Abstract
Background and Objective
Low-level laser (light) therapy (LLLT) is a noninvasive, nonthermal approach to disorders requiring reduction of pain and inflammation and stimulation of healing and tissue regeneration. Within the last decade, LLLT started being investigated as an adjuvant to liposuction, for noninvasive body contouring, reduction of cellulite, and improvement of blood lipid profile. LLLT may also aid autologous fat transfer procedures by enhancing the viability of adipocytes. However the underlying mechanism of actions for such effects still seems to be unclear. It is important, therefore, to understand the potential efficacy and proposed mechanism of actions of this new procedure for fat reduction.
Materials and Methods
A review of the literature associated with applications of LLLT related to fat layer reduction was performed to evaluate the findings from pre-clinical and clinical studies with respect to the mechanism of action, efficacy, and safety.
Results
The studies as of today suggest that LLLT has a potential to be used in fat and cellulite reduction as well as in improvement of blood lipid profile without any significant side effects. One of the main proposed mechanism of actions is based upon production of transient pores in adipocytes, allowing lipids to leak out. Another is through activation of the complement cascade which could cause induction of adipocyte apoptosis and subsequent release of lipids.
Conclusion
Although the present studies have demonstrated safety and efficacy of LLLT in fat layer reduction, studies demonstrating the efficacy of LLLT as a stand-alone procedure are still inadequate. Moreover, further studies are necessary to identify the mechanism of action.
Keywords: body contouring, cellulite, cholesterol, fat, lipoplasty, LLLT, liposuction
INTRODUCTION
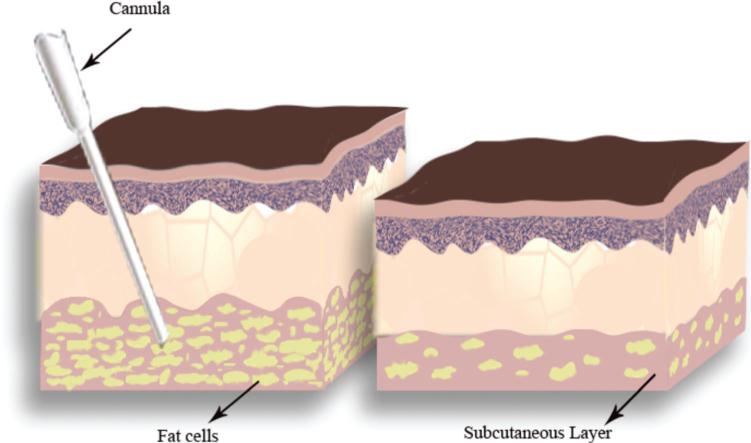
The concept of lipoplasty was introduced by Charles Dujarrier of France in the 1920s. In an attempt to remove subcutaneous tissue from a dancer's calves, Dujarrier ultimately caused gangrene and the death of his patient [1]. Lipoplasty was reintroduced in 1974 by Dr. Giorgio Fischer, and his son who utilized oscillating blades within a cannula to cut away subcutaneous tissue [2]. In 1983, Illouz [3] reported his 5-year experience with a new lipoplasty technique utilizing cannulas as large as 10 cm and suction tubing to safely remove fat from different regions in the body. Figure 1 shows a graphical representation of this technique. This success ushered in the era of modern lipoplasty. Over the ensuing decades the concept of tumescent technique decreased blood loss and subsequent morbidity associated with liposuction and led to improved results. Ultrasound and laser lipoplasty methods have provided further advancement in the range of technical choices offered to the plastic surgeon however they all have limitations and carry certain risks [4–6]. These limitations led to investigation of noninvasive alternative modalities for fat reduction such as cryolipolysis, radiofrequency, and low-level laser therapy [7].
Fig. 1.
Illustration of liposuction with a cannula. A cannula is inserted to the subcutaneous layer and the fat is suctioned with the aid of a suction tube in order to remove fat from different regions in the body.
LOW-LEVEL LASER (LIGHT) THERAPY (LLLT)
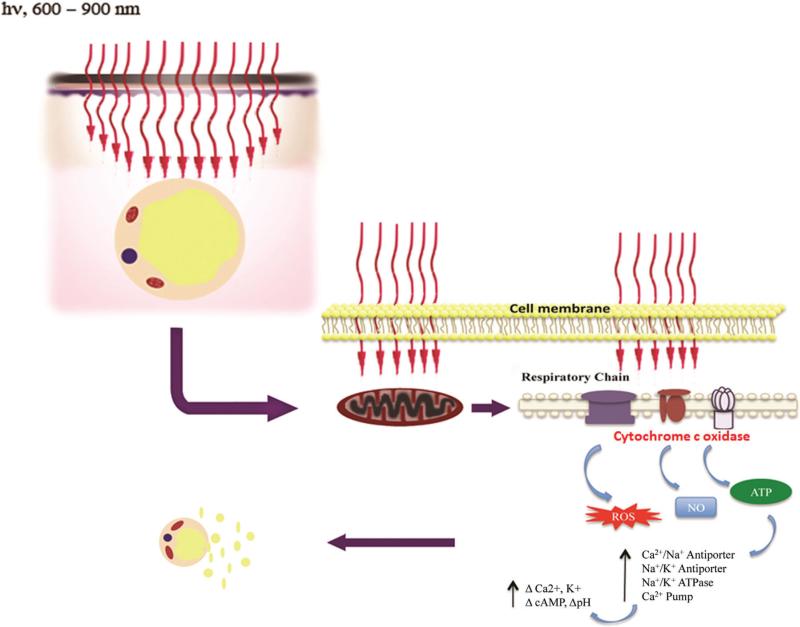
The first reports of LLLT were published by Endre Mester from the Semmelweiss University in Hungary. He originally noticed hair regrowth in mice exposed to a ruby laser (694 nm) [8] and later used HeNe laser (632.8 nm) to stimulate wound healing in animal models [9] and subsequently in clinical studies [10]. Since those early days LLLT has become widely practiced by physical therapists and chiropractors, although it is still regarded with a degree of skepticism by the medical profession at large [11]. LLLT is highly effective to relieve pain, inflammation, and edema in orthopedic injuries and degenerative disease [12], and is also used for nonhealing leg ulcers [13]. LLLT has great potential to prevent tissue death and stimulate tissue regeneration in a wide variety of diseases in neurology [14], ophthalmology [15], cardiology [16], and otolaryngology [17]. It was shown to be effective in reducing pain following breast augmentation surgery and in 2008, Erchonia EML, 630–640 nm (Erchonia Medical, Inc., McKinney, TX) received FDA market clearance for this purpose [18]. Another important application is in prevention of oral mucositis as a side effect of cancer therapy [19]. Although all the early studies used coherent lasers as the light source, it is now thought that noncoherent light emitting diodes [20] are also effective. The mechanism is based on absorption of red and near-infrared photons by chromophores in the mitochondria (particular cytochrome c oxidase) leading to increases of mitochondrial membrane potential, oxygen consumption, adenosine triphosphate (ATP), a transient increase in reactive oxygen species (ROS) [21], and a release of nitric oxide (NO). Transcription factors such as nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) are activated [22] leading to signaling pathways that promote cell survival, cell proliferation, and cell migration. Figure 2 shows the cell signaling and downstream effects caused by photon absorption in the mitochondria. In this article we will mainly focus on several studies that have been reported on LLLT's use in liposuction [20,23–25], noninvasive body contouring and fat reduction [26–33], reduction of cellulites [26,27,31], and reduction in serum cholesterol and triglyceride levels [34,35].
Fig. 2.
Possible mechanism of action of LLLT in reduction of fat. LLLT stimulates the cytochrome c found within the respiratory chain in the mitochondria in adipocytes. This stimulation in turn leads to a transient increase in reactive oxygen species (ROS), release of nitric oxide (NO) and cause increased levels of ATP synthesis with subsequent upregulation of cAMP.
LLLT ASSISTED LIPOSUCTION
In 2000 a new technique was introduced by Niera et al. [36] which utilized LLLT as an adjunct to liposuction. They used a dose rate that caused no detectable temperature rise in the tissue and no macroscopic changes in the tissue structure were observed [24,36]. This application of LLLT was derived from prior investigations of LLLT in wound healing, pain relief, and edema prevention [37,38]. The development of LLLT was predicated on determining the optimum wavelength, and power necessary to augment lipoplasty without altering macroscopic structure of the tissue [39]. Evidence existed that wavelengths between 630 and 640 nm were optimum for biomodulation [40–45] and these wavelengths were therefore used for LLLT-assisted lipoplasty [24,25]. Moreover, LLLT has been reported to reduce inflammatory response [46,47] and pain [48–50], and promote wound healing [51–53] which would all facilitate the post-surgical healing [20,23–25].
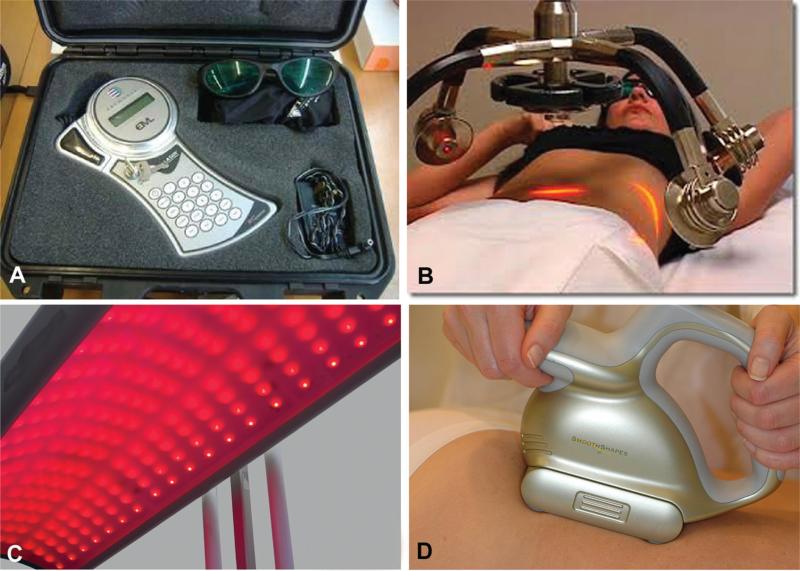
These findings prompted the development of a device, the EML Laser (Erchonia Medical, Inc.) that emits 14 mW of 635-nm light (Fig. 3A). It was applied to the surface of the skin before liposuction, with the intent to emulsify the fat thereby softening the area prior to aspiration. A placebo-controlled, randomized, double-blind, multicentered clinical study was performed to evaluate the clinical utility of this application as an adjunct to liposuction and the results suggested that laser therapy decreased operating room times, increased the volume of fat extracted, less force was required by the physician to breakup fat, and the recovery for patients was significantly improved [54]. Based on the findings of this study the FDA issued 510k clearance for the EML device in 2001 for use as an adjunctive therapy to liposuction.
Fig. 3.
Examples of LLLT devices. This figure shows four of the light source devices that either been approved or clinically applied for fat reduction. A: The EML low-level laser for laser assisted liposuction from Erchonia Medical, Inc. B: The Zerona LipoLaser for noninvasive body contouring from Erchonia Medical, Inc. C: The NovoThor LED canopy for weight loss from Thor Photomedicine (Chesham, Bucks, UK). D: The SmoothShapes system for cellulite reduction from Eleme Medical.
Niera et al. studied samples of human adipose tissue from 12 lipectomy patients who were operated with and without tumescent technique and externally irradiated with a 635-nm, 10 mW diode laser with total energy values of 1.2–3.6 J/cm2 for 0–6 minutes. The group found out that the tumescent technique had synergistic effects, facilitated laser light penetration, and intensity, thus improved fat liquefaction [24]. While after 4 minutes of laser exposure 80% of the fat was released from the adipose cells, after 6 minutes of laser exposure almost all of the fat was released from the adipocyte. When no tumescent solution was applied and adipose tissue was exposed to laser beam for 4 and 6 minutes, scanning electron microscope (SEM) and transmission electron microscope (TEM) images after 6 minutes laser exposure in samples taken without tumescent solution corresponded to those observed in samples exposed to 4 minutes of laser irradiation with equal parameters and the tumescent solution. Without laser exposure and only tumescent technique, the adipose tissue remained intact and adipocytes maintained their original spherical structure.
It should be noted that there is another procedure termed “laser assisted liposuction [55]. In 2012, Chia and Theodorou [55] reported 1,000 consecutive cases of laser-assisted liposuction and suction-assisted lipectomy managed with local anesthesia. This procedured used a high power Nd:YAG laser at either 1,064-nm (pulsed at 40 Hz) or a dual wavelength device at 1,064/1,320-nm pulsed at 25 Hz. After injection of tumescent solution containing local anesthetic, a fiber optic was inserted via a cannula into the deep and intermediate subcutaneous spaces moving at a rate of at least 1 cm/second. The applied power setting ranged from 7 to 38 W, with a total fluence ranging from 2,000 to 64,000 J per site [56]. Suction-assisted lipolysis was then performed using standard manual Mercedes-style-tip liposuction cannulas. Even though results were satisfactory, burn and hematoma were possible complications of this procedure [5,55].
MECHANISM OF ACTION OF LLLT FOR FAT REMOVAL
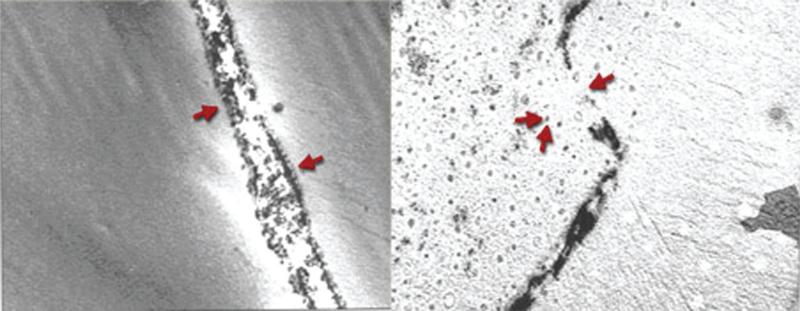
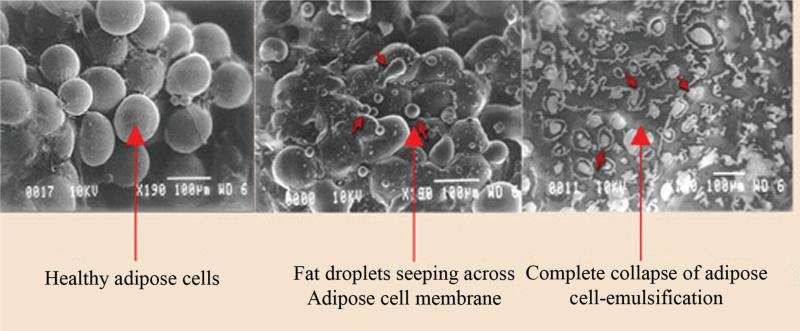
The mechanism of action of LLLT on fat remains somewhat controversial. In Neira's first article the effects of LLLT on adipocytes were attributed to formation of transitory micropores which were visualized on SEM (see Fig. 4) [24]. These pores were proposed to allow the release of intracellular lipids from adipocytes. Based on these data it was proposed that up to 99% of fat could be released from the adipocytes via application of 635 nm, 10 mW intensity LLLT for a period of 6 minutes [24]. One possible explanation might be that, increased ROS levels following LLLT initiate a process known as lipid peroxidation where ROS reacts with lipids found within the cellular membranes, and temporarily damages them by creating pores [22,57–59]. However, in an attempt to replicate Neira et al.'s data [24], Brown et al. [23] failed to visualize any transitory micropores. In another study, Medrado et al. investigated the action of different fluences (9 mW, 670 nm, 4, 8, 12, and 16 J/cm2 for 31, 62, 124, and 248 seconds, respectively) from a gallium–aluminum arsenide laser which was applied through the intact skin to the dorsal fat pad of rats. LLLT caused brown adipose fat droplets to coalesce and fuse, apparently transforming them into yellow fat but had only negligible effect on yellow fat itself [60]. Increased vascular proliferation, mitochondria, and congestion were evident findings in the laser irradiated brown fat. Considering most changes were restricted to the brown fatty tissue only and yellow tissue always preserved its appearance with no signs of lipolysis observed, results from this study were not in accordance with Niera et al.'s study. However, it is worthwhile to mention that experimental parameters used in these studies were not the same. Another possible mechanism of action for release of lipids was proposed to be through activation of the complement cascade which could cause induction of adipocyte apoptosis and subsequent release of lipids [29]. To investigate the complement activation theory, Caruso-Davis et al. [29] exposed differentiated human adipocytes to plasma. With and without irradiation there was noted to be no difference in complement induced lysis of adipocytes. Although no enzymatic assays were done to determine levels of complement within the plasma, the group concluded that laser does not activate complement. Lastly, unlike Niera et al.'s [60] findings, the external cell membrane preserved its normal appearance in electron microscopy, presenting no ruptures nor pores, in spite of the disposition of its fused fatty vacuoles, and no other signs of lipolysis were observed. An additional paper called into question the ability of red light (635 nm) to penetrate effectively below the skin surface and into the subdermal tissues [61]. In a supportive commentary Peter Fodor stated; “One could postulate that the presence of the black dots on SEM images on the surface of fat cells reported by Neira et al. could represent an artifact” [23].
Fig. 4.
Scanning electron microscopy (SEM) images of transitory pores formed in cell membrane of adipocytes following LLLT [24]. Taken with permission.
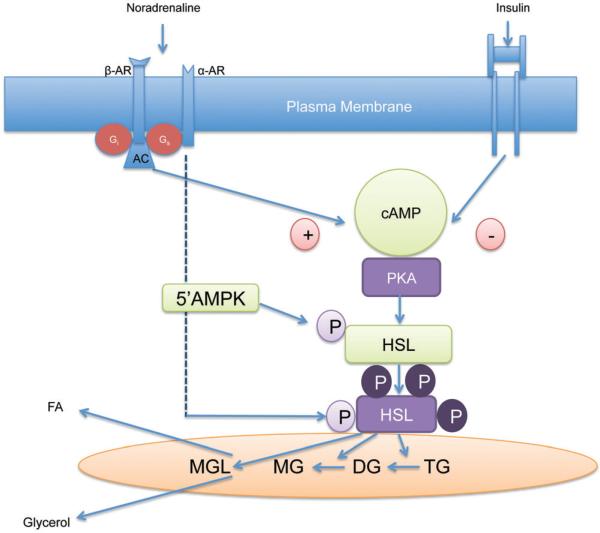
It is also possible that LLLT stimulates the mitochondria in adipocytes that in turn leads to an increase ATP synthesis with subsequent upregulation of cAMP [62–65]; the increased cAMP could activate protein kinase which could stimulate cytoplasmic lipase, an enzyme that converts triglycerides into fatty acids and glycerol, which can both pass through pores formed in the cell membrane may cause a shrinkage in adipocytes [30,66] (see Fig. 5). However, Caruso-Davis et al. findings from in vitro studies on human fat cells obtained from subcutaneous fat, irradiated with 635–680 nm LLLT for 10 minutes demonstrated no increase of glycerol and fatty acids suggesting that fat loss from the adipocytes in response to laser treatment was not due to a stimulation of lipolysis, however they did detect increased triglyceride levels which further supported the formation of pores in adipocytes [29]. Figure 6 graphically illustrates many of the proposed mechanisms that have been devised to explain the use of LLLT for fat removal.
Fig. 5.
Scanning electron microscopy (SEM) images of adipocytes following LLLT [24]. Taken with permission.
Fig. 6.
A schematic illustration of lipolysis pathway. The binding of the ligand adenylate cyclase (AC) to its receptor-β-adrenergic receptor (β-AR) via protein G (Gs) elevates the levels of cyclic adenosine monophosphate (cAMP) which in turn activates protein kinase (PKA). PKA phosphorylates hormone sensitive lipase (HSL) that in turn causes degradation of triglycerides (TG) and diglycerides (DG) to monoglycerides (MG). With the help of monoglyceride lipase (MGL) monoglycerides are further degragated to fatty acid and glycerol.
LLLT FOR NONINVASIVE BODY CONTOURING
The Zerona LipoLaser (Erchonia Medical, Inc.) is a device with five rotating independent diode laser heads each emitting 17 mW of 635 nm laser light (Fig. 3B). It was the first noninvasive aesthetic device to receive FDA market clearance in the US for circumferential reduction of the waist, hips, and thighs following completion of a placebo-controlled, randomized, double-blind, multisite clinical investigation evaluating 67 study participants [67]. The results obtained from that study demonstrated an average reduction of 3.51 inches across patient's waist, hips, and thighs in as little as 2 weeks. The clinical trial, absence of diet restrictions, exercise requirements, or any other adjunctive components properly illustrated the clinical utility of the Zerona and set the precedent on how aesthetic devices should be evaluated.
In a randomized study, Caruso-Davis used 635–680 nm LLLT device (Meridian LAPEX 2000 LipoLaser System, Meridian Medical Inc. Anyang, Korea) for 30 minutes twice a week for 4 weeks on 40 healthy young men and women and subjects were asked not to change their diet nor exercise habits [29]. Results demonstrated that LLLT achieved safe and significant girth loss at the end of the treatment period. However it is worthwhile to note that this device is currently approved by the FDA for hand and wrist pain associated with carpal tunnel syndrome only. Another study by Jackson et al. demonstrated a significant reduction (overall mean reduction of 5.17 inches across all measurement points) in circumferential measurements across waist, hips, and thighs of 689 patients following LLLT with Zerona LipoLaser (Erchonia Medical, Inc.). Treatment period was for two consecutive weeks, with each patient receiving three treatments per week every other day for a total of 40 minutes. The authors also noted that circumferential reduction exhibited following LLLT was not attributable to fluid nor fat relocation since all the measurement points including nontreated regions reported an inch loss. Moreover, a double-blind, controlled, randomized study designed to assess the efficacy of 635 nm LLLT (3.94 J/cm2, 17 mW) in reducing upper arm circumference, LLLT group (n = 20) demonstrated a significant progressive and cumulative treatment effect compared to sham treated group (n = 20) following six treatments with no side effects [30].
A recent study investigated the efficacy of LLLT –635 nm device that consists of 5 diodes generating an output intensity of ~0.95 J/cm2 each and the group demonstrated an average of 2.99 inches reduction in waist, hips, and thigh at the end of the treatment period. However, the study had several limitations such as lack of control group as well as administration of dietary supplements (niacin, niacinamide, l-carnitine, omega-3 fish oil, ginko biloba, and decaffeinated green tea) in the study subjects [68].
LLLT FOR CELLULITE REDUCTION
Even though etiology of cellulite remains controversial, it manifests itself at the histological level not only by the presence of thinner, more radially oriented supporting fibrous septae in the deep subcutis [69], but also by an irregular dermohypo-dermal interface produced by herniation of subdermal fat into the reticular and papillary dermis [21]. Sasaki et al. [20] conducted a double-blinded study among nine female volunteers to evaluate the efficacy of phosphatidylcholine-based anticellulite gel (active gel) in combination with a LED at wavelengths of red (660 nm) and near-infrared (950 nm), a deeper penetrating wavelength, for treatment of cellulite [26]. Study subjects were treated twice daily for 3 months with an active gel on one thigh and placebo gel on the other thigh. Twice a week, each thigh was exposed to 15 minutes of LED with a total of 24 treatments. Digital ultrasound at the dermal–adiposal interface revealed not only a signifi-cant reduction of subcutaneous fat immediately below the dermis but also less echo-like intrusions were observed in the dermal layer of active gel and LED treated thighs. Among three of six biopsies taken from thighs that were treated for 3 months, with the active gel in combination with LED, less intrusion of subcutaneous fat into the papillary and reticular dermis have been noted upon histologic analysis. However, in nine placebo and LED only treated thighs minimal changes were observed. One of the limitations of this study was the lack of active gel treated only group, which leaves a possibility of LED having no enhancing effect in the combination therapy. Lastly, it is worthwhile to note that at the 18th month of evaluation period, five responsive thighs reverted back to their original cellulite grading. Some of the gels used in this study contained methylxanthine caffeine that inhibits the action of cyclic 3′,5′-phosphadiesterase, the enzyme that causes degradation of cAMP into 5′-AMP [26]. As mentioned earlier, inhibition of this enzyme results in higher levels of cAMP, which stimulates a protein kinase that converts inactive hormone-sensitive lipase into its active form and result in hydrolysis of triglycerides into free fatty acids and glycerol. This study was similar to Neira's study in the sense that both epinephrine contained in the tumescent solution and methylxanthine caffeine contained in some of the gels had similar effects on levels of cAMP and when used in combination with LLLT (which may also increase levels of cAMP) had synergistic effects for degradation of fat [24].
Although several other studies reported satisfactory results using devices that combine LLLT sources with vacuum and massage such as FDA-cleared SmoothShapes system (Eleme Medical, Merrimack, NH) (Fig. 3D) and TriActive (Deka Lasers, Florence, Italy) which is currently available only in Europe [27,31,70–74], as of today there is only one study by Jackson et al. [75] that used LLLT (six 532-nm green diodes, with a total power output of 102 mW applied for 15 minutes) as a stand-alone procedure. Even though results from this study demonstrated significant improvement in appearance of cellulite, long-term effects still need to be assessed.
LLLT ON REDUCTION OF SERUM LIPID LEVELS
Although it had been hypothesized that fat released following LLLT treatment may appear in the bloodstream where it might adversely affect the lipid profile, a nonrandomized, uncontrolled pilot study demonstrated an actual reduction in serum cholesterol and leptin levels following LLLT [56]. Two other studies by Rushdi [35] and Jackson et al. [34] demonstrated similar effects in blood lipid profiles following LLLT treatments using i-lipo (Chromogenex, South Wales, United Kingdom) and Erchonia Zerona (Erchonia Medical, Inc.) devices, respectively.
LLLT IN AUTOLOGOUS FAT TRANSPLANTATION
Autologous fat transplantation has become a well-established method of soft tissue augmentation for both cosmetic and reconstructive indications, however it still faces significant challenges such as fat graft failures and volume reduction [76–78]. This is most likely due to mechanical stress during harvest, ischemia, and nutrient deprivation. In one of the previously mentioned studies by Neira et al.; when irradiated adipose cells were recultured, they were shown to be able to recover to their original cell membrane structure and remain alive or viable [24], which was also confirmed by Caruso-Davis et al. [29] above mentioned study where they compared the number of viable adipocytes in the laser-treated and untreated group by live dead assay. Moreover, a few other animal studies successfully demonstrated LLLT's beneficial effects on increasing viability and survival of grafts [79,80]. Based on these findings, LLLT could be potentially used to improve the outcomes in autologous fat transplantations where the cell viability is critical.
CONCLUSION AND FUTURE DIRECTIONS
The continuing growth in aesthetic procedures suggests that LLLT will continue to be used in both lipoplasty and body contouring procedures. LLLT could also prevent skin burns that are possible risks encountered in radiofrequency-, laser-, and ultrasound-assisted liposuction [5,6,81]. Additional applications of LLLT could be to facilitate autologous fat transplant procedures when applied to both the donor and recipient sites. Since adipose cells were shown to be alive and were able to recover their anatomy, application of LLLT could increase the number of viable adipocytes that survive [82,83]. Improved blood lipid profiles following LLLT also suggest another potential application. However the lack of certainty on the mechanism of action will tend to slow down the widespread adoption of these techniques. Moreover, there is still lack of adequate number of studies where LLLT was investigated as a stand-alone therapy. Lastly, it is worthwhile to note that LLLT parameters used for facial skin rejuvenation and acne treatments are close to the ones used in fat reduction [84,85]. Therefore, it is possible that facial volume loss may occur while using LLLT. This possibility should be considered and safety of LLLT parameters should be carefully evaluated based on treatment location.
ACKNOWLEDGMENT
This work was supported by the US NIH (R01AI050875 to M.R.H.).
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1.Thorek M. Plastic reconstruction of the female breasts and abdomen. Am J Surg. 1939;43(2):268–278. [Google Scholar]
- 2.Fischer G. Liposculpture: The “correct” history of liposuction. Part I. J Dermatol Surg Oncol. 1990;16(12):1087–1089. doi: 10.1111/j.1524-4725.1990.tb00017.x. [DOI] [PubMed] [Google Scholar]
- 3.Illouz YG. Body contouring by lipolysis: A 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591–597. doi: 10.1097/00006534-198311000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Sterodimas A, Boriani F, Magarakis E, Nicaretta B, Pereira LH, Illouz YG. Thirtyfour years of liposuction: Past, present and future. Eur Rev Med Pharmacol Sci. 2012;16(3):393–406. [PubMed] [Google Scholar]
- 5.Katz B, McBean J. Laser-assisted lipolysis: A report on complications. J Cosmet Laser Ther. 2008;10(4):231–233. doi: 10.1080/14764170802524437. [DOI] [PubMed] [Google Scholar]
- 6.Sadick NS. Overview of ultrasound-assisted liposuction, and body contouring with cellulite reduction. Semin Cutan Med Surg. 2009;28(4):250–256. doi: 10.1016/j.sder.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Jalian HR, Avram MM. Body contouring: The skinny on noninvasive fat removal. Semin Cutan Med Surg. 2012;31(2):121–125. doi: 10.1016/j.sder.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Mester E, Szende B, Gartner P. The effect of laser beams on the growth of hair in mice. Radiobiol Radiother (Berl) 1968;9(5):621–626. [PubMed] [Google Scholar]
- 9.Mester E, Spiry T, Szende B, Tota JG. Effect of laser rays on wound healing. Am J Surg. 1971;122(4):532–535. doi: 10.1016/0002-9610(71)90482-x. [DOI] [PubMed] [Google Scholar]
- 10.Mester E, Korenyi-Both A, Spiry T, Scher A, Tisza S. Stimulation of wound healing by means of laser rays. Clinical and electron microscopical study. Acta Chir Acad Sci Hung. 1973;14(4):347–356. [PubMed] [Google Scholar]
- 11.Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533. doi: 10.1007/s10439-011-0454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jang H, Lee H. Meta-analysis of pain relief effects by laser irradiation on joint areas. Photomed Laser Surg. 2012;30(8):405–417. doi: 10.1089/pho.2012.3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Minatel DG, Frade MA, Franca SC, Enwemeka CS. Photo-therapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med. 2009;41(6):433–441. doi: 10.1002/lsm.20789. [DOI] [PubMed] [Google Scholar]
- 14.Hashmi JT, Huang YY, Osmani BZ, Sharma SK, Naeser MA, Hamblin MR. Role of low-level laser therapy in neurorehabilitation. PM R. 2010;2((2 Suppl. 2):S292–S305. doi: 10.1016/j.pmrj.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ivandic BT, Ivandic T. Low-level laser therapy improves vision in patients with age-related macular degeneration. Photomed Laser Surg. 2008;26(3):241–245. doi: 10.1089/pho.2007.2132. [DOI] [PubMed] [Google Scholar]
- 16.Tuby H, Maltz L, Oron U. Induction of autologous mesenchymal stem cells in the bone marrow by low-level laser therapy has profound beneficial effects on the infarcted rat heart. Lasers Surg Med. 2011;43(5):401–409. doi: 10.1002/lsm.21063. [DOI] [PubMed] [Google Scholar]
- 17.Rhee CK, He P, Jung JY, Ahn JC, Chung PS, Suh MW. Effect of low-level laser therapy on cochlear hair cell recovery after gentamicin-induced ototoxicity. Lasers Med Sci. 2012;27(5):987–992. doi: 10.1007/s10103-011-1028-5. [DOI] [PubMed] [Google Scholar]
- 18.Jackson FR, Gregory R, Mangione T. Low-level laser therapy effectiveness for reducing pain after breast augmentation. Am J Cosmet Surg. 2009;26(3):144–148. [Google Scholar]
- 19.Bjordal JM, Bensadoun RJ, Tuner J, Frigo L, Gjerde K, Lopes-Martins RA. A systematic review with meta-analysis of the effect of low-level laser therapy (LLLT) in cancer therapy-induced oral mucositis. Support Care Cancer. 2011;19(8):1069–1077. doi: 10.1007/s00520-011-1202-0. [DOI] [PubMed] [Google Scholar]
- 20.Neira R, Toledo L, Arroyave J, Solarte E, Isaza C, Gutierrez O, Criollo W, Ramirez H, Gutierrez MI, Ortiz-Neira CL. Low-level laser-assisted liposuction: The Neira 4 L technique. Clin Plast Surg. 2006;33(1):117–127. vii. doi: 10.1016/j.cps.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Rosenbaum M, Prieto V, Hellmer J, Boschmann M, Krueger J, Leibel RL, Ship AG. An exploratory investigation of the morphology and biochemistry of cellulite. Plast Reconstr Surg. 1998;101(7):1934–1939. doi: 10.1097/00006534-199806000-00025. [DOI] [PubMed] [Google Scholar]
- 22.Chen AC, Arany PR, Huang YY, Tomkinson EM, Sharma SK, Kharkwal GB, Saleem T, Mooney D, Yull FE, Blackwell TS, Hamblin MR. Low-level laser therapy activates NF-κB via generation of reactive oxygen species in mouse embryonic fibroblasts. PLoS ONE. 2011;6(7):e22453. doi: 10.1371/journal.pone.0022453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown SA, Rohrich RJ, Kenkel J, Young VL, Hoopman J, Coimbra M. Effect of low-level laser therapy on abdominal adipocytes before lipoplasty procedures. Plast Reconstr Surg. 2004;113(6):1796–1804. doi: 10.1097/01.prs.0000117302.73214.1a. discussion 1805–1806. [DOI] [PubMed] [Google Scholar]
- 24.Neira R, Arroyave J, Ramirez H, Ortiz CL, Solarte E, Sequeda F, Gutierrez MI. Fat liquefaction: Effect of low-level laser energy on adipose tissue. Plast Reconstr Surg. 2002;110(3):912–922. doi: 10.1097/00006534-200209010-00030. discussion 923–925. [DOI] [PubMed] [Google Scholar]
- 25.Neira R, Ortiz-Neira C. Low-level laser-assisted liposculpture: Clinical report of 700 cases. Aesthet Surg J. 2002;22(5):451–455. doi: 10.1067/maj.2002.128622. [DOI] [PubMed] [Google Scholar]
- 26.Sasaki GH, Oberg K, Tucker B, Gaston M. The effectiveness and safety of topical PhotoActif phosphatidylcholine-based anti-cellulite gel and LED (red and near-infrared) light on Grade II–III thigh cellulite: A randomized, double-blinded study. J Cosmet Laser Ther. 2007;9(2):87–96. doi: 10.1080/14764170701213439. [DOI] [PubMed] [Google Scholar]
- 27.Lach E. Reduction of subcutaneous fat and improvement in cellulite appearance by dual-wavelength, low-level laser energy combined with vacuum and massage. J Cosmet Laser Ther. 2008;10(4):202–209. doi: 10.1080/14764170802516680. [DOI] [PubMed] [Google Scholar]
- 28.Jackson RF, Stern FA, Neira R, Ortiz-Neira CL, Maloney J. Application of low-level laser therapy for noninvasive body contouring. Lasers Surg Med. 2012;44(3):211–217. doi: 10.1002/lsm.22007. [DOI] [PubMed] [Google Scholar]
- 29.Caruso-Davis MK, Guillot TS, Podichetty VK, Mashtalir N, Dhurandhar NV, Dubuisson O, Yu Y, Greenway FL. Efficacy of low-level laser therapy for body contouring and spot fat reduction. Obes Surg. 2011;21(6):722–729. doi: 10.1007/s11695-010-0126-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nestor MS, Zarraga MB, Park H. Effect of 635 nm low-level laser therapy on upper arm circumference reduction: A double-blind, randomized, Sham-controlled Trial. J Clin Aesthet Dermatol. 2012;5(2):42–48. [PMC free article] [PubMed] [Google Scholar]
- 31.Gold MH, Khatri KA, Hails K, Weiss RA, Fournier N. Reduction in thigh circumference and improvement in the appearance of cellulite with dual-wavelength, low-level laser energy and massage. J Cosmet Laser Ther. 2011;13(1):13–20. doi: 10.3109/14764172.2011.552608. [DOI] [PubMed] [Google Scholar]
- 32.Podichetty VK, Bourassa DC. Effects of low-level laser therapy in subcutaneous fat reduction and improvement in body contour. Lasers Surg Med. 2010;42(Suppl. 22):62. [Google Scholar]
- 33.Nestor MS, Newburger J, Zarraga MB. Body contouring using 635-nm low level laser therapy. Semin Cutan Med Surg. 2013;32(1):35–40. [PubMed] [Google Scholar]
- 34.Jackson FR, Roche GC, Wisler K. Reduction in cholesterol and triglyceride serum levels following low-level laser irradiation: A noncontrolled, nonrandomized pilot study. Am J Cosmet Surg. 2010;27(4):177–184. [Google Scholar]
- 35.Rushdi AT. Effect of low-level laser therapy on cholesterol and triglyceride serum levels in ICU patients: A controlled, randomized study. EJCTA. 2010;4:96–99. [Google Scholar]
- 36.Niera R, Solarte E, Reyes MA, et al. Low level assisted lipoplasty: A new techique; In Proceedings of the World Congress on Lipoplasty; Dearborn, MI. 2000. [Google Scholar]
- 37.King P. Low level laser therapy: A review. Laser Med Sci. 1989;4(3):141–150. [Google Scholar]
- 38.Baxter G, Bell A, Allen J, Ravey J. Low level laser therapy: Current clinical practice in Northern Ireland. Physiotherapy. 1991;77(3):171–178. [Google Scholar]
- 39.Oschmann JI. Energy medicine: The scientific basis. Churchill Livingstone; Edinburgh: 2000. [Google Scholar]
- 40.Frohlich H. Long-range coherence and energy storage in biological systems. Int J Quantum Chem. 1968;2(5):641–649. [Google Scholar]
- 41.Frohlich H. Long range coherence and the action of enzymes. Nature. 1970;228(5276):1093. doi: 10.1038/2281093a0. [DOI] [PubMed] [Google Scholar]
- 42.Frohlich H. The extraordinary dielectric properties of biological materials and the action of enzymes. Proc Natl Acad Sci USA. 1975;72(11):4211–4215. doi: 10.1073/pnas.72.11.4211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sroka R, Schaffer M, Fuchs C, Pongratz T, Schrader-Reichard U, Busch M, Schaffer PM, Dühmke E, Baumgartner R. Effects on the mitosis of normal and tumor cells induced by light treatment of different wavelenghts. Lasers Surg Med. 1999;25(3):263–271. doi: 10.1002/(sici)1096-9101(1999)25:3<263::aid-lsm11>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 44.van Breugel HH, Bar PR. Power density and exposure time of He–Ne laser irradiation are more important than total energy dose in photo-biomodulation of human fibroblasts in vitro. Lasers Surg Med. 1992;12(5):528–537. doi: 10.1002/lsm.1900120512. [DOI] [PubMed] [Google Scholar]
- 45.Al-Watban F, Zang X. Comparison of the effects of laser therapy on wound healing using different laser wavelengths. Laser Ther. 1996;8(2):127–135. [Google Scholar]
- 46.Fukuda TY, Tanji MM, Silva SR, Sato MN, Plapler H. Infrared low-level diode laser on inflammatory process modulation in mice: Pro- and anti-inflammatory cytokines. Lasers Med Sci. 2012 doi: 10.1007/s10103-012-1231-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 47.Assis L, Moretti AI, Abrahao TB, Cury V, Souza HP, Hamblin MR, Parizotto NA. Low-level laser therapy (808 nm) reduces inflammatory response and oxidative stress in rat tibialis anterior muscle after cryolesion. Lasers Surg Med. 2012;44(9):726–735. doi: 10.1002/lsm.22077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kasai S, Kono T, Yamamoto Y, Kotani H, Sakamoto T, Mito M. Effect of low-power laser irradiation on impulse conduction in anesthetized rabbits. J Clin Laser Med Surg. 1996;14(3):107–109. doi: 10.1089/clm.1996.14.107. [DOI] [PubMed] [Google Scholar]
- 49.Ohno T. [Pain suppressive effect of low power laser irradiation. A quantitative analysis of substance P in the rat spinal dorsal root ganglion]. Nihon Ika Daigaku Zasshi. 1997;64(5):395–400. doi: 10.1272/jnms1923.64.395. [DOI] [PubMed] [Google Scholar]
- 50.Saber K, Chiniforush N, Shahabi S. The effect of low level laser therapy on pain reduction after third molar surgery. Minerva Stomatol. 2012;61(7–8):319–322. [PubMed] [Google Scholar]
- 51.Hussein AJ, Alfars AA, Falih MA, Hassan AN. Effects of a low level laser on the acceleration of wound healing in rabbits. N Am J Med Sci. 2011;3(4):193–197. doi: 10.4297/najms.2011.3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carvalho RL, Alcantara PS, Kamamoto F, Cressoni MD, Casarotto RA. Effects of low-level laser therapy on pain and scar formation after inguinal herniation surgery: A randomized controlled single-blind study. Photomed Laser Surg. 2010;28(3):417–422. doi: 10.1089/pho.2009.2548. [DOI] [PubMed] [Google Scholar]
- 53.Medrado AR, Pugliese LS, Reis SR, Andrade ZA. Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers Surg Med. 2003;32(3):239–244. doi: 10.1002/lsm.10126. [DOI] [PubMed] [Google Scholar]
- 54.Jackson FR, Roche G, Kimberly JB, Douglas DD, T KS. Low-level laser-assisted liposuction: A 2004 clinical study of its effectiveness for enhancing ease of liposuction procedures and facilitating the recovery process for patients undergoing thigh, hip and stomach countouring. Am J Cosmet Surg. 2004;21(4):191–194. [Google Scholar]
- 55.Chia CT, Theodorou SJ. 1,000 consecutive cases of laser-assisted liposuction and suction-assisted lipectomy managed with local anesthesia. Aesthetic Plast Surg. 2012;36(4):795–802. doi: 10.1007/s00266-012-9885-2. [DOI] [PubMed] [Google Scholar]
- 56.Maloney RJ, Shanks SC, Jenney E. The reduction in cholesterol and triglyceride serum levels following low-level laser irradiation: A non-controlled, non-randomized pilot study. Lasers Surg Med. 2009;21S:66. [Google Scholar]
- 57.Geiger PG, Korytowski W, Girotti AW. Photodynamically generated 3-beta-hydroxy-5 alpha-cholest-6-ene-5-hydroper-oxide: Toxic reactivity in membranes and susceptibility to enzymatic detoxification. Photochem Photobiol. 1995;62(3):580–587. doi: 10.1111/j.1751-1097.1995.tb02388.x. [DOI] [PubMed] [Google Scholar]
- 58.Tafur J, Mills PJ. Low-intensity light therapy: Exploring the role of redox mechanisms. Photomed Laser Surg. 2008;26(4):323–328. doi: 10.1089/pho.2007.2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Karu TI. Mitochondrial signaling in mammalian cells activated by red and near-IR radiation. Photochem Photobiol. 2008;84(5):1091–1099. doi: 10.1111/j.1751-1097.2008.00394.x. [DOI] [PubMed] [Google Scholar]
- 60.Medrado AP, Trindade E, Reis SR, Andrade ZA. Action of low-level laser therapy on living fatty tissue of rats. Lasers Med Sci. 2006;21(1):19–23. doi: 10.1007/s10103-005-0367-5. [DOI] [PubMed] [Google Scholar]
- 61.Kolari PJ, Airaksinen O. Poor penetration of infra-red and helium neon low power laser light into the dermal tissue. Acupunct Electrother Res. 1993;18(1):17–21. doi: 10.3727/036012993816357566. [DOI] [PubMed] [Google Scholar]
- 62.Karu T. Photobiology of low-power laser effects. Health Phys. 1989;56(5):691–704. doi: 10.1097/00004032-198905000-00015. [DOI] [PubMed] [Google Scholar]
- 63.Karu TI, Afanas'eva NI. [Cytochrome c oxidase as the primary photoacceptor upon laser exposure of cultured cells to visible and near IR-range light]. Dokl Akad Nauk. 1995;342(5):693–695. [PubMed] [Google Scholar]
- 64.Karu TI, Lobko VV, Lukpanova GG, Parkhomenko IM, Chirkov I. [Effect of irradiation with monochromatic visible light on the cAMP content in mammalian cells]. Dokl Akad Nauk SSSR. 1985;281(5):1242–1244. [PubMed] [Google Scholar]
- 65.Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999;49(1):1–17. doi: 10.1016/S1011-1344(98)00219-X. [DOI] [PubMed] [Google Scholar]
- 66.Honnor RC, Dhillon GS, Londos C. cAMP-dependent protein kinase and lipolysis in rat adipocytes. II. Definition of steady-state relationship with lipolytic and antilipolytic modulators. J Biol Chem. 1985;260(28):15130–15138. [PubMed] [Google Scholar]
- 67.Jackson RF, Dedo DD, Roche GC, Turok DI, Maloney RJ. Low-level laser therapy as a non-invasive approach for body contouring: A randomized, controlled study. Lasers Surg Med. 2009;41(10):799–809. doi: 10.1002/lsm.20855. [DOI] [PubMed] [Google Scholar]
- 68.McRae E, Boris J. Independent evaluation of low-level laser therapy at 635 nm for non-invasive body contouring of the waist, hips, and thighs. Lasers Surg Med. 2013;45(1):1–7. doi: 10.1002/lsm.22113. [DOI] [PubMed] [Google Scholar]
- 69.Nurnberger F, Muller G. So-called cellulite: An invented disease. J Dermatol Surg Oncol. 1978;4(3):221–229. doi: 10.1111/j.1524-4725.1978.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 70.Boyce S, Pabby A, Chuchaltkaren P, Brazzini B, Goldman MP. Clinical evaluation of a device for the treatment of cellulite: TriActive. Am J Cosmet Surg. 2005;22(4):233–237. [Google Scholar]
- 71.Nootheti PK, Magpantay A, Yosowitz G, Calderon S, Goldman MP. A single center, randomized, comparative, prospective clinical study to determine the efficacy of the VelaSmooth system versus the Triactive system for the treatment of cellulite. Lasers Surg Med. 2006;38(10):908–912. doi: 10.1002/lsm.20421. [DOI] [PubMed] [Google Scholar]
- 72.Gold M. The use of rhythmic suction massage, low level laser irradiation, and superficial cooling to effect changes in adipose tissue/cellulite. Lasers Surg Med. 2006;38(Suppl.):65. [Google Scholar]
- 73.Kulick MI. Evaluation of a noninvasive, dual-wavelength laser-suction and massage device for the regional treatment of cellulite. Plast Reconstr Surg. 2010;125(6):1788–1796. doi: 10.1097/PRS.0b013e3181cb6515. [DOI] [PubMed] [Google Scholar]
- 74.Gold MH. Cellulite—An overview of non-invasive therapy with energy-based systems. J Dtsch Dermatol Ges. 2012;10(8):553–558. doi: 10.1111/j.1610-0387.2012.07950.x. [DOI] [PubMed] [Google Scholar]
- 75.Jackson RF, Roche GC, Shanks SC. A double-blind, placebo-controlled randomized trial evaluating the ability of low-level laser therapy to improve the appearance of cellulite. Lasers Surg Med. 2013;45(3):141–147. doi: 10.1002/lsm.22119. [DOI] [PubMed] [Google Scholar]
- 76.Boschert MT, Beckert BW, Puckett CL, Concannon MJ. Analysis of lipocyte viability after liposuction. Plast Reconstr Surg. 2002;109(2):761–765. doi: 10.1097/00006534-200202000-00054. discussion 766–767. [DOI] [PubMed] [Google Scholar]
- 77.Bucky LP, Percec I. The science of autologous fat grafting: Views on current and future approaches to neoadipogenesis. Aesthet Surg J. 2008;28(3):313–321. doi: 10.1016/j.asj.2008.02.004. quiz 322–324. [DOI] [PubMed] [Google Scholar]
- 78.Lam SM, Glasgold RA, Glasgold MJ. Limitations, complications, and long-term sequelae of fat transfer. Facial Plast Surg Clin North Am. 2008;16(4):391–399, v. doi: 10.1016/j.fsc.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 79.Prado RP, Garcia SB, Thomazini JA, Piccinato CE. Effects of 830 and 670 nm laser on viability of random skin flap in rats. Photomed Laser Surg. 2012;30(8):418–424. doi: 10.1089/pho.2011.3042. [DOI] [PubMed] [Google Scholar]
- 80.Pinfildi CE, Hochman BS, Nishioka MA, Sheliga TR, Neves MA, Liebano RE, Ferreira LM. What is better in TRAM flap survival: LLLT single or multi-irradiation? Lasers Med Sci. 2013;28(3):755–761. doi: 10.1007/s10103-012-1130-3. [DOI] [PubMed] [Google Scholar]
- 81.Ion L, Raveendran SS, Fu B. Body-contouring with radio-frequency-assisted liposuction. J Plast Surg Hand Surg. 2011;45(6):286–293. doi: 10.3109/2000656X.2011.613263. [DOI] [PubMed] [Google Scholar]
- 82.Kirkham JC, Lee JH, Medina MA. III, McCormack MC, Randolph MA, Austen WG, Jr. The impact of liposuction cannula size on adipocyte viability. Ann Plast Surg. 2012;69(4):479–481. doi: 10.1097/SAP.0b013e31824a459f. [DOI] [PubMed] [Google Scholar]
- 83.Agostini T, Lazzeri D, Pini A, Marino G, Li Quattrini A, Bani D, Dini M. Wet and dry techniques for structural fat graft harvesting: Histomorphometric and cell viability assessments of lipoaspirated samples. Plast Reconstr Surg. 2012;130(2):331e–339e. doi: 10.1097/PRS.0b013e3182589f76. [DOI] [PubMed] [Google Scholar]
- 84.Aziz-Jalali MH, Tabaie SM, Djavid GE. Comparison of red and infrared low-level laser therapy in the treatment of acne vulgaris. Indian J Dermatol. 2012;57(2):128–130. doi: 10.4103/0019-5154.94283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yu HS, Wu CS, Yu CL, Kao YH, Chiou MH. Helium-neon laser irradiation stimulates migration and proliferation in melanocytes and induces repigmentation in segmental-type vitiligo. J Invest Dermatol. 2003;120(1):56–64. doi: 10.1046/j.1523-1747.2003.12011.x. [DOI] [PubMed] [Google Scholar]