Abstract
Purpose
To study the pattern of ocular adnexal lymphoproliferative disorders (OALD) in an ophthalmic referral center in Saudi Arabia and to review their, histopathological characteristics with clinical correlation.
Methods
Retrospective chart review of 40 cases of patients who underwent incisional biopsy with the suspected diagnosis of periocular and/or adnexal lymphoid lesions over the period: 2000–2012 at the King Khaled Eye Specialist Hospital (KKESH), Riyadh, Saudi Arabia. The routine histopathologic slides are reviewed by a single pathologist to identify cases of Benign Reactive Lymphoid Hyperplasia (RLH), Atypical Lymphoid Hyperplasia and probable lymphoma. The identification of the specific types of lymphoma is performed at a tertiary general hospital: King Faisal Specialist Hospital and Research Centre (KFSH&RC).
Results
Forty patients are included with an age range of 11–91 years and a median of 36 years. The males constitute 70% and females 30% of the cases. The right eye and/or orbit are involved in 48%. The left eye is involved in 45% while a bilateral disease is found in 7.5%. The median duration of symptoms is 5 months. The site distribution is conjunctiva (42.5%), orbit (25%), lacrimal gland (12.5%), eyelid (10%), lacrimal sac (7.5%) and caruncle (2.5%). One case is excluded after histopathologic diagnosis of malignant melanoma. Diagnosis in the remaining 39 cases includes: RLH in 14 cases (35%), atypical lymphoid hyperplasia in three cases (9%), and lymphoma in 22 cases (56%). Classification of the lymphoma group is: extranodal marginal zone lymphoma (EMZL) in 9/22 cases (41%), diffuse large B cell lymphoma (DLBCL) in 4/22 cases (18%), Castelman’s disease in 3/22 cases (14%), Burkitt’s lymphoma in 2/22 cases (9%), follicular lymphoma and T cell-rich B cell lymphoma: one case each (4.5%).Two cases remain unclassified.
Conclusion
We have a wide age range which is comparable to other studies. Our results show male predominance and the commonest site of involvement is conjunctival, however if RLH cases are excluded, the commonest site for lymphoma is orbit/lacrimal gland in 45% followed by conjunctival in 23%. The commonest type of lymphoma is: EMZL in 41% followed by DLBCL in 18% then other types of lymphoma including follicular lymphoma.
Keywords: Lymphoma, Orbit, Adnexal, Lymphoid hyperplasia, Lacrimal
Introduction
Lymphoproliferative disease of the ocular adnexa (conjunctiva, eyelids and orbit) is relatively uncommon. Ocular lymphoma constitutes less than 1% of all non-Hodgkin lymphomas (NHLs) and 5–15% of all extranodal cases. Most of these are primary tumors and are usually NHLs of B-cell type. It has been recognized that most ocular adnexal lymphomas are low grade, extranodal, marginal zone (EMZL) B-cell lymphomas of the mucosa-associated lymphoid tissue (MALT) type.1
Lymphoproliferative lesions of the ocular adnexa may present with symptoms of conjunctival salmon patches, ptosis from eyelid involvement or the insidious and painless development of proptosis and/or diplopia due to an orbital mass. Clinical and radiological features do not allow distinction of benign hyperplasias from malignant lymphoma, and tissue is ultimately required for histological diagnosis.1,2
Methods
Retrospective review of the medical records of 40 cases of patients who underwent incisional biopsy with the suspected diagnosis of periocular and/or adnexal lymphoid tumors over the period of 2000–2012 at KKESH is performed. Special data collection sheet is designed to include demographic data, clinical information (including site of disease/relevant medical history/ocular symptoms) and histopathological diagnosis.
The routine histopathologic slides are reviewed by a single pathologist at our institution; however the completion of the panel of all immunohistochemical (IHC) stainings designed for suspected lymphoma cases and the final histopathologic diagnosis are performed at KFSH&RC where such patients have been usually referred for staging and further management.
This work has been performed with the approval of the Research Council and Human Ethics Committee at the institution.
Results
A total number of 40 patients are included with an age range of 11–91 years and a median of 36 years. The males constitute 70% and females 30% of the cases. The right eye and/or orbit is involved in 48%. The left eye is involved in 45% while a bilateral disease is found in 7.5% of the cases.
The clinical presentation is summarized in Table 1. The median duration of symptoms is 5 months. One case only has evidence of systemic lymphoma.
Table 1.
The main presenting symptoms of 40 cases.
| Symptom | Frequency % |
|---|---|
| Dryness | 2.5 |
| Globe displacement | 5 |
| Reduced vision | 10 |
| Ptosis ⩾ 2 mm | 12.5 |
| Eyelid swelling and/or edema | 17.5 |
| Proptosis | 20 |
| Conjunctival mass | 42.5 |
The site distribution was conjunctiva (42.5%), orbit (25%), lacrimal gland (12.5%), eyelid (10%), lacrimal sac (7.5%) and caruncle (2.5%).
Following histopathologic identification of the 40 cases, one case is excluded because of the final tissue diagnosis of malignant melanoma. The distribution of the remaining 39 cases according to the tissue diagnosis is: RLH in 14 cases (35%), atypical lymphoid hyperplasia in three cases (9%), and lymphoma in 22 cases (56%).
The classification of cases in the lymphoma group is summarized in Table 2. The commonest being EMZL (Fig. 1a and b) in 9/22 cases (41%), Diffuse Large B cell lymphoma (DLBCL) in 4/22 cases (18%) with a clinical example shown in (Fig. 2a–c), Castleman’s disease (Fig. 3) in 3/22 cases (14%), Burkitt’s lymphoma (Fig. 4) in 2/22 cases (9%), follicular lymphoma (Fig. 5a and b) and T cell-rich B cell lymphoma: one case each (4.5%). Two cases remain unclassified.
Table 2.
Final diagnosis of the 22 confirmed lymphoma cases.
| Lymphoma type | No. | % |
|---|---|---|
| Extranodal marginal zone | 9 | 41 |
| DLBCL | 4 | 18 |
| Castelman’s | 3 | 14 |
| Burkitt’s | 2 | 9 |
| Unclassified | 2 | 9 |
| Follicular | 1 | 4.5 |
| T cell-rich B cell | 1 | 4.5 |
Figure 1.

(A) and (B): The low power appearance of the EMZL Lymphoma (Hematoxylin & eosin original magnification x50) with higher magnification showing diffuse sheets of mature lymphocytes in 1B (Hematoxylin & eosin original magnification x100).
Figure 2.
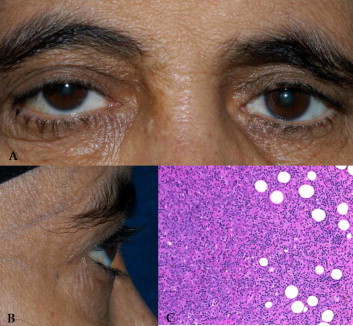
(A) and (B): The clinical appearance of right orbital swelling in a patient with DLBCL. The histopathologic appearance of the large lymphocytes infiltrating the orbital fat is shown in (2C) (Hematoxylin & eosin original magnification x100).
Figure 3.

The histologic appearance of the lymphoid cells in Castleman’s disease affecting a lacrimal gland (Hematoxylin & eosin original magnification x200).
Figure 4.

The classic “starry sky “ histologic appearance in a case of Burkitt’s lymphoma affecting an 11 year old girl (Hematoxylin & eosin original magnification x200).
Figure 5.
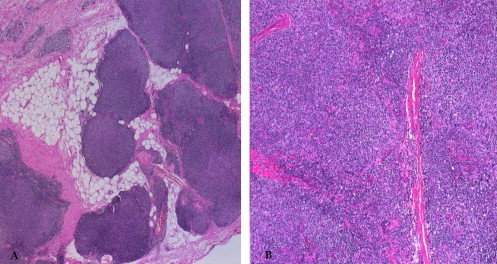
(A) and (B): The low power appearance of a follicular Lymphoma (Hematoxylin & eosin original magnification x25) with higher magnification showing proliferating lymphocytes in (5B) (Hematoxylin & eosin original magnification x100).
Discussion
Ocular adnexal lymphoma (OAL) is considered primary if it involves the ocular adnexa alone and secondary if it is accompanied by a lymphoma of identical type at another site. The extent of OAL is defined as solitary if it involves one or both orbits, extension if it involves contiguous sites such as the sinuses, and systemic if remote sites are involved.1–3
Previous studies have demonstrated that with sufficiently long follow up, between one-third and one-half of the patients with OALD develop systemic lymphoma. In our case series, one patient only has shown evidence of systemic lymphoma. .It has been recognized that the majority of the primary ocular adnexal lymphomas are low-grade tumors, with features of extranodal marginal zone lymphoma (EMZL). These tumors are generally localized at presentation.1–4,7
The frequency of the involvement of periocular sites has been reported as follows: conjunctiva, 20–33%; orbit, 46–74%; and eyelid, 5–20%. These numbers are somewhat variable and may not reflect as clear a distinction as implied, because separation between these immediately proximate structures can be difficult to make, and few studies describe combinations of sites of involvement. Estimates of multisite involvement range from 10% to 20%. Bilaterality is reported in 10–20% of cases.1,2,7 In our cases -with exclusion of RLH-, the commonest site for lymphoma is orbit/lacrimal gland in 45% followed by conjunctival in 23%. Bilaterality was similarly found in 7.5%.
Classification schemes of lymphomas have evolved with time from those based on morphology alone such as the working formulation to the most recent proposed World Health Organization Classification and its precursor, Revised European American Lymphoma Classification (REAL), which incorporate clinical features and ancillary laboratory investigations such as immunophenotyping and genotyping in addition to the histopathological findings. Recent reports of ocular adnexal lymphomas demonstrated that this classification scheme was useful in prediction of the stage of disease at diagnosis, persistence of disease at the final follow up and lymphoma-related death.7
Clinical and imaging data cannot be used to make the diagnosis of OAL with certainty. Diagnosis is made based on a combination of histopathologic, immunophenotypic, and molecular genetic information. Diagnostically, three questions are asked: (1) Is the lesion malignant (OAL), transitional (atypical RLH), or benign (RLH)? (2) What specific type of OAL is present? (3) Can specific prognostic features be identified?1,3,7
Routine histologic analysis can often answer the question of the degree of malignancy. Nevertheless, because the WHO classification is dependent on immunophenotyping and molecular genetic data, lymphoproliferative lesions should undergo immunophenotypic analysis (IPA) for B-cell and T-cell markers, heavy and light chain restriction, CD5, CD10, CD23, cyclin D1, and bcl-2. When possible based on the amount of available tissue, flow cytometry should be performed because of its quantitative nature.1–3,7
Immunohistochemical (IHC) analysis can answer several general questions. The histologically similar mantle cell and marginal cell tumors can usually be distinguished owing to the differential expression of CD5.1–7 Molecular genetic analysis for gene rearrangements of the IgG heavy chain can identify clonality at a much more sensitive level but can provide false positive data (especially in PCR-amplified studies) based on sampling problems.1–3
In our case series, the final classification of our 22 suspected lymphoma specimens were dealt with by professional pathologist in the field using the necessary IHC characteristics and gene rearrangement at KFSH&RC. The commonest type of lymphoma is: EMZL in 41% followed by DLBCL in 18% then other types of lymphoma including follicular lymphoma.
Ocular adnexal lymphomas are mainly B-cell tumors developing in older adults, predominantly among women. In our study we had a wide range of ages at presentation with male predominance in 70%.
Most of patients with ocular adnexal MALT lymphoma have primary orbital disease. White et al. in a review of 42 cases, had one case only out of 16 MALT lymphoma as secondary.4 In our study we had a single known case of lymphoma with secondary orbital involvement.
With regard to the site, some authors suggest dominance of RLH in the conjunctiva compared to the orbit, while others state the opposite.5,6 Coupland et al. diagnosed RLH in 10% of all patients with ocular adnexal lymphoid proliferation, which represents 16% of orbital cases but 10% of the conjunctival lesions.2 In our study we had RLH in 36% of all cases, which constituted 12/17 of our conjunctival lesions in particular (71%). The distribution of site was a higher proportion of conjunctival lesions in 42.5%, possibly because of easy accessibility, Orbit and/or lacrimal gland in 37.5%, Eyelid involvement was in 10%, Lacrimal sac in 7.5% and the least common was in the caruncle 2.5%.
It has been suggested that there are no characteristic symptoms for orbital malignant lymphoma.8 In White et al. review, the commonest presenting symptoms were mass in 48% or swelling in 45%, followed by diplopia, ptosis then proptosis.4 Our commonest presenting symptom was also a mass or swelling in 42.5% and 17.5% of the cases, followed by proptosis, ptosis and vision disturbance.
Management of OAL is optimally an integrated multidisciplinary endeavor requiring a comprehensive staging evaluation. A thorough physical examination by a physician familiar with lymphoma is optimal. The use of ancillary staging studies has evolved with the development of new imaging modalities. Imaging and fine-needle biopsy have replaced laparotomy, although some question the ability of fine-needle aspiration biopsy to obtain diagnostically representative specimens.1,3,7
The selection of treatment for OAL is dependent on the specific tumor type and its staging. Controversy exists as to whether OAL is curable. Those who believe so pursue more aggressive but potentially toxic therapies, whereas those who believe it is not curable may treat indolent disease only as it becomes symptomatic or transforms to high-grade lymphoma. Other clinicians will treat the patient based on an attempt to prevent transformation to a high-grade lymphoma. In some cases, observation without intervention is selected.1–7
The patients in our series are all managed at other general health care facilities and the discussion of their treatment outcome is beyond the scope of this paper.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Coupland S.E., Krause L., Delecluse H.J. Lymphoproliferative lesions of the ocular adnexa: analysis of 112 cases. Ophthalmology. 1998;105(8):1430–1441. doi: 10.1016/S0161-6420(98)98024-1. [DOI] [PubMed] [Google Scholar]
- 2.Knowles D.M., Jakobiec F.A., McNally L., Burke J.S. Lymphoid hyperplasia and malignant lymphoma occurring in the ocular adnexa (orbit, conjunctiva and eyelids): a prospective multiparametric analysis of 108 cases during 1977–1987. Hum Pathol. 1990;21:959–973. doi: 10.1016/0046-8177(90)90181-4. [DOI] [PubMed] [Google Scholar]
- 3.McKelvie P.A., McNab A., Francis I.C. Ocular adnexal lymphoproliferative disease: a series of 73 cases. Clin Exp Ophthalmol. 2001;29(6):387–393. doi: 10.1046/j.1442-9071.2001.d01-18.x. [DOI] [PubMed] [Google Scholar]
- 4.White W.L., Ferry J.A., Harris N.L., Grove A.S., Jr. Ocular adnexal lymphoma. A clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology. 1995;102:1994–2006. doi: 10.1016/s0161-6420(95)30764-6. [DOI] [PubMed] [Google Scholar]
- 5.Knowles D.M., Jakobiec F.A. Ocular adnexal lymphoid neoplasms: clinical, histopathologic, electron microscopic and immunologic characteristics. Hum Pathol. 1982;13:148–162. doi: 10.1016/s0046-8177(82)80118-4. [DOI] [PubMed] [Google Scholar]
- 6.Medeiros L.J., Harris N.L. Lymphoid infiltrates of the orbit and conjunctiva. A morphologic and immunophenotypic study of 99 cases. Am J Surg Pathol. 1989;13:459–471. doi: 10.1097/00000478-198906000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Shields C.L., Shields J.A., Carvahlo C. Conjunctival lymphoid tumors: clinical analysis of 117 cases and relationship to systemic lymphoma. Ophthalmology. 2001;108:979–984. doi: 10.1016/s0161-6420(01)00547-4. [DOI] [PubMed] [Google Scholar]
- 8.Takamura H., Terashima K., Yamashita H. Diagnosis and treatment of orbital malignant lymphoma: a 14-year review at Yamagata University. Jpn J Ophthalmol. 2001;45:305–312. doi: 10.1016/s0021-5155(01)00327-6. [DOI] [PubMed] [Google Scholar]



