Abstract
Background
Little is known about factors associated with systemic corticosteroid (SC) use in emergency department (ED) patients with acute asthma.
Objective
To determine the patient and system factors associated with delayed use or nonuse of SCs in the ED.
Methods
We analyzed the asthma component of the National Emergency Department Safety Study. Patients with acute asthma in 62 urban EDs in 23 US states between 2003 and 2006 were identified. The primary outcome measure was the pattern of SC use in the ED, which was categorized as timely use (≤60 minutes), delayed use (>60 minutes), or nonuse. Multinomial logistic regression was performed to identify factors associated with delayed use or nonuse of SCs.
Results
A total of 2,559 of 3,798 patients with acute asthma (67.4%) received SCs. Of these, the median door-to-SC time was 62 minutes (interquartile range, 35–100 minutes), with 1,319 patients (51.5%) having delayed SC treatment. Nonuse of SCs was largely explained by markers of asthma exacerbations (never intubated for asthma, lower respiratory rate, and higher oxygen saturation). In contrast, in addition to these factors, delayed SC treatment was associated with age of 40 years or older, female sex, longer duration of symptoms, ED presentation between 8 AM and 11:59 PM, and ED with a longer average patient wait time.
Conclusions
Physicians in the ED seem to appropriately administer SCs to higher-acuity asthmatic patients; however, the additional nonmedical factors represent opportunities to improve the timeliness of SC treatment in the ED.
INTRODUCTION
Acute asthma is a common presentation to the emergency department (ED), accounting for approximately 2 million ED visits each year.1 One of the primary and evidence-based therapies for acute asthma in the acute setting is systemic corticosteroids (SCs). Most asthma guidelines suggest that SCs be given to patients who have moderate to severe asthma exacerbations.2,3 Furthermore, although corticosteroids are traditionally thought to exert their effect over hours rather than minutes, there is theoretical and clinical evidence of acute treatment effects.4 – 6 A meta-analysis7 summarizing 12 randomized trials has shown that the use of SC within 1 hour of ED arrival significantly improves pulmonary function and reduces the odds of hospital admission by 60%. The evidence also suggests little benefit for higher doses8 or for intravenous treatment.7 Consequently, prompt administration of SCs in the ED may have greater benefits than delayed use.
Previous studies have reported that approximately 60% to 70% of ED patients with asthma exacerbations receive SC treatment in the ED9,10 and that among those who receive SCs, there often is a delay in delivery.10 Little is known, however, about factors associated with the pattern of SC use (ie, delayed use or nonuse) in ED patients with acute asthma. Understanding the determinants of delayed use or nonuse of SCs may help identify important opportunities for improving timely and appropriate use of SCs in acute asthma. In particular, if factors that are not medically justified are identified, interventions should be implemented to minimize these factors. Using data from a large multicenter study, we sought to determine the patient and system factors associated with delayed use or nonuse of SCs in ED patients with acute asthma.
METHODS
Study Design and Setting
This retrospective cohort study was part of the National Emergency Department Safety Study (NEDSS), a large multicenter study that sought to characterize organizational- and physician-related factors associated with the occurrence of errors in EDs. Details of the study design and data collection have been published previously.11 Three clinical conditions were examined in the NEDSS, including acute myocardial infarction, dislocations, and acute asthma. The present analysis used the asthma component.10
The NEDSS was coordinated by the Emergency Medicine Network (EMNet) (http://www.emnetusa.org). The NEDSS recruited EDs by directly inviting sites affiliated with EMNet; EDs not yet affiliated with EMNet were invited through postings on emergency medicine listservs and presentations at national emergency medicine meetings. The NEDSS excluded military hospitals, Veterans Affairs hospitals, children’s hospitals, and hospitals in US territories. The institutional review boards at all participating hospitals approved the study. A total of 63 US EDs in 23 US states completed the asthma component of the NEDSS.
Inclusion and Exclusion Criteria
Using a standardized data abstraction tool, trained research personnel at each site abstracted data from 70 randomly selected ED visits for acute asthma during a 12-month period in 2003 to 2006. Sites with less than 70 medical records reviewed all eligible medical records. The visits were identified by using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 493.xx. The ICD-10 codes were not yet implemented in the United States during the study period. The inclusion criteria were age of 14 to 54 years and a history of asthma before the index visit. The following visits were excluded: repeated visits; transfer visits; patient visits with a history of chronic obstructive pulmonary disease, emphysema, or chronic bronchitis; or visits not prompted, in large part, by asthma exacerbation. The final sample consisted of 4,053 visits from 63 EDs.
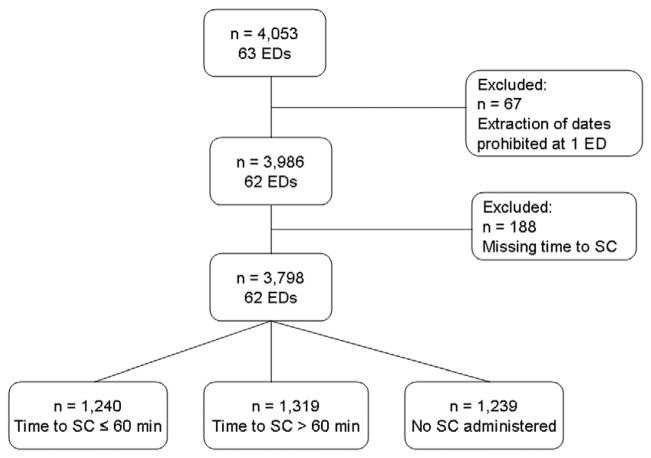
Because one site was prohibited by its institutional review board to document dates (including date of birth), for the purpose of this time-related analysis, this site was omitted from the analysis (n = 67). We further excluded patients who received SCs in the ED but the times to SC treatment were not documented (n = 188). The patient flow is illustrated in Figure 1.
Figure 1.
Patient flow. ED indicates emergency department; SC, systemic corticosteroid.
Data Collection and Processing
Data abstracted included baseline patient characteristics, asthma history, details of ED presentation, ED provider type, ED management, and ED disposition. The timing of ED arrival and ED treatments also were collected from medical records. The time of ED arrival was defined as the earliest documented time in the medical record, which may be the time of triage (most), the time of registration, or the time of arrival in the ambulance notes. This definition is consistent with the consensus on ED performance measures,12 which defines the arrival time as the time that the patient first is recognized and recorded by the ED system. Treatment with SCs included oral, intravenous, or intramuscular administration. Peak expiratory flow (PEF) was recorded in liters per minute and is expressed as the absolute value; no predicted values are presented because of infrequent recording of the patient’s height in ED medical records. Severity of acute asthma was classified according to the initial PEF as follows: mild, 300 L/min or greater for women and 400 L/min or greater for men; moderate, 200 to 299 L/min for women and 250 to 399 L/min for men; severe, 120 to 199 L/min for women and 150 to 249 L/min for men; and very severe, less than 120 L/min for women and less than 150 L/min for men. The absolute PEF cutoff values represented approximately 70%, 40%, and 25% of predicted, respectively, for typical adult women and men.13
We also distributed a key informant survey at each site to collect data on ED characteristics such as annual visit volume. A few variables related to ED crowding were collected, such as average patient wait times in the past year and the presence of an ED policy on ambulance diversion. Geographic regions (Northeast, South, Midwest, and West) were defined according to US Census Bureau boundaries.14
Outcome Measures
The time to SC treatment was calculated from the documented date and time of ED arrival to the documented date and time of first administration of SCs in the ED. Based on the cutoff time suggested by the systematic review,7 delayed SC treatment was defined as a time to SC treatment greater than 60 minutes. The primary outcome measure was the pattern of SC use in the ED, which was categorized as timely use (time to SC treatment ≤60 minutes), delayed use (time to SC treatment >60 minutes), and nonuse.
Statistical Analysis
Summary statistics at the patient and ED levels are presented as proportions (with 95% confidence intervals [CIs]) or as medians (with interquartile ranges [IQRs]). The univariable associations between pattern of SC use and other variables were analyzed using χ2, Fisher exact, and Kruskal-Wallis tests, as appropriate. Multivariable multinomial logistic regression was performed to identify patient and ED characteristics independently associated with delayed use or nonuse of SCs compared with timely use. Model variables were selected a priori15 or from variables associated with the pattern of SC use at P<.10 in univariable analyses.16 These variables included age, sex, race/ethnicity, ever intubated or ventilated for asthma, long-term use of oral corticosteroids, time from symptom onset to ED presentation, time of ED presentation, recent upper respiratory tract infection, initial respiratory rate, initial oxygen saturation, initial PEF, calendar year, and the following 6 ED characteristics: number of beds in the ED, annual visit volume, region, affiliation with an emergency medicine residency program, average patient wait times in the past year, and the presence of an ED policy on ambulance diversion. Variables with missing data (race/ethnicity and PEF) were dummy coded using the missing indicator method.17 We tested for a priori 2-way interaction by multiplying the 2 factors of interest and including an interaction term in the final multivariable model. To account for the potential effects of clustering of patients within EDs, the multivariable analyses were performed by specifying the cluster option to obtain robust estimates of standard errors. This method is statistically equivalent to fitting models using generalized estimating equations with an independence working covariance matrix.18 All analyses were performed using a software program (Stata v10.0; StataCorp LLP, College Station, Texas). All odds ratios are presented with 95% CIs.
Subgroup and Sensitivity Analyses
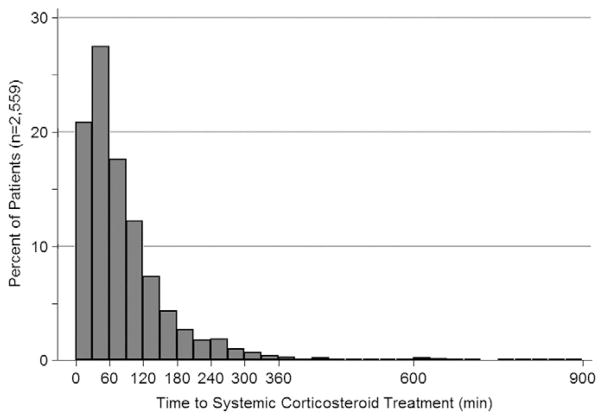
We performed subgroup and sensitivity analyses in patients who received SCs in the ED. We plotted the distribution of the interval from ED arrival to SC administration. We modeled time to SC treatment as a continuous variable to identify factors associated with a longer time to SC treatment. Because the distribution of time to SC treatment was skewed, we log transformed this variable for performing linear regression and converted back to the original values using geometric means for presenting the results.19 The linear regression model included the same covariates as the multinomial logistic regression model in the main analysis.
RESULTS
ED Characteristics
The EDs in this study were all urban but were located in different geographic regions of the country. Most of them were affiliated with an emergency medicine residency program and had a policy that allowed ambulance diversion. There were no statistically significant differences in ED characteristics according to SC use except that patients with delayed use of SCs were more likely to be treated in EDs with more beds and a slightly longer average patient wait time.
Patient Characteristics
Of the 3,798 patients with acute asthma from the 62 EDs, 2,559 (67.4%) received SC treatment in the ED. Figure 2 shows the patient distribution of the times to ED treatment with SCs. In those who received SC treatment, the median door-to-SC time was 62 minutes (IQR, 35–100 minutes), with 1,319 patients (51.5%) having delayed SC treatment according to the 1-hour cutoff time.
Figure 2.
Distribution of the time from emergency department arrival to systemic corticosteroid treatment.
Overall, the median age of these patients was 34 years (IQR, 24 – 43 years); 64% were women and 46% were black. Table 1 displays the patient and ED characteristics according to the pattern of SC use in the ED. Patients with delayed use of SCs were slightly older and were more likely to be women, but no racial/ethnic differences in SC use were observed. Patients with timely use of SCs had more severe chronic asthma, as reflected by higher numbers of admissions and ED visits and a higher chance of being intubated for asthma in the past. Patients with timely use of SCs also had more severe acute asthma, as suggested by higher respiratory rates, lower oxygen saturation values, and lower PEF at ED presentation. Patients with delayed use of SCs were more likely to present to the ED (1) later after symptom onset and (2) between 8 AM to 11:59 PM. Regarding ED outcomes, the ED length of stay was longer in the group with delayed SC use. Patients with no SC use were more likely to be discharged from the ED.
Table 1.
Patient and ED Characteristics
| Characteristic | Timely use of SCs (n = 1,240) | Delayed use of SCs (n = 1,319) | Nonuse of SCs (n = 1,239) | P value |
|---|---|---|---|---|
| Demographic Factors | ||||
| Age, median (IQR), y | 34 (24–43) | 35 (25–44) | 32 (22–42) | <.001 |
| Female sex, % | 62 | 67 | 64 | .03 |
| Race/ethnicity, %a | .054 | |||
| White | 35 | 33 | 33 | |
| Black | 47 | 48 | 45 | |
| Hispanic | 16 | 15 | 19 | |
| Other | 2 | 4 | 3 | |
| Chronic Asthma Factors | ||||
| Admitted for asthma in past year, % | 13 | 8 | 6 | <.001 |
| ED visit for asthma in past year, % | 27 | 26 | 18 | <.001 |
| Ever intubated or ventilated for asthma, % | 13 | 7 | 5 | <.001 |
| ED Presentation | ||||
| Time from symptom onset to ED presentation, % | <.001 | |||
| <1 d | 40 | 26 | 42 | |
| 1–3 d | 42 | 45 | 35 | |
| 4–7 d | 11 | 16 | 12 | |
| >7 d | 7 | 12 | 10 | |
| Time of ED presentation, % | <.001 | |||
| Midnight to 7:59 AM | 29 | 17 | 22 | |
| 8 AM to 3:59 PM | 36 | 40 | 41 | |
| 4 PM to 11:59 PM | 36 | 43 | 37 | |
| Initial respiratory rate, median (IQR), breaths/min | 24 (20–26) | 20 (18–24) | 20 (18–24) | <.001 |
| Initial oxygen saturation, median (IQR), % | 97 (94–99) | 97 (95–99) | 98 (96–99) | <.001 |
| Initial PEF, median (IQR), L/minb | 220 (150–300) | 240 (165–300) | 270 (200–350) | <.001 |
| Severity based on initial PEF, %bc | <.001 | |||
| Mild | 17 | 21 | 33 | |
| Moderate | 37 | 38 | 43 | |
| Severe | 32 | 31 | 20 | |
| Very severe | 14 | 10 | 5 | |
| ED Outcomes | ||||
| ED length of stay, median (IQR), min | 152 (105–240) | 218 (152–315) | 145 (92–231) | <.001 |
| ED disposition, % | <.001 | |||
| Sent home | 73 | 78 | 87 | |
| Admission (hospital ward/observation unit) | 21 | 19 | 9 | |
| ICU admission | 3 | 1 | 1 | |
| Other (eg, left against medical advice) | 3 | 2 | 3 | |
| ED Characteristics | ||||
| Urban location, % | 100 | 100 | 100 | NA |
| Census region, % | .05 | |||
| Northeast | 39 | 44 | 43 | |
| Midwest | 30 | 25 | 25 | |
| South | 12 | 12 | 12 | |
| West | 20 | 19 | 21 | |
| Residency affiliated, % | 75 | 79 | 76 | .07 |
| ED visits per year, median (IQR), No. | 60,000 (45,000–75,595) | 60,000 (45,000–74,416) | 55,100 (43,000–74,416) | .08 |
| ED visits for asthma per year, median (IQR), No. | 1,020 (511–1,825) | 1,020 (511–1,767) | 1,011 (511–1,663) | .78 |
| ED beds, median (IQR), No. | 39 (27–50) | 40 (28–50) | 39 (27–46) | .002 |
| Had a policy that allowed ambulance diversion, % | 94 | 94 | 94 | .98 |
| Average patient wait times in the past year, median (IQR), min | 60 (34–100) | 60 (46–120) | 60 (45–120) | <.001 |
Abbreviations: ED, emergency department; ICU, intensive care unit; IQR, interquartile range; NA, not applicable; PEF, peak expiratory flow; SC, systemic corticosteroid.
Documented for 2,427 patients.
Documented for 1,735 patients.
See the “Methods” section of the text for details on classification.
Multivariable Analyses
Table 2 lists patient and ED characteristics significantly associated with delayed use or nonuse of SCs in the multivariable analyses. Patient factors independently associated with delayed SC treatment included age of 40 years or older, female sex, never intubated for asthma, longer duration of symptoms, ED presentation between 8 AM and 11:59 PM, lower respiratory rate, and higher oxygen saturation. The only significant ED factor associated with delayed SC treatment was average patient wait times in the past year.
Table 2.
Multivariable Multinomial Logistic Model of Factors Associated With Delayed Use or Nonuse of SCs in Emergency Department Patients With Acute Asthma
| Variable | Adjusted OR (95% CI)a
|
||
|---|---|---|---|
| Timely use of SCs | Delayed use of SCs | Nonuse of SCs | |
| Age group, y | NS | ||
| 14–19 | 1.0 | 1 [Reference] | |
| 20–29 | 1.0 | 1.3 (0.9–1.7) | |
| 30–39 | 1.0 | 1.3 (0.9–1.6) | |
| 40–49 | 1.0 | 1.4 (1.02–1.9) | |
| 50–54 | 1.0 | 1.4 (1.02–2.0) | |
| Female sex | 1.0 | 1.2 (1.02–1.5) | NS |
| Ever intubated or ventilated for asthma | 1.0 | 0.5 (0.4–0.7) | 0.5 (0.3–0.7) |
| Time from symptom onset to ED presentation | |||
| <1 d | 1.0 | 1 [Reference] | 1 [Reference] |
| 1–3 d | 1.0 | 1.4 (1.2–1.8) | 0.7 (0.6–0.8) |
| 4–7 d | 1.0 | 1.8 (1.3–2.4) | 0.9 (0.6–1.2) |
| >7 d | 1.0 | 2.2 (1.5–3.1) | 1.1 (0.8–1.6) |
| Time of ED presentation, % | |||
| Midnight to 7:59 AM | 1.0 | 1 [Reference] | 1 [Reference] |
| 8 AM to 3:59 PM | 1.0 | 1.9 (1.5–2.4) | 1.5 (1.1–2.0) |
| 4 PM to 11:59 PM | 1.0 | 2.0 (1.6–2.4) | 1.5 (1.2–2.9) |
| Initial respiratory rate, per increase in 5 breaths/min | 1.0 | 0.7 (0.7–0.8) | 0.6 (0.6–0.7) |
| Initial oxygen saturation, per increase of 5% | 1.0 | 1.2 (1.02–1.3) | 2.1 (1.8–2.4) |
| Initial PEF, per increase of 100 L/min | 1.0 | NS | 1.3 (1.1–1.5) |
| Average patient ED wait times, per 30-min increase | 1.0 | 1.05 (1.0003–1.1) | NS |
Abbreviations: CI, confidence interval; ED, emergency department; NS, not significant; OR, odds ratio; PEF, peak expiratory flow; SC, systemic corticosteroid.
The multivariable model was adjusted for age, sex, race/ethnicity, ever intubated or ventilated for asthma, chronic use of oral corticosteroids, time from symptom onset to ED presentation, time of ED presentation, recent upper respiratory tract infection, initial respiratory rate, initial oxygen saturation, initial PEF, calendar year, and the following 6 ED characteristics: number of beds in the ED, annual visit volume, region, affiliation with an emergency medicine residency program, average patient wait times in the past year, and the presence of an ED policy on ambulance diversion. The table shows only statistically significant predictors of either delayed use or nonuse of SCs in the multivariable model.
The nonuse of SCs was largely explained by markers of less severe exacerbations, including never intubated for asthma, lower respiratory rate, higher oxygen saturation, and higher PEF. There were no statistically significant interactions in the multivariable model.
Subgroup and Sensitivity Analyses
In patients who received SCs in the ED, modeling door-to-SC time as a continuous variable did not materially change the results. For example, the adjusted geometric mean of time to SC treatment was significantly longer for patients presenting to the ED between 4 PM and 11:59 PM (65 minutes; 95% CI, 60 –70 minutes) compared with those presenting between midnight and 7:59 AM (48 minutes; 95% CI, 43–54 minutes).
DISCUSSION
In this study of 3,798 patients with acute asthma presenting to 62 EDs, we found that approximately two-thirds received SCs; of these, approximately half did not receive SCs within 1 hour of ED arrival. We also found that nonuse of SCs was largely explained by markers of less severe asthma exacerbations (never intubated for asthma, lower respiratory rate, and higher oxygen saturation). In contrast, in addition to factors relating to asthma acuity, delayed SC treatment was associated with several medically unjustified patient-level factors, such as age and sex, and system-level factors.
The delays in SC treatment were greatest in certain patient subgroups, such as those 40 years or older and women. Similar findings, however, have been reported in the setting of ST-elevation myocardial infarction, with older patients and women having significantly longer door-to-balloon times.20 Data from a national ED survey (1997–2004)21 also suggest that wait times are significantly longer in women. In the present study, these findings persisted even after adjustment for severity of exacerbations, indicating that the differences might result from physician practice patterns or patient preference. Given that SC treatment has been shown to be equally effective in age and sex subgroups,7 this finding is concerning and unacceptable. Although the magnitude of the differences was not large, ED physicians should be aware of these findings and increase efforts to minimize these disparities.
Systemwide health care crowding has left many EDs in North America with considerable overcrowding pressures.22,23 Several studies have shown that ED crowding is associated with delays in delivery of timely emergency care,24 such as delays in antibiotic administration in community-acquired pneumonia25 and thrombolysis delays in myocardial infarction.26 In the present study, a longer average patient wait time may serve as a proxy measure for a crowded ED and, therefore, is associated with delays in SC treatment.
Another proxy for crowding may be the time of ED presentation. A survey of 575 ED directors in the United States showed that the perceived worst crowding occurred between 3 PM and 11 PM, followed by 7 AM to 3 PM.27 Patients presenting to the ED during these periods may be more susceptible to ED crowding, which, in turn, leads to a longer door-to-SC time. This circadian difference in SC use has also been reported in a previous multicenter study28 of acute asthma in 1996 to 1998, with nighttime patients more likely to receive SCs in the ED. Similarly, nighttime patients were approximately 2 times more likely to receive timely antibiotic treatment in community-acquired pneumonia.25 Taken together, these findings suggest that time of ED presentation may be related to ED crowding and its adverse consequences. This important issue merits further investigation.
Consistent with guideline recommendations,2,3 the present data suggest that ED physicians appropriately administer SCs in patients with more severe exacerbations (ie, history of intubation for asthma, higher respiratory rate, and lower oxygen saturation). Another factor, early presentation to the ED after symptom onset, may also relate to physician judgment. For example, patients who present early may elicit more urgency from ED physicians to initiate SC treatment. Alternatively, patients who present late may exhibit more atypical symptoms that subsequently lead to delayed treatments, a finding that has been reported in acute myocardial infarction.29
This study has some potential limitations. First, arrival time was documented in the medical record and may represent triage or registration time, which might be collected by electronic or paper processes. In addition, the timing of the administration of the SC may not be precise because it is recorded by nurses after the fact. Consequently, data on door-to-SC time may be affected by random variability in calculating this interval. Although this random measurement error would bias the findings toward the null,30 we still identified several important patient and ED factors associated with delays in SC treatment. In other words, these associations could have been stronger had the measurement errors been corrected. Second, the EDs that composed this sample are predominantly urban, academically affiliated hospitals. This may make these results less generalizable to community hospitals without academic affiliation. Third, the ED wait time was the average delay at each institution across all conditions, not the wait time for the individual asthma visit. As a result, its impact on time to SC was diluted. Fourth, because it was an observational study, which is prone to confounding by severity,31 we did not demonstrate the association between timely SC use and improved clinical outcomes. Finally, this study used a retrospective data approach, which has known recording biases; however, the information used in this analysis was medication timing, which has been shown to be valid previously.32
In summary, we found that approximately one-third of patients with acute asthma did not receive SCs in the ED, and of those who did receive ED corticosteroids, approximately half did not receive this treatment within 1 hour of arrival. Physicians in the ED seem to appropriately administer SCs to higher-acuity asthmatic patients; however, the additional nonmedical factors associated with delayed SC treatment are concerning. Delays are more pronounced in subgroups of women and patients 40 years or older and are associated with ED factors related to crowding. For physicians, these results indicate opportunities to improve timeliness and minimize disparities in the patient care of acute asthma. For policy makers, these results suggest the need for quality improvement efforts to resolve the problem of ED crowding.
Acknowledgments
Funding Sources: This study was supported by grant R01 HS-13099 from the Agency for Healthcare Research and Quality, grant R01 HL-84401 from the National Institutes of Health (Dr Camargo), and a 21st Century Research Chair from the Government of Canada (Dr Rowe).
We thank David Blumenthal, Paul D. Cleary, James A. Gordon, Edward Guadagnoli, Rainu Kaushal, David J. Magid, and Sowmya R. Rao for their contributions to the NEDSS. We also thank the NEDSS site principal investigators and local medical record abstractors.
Footnotes
Disclosures: Dr Camargo has received financial support from a variety of groups for participation in conferences, consulting, and medical research; recent industry sponsors with an interest in asthma were AstraZeneca, Dey, GlaxoSmithKline, Merck, Novartis, and Schering-Plough. Dr Rowe has received financial support from AstraZeneca for speaking engagements and medical research in the past 2 years.
References
- 1.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma—United States, 1980 –2004. MMWR Surveill Summ. 2007;56:1–54. [PubMed] [Google Scholar]
- 2.National Asthma Education and Prevention Program. Expert Panel Report II: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health; 1997. [Google Scholar]
- 3.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma—Summary Report 2007. J Allergy Clin Immunol. 2007;120(suppl):S94–s138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 4.Schneider SM, Pipher A, Britton HL, Borok Z, Harcup CH. High-dose methylprednisolone as initial therapy in patients with acute bronchospasm. J Asthma. 1988;25:189–193. doi: 10.3109/02770908809071365. [DOI] [PubMed] [Google Scholar]
- 5.Storr J, Barrell E, Barry W, Lenney W, Hatcher G. Effect of a single oral dose of prednisolone in acute childhood asthma. Lancet. 1987;1:879– 882. doi: 10.1016/s0140-6736(87)92857-1. [DOI] [PubMed] [Google Scholar]
- 6.Littenberg B, Gluck EH. A controlled trial of methylprednisolone in the emergency treatment of acute asthma. N Engl J Med. 1986;314:150–152. doi: 10.1056/NEJM198601163140304. [DOI] [PubMed] [Google Scholar]
- 7.Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001;(1):CD002178. doi: 10.1002/14651858.CD002178. [DOI] [PubMed] [Google Scholar]
- 8.Manser R, Reid D, Abramson M. Corticosteroids for acute severe asthma in hospitalised patients. Cochrane Database Syst Rev. 2001;(1):CD001740. doi: 10.1002/14651858.CD001740. [DOI] [PubMed] [Google Scholar]
- 9.Banerji A, Clark S, Afilalo M, Blanda MP, Cydulka RK, Camargo CA., Jr Prospective multicenter study of acute asthma in younger versus older adults presenting to the emergency department. J Am Geriatr Soc. 2006;54:48–55. doi: 10.1111/j.1532-5415.2005.00563.x. [DOI] [PubMed] [Google Scholar]
- 10.Tsai CL, Sullivan AF, Gordon JA, et al. Quality of care for acute asthma in 63 US emergency departments. J Allergy Clin Immunol. 2009;123:354–361. doi: 10.1016/j.jaci.2008.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sullivan AF, Camargo CA, Jr, Cleary PD, et al. The National Emergency Department Safety Study: study rationale and design. Acad Emerg Med. 2007;14:1182–1189. doi: 10.1197/j.aem.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Welch S, Augustine J, Camargo CA, Jr, Reese C. Emergency department performance measures and benchmarking summit. Acad Emerg Med. 2006;13:1074–1080. doi: 10.1197/j.aem.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 13.Radeos MS, Camargo CA., Jr Predicted peak expiratory flow: differences across formulae in the literature. Am J Emerg Med. 2004;22:516–521. doi: 10.1016/j.ajem.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 14.US Bureau of the Census. [Accessed March 9, 2009];Census regions and divisions of the United States. http://www.census.gov/geo/www/us_regdiv.pdf.
- 15.Tsai CL, Camargo CA., Jr Methodological considerations, such as directed acyclic graphs, for studying “acute on chronic” disease epidemiology: chronic obstructive pulmonary disease example [published online ahead of print February 9, 2009] J Clin Epidemiol. doi: 10.1016/j.jclinepi.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79:340–349. doi: 10.2105/ajph.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miettinen OS. Theoretical Epidemiology: Principles of Occurrence Research in Medicine. New York, NY: John Wiley & Sons; 1985. [Google Scholar]
- 18.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 19.Bland JM, Altman DG. The use of transformation when comparing two means. BMJ. 1996;312:1153. doi: 10.1136/bmj.312.7039.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehta RH, Bufalino VJ, Pan W, et al. Achieving rapid reperfusion with primary percutaneous coronary intervention remains a challenge: insights from American Heart Association’s Get With the Guidelines program. Am Heart J. 2008;155:1059–1067. doi: 10.1016/j.ahj.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Wilper AP, Woolhandler S, Lasser KE, et al. Waits to see an emergency department physician: U.S. trends and predictors, 1997–2004. Health Aff (Millwood) 2008;27:w84–w95. doi: 10.1377/hlthaff.27.2.w84. [DOI] [PubMed] [Google Scholar]
- 22.Epstein SK, Burstein JL, Case RB, et al. The National Report Card on the State of Emergency Medicine: evaluating the emergency care environment state by state 2009 edition. Ann Emerg Med. 2009;53:4–148. doi: 10.1016/j.annemergmed.2008.10.028. [DOI] [PubMed] [Google Scholar]
- 23.US Institute of Medicine, Committee on the Future of Emergency Care in the US Health System. The Future of Emergency Care in the United States Health System. Washington, DC: National Academy Press; 2006. [DOI] [PubMed] [Google Scholar]
- 24.Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 25.Fee C, Weber EJ, Maak CA, Bacchetti P. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2007;50:501–509. 509.e1. doi: 10.1016/j.annemergmed.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577–585. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Derlet R, Richards J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001;8:151–155. doi: 10.1111/j.1553-2712.2001.tb01280.x. [DOI] [PubMed] [Google Scholar]
- 28.Brenner BE, Chavda KK, Karakurum MB, Karras DJ, Camargo CA., Jr Circadian differences among 4,096 emergency department patients with acute asthma. Crit Care Med. 2001;29:1124–1129. doi: 10.1097/00003246-200106000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Ting HH, Bradley EH, Wang Y, et al. Delay in presentation and reperfusion therapy in ST-elevation myocardial infarction. Am J Med. 2008;121:316–323. doi: 10.1016/j.amjmed.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 31.Clark S, Costantino T, Rudnitsky G, Camargo CA., Jr Observational study of intravenous versus oral corticosteroids for acute asthma: an example of confounding by severity. Acad Emerg Med. 2005;12:439– 445. doi: 10.1197/j.aem.2004.11.030. [DOI] [PubMed] [Google Scholar]
- 32.McDermott MF, Lenhardt RO, Catrambone CD, Walter J, Weiss KB. Adequacy of medical chart review to characterize emergency care for asthma: findings from the Illinois Emergency Department Asthma Collaborative. Acad Emerg Med. 2006;13:345–348. doi: 10.1197/j.aem.2005.09.006. Reprints are not available. [DOI] [PubMed] [Google Scholar]