Abstract
Objective:
We aimed to systematically assess the evidence for differences in the incidence of stroke and distribution of its subtypes in Chinese compared with white populations.
Methods:
We comprehensively sought studies conducted since 1990 in Chinese populations of 1) first-ever stroke incidence (community-based studies only), and 2) pathologic types/subtypes of stroke (hospital- or community-based studies of first-ever or recurrent strokes). We identified community-based studies in white populations from a recent systematic review. For each study, we calculated age-standardized stroke incidence and the proportions of each pathologic type and ischemic subtype, using random-effects meta-analysis to pool proportions of stroke types/subtypes in Chinese and in white populations.
Results:
Age-standardized annual first-ever stroke incidence in community-based studies was higher among Chinese than white populations (for ages 45–74 years, range 205–584 vs 170–335 per 100,000, respectively). Intracerebral hemorrhage accounted for a larger, more variable proportion of strokes in China than Taiwan (range 27%–51% vs 17%–28%), in Chinese community-based than hospital-based studies (27%–51% vs 17%–30%), and in community-based Chinese than white studies (pooled proportion 33% vs 12%). Although the overall proportion of lacunar ischemic stroke appeared higher in Chinese than white populations, variable study methodologies precluded reliable comparisons.
Conclusions:
There is good evidence for a slightly higher overall stroke incidence and higher proportion of intracerebral hemorrhage in Chinese vs white populations, but no clear evidence for different distributions of ischemic stroke subtypes. Studies using comparable, population-based case ascertainment and similar classification methods are needed to address this.
Stroke is the second most common cause of death worldwide, and a major global cause of disability. Its increasing global impact in the decades ahead is predicted to be greatest in middle-income countries. These include China, which accounts for almost one-fifth of the world's total population and where stroke is already the leading cause of death and adult disability.1–3
Stroke is a clinical syndrome with 3 main pathologic types (ischemic stroke, intracerebral hemorrhage [ICH], and subarachnoid hemorrhage [SAH]). Each has several subtypes with distinct underlying vascular pathologies. Compared with white populations of European origin, Chinese populations have been reported to have a higher incidence of stroke overall, a higher proportion of ICH, and a different distribution of ischemic stroke subtypes.4–8 However, reliable comparisons have been precluded by a lack of methodologically robust studies of stroke incidence among Chinese populations, age standardization of incidence rates in different studies to different standard populations, and variable methods for classifying stroke types and subtypes.9,10 Furthermore, no previous review of the epidemiology of stroke in Chinese populations has taken an explicitly systematic approach.
To clarify what is known and what remains uncertain about the epidemiology of stroke in Chinese populations and differences from white populations, we aimed to systematically evaluate the incidence of stroke and the distribution of its main pathologic types and ischemic subtypes in Chinese populations, and to compare these with data from white populations, standardized to the same world population.
METHODS
Search strategy and selection criteria.
We comprehensively sought articles published in any language on incidence of stroke and its pathologic types and subtypes in populations of Chinese origin. We used electronic searches in Medline and EMBASE from 1990 (because before this, brain imaging with CT or MRI was not widely used) to January 2012 (appendices e-1 and e-2 on the Neurology® Web site at www.neurology.org), citation searches of relevant reviews,7,9 and perusal of the reference lists of included primary articles and relevant reviews.
We adapted inclusion criteria from those proposed for an “ideal” study of stroke incidence11,12: standard World Health Organization, National Institute of Neurological Disorders and Stroke, or Atherosclerosis Risk in Communities definition of stroke13–15; first-ever strokes from a large, well-defined population; comprehensive, community-based ascertainment—including fatal and nonfatal cases not admitted to hospital—using multiple overlapping sources (primary- and secondary-care clinics, hospital admissions, death certificates, etc.); prospective study design, ideally with “hot pursuit” of cases; lower age limit 45 years or younger; no upper age limit; data collection from 1990 onward; and numbers of first-ever stroke cases per year and of people in the population (or age-specific annual incidence) available in 10-year mid-decade age bands.
For studies of pathologic types and subtypes of stroke, we relaxed the above criteria to include both community-based and hospital-based studies of recurrent as well as first-ever strokes because we expected to find few “ideal” studies. However, for reliable classification of types/subtypes, we required brain CT/MRI (or autopsy) in >70% of cases. Strokes had to be classified as ischemic stroke, ICH, SAH, or unknown pathologic type.16 Ischemic strokes had to be classified into 5 etiologic subtypes (large-artery atherosclerotic, cardioembolic, intracranial small-vessel disease, other determined etiology, and undetermined etiology) according to the Trial of Org 10172 in Acute Ischemic Stroke (TOAST) or National Institute of Neurological Disorders and Stroke classification schemes, or into the 4 anatomical subtypes of the Oxfordshire Community Stroke Project (OCSP) classification scheme (lacunar infarct, total anterior circulation infarct, partial anterior circulation infarct, and posterior circulation infarct).17,18
We excluded studies with highly selected patients, unclear classification methods, or serious data inconsistencies. We sought essential information that was unavailable in the publication(s) directly from the study authors.
Data extraction.
From included studies of overall stroke incidence, we extracted the following information: geographical area of the study; sources of case ascertainment; study period; size and age range of the population; stroke definition; number of first-ever strokes; mean age and sex distribution of stroke cases; the proportion with brain CT or MRI and admission to hospital; and 1-month case fatality. We extracted or calculated age-specific incidence for each 10-year mid-decade age group. From each included study of stroke types/subtypes, we also extracted data on whether it was community- or hospital-based, whether it included recurrent as well as first-ever strokes, stroke type/subtype classification method, and numbers of each pathologic type or ischemic subtype of stroke. One author selected studies and extracted data, resolving uncertainties through discussion with a second.
Comparison studies in white populations.
For comparison, we selected studies performed from 1990 onward in predominantly white populations of European origin from a recent worldwide systematic review of community-based stroke incidence studies.9 We sought relevant additional studies published up to January 2012 through forward citation searches of this review, and perused reference lists of relevant publications identified. We used the same inclusion criteria as outlined above, except that no hospital-based studies were included.
Statistical analysis.
For each included study, we calculated age-standardized (to the World Health Organization standard population) incidence of first-ever-in-a-lifetime stroke per 100,000 person-years and 95% confidence intervals (CIs).19,20 We standardized for sex to a standard population with equal proportions of males and females in each age stratum. To compare studies, we focused on standardized incidence data for ages 45–74 and 45–75+ years, allowing the most comprehensive inclusion of data from all studies.
For stroke type/subtype studies, we calculated the proportions of all strokes of each main pathologic type and the proportions of all ischemic strokes of each ischemic subtype. Where possible, we repeated these calculations using age-standardized incidence data (to obtain the age-adjusted proportion of each type/subtype). We compared community-based vs hospital-based Chinese studies, different geographical areas among the Chinese populations, and Chinese vs white populations by visual inspection of graphical data. Using StatsDirect software (http://www.statsdirect.com), we calculated and compared distributions of random-effects pooled proportions of pathologic types and ischemic subtypes in Chinese and white populations.
RESULTS
Stroke incidence.
Of 3,063 articles describing studies in Chinese populations, 45 were potentially relevant but only 6 (described in 4 articles, all published in English) fulfilled our inclusion criteria (figure e-1A). They included 404,254 people, 2,044,941 person-years, and 3,935 first-ever stroke patients.e1–e4
Characteristics of these studies are shown in table 1. Four were based in China and 2 in Taiwan. Mean age of stroke onset was 66 to 70 years.e2,e4 The proportions of stroke cases with brain imaging varied widely (30%–91%, mean [weighted by study size] 76%). Age-standardized stroke incidence rates across all ages included varied widely (92–328 per 100,000 person-years), but are not fully comparable because of likely substantial variation in the distribution of ages within the open-ended upper age band and exclusion from one study of people younger than 35 years. Age-standardized stroke incidence also varied more than 4-fold among the 7 Chinese cities included in one study, being higher in the north (Harbin) than in the south (Shanghai) of China (data standardized to the world population were not available separately for the 7 cities included in this studye3). As expected, age-specific annual incidence increased with age (figure e-2).
Table 1.
Characteristics of included community-based stroke incidence studies in Chinese populations

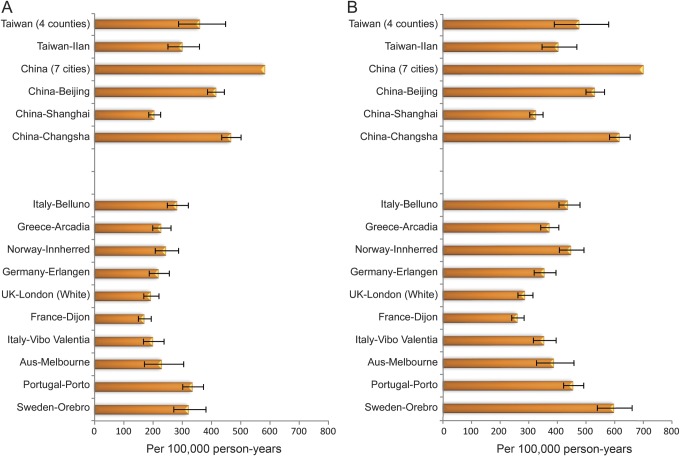
We compared these results from Chinese populations with those from 10 community-based studies among white populations (1,885,067 people, 3,256,868 person-years, and 4,568 first-ever stroke cases). Mean age of stroke onset was younger in Chinese populations (range 66–70 vs 72–76 years). Age-standardized annual first-ever stroke incidence was more variable and somewhat higher among Chinese than white populations for ages 45–74 years (range 205–584 vs 170–335 per 100,000) (figure 1A). There were similar although less marked Chinese-white differences for ages 45–75+ years. These data include many more incident strokes because all ages over 75 years are included, but are less comparable because of age variation in the open-ended upper age band (figure 1B). Additional standardization for sex made no material difference to the results (data not shown).
Figure 1. Age-standardized incidence (per 100,000 person-years) in Chinese and white populations.
Age-standardized incidence (per 100,000 person-years) for (A) ages 45–74 years and (B) ages 45–75+ years. Confidence interval could not be calculated in one study because the number of strokes in each age-specific group was not available.e3
Pathologic types of stroke and ischemic stroke subtypes.
For stroke types/subtypes, from 5,160 articles, 43 studies were potentially relevant, and 25 (11 pathologic type and 14 ischemic subtype studies) described in 17 articles (14 published in English, 3 in Chinese) met our inclusion criteria (figure e-1B).
Of the 11 pathologic type studies, 5 were community-based and 6 were hospital-based (table 2).e2,e5–e12 There were 64,392 first-ever or recurrent stroke cases. Mean age of stroke onset (reported in 8 studies) was 63–73 years; 74%–100% of stroke cases had brain imaging; and 41%–79% of strokes were classified as ischemic, 17%–52% as ICH, 1%–8% as SAH, and 0%–10% as unclassified type. We were only able to calculate age-standardized proportions for one study, and found the age-standardized and crude distributions of pathologic types to be very similar (data not shown).e2
Table 2.
Characteristics of included studies of stroke pathologic type in Chinese populations

For comparison, we identified 13 community-based studies in white populations, including 6,065 first-ever stroke cases. In Chinese populations, a greater, more variable proportion of strokes were ICH type in China than Taiwan (range 27%–51% vs 17%–28%) and in community- than hospital-based studies (27%–51% vs 17%–30%) (figure 2A). Chinese generally had a higher proportion of ICH than white populations (17%–51% vs 6%–20%). The random-effects pooled proportion of ICH was higher in Chinese than in white populations (28.0% [95% CI 23.6%–32.6%] vs 12.4% [95% CI 10.2%–14.7%]), whereas the proportion with unclassified pathologic type was lower in Chinese (1.7% [95% CI 0.5%–3.6%] vs 7.3% [95% CI 5.2%–9.7%]). Considering community-based studies of pathologic types only, the pooled proportion of ICH was even higher in Chinese compared with white populations (33.5% [95% CI 24.4%–43.1% vs 12.4% [95% CI 10.2%–14.7%]), whereas proportions of unclassified stroke type were similar (5.4% [95% CI 3.2%–8.0%] vs 7.3% [95% CI 5.2%–9.7%]) (table e-1).
Figure 2. Distributions of stroke pathologic and ischemic subtypes in Chinese and white populations.
(A) Stroke pathologic types. (B) Ischemic stroke subtypes by TOAST classification. (C) Ischemic stroke subtypes by OCSP classification. C = community-based; CE = cardioembolism; H = hospital-based; ICH = intracerebral hemorrhage; IS = ischemic stroke; L = large-artery atherosclerosis; LACI = lacunar infarct; O = other determined etiology; OCSP = Oxfordshire Community Stroke Project; PACI = partial anterior circulation infarct; POCI = posterior circulation infarct; S = small-vessel occlusion; SAH = subarachnoid hemorrhage; TACI = total anterior circulation infarct; TOAST = Trial of Org 10172 in Acute Ischemic Stroke; U = undetermined etiology; UC = unclassified. *Study in 1995.e13 **Study in 1997.e8
All 14 ischemic stroke subtype studies in Chinese populations were hospital-based; 10 used the TOAST (or similar) etiologic classification and 4 the OCSP anatomical classification (table 3).e8–e10,e13–e23 In total, they included 33,923 first-ever or recurrent stroke cases. Mean age of stroke onset (reported in 10 studies) was 61 to 69 years.
Table 3.
Characteristics of included studies of IS subtype using TOAST and OCSP classifications in Chinese populations

Among the TOAST studies, the proportion of strokes due to large-artery atherosclerosis ranged from 12% to 54%, small-vessel disease 20% to 42%, cardioembolism 10% to 26%, and the combination of other specific determined and undetermined etiology subtypes (presented together because not all studies presented data separately for these 2 subtypes) 4% to 34%. We compared random-effects pooled proportions of ischemic subtypes from these Chinese studies with those from 5 community-based TOAST studies in white populations (including a total of 4,163 ischemic strokes) (figure 2B). Hospital-based studies in Chinese populations had a higher proportion of small-vessel disease stroke (33.1% [95% CI 29.7%–36.7%] vs 19.3% [95% CI 14.7%–24.3%]) and of atherothrombotic stroke (25.4% [95% CI 19.1%–32.3%] vs 14.7% [95% CI 9.0%–21.4%]), and a lower proportion of cardioembolic (15.8% [95% CI 12.8%–19.0%] vs 25.7% [95% CI 22.1%–29.6%]) and other/unknown ischemic stroke (23.2% [95% CI 18.5%–29.2%] vs 38.8% [95% CI 28.0%–50.1%]) (table e-1). However, there was substantial variation in the distribution of ischemic subtypes, especially among the Chinese studies. Few studies in Chinese or white populations reported the proportion of patients undergoing various investigations, such as echocardiography and imaging of the extra- or intracranial arteries. Where reported, investigation rates were low.
Among the hospital-based OCSP studies in Chinese populations, the proportions of different ischemic subtypes were more consistent than among the TOAST studies: lacunar infarction 38%–46%, total or partial anterior circulation infarction 40%–48%, and posterior circulation stroke 10%–18%. Comparison of pooled proportions with one available community-based study in white people showed a slightly higher proportion of lacunar infarction (42.1% [95% CI 38.6%–45 0.7%] vs 32.2% [95% CI 28.7%–35.8%]), and slightly lower proportions of total and partial anterior circulation infarction and posterior circulation stroke in Chinese vs white populations (figure 2C, table e-1). Heterogeneity between individual studies' proportions was substantial in all comparisons of pooled proportions of stroke types and subtypes.
DISCUSSION
To our knowledge, this is the first systematic review of the epidemiology of stroke and its pathologic types and ischemic subtypes comparing data from Chinese populations with data from predominantly white populations of European origin.
We have shown that, compared with white populations, Chinese have a higher age-adjusted incidence of stroke, a lower mean age of stroke onset, and a higher proportion of strokes attributable to ICH. These differences are based on comparisons of methodologically robust community-based studies, with appropriate age standardization, avoiding inclusion of an open-ended upper age band. They are therefore unlikely to be an artifact of variable hospital admission rates or of incomplete adjustment for age. Indeed, the proportion of strokes due to ICH was generally lower in hospital-based than in community-based studies in Chinese. In addition, there was striking variation among Chinese populations both in overall stroke incidence (which varied approximately 3-fold in the age range 45–74) and in the proportion of strokes due to ICH (which varied almost 2-fold among community-based studies).
We have further shown an apparently different distribution of ischemic stroke subtypes among Chinese compared with white populations, with higher overall proportions of small-vessel disease (lacunar) ischemic stroke in Chinese. However, because only hospital-based studies were available from Chinese populations, different hospital admission rates could contribute to the variation among Chinese studies as well as between the Chinese studies and the community-based studies in white populations. In addition, the proportion of strokes in the “other or undetermined” TOAST ischemic stroke subtype category varied widely among the Chinese studies, and was generally lower than among studies in white people. This could be attributable to differences in the interpretation and application of etiologic classification systems for ischemic stroke subtypes, or in the proportion of stroke cases with complete investigation, because the higher this proportion, the lower the proportion assigned an undetermined subtype. The problem of variable investigation rates does not influence the anatomical OCSP classification system, which is based on symptoms and signs, requiring no investigation results beyond a brain scan to exclude hemorrhage. This may explain the more consistent findings among the Chinese studies using the OCSP system, and makes comparisons between studies based on this system more reliable. However, although the OCSP-based Chinese-white comparisons suggest a higher proportion of lacunar ischemic strokes in Chinese populations, only comparisons derived from community-based studies will be able to confirm this finding.
Earlier studies suggested higher stroke incidence in Chinese vs white populations, and variable stroke incidence rates within China (higher rates in the north), but did not include people older than 64 years, and some comparisons included recurrent as well as first-ever strokes.4,21 Our results show reliably that such differences exist after 1990 and extend previous findings to those aged 65 years and older, among whom most strokes occur.
Although previous studies have reported a higher proportion of ICH in Chinese vs white populations, as well as regional variation within China, these have been mostly hospital-based.22,23 Immigration studies provide additional relevant data but there are few studies of stroke incidence and subtypes among Chinese and white people living in the same region.24–26 A recent systematic review of population-based studies of ICH found 2-fold-higher ICH incidence in Asian vs white people, whether living in the same geographical area or in different countries, but included only one study in Chinese and did not consider Chinese populations separately.27
Proposed explanations for Chinese-white differences and variation among Chinese populations in overall stroke incidence and in the proportion of ICH include differences in hypertension, hyperlipidemia, diabetes, obesity, dietary habits (e.g., variable intake of salt and preserved food), smoking, extreme weather, socioeconomic status, and genetic factors.22,23,27 These vary substantially within Chinese populations as well as between Chinese and white populations.21
The Sino-MONICA-Beijing community-based stroke incidence study among people aged 25 to 74 years found, between 1984 and 2004, a 4% increase in age-standardized incidence of all types of stroke, a 5% increase in ischemic stroke, and a 1% decrease in hemorrhagic stroke (ICH and SAH), with a large reduction in the proportion of incident strokes attributed to hemorrhage (43% in 1984 vs 14% in 2004).28 Some—but certainly not all—of this change may be explained by overdiagnosis of hemorrhagic stroke in the 1980s when CT brain scan rates were low. These changes occurred during a time of rapid economic development and increasing adoption of Western lifestyles in China, increased dietary fat and cholesterol intake, increased mean cholesterol levels, increased prevalence of obesity and diabetes, and possibly better hypertension control. Our study shows that the higher proportion of hemorrhagic stroke is attributable to ICH, not SAH, and has persisted in the most recent studies of incident stroke in Chinese populations, even those with highly developed economies, such as Taiwan. However, there are no comparable community-based data yet available after 2000, and further economic and lifestyle changes in mainland China may have further affected stroke rates.
The major strengths of our study are as follows: rigorous, systematic methods, including a comprehensive search strategy for relevant studies published in any language (including Chinese), reducing the potential bias of including only reports published in English; inclusion of Hong Kong and Taiwan as well as mainland China, covering >95% of Chinese populations worldwide and including those with highly developed economies; age standardization of data from Chinese and white populations to the same world population; and inclusion of data from older people, who were omitted from many previous Chinese stroke incidence studies.
An important limitation is that, despite comprehensive searching, we found few community-based studies of incidence of stroke and its pathologic types in Chinese populations, and none of ischemic subtypes published up to January 2012. Also, despite including only studies that appeared to fulfill accepted methodologic criteria, we cannot exclude the possibility of inaccurate or incomplete case ascertainment in some included studies. However, rapid developments and improvements in comprehensive primary health care and centralized health insurance should facilitate future, well-designed epidemiologic studies.3,29,30
Thus, we report a slightly higher overall stroke incidence and a higher proportion of ICH in Chinese compared with white populations since 1990, with substantial regional variation among Chinese populations. Confirming variation in the distribution of ischemic subtypes will require comparable population-based studies with consistent definitions in Chinese populations. A better understanding of the reasons for the observed differences in epidemiology of stroke and its subtypes should help us to better predict the potential effects of the rapidly growing economy and changing lifestyles, and contribute to efforts to reduce the stroke burden in Chinese populations.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Professor Ming Liu, Professor Ping-Keung Yip, and Dr. Jiann-Shing Jeng for their kind help in providing additional references and relevant information. The authors are grateful to Professor Peter Sandercock, Professor Martin Dennis, Dr. Rustam Al-Shahi Salman, Dr. Will Whiteley, and the anonymous reviewers for their valuable comments on earlier versions of this manuscript.
GLOSSARY
- CI
confidence interval
- ICH
intracerebral hemorrhage
- OCSP
Oxfordshire Community Stroke Project
- SAH
subarachnoid hemorrhage
- TOAST
Trial of Org 10172 in Acute Ischemic Stroke
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
Study concept and design: C.-F. Tsai and C. Sudlow. Literature search and acquisition of data: C.-F. Tsai and B. Thomas. Analysis and interpretation of data: C.-F. Tsai and C. Sudlow. Manuscript drafting: C.-F. Tsai. Critical revision of the manuscript for important intellectual content: C. Sudlow and B. Thomas. Study supervision: C. Sudlow.
STUDY FUNDING
C.-F. Tsai reports receiving a postgraduate scholarship from Cardinal Tien Hospital and a scholarship to study abroad from the Ministry of Education in Taiwan. C. Sudlow is funded by the Scottish Funding Council. The funding sources had no role in study design, literature search, data acquisition, analysis and interpretation of data, or manuscript writing.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modeling. Lancet Neurol 2009;8:345–354 [DOI] [PubMed] [Google Scholar]
- 3.Liu L, Wang D, Wong KSL, Wang Y. Stroke and stroke care in China. Stroke 2011;42:3651–3654 [DOI] [PubMed] [Google Scholar]
- 4.Thorvaldsen P, Asplund K, Kuulasmaa K, Rajakangas AM, Schroll M. Stroke incidence, case fatality, and mortality in the WHO MONICA Project. Stroke 1995;26:361–367 [DOI] [PubMed] [Google Scholar]
- 5.Chau PH, Woo J, Goggins WB, et al. Trends in stroke incidence in Hong Kong differ by stroke subtype. Cerebrovasc Dis 2011;31:138–146 [DOI] [PubMed] [Google Scholar]
- 6.Fuh JL, Wang SJ, Liu HC, Shyu HY. Incidence of stroke on Kinmen, Taiwan. Neuroepidemiology 2000;19:258–264 [DOI] [PubMed] [Google Scholar]
- 7.Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ. Stroke in China: epidemiology, prevention and management strategies. Lancet Neurol 2007;6:456–464 [DOI] [PubMed] [Google Scholar]
- 8.Jeng JS, Su TC. Epidemiological studies of cerebrovascular diseases and carotid atherosclerosis in Taiwan. Acta Neurol Taiwan 2007;16:190–202 [PubMed] [Google Scholar]
- 9.Feigin VL, Lawes CMM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009;8:355–369 [DOI] [PubMed] [Google Scholar]
- 10.Feigin VL, Lawes CMM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol 2003;2:43–53 [DOI] [PubMed] [Google Scholar]
- 11.Sudlow CLM, Warlow CP. Comparing stroke incidence worldwide: what makes studies comparable? Stroke 1996;27:550–558 [DOI] [PubMed] [Google Scholar]
- 12.Feigin VL, Hoorn SV. How to study stroke incidence? Lancet 2004;363:1920–1921 [DOI] [PubMed] [Google Scholar]
- 13.National Institute of Neurological Disorders and Stroke Ad Hoc Committee Classification of cerebrovascular diseases III. Stroke 1990;21:637–676 [DOI] [PubMed] [Google Scholar]
- 14.Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 1976;54:541–553 [PMC free article] [PubMed] [Google Scholar]
- 15.Rosamod WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) Cohort. Stroke 1999;30:736–743 [DOI] [PubMed] [Google Scholar]
- 16.Sudlow CL, Warlow CP. Comparable studies of incidence of stroke and its pathological types: results from an international collaboration. Stroke 1997;28:491–499 [DOI] [PubMed] [Google Scholar]
- 17.Adams HP, Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST Trial of Org 10172 in Acute Ischemic Stroke. Stroke 1993;24:35–41 [DOI] [PubMed] [Google Scholar]
- 18.Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 1991;337:1521–1526 [DOI] [PubMed] [Google Scholar]
- 19.Ahmad O, Boschi-Pinto C, Lopez A, Murray C, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Standard. GPE discussion paper series: no. 31 Geneva: World Health Organization; 2000 [Google Scholar]
- 20.Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Stat Med 1997;16:791–801 [DOI] [PubMed] [Google Scholar]
- 21.Wu Z, Yao C, Zhao D, et al. Sino-MONICA Project: a collaborative study on trends and determinants in cardiovascular diseases in China. Part I: morbidity and mortality monitoring. Circulation 2001;103:462–468 [DOI] [PubMed] [Google Scholar]
- 22.Wei JW, Arima H, Huang Y, et al. Variation in the frequency of intracerebral haemorrhage and ischemic stroke in China: a national, multicentre, hospital register study. Cerebrovasc Dis 2010;29:321–327 [DOI] [PubMed] [Google Scholar]
- 23.Yang QD, Niu Q, Zhou YH, et al. Incidence of cerebral haemorrhage in the Changsha community. Cerebrovasc Dis 2004;17:303–313 [DOI] [PubMed] [Google Scholar]
- 24.Fang J, Foo SH, Jeng JS, Yip PK, Alderman MH. Clinical characteristics of stroke among Chinese in New York City. Ethn Dis 2004;14:378–383 [PubMed] [Google Scholar]
- 25.Feigin V, Carter K, Hackett M, et al. Ethnic disparities in incidence of stroke subtypes: Auckland Regional Community Stroke Study, 2002–2003. Lancet Neurol 2006;5:130–139 [DOI] [PubMed] [Google Scholar]
- 26.Khan FA, Zia E, Janzon L, Engstrom G. Incidence of stroke and stroke subtypes in Malmo, Sweden, 1990–2000: marked differences between groups defined by birth country. Stroke 2004;35:2054–2058 [DOI] [PubMed] [Google Scholar]
- 27.Asch CJJV, Luites MJA, Rinkel GJE, Tweel IVD, Algra A, Klijn CJM. Incidence, case fatality, and functional outcome of intracranial haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 2010;9:167–176 [DOI] [PubMed] [Google Scholar]
- 28.Zhao D, Liu J, Wang W, et al. Epidemiological transition of stroke in China: twenty-one-year observational study from the Sino-MONONICA-Beijing Project. Stroke 2008;39:1668–1674 [DOI] [PubMed] [Google Scholar]
- 29.Heeley E, Anderson CS, Huang Y, et al. Role of health insurance in averting economic hardship in families after acute stroke in China. Stroke 2009;40:2149–2156 [DOI] [PubMed] [Google Scholar]
- 30.Wang LD, Kong LZ, Wu F, Bai YM, Burton R. Preventing chronic diseases in China. Lancet 2005;366:1821–1824 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.