Abstract
Context
Elderly patients have more cardiovascular risk factors and a greater burden of ischemic disease than younger patients.
Aims
To examine the impact of age on clinical presentation and outcomes in patients presenting with acute coronary syndrome (ACS).
Methods and material
Collected data from the 2nd Gulf Registry of Acute Coronary Events (Gulf RACE-2), which is a prospective multicenter study from six adjacent Arab Middle Eastern Gulf countries. Patients were divided into 3 groups according to their age: ≤50 years, 51–70 years and >70 years and their clinical characteristics and outcomes were analyzed. Mortality was assessed at one and 12 months.
Statistical analysis used
One-way ANOVA test for continuous variables, Pearson chi-square (X2) test for categorical variables and multivariate logistic regression analysis for predictors were performed.
Results
Among 7930 consecutive ACS patients; 2755 (35%) were ≤50 years, 4110 (52%) were 51–70 years and 1065 (13%) >70 years old. The proportion of women increased with increasing age (13% among patients ≤50 years to 31% among patients > 70 years). The risk factor pattern varied with age; younger patients were more often obese, smokers and had a positive family history of CAD, whereas older patients more likely to have diabetes mellitus, hypertension, and dyslipidemia. Advancing age was associated with under-treatment evidence-based therapies. Multivariate logistic regression analysis after adjusting for relevant covariates showed that old age was independent predictors for re-ischemia (OR 1.29; 95% CI 1.03–1.60), heart failure (OR 2.8; 95% CI 2.17–3.52) and major bleeding (OR 4.02; 95% CI 1.37–11.77) and in-hospital mortality (age 51–70: OR 2.67; 95% CI 1.86–3.85, and age >70: OR 4.71; 95% CI 3.11–7.14).
Conclusion
Despite being higher risk group, elderly are less likely to receive evidence-based therapies and had worse outcomes. Guidelines adherence is highly recommended in elderly.
Keywords: Acute coronary syndrome, Age, Elderly
1. Introduction
Coronary artery disease (CAD) is the leading cause of death worldwide, particularly in elderly patients.1 Previous studies addressed the need to define the impact of age across the spectrum of acute coronary syndromes (ACS).2 According to the American Heart Association (AHA) statistics, 83% of CAD deaths were in patients' ≥65 years of age.3 The expected mortality rates from ACS increase by an odds ratio of 1.7 for each 10-year increment over age 65 years.4 Elderly patients have more cardiovascular risk factors and a greater burden of ischemic disease than younger patients and therefore, they derive a greater absolute benefit from evidence-based therapies including revascularization. However, they are also more likely to experience procedural complications, owing to age-related physiological changes, frailty, and comorbidities.
Although the American College of Cardiology/American Heart Association (ACC/AHA) guidelines clearly state that a patient's age should not influence decisions about cardiac care, elderly patients are much less likely to receive evidence-based therapies compared to their younger counterparts.5,6 Despite increasing prevalence and burden of CAD, the elderly are often underrepresented in many cardiovascular clinical trials, and the proportion of the elderly included in clinical registries remains low.7 Therefore, relatively little is known about the management and outcomes of ACS in the elderly. Furthermore, the vast majority of studies was conducted in the developed world and mainly included Caucasian patients. Data on the outcome of elderly ACS patients among other ethnicities are scarce. In the current study we evaluate the impact of age on clinical presentation and short- and long-term clinical outcomes in the Arab Middle Eastern population.
2. Materials and methods
Data were collected from a prospective, multicenter study of the 2nd Gulf Registry of Acute Coronary Events (Gulf RACE-2) between October 2008 and June 2009. We recruited 7930 consecutive ACS patients from six adjacent Middle Eastern Gulf countries (Bahrain, Kingdom of Saudi Arabia, Qatar, Oman, United Arab Emirates, and Yemen). Patients diagnosed with ACS, including unstable angina (UA) and non-ST- and ST-elevation myocardial infarction (NSTEMI and STEMI, respectively), were enrolled from 65 hospitals. On-site cardiac catheterization laboratory was available in 43% of the participating hospitals. There were no exclusion criteria, and thus, all the prospective patients with ACS were actually enrolled. The study received ethics approval from the institutional review boards in all participating countries. Diagnosis of the different types of ACS and definitions of data variables were based on the American College of Cardiology (ACC) clinical data standards.8 A Case Report Form (CRF) for each patient with suspected ACS was filled out upon hospital admission by assigned physicians and/or research assistants using standard definitions and was completed throughout the patient's hospital stay. All CRFs were verified by a cardiologist and then sent online to the principal coordinating center, where the forms were further checked for mistakes before submission for final analysis.9
2.1. Statistical analysis
Data were presented as proportions or mean ± standard deviation (SD) as appropriate. Baseline demographic characteristics, past medical history, clinical presentation, medical therapy, cardiac procedures and clinical outcomes were compared between the three age groups (≤50, 51–70, and >70 years).10 Statistical analyses were conducted using one-way ANOVA test for continuous variables and Pearson chi-square (X2) test for categorical variables. The clinical hospital outcomes included recurrent ischemia, myocardial reinfarction, heart failure (HF), shock, stroke, major bleedings and mortality. Mortality was assessed also at 1 month and 12 months after discharge. In order to assess the independent association of age with clinical outcomes, a multivariate logistic regression analysis was performed. We included important variables in the analysis that predicted the outcomes of interest. These variables included age, sex, diabetes mellitus, hypertension, dyslipidemia, current smoking, renal failure, and medications. All P-values were the results of two-tailed tests and values <0.05 were considered significant. Data analysis was carried out using the Statistical Package for Social Sciences Version 18 (SPSS Inc. USA).
3. Results
3.1. Baseline patient characteristics
The clinical characteristics of 7930 patients are presented in Table 1 according to age group. The patients' ages ranged from 21 to 105 years with a mean age of 57 ± 13 years; 2755 (35%) were ≤50 years old, 4110 (52%) were 51–70 years old and 1065 (13%) >70 years old. Women were increasingly represented with increasing age comprising 13% of patients ≤50 years and reaching 31% of patients >70 years (P = 0.001). In all age groups, ischemic chest pain was the most frequent symptom at hospital admission. Elderly patients were more likely to have diabetes mellitus, hypertension and dyslipidemia (P = 0.001). Current smoking and family history of CAD were more prevalent in patients ≤50 years and were least in those >70 years (P = 0.001). A higher diastolic blood pressure and body mass index were prevalent in patients ≤70 years (P = 0.001). Also, a higher total cholesterol, serum triglyceride and low-density lipoprotein were more prevalent in patients ≤70 years (P = 0.001). Conversely, elderly patients were more likely to have comorbidities such as renal failure, prior myocardial infarction (MI), prior coronary artery bypass graft surgery (CABG), prior stroke and prior peripheral arterial disease (PAD) (P = 0.001). Fasting blood sugar was higher in patients ≤70 years (P = 0.001), but there was no difference in hemoglobin A1c between elderly patients and patients ≤50 years (P = 0.09).
Table 1.
Baseline demographic and clinical characteristics.
| Variables | ≤50 Years | 51–70 Years | >70 Years | P-value |
|---|---|---|---|---|
| Number (%) | 2755 (35%) | 4110 (52%) | 1065 (13%) | |
| Sex (females) | 12.5 | 24.7 | 30.8 | 0.001 |
| Diabetes mellitus | 30.9 | 44.9 | 45.6 | 0.001 |
| Hypertension | 34 | 53.8 | 59.7 | 0.001 |
| Dyslipidemia | 29.9 | 41 | 42.8 | 0.001 |
| Current smoker | 67.3 | 48.1 | 33.7 | 0.001 |
| Renal failure | 1.3 | 4.5 | 9.5 | 0.001 |
| Family history of CAD | 13.4 | 11.1 | 8.6 | 0.001 |
| Prior MI | 14.1 | 21.9 | 26.6 | 0.001 |
| Prior PCI | 6.5 | 11 | 9.5 | 0.001 |
| Prior CABG | 1.5 | 5.1 | 7.9 | 0.001 |
| Prior stroke | 1.7 | 4.8 | 9.3 | 0.001 |
| Prior PAD | 0.8 | 2.1 | 3.7 | 0.001 |
| Heart rate (beats/min) (mean ± SD) | 83.6 ± 18 | 84.8 ± 20.9 | 85.6 ± 22 | 0.001 |
| Systolic blood pressure (mmHg) (mean ± SD) | 132.9 ± 26 | 137 ± 30 | 136 ± 31 | 0.001 |
| Diastolic blood pressure (mmHg) (mean ± SD) | 82.7 ± 17.5 | 81.2 ± 17.8 | 77.9 ± 18 | 0.001 |
| Body mass index (Kg/m2) (mean ± S.D) | 27 ± 5 | 27.2 ± 5.5 | 26 ± 5.4 | 0.001 |
| Fasting blood sugar (mmol/l) (mean ± S.D) | 7.2 ± 3.3 | 7.5 ± 3.2 | 7.1 ± 2.9 | 0.001 |
| Total cholesterol (mmol/l) (mean ± S.D) | 5.0 ± 1.3 | 4.9 ± 1.6 | 4.7 ± 2.1 | 0.001 |
| Serum triglyceride (mmol/l) (mean ± S.D) | 2.0 ± 1.3 | 1.8 ± 1.05 | 1.5 ± 0.8 | 0.001 |
| Low-Density Lipoprotein (mmol/l) (mean ± S.D) | 3.3 ± 1.2 | 3.1 ± 1.4 | 2.8 ± 1.2 | 0.001 |
| High-Density Lipoprotein (mmol/l) (mean ± S.D) | 1.01 ± 0.5 | 1.1 ± 0.5 | 1.1 ± 0.4 | 0.001 |
| Troponin T (mean ± S.D) | 1.21 ± 0.4 | 1.3 ± 0.44 | 1.24 ± 0.42 | 0.001 |
| Hemoglobin A1c (mean ± S.D) | 7.6 ± 2.4 | 7.8 ± 2.4 | 7.5 ± 2.2 | 0.09 |
| Killip class >1 | 14.3 | 24.9 | 62.1 | 0.001 |
| Symptom >12 h | 58.3 | 59 | 54.9 | 0.49 |
| Ischemic chest pain | 90.2 | 82.9 | 73.0 | 0.001 |
| Atypical chest pain | 4.1 | 5.3 | 6.6 | 0.001 |
| Dyspnea | 3.3 | 7.7 | 14.1 | 0.001 |
| ST-elevation MI | 55.4 | 40.7 | 31.6 | 0.001 |
| NST-elevation MI | 23.8 | 31.3 | 41.7 | 0.001 |
| Unstable angina | 20.3 | 26.9 | 25.1 | 0.001 |
CAD = coronary artery disease, MI = myocardial infarction, PCI = percutaneous coronary intervention, CABG = coronary artery bypass graft, PAD = peripheral arterial disease, NST = non-ST.
3.2. Clinical presentation
Elderly patients presented less frequently with typical ischemic chest pain in comparison to the other age groups (P = 0.001). Atypical chest pain was more prevalent (6.6%) in patients >70 years old than in other age groups (P = 0.001). Presentation with dyspnea was less frequent in the youngest age group when compared to the elderly (3.3% and 14% respectively). The proportion of patients with Killip class >1 increased with age (P = 0.001). However, the interval from chest pain onset to emergency department arrival was not influenced by age (P = 0.49).
3.3. Acute coronary artery syndrome type
Of the 7930 patients, 3613 (46%) presented with STEMI, 2386 (30%) with NSTEMI and 1931 (24%) with UA. STEMI decreased with increasing age from 55% of patients aged <50 years to 32% of patients >70 years (P = 0.001). Conversely, NSTEMI increased with increasing age from 24% of patients aged ≤50 years to 42% of patients >70 years (P = 0.001). Unstable angina (UA) was lesser in frequency (20%) in patients ≤50 years of age than in other age groups (25–27%; P = 0.001).
3.4. Management
The proportion of patients who received in-hospital management in a specific age group is shown in Table 2. The use of aspirin, clopidogrel, beta-blockers and statins was more prevalent in patients ≤70 years of age (P = 0.001 for all). The use of angiotensin converting enzyme (ACE) inhibitors/angiotensinogen receptor blockers (ARBs) was similar among age groups (P = 0.08). Elderly patients with STEMI were less likely (28%) to receive thrombolytic therapy than in other age groups (47%–61%, P = 0.001). Also, they were less likely to receive glycoprotein (GP) inhibitors and heparin. On discharge, elderly patients >70 years old were less likely to be treated by aspirin (89% vs. 95%), clopidogrel (58% vs. 76%), beta-blockers (72% vs. 83%) and statins (87% vs. 94%) than those ≤50 years (P = 0.001 for all). The use of ACE inhibitors/ARBs was not significantly influenced by age (P = 0.24).
Table 2.
Medical therapy, cardiac procedures and interventions.
| Variables | ≤50 Years | 51–70 Years | >70 Years | P-value |
|---|---|---|---|---|
| 1st 24 h therapy in % | ||||
| Aspirin | 98.8 | 98.3 | 97.3 | 0.009 |
| Clopidogrel | 82.8 | 74 | 67.2 | 0.001 |
| Beta-blockers | 78.1 | 73.6 | 67.4 | 0.001 |
| ACE inhibitors/ARBs | 73.9 | 78.3 | 75.7 | 0.08 |
| Statins | 96.3 | 94.4 | 92.4 | 0.001 |
| Thrombolytic therapy | 60.5 | 46.9 | 27.7 | 0.001 |
| GP inhibitors | 7.4 | 6.6 | 4.7 | 0.013 |
| Heparin | 14.6 | 12.5 | 11.5 | 0.004 |
| LMWH | 41 | 38 | 39 | 0.04 |
| Coronary angiography % | 34.7 | 32.5 | 26.5 | 0.001 |
| 1-vessel CAD | 12.3 | 8.6 | 6.4 | 0.001 |
| 2-vessel CAD | 8.3 | 8.4 | 4.8 | 0.001 |
| 3-vessel CAD | 7.8 | 10.4 | 12.0 | 0.001 |
| PCI % | 17 | 14.1 | 11 | 0.001 |
| CABG % | 2.3 | 3.2 | 3.7 | 0.001 |
| Echocardiogram % | 77.8 | 75.6 | 76.3 | 0.12 |
| Mild LV dysfunction (LVEF 40–50%) | 42.6 | 40.7 | 36.8 | 0.001 |
| Moderate LV dysfunction (LVEF 30–39%) | 15.5 | 18.6 | 21.9 | 0.001 |
| Severe LV dysfunction (LVEF 30%) | 6 | 8.5 | 14.6 | 0.001 |
| Discharge medications % | ||||
| Aspirin | 95.4 | 92.2 | 88.6 | 0.001 |
| Clopidogrel | 75.7 | 65.1 | 58.7 | 0.001 |
| Beta-blockers | 82.9 | 78.6 | 72.2 | 0.001 |
| ACE inhibitors/ARBs | 77.6 | 78.3 | 75.9 | 0.24 |
| Statins | 93.9 | 90.7 | 86.8 | 0.001 |
Elderly patients were less likely to have coronary angiography (27%) than in other age groups (33–35%, P = 0.001). Single-vessel disease was more common in patients ≤50 years old, while three-vessel disease was more prevalent with increasing age (P = 0.001). Patients >70 years old were less likely to be treated by percutaneous coronary intervention (PCI) (11%) than in other age groups (14%–17%, P = 0.001) and CABG increased from 2% among patients ≤50 years to 4% in patients >70 years (P = 0.001). Older patients had significantly lower left ventricular ejection fraction (LVEF) than younger patients.
3.5. Clinical outcomes
Elderly patients had more unfavorable hospital outcomes compared with younger patients in terms of myocardial re-ischemia, heart failure, cardiogenic shock, stroke, major bleeding and mortality when compared to patients ≤50 years (Tables 3 and 4). Multivariate logistic regression analysis after adjusting for relevant covariates showed that old age was independent predictors for re-ischemia (OR 1.29; 95% CI 1.03–1.60), heart failure (OR 2.8; 95% CI 2.17–3.52) and major bleeding (OR 4.02; 95% CI 1.37–11.77).
Table 3.
In-hospital and long-term outcomes.
| Variables (%) | ≤50 Years | 51–70 Years | >70 Years | P-value |
|---|---|---|---|---|
| Re-ischemia | 13.9 | 16 | 17.5 | 0.007 |
| Re-infarction | 1.9 | 2.1 | 3.2 | 0.04 |
| Congestive heart failure | 7.4 | 14.4 | 23.3 | 0.001 |
| Cardiogenic shock | 3.8 | 6 | 10 | 0.001 |
| Stroke | 0.4 | 0.8 | 1 | 0.05 |
| Major bleeding | 0.3 | 0.6 | 1.3 | 0.001 |
| In-hospital mortality | 2 | 5 | 10 | 0.001 |
| 1-month mortality | 4 | 9 | 15 | 0.001 |
| 12-month mortality | 6 | 13.5 | 25 | 0.001 |
Table 4.
Multivariate Logistic regression for in-hospital, 1- and 12-month mortality.
| Variable | In-hospital mortality |
1-Month mortality |
12-Month mortality |
|||
|---|---|---|---|---|---|---|
| OR | 95% C.I | OR | 95% C.I | OR | 95% C.I | |
| Gender male | 0.70 | 0.51–0.95 | 0.75 | 0.58–0.96 | 0.84 | 0.67–1.04 |
| Diabetes mellitus | 1.28 | 0.95–1.73 | 1.17 | 0.92–1.49 | 1.29 | 1.05–1.59 |
| Hypertension | 1.06 | 0.80–1.39 | 0.98 | 0.79–1.22 | 1.05 | 0.87–1.28 |
| Dyslipidemia | 0.60 | 0.43–0.79 | 0.74 | 0.58–0.93 | 0.85 | 0.69–1.04 |
| Renal failure | 1.55 | 0.95–2.53 | 1.55 | 1.03–2.31 | 1.49 | 1.05–2.12 |
| Smoking | 0.92 | 0.70–1.24 | 1.06 | 0.84–1.34 | 0.90 | 0.73–1.10 |
| Aspirin | 0.62 | 0.34–1.15 | 0.71 | 0.41–1.25 | 0.77 | 0.45–1.33 |
| Clopidogrel | 1.34 | 1.0–1.79 | 1.21 | 0.95–1.53 | 1.00 | 0.82–1.23 |
| β-Blocker | 0.26 | 0.20–0.34 | 0.34 | 0.28–0.41 | 0.44 | 0.37–0.53 |
| ACE inhibitor | 0.29 | 0.22–0.37 | 0.51 | 0.41–0.63 | 0.61 | 0.50–0.75 |
| Statin | 0.43 | 0.30–0.62 | 0.52 | 0.38–0.72 | 0.56 | 0.41–0.76 |
| PCI | 0.51 | 0.30–0.86 | 0.54 | 0.36–0.79 | 0.53 | 0.38–0.74 |
| Age groupa | ||||||
| 51–70 Years | 2.67 | 1.86–3.85 | 2.31 | 1.75–3.03 | 2.16 | 1.70–2.85 |
| >70 Years | 4.71 | 3.11–7.14 | 3.74 | 2.71–5.17 | 4.10 | 3.10–5.42 |
CI = confidence interval, OR = odd ratio, PCI = percutaneous coronary intervention.
The reference group is age ≤50 years.
One- and twelve-month mortality rate was higher in elderly (P = 0.001 for all) (Fig. 1). Age >50 was independent predictor for in-hospital mortality (OR 2.67; 95% CI 1.86–3.85, for age 51–70 and OR 4.71; 95% CI 3.11–7.14, for age >70).
Fig. 1.
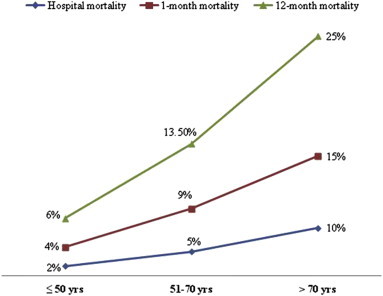
Hospital, 1-month and 12-month mortality in patients presenting with acute coronary syndrome according to age groups.
4. Discussion
The current study demonstrates the paradox of under-treatment of older higher risk ACS Middle Eastern patients with evidence-based therapies. Older patients had higher risk of adverse hospital outcomes, short- and long-term mortality rates when compared to younger patients.
Patients in the current registry (Gulf RACE-2), with a mean age of 57 years were of comparable age to those in the CREATE (Treatment and outcomes of acute coronary syndromes in India) registry,10 and 6 years younger than patients in the Euro Heart Surveys of ACS.11,12 This difference in age at presentation may be due to the higher prevalence of CAD risk factors in our study. As in a previous study,2 the proportion of women increased with increasing age and the risk factor pattern also varied with age. The most prevalent CAD risk factors in the younger patients were smoking; higher body mass index and a higher prevalence of positive family history of CAD, whereas history of diabetes mellitus, hypertension, dyslipidemia, prior cardiovascular disease and prior cerebrovascular events were more often seen in elderly patients. This variation in risk factor patterns in young and elderly patients highlights the urgent need for a real effort and international awareness of primary and secondary prevention of CAD.
4.1. Clinical presentation and ACS type
Elderly ACS patients were more likely to present with atypical chest pain than younger patients putting them at increased risk for misdiagnosis. Previous studies13–19 demonstrated that between 0.4% and 10% of patients who have acute MI were incorrectly discharged from the emergency department. Moreover, four subgroups of patients were at greater risk for misdiagnosis, including the very young and very old patients, women, as well as diabetics. Because of atypical presentation, a high index of suspicion for ACS is advisable in the elderly.
The presence of heart failure increased significantly with increasing age as shown in other registries.7,18,20 Similar to previous studies2,19 our study demonstrated that elderly with MI were more likely to have NSTEMI and the proportion of STEMI decreased with increasing age. Also, Mehta et al, demonstrated that STEMI accounted only for ≤30% of all elderly patients admitted with ACS.21
4.2. Hospital management and outcomes
Age is the most important determinant of ACS outcomes.22 Although elderly patients were more likely to have worse clinical profile; they were less likely to receive guideline-recommended medical and interventional therapies. Previous studies13,19,23–25 reported similar age-dependent results. The ACC/AHA guidelines (2004) on the management of STEMI and the 2007 ACC/AHA focused update did not recommend an age limitation to fibrinolytic therapy, and prompt reperfusion for patients with STEMI is a Class I guideline recommendation and has been shown to reduce mortality.6 In the present study, elderly patients with STEMI were less likely to receive thrombolysis than younger patients. Only, 28% of STEMI patients >70 years of age received thrombolytic therapy. In TIMI III registry,26 elderly patients were shown to receive less aggressive anti-ischemic therapy and were less likely to undergo coronary angiography, with fewer revascularization procedures than their younger counterparts. Although most elderly patients will benefit from thrombolysis, the risk/benefit ratio has to be evaluated on a case-by-case basis to optimize outcome. Also, in the present study, the proportion of ACS patients treated by PCI decreased significantly with age.
In CRUSADE (Can Rapid stratification of Unstable angina Suppress ADverse outcomes with Early implementation of the American College of Cardiology/American Heart Association guidelines) database7,23 showed that although elderly patients (>90 years old) had a higher risk of bleeding from aggressive treatment, the benefit still outweighed this risk. So, advanced patient age should not be a contraindication for aggressive treatment. Lower rate of in-hospital mortality was found in those who were treated with early coronary angiography and revascularization than who were treated with a more delayed conservative approach. Consistent with previous studies13,23 the use of evidenced-based medical therapies at hospital discharge was less often with increasing age except, the use of ACE inhibitors/ARBs was not significantly influenced by patient age. In the present study, coronary artery bypass grafting (CABG) was more prevalent in patients >70 years of age than in other age groups and this may be due to the fact that they more likely presented with more severe and extensive CAD hence warranting consideration of surgical revascularization.27 Similar findings were observed in a prior study,19 where the rate of CABG surgery was the highest among patients aged 65–74 years.
Consistent with previous studies,4,13,19,22 the risk of myocardial re-ischemia, reinfarction, heart failure, cardiogenic shock, major bleeding and in-hospital mortality was more prevalent in the elderly than in the other age group. Consistent with findings from GRACE (Global registry of acute coronary events),18 the risk of 12-month mortality increased with increasing patient age. After adjustment for patient and hospital factors, the odds ratio of 12-month mortality for older age groups compared with age ≤50 was 2.16 for patients aged 51–70 years, 4.10 for those aged >70 years (Table 4).
The overall worse prognosis in the elderly is likely due to multiple factors that include increasing age itself,2,22 greater co-morbidity, extensive CAD disease, impaired left ventricular systolic function28 and the under-use of Guideline-recommended medical and interventional therapies.2,22,23 The magnitude of the effect of adherence to guideline-recommended therapies was illustrated in an observational study. Every 10% increase in composite adherence to ACC/AHA guideline-recommended therapies was associated with a 10% reduction of in-hospital mortality.29
4.3. Limitations
Our data were collected from an observational study. The fundamental limitations of observational studies cannot be eliminated because of the nonrandomized nature and unmeasured confounding factors. However, well-designed observational studies provide valid results and do not systemically overestimate the results compared with the results of randomized controlled trials.
5. Conclusions
Despite being a high-risk group, elderly patients presenting with ACS were less likely to receive guideline-recommended therapies. They had a high rate of adverse hospital outcomes and short- and long-term mortality. Guidelines' adherence and improvement in hospital care for elderly patients with ACS may potentially improve the outcomes and save a substantial number of patients.
Funding
Gulf RACE is a Gulf Heart Association (GHA) project and was financially supported by the GHA, Sanofi Aventis, and the College of Medicine Research Center at King Khalid University Hospital, King Saud University, Riyadh, Saudi Arabia. The sponsors had no role in study design, data collection, data analysis, writing of the report, or submission of the manuscript. Ethical approvals were obtained prior to the study.
Conflicts of interest
All authors have none to declare.
Acknowledgment
We thank the staff in all the participating centres for their invaluable cooperation. Special thanks to Zenaida Ramoso and Kazi NurAsfina for data coordination and secretarial assistance, and also to the physicians who participated in this registry.
Footnotes
This study was presented in part in the World Heart federation, WCC, 18–21 April, 2012, Dubia, United Arab Emirates.
References
- 1.Lopez A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Rosengren A., Wallentin L., Simoons M. Age, clinical presentation, and outcome of acute coronary syndromes in the euro heart acute coronary syndrome survey. Eur Heart J. 2006;27:789–795. doi: 10.1093/eurheartj/ehi774. [DOI] [PubMed] [Google Scholar]
- 3.Rosamond W., Flegal K., Furie K. Heart disease and stroke statistics-2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 4.Granger C.B., Goldberg R.J., Dabbous O., Global Registry of Acute Coronary Events Investigators Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 5.Wright R.S., Anderson J.L., Adams C.D. 2011 ACCF/AHA focused update of the guidelines for the management of patients with unstable Angina/Non-ST-elevation myocardial infarction (updating the 2007 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice guidelines developed in collaboration with the American College of Emergency physicians, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;57:1920–1959. doi: 10.1016/j.jacc.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Kushner F.G., Hand M., Smith S.C., Jr. 2009 Focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Skolnick A.H., Alexander K.P., Chen A.Y. Characteristics, management, and outcomes of 5,557 patients age ≥90 years with acute coronary syndromes: results from the CRUSADE initiative. J Am Coll Cardiol. 2007;49:1790–1797. doi: 10.1016/j.jacc.2007.01.066. [DOI] [PubMed] [Google Scholar]
- 8.Cannon C.P., Battler A., Brindis R.G. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee) J Am Coll Cardiol. 2001;38:2114–2130. doi: 10.1016/s0735-1097(01)01702-8. [DOI] [PubMed] [Google Scholar]
- 9.El-Menyar A., AlHabib K.F., Al-Motarreb A. Prior antiplatelet use and cardiovascular outcomes in patients presenting with acute coronary syndromes. Am J Cardiovasc Drugs. 2012;12:127–135. doi: 10.2165/11597580-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 10.Xavier D., Pais P., Devereaux P.J. CREATE registry investigators. Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 11.Hasdai D., Behar S., Wallentin L. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS) Eur Heart J. 2002;23:1190–1201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- 12.Mandelzweig L., Battler A., Boyko V. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 13.Bean D.B., Roshon M., Garvey J.L. Chest pain: diagnostic strategies to save lives, time, and money in the ED. Emerg Med Pract. 2003;5:1–32. [Google Scholar]
- 14.Boie E.T. Initial evaluation of chest pain. Emerg Med Clin North Am. 2005;23:937–957. doi: 10.1016/j.emc.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Swap C.J., Nagurney J.T. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005;294:2623–2629. doi: 10.1001/jama.294.20.2623. [DOI] [PubMed] [Google Scholar]
- 16.Croskerry P. Achilles heels of the ED: delayed or missed diagnoses. ED Legal Lett. 2003;14:109–120. [Google Scholar]
- 17.Haro L.H., Decker W.W., Boie E.T., Wright R.S. Initial approach to the patient who has chest pain. Cardiol Clin. 2006;24:1–17. doi: 10.1016/j.ccl.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Brieger D., Eagle K.A., Goodman S.G. Acutecoronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the global registry of acute coronary events – 2004. Chest. 2009;136(5 suppl):e30. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 19.Avezum A., Makdisse M., Spencer F., GRACE Investigators Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE) Am Heart J. 2005;149:67–73. doi: 10.1016/j.ahj.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Alexander K.P., Newby L.K., Armstrong P.W. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2570–2589. doi: 10.1161/CIRCULATIONAHA.107.182616. [DOI] [PubMed] [Google Scholar]
- 21.Mehta R.H., Rathore S.S., Radford M.J., Wang Y., Wang Y., Krumholz H.M. Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol. 2001;38:736–741. doi: 10.1016/s0735-1097(01)01432-2. [DOI] [PubMed] [Google Scholar]
- 22.Alexander K.P., Newby L.K., Cannon C.P. Acute coronary care in the elderly, part I: non-ST-Segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2549–2569. doi: 10.1161/CIRCULATIONAHA.107.182615. [DOI] [PubMed] [Google Scholar]
- 23.Alexander K.P., Roe M.T., Chen A.Y. Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative. J Am Coll Cardiol. 2005;46:1479–1487. doi: 10.1016/j.jacc.2005.05.084. [DOI] [PubMed] [Google Scholar]
- 24.Schoenenberger A.W., Radovanovic D., Stauffer J.C. Age-related difference in the use of guideline-recommended medical and interventional therapies for acute coronary syndromes: A cohort study. J Am Geriatr Soc. 2008;56:510–516. doi: 10.1111/j.1532-5415.2007.01589.x. [DOI] [PubMed] [Google Scholar]
- 25.Collinson J., Bakhai A., Flather M., Fox K. The management and investigation of elderly patients with acute coronary syndromes without ST elevation: an evidence-based approach? Results of the prospective registry of acute ischemic syndromes in the United Kingdom (PRAIS-UK) Age Ageing. 2005;34:61–66. doi: 10.1093/ageing/afh236. [DOI] [PubMed] [Google Scholar]
- 26.Stone P.H., Thompson B., Anderson H.V. Influence of race, sex, and age on management of unstable angina and non-Q-wave myocardial infarction: the TIMI III registry. JAMA. 1996;275:1104–1112. [PubMed] [Google Scholar]
- 27.Aronow W.S., Fleg J., editors. Cardiovascular Disease in the Elderly. 3rd ed. Marcel Dekker, Inc; New York: 2004. [Google Scholar]
- 28.Jaber W.A., Prior D.L., Marso S.P., Houghtaling P.L., Menon V., Harrington R.A. CHF on presentation is associated with markedly worse outcomes among patients with acute coronary syndromes: PURSUIT trial findings. Circulation. 1999;100(suppl 1):1–433. [Google Scholar]
- 29.Peterson E.D., Roe M.T., Mulgund J. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295:1912–1920. doi: 10.1001/jama.295.16.1912. [DOI] [PubMed] [Google Scholar]


