppe R, de Lorgeril M, Salen P, Laporte F, Di Castelnuovo A, Krogh V, Siani A, Arnout J, Cappuccio FP, van Dongen M, et al. Alcohol consumption and n-3 polyunsaturated fatty acids in healthy men and women from 3 European populations. Am J Clin Nutr. 2009;89:354–362. doi: 10.3945/ajcn.2008.26661. [DOI] [PubMed] [Google Scholar]
- 14.Khan J, Solakivi T, Seppänen H, Lappalainen-Lehto R, Järvinen S, Ronkainen J, Sand J, Nordback I. Serum lipid and fatty acid profiles are highly changed in patients with alcohol induced acute pancreatitis. Pancreatology. 2012;12:44–48. doi: 10.1016/j.pan.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Marosvolgyi T, Horvath G, Dittrich A, Cseh J, Lelovics Z, Szabo E, Decsi T, Figler M. Fatty acid composition of plasma lipid classes in chronic alcoholic pancreatitis. Pancreatology. 2010;10:580–585. doi: 10.1159/000289466. [DOI] [PubMed] [Google Scholar]
- 16.Kremmyda LS, Tvrzicka E, Stankova B, Zak A. Fatty acids as biocompounds: their role in human metabolism, health and disease: a review. part 2: fatty acid physiological roles and applications in human health and disease. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2011;155:195–218. doi: 10.5507/bp.2011.052. [DOI] [PubMed] [Google Scholar]
- 17.Park KS, Lim JW, Kim H. Inhibitory mechanism of omega-3 fatty acids in pancreatic inflammation and apoptosis. Ann N Y Acad Sci. 2009;1171:421–427. doi: 10.1111/j.1749-6632.2009.04887.x. [DOI] [PubMed] [Google Scholar]
- 18.Kilian M, Heukamp I, Gregor JI, Schimke I, Kristiansen G, Wenger FA. Fish oil, but not soy bean or olive oil enriched infusion decreases histopathological severity of acute pancreatitis in rats without affecting eicosanoid synthesis. Inflammation. 2011;34:597–602. doi: 10.1007/s10753-010-9267-3. [DOI] [PubMed] [Google Scholar]
- 19.Kilian M, Gregor JI, Heukamp I, Wagner C, Walz MK, Schimke I, Kristiansen G, Wenger FA. Early inhibition of prostaglandin synthesis by n-3 fatty acids determinates histologic severity of necrotizing pancreatitis. Pancreas. 2009;38:436–441. doi: 10.1097/MPA.0b013e318198283b. [DOI] [PubMed] [Google Scholar]
- 20.Weylandt KH, Nadolny A, Kahlke L, Köhnke T, Schmöcker C, Wang J, Lauwers GY, Glickman JN, Kang JX. Reduction of inflammation and chronic tissue damage by omega-3 fatty acids in fat-1 transgenic mice with pancreatitis. Biochim Biophys Acta. 2008;1782:634–641. doi: 10.1016/j.bbadis.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kilian M, Heukamp I, Gregor JI, Bretthauer C, Walz MK, Jacobi CA, Lochs H, Schimke I, Guski H, Wenger FA. n-3, n-6, and n-9 polyunsaturated fatty acids--which composition in parenteral nutrition decreases severity of acute hemorrhagic necrotizing pancreatitis in rats? Int J Colorectal Dis. 2006;21:57–63. doi: 10.1007/s00384-004-0724-z. [DOI] [PubMed] [Google Scholar]
- 22.Lasztity N, Hamvas J, Biró L, Németh E, Marosvölgyi T, Decsi T, Pap A, Antal M. Effect of enterally administered n-3 polyunsaturated fatty acids in acute pancreatitis--a prospective randomized clinical trial. Clin Nutr. 2005;24:198–205. doi: 10.1016/j.clnu.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 23.Kröger J, Zietemann V, Enzenbach C, Weikert C, Jansen EH, Döring F, Joost HG, Boeing H, Schulze MB. Erythrocyte membrane phospholipid fatty acids, desaturase activity, and dietary fatty acids in relation to risk of type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Am J Clin Nutr. 2011;93:127–142. doi: 10.3945/ajcn.110.005447. [DOI] [PubMed] [Google Scholar]
- 24.Viviani Anselmi C, Ferreri C, Novelli V, Roncarati R, Bronzini R, Marchese G, Somalvico F, Condorelli G, Montenero AS, Puca AA. Fatty acid percentage in erythrocyte membranes of atrial flutter/fibrillation patients and controls. J Interv Card Electrophysiol. 2010;27:95–99. doi: 10.1007/s10840-009-9466-8. [DOI] [PubMed] [Google Scholar]
- 25.Novák F, Borovská J, Vecka M, Vávrová L, Kodydková J, Mrácková M, Novák F, Nováková O, Zák A. [Alterations in fatty acid composition of plasma and erythrocyte lipids in critically ill patients during sepsis] Cas Lek Cesk. 2010;149:324–331. [PubMed] [Google Scholar]
- 26.Woźniak B, Musiałkiewicz D, Woźniak A, Drewa G, Drewa T, Drewa S, Mila-Kierzenkowska C, Porzych M, Musiałkiewicz M. Lack of changes in the concentration of thiobarbituric acid-reactive substances (TBARS) and in the activities of erythrocyte antioxidant enzymes in alcohol-dependent patients after detoxification. Med Sci Monit. 2008;14:CR32–CR36. [PubMed] [Google Scholar]
- 27.Bogdanska J, Todorova B, Labudovic D, Korneti PG. Erythrocyte antioxidant enzymes in patients with alcohol dependence syndrome. Bratisl Lek Listy. 2005;106:107–113. [PubMed] [Google Scholar]
- 28.Uçar G, Demir B, Uluğ B. Lipid peroxidation and antioxidant enzyme activities in erythrocytes of type I and II alcoholics. Cell Biochem Funct. 2005;23:29–37. doi: 10.1002/cbf.1125. [DOI] [PubMed] [Google Scholar]
- 29.Gabbianelli R, Cifani C, Massi M, Polidori C, Falcioni G. Oxidative damage in rat erythrocyte membranes following ethanol intake: effect of ethyl pyruvate. Chem Biol Interact. 2007;169:122–131. doi: 10.1016/j.cbi.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Bannenberg G, Serhan CN. Specialized pro-resolving lipid mediators in the inflammatory response: An update. Biochim Biophys Acta. 2010;1801:1260–1273. doi: 10.1016/j.bbalip.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Calder PC. Polyunsaturated fatty acids and inflammatory processes: New twists in an old tale. Biochimie. 2009;91:791–795. doi: 10.1016/j.biochi.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 32.Wong SW, Kwon MJ, Choi AM, Kim HP, Nakahira K, Hwang DH. Fatty acids modulate Toll-like receptor 4 activation through regulation of receptor dimerization and recruitment into lipid rafts in a reactive oxygen species-dependent manner. J Biol Chem. 2009;284:27384–27392. doi: 10.1074/jbc.M109.044065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee JY, Sohn KH, Rhee SH, Hwang D. Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. J Biol Chem. 2001;276:16683–16689. doi: 10.1074/jbc.M011695200. [DOI] [PubMed] [Google Scholar]
- 34.Bergamini CM, Gambetti S, Dondi A, Cervellati C. Oxygen, reactive oxygen species and tissue damage. Curr Pharm Des. 2004;10:1611–1626. doi: 10.2174/1381612043384664. [DOI] [PubMed] [Google Scholar]
- 35.Jaworek J, Szklarczyk J, Jaworek AK, Nawrot-Porąbka K, Leja-Szpak A, Bonior J, Kot M. Protective effect of melatonin on acute pancreatitis. Int J Inflam. 2012;2012:173675. doi: 10.1155/2012/173675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leung PS, Chan YC. Role of oxidative stress in pancreatic inflammation. Antioxid Redox Signal. 2009;11:135–165. doi: 10.1089/ars.2008.2109. [DOI] [PubMed] [Google Scholar]
- 37.Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39:44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 38.Dambrauskas Z, Giese N, Gulbinas A, Giese T, Berberat PO, Pundzius J, Barauskas G, Friess H. Different profiles of cytokine expression during mild and severe acute pancreatitis. World J Gastroenterol. 2010;16:1845–1853. doi: 10.3748/wjg.v16.i15.1845. [DOI] [PMC free article] [PubMed] [Google Scholar]


