Abstract
Background
Thyroid disorders are prevalent in Western society, yet many subjects experience limited symptoms at diagnosis, especially in hypothyroidism. We hypothesize that health-related quality of life (HR-QOL) is more severely impaired in subjects with more abnormal thyroid hormone function tests.
Methods
This is a cross-sectional study of Dutch adults participating in the LifeLines Cohort Study between December 2009 and August 2010. In 9491 Western European participants (median age 45 years; 3993 men and 5498 women), without current or former use of thyroid medication, we compared HR-QOL using the RAND 36-Item Health Survey between subjects with normal thyrotropin (TSH) values and subjects with disturbed thyroid hormone status (serum TSH, free thyroxine, and free triiodothyronine). The influence of possible confounders (age, smoking, co-morbidity) on HR-QOL was evaluated as well.
Results
Suppressed TSH values (TSH <0.5 mU/L) were found in 114 (1.2%), while 8334 (88.8%) had TSH within the normal range, 973 participants (10.3%) had TSH between 4 and 10 mU/L, and 70 (0.7%) had TSH >10 mU/L. Men had a higher HR-QOL than women (70–92 vs. 65–89; p<0.001), except for the domain “general health” (72 vs. 72; p=0.692). Men with suppressed or elevated TSH values did not score significantly lower than euthyroid men for any of nine domains of the RAND 36-Item Health Survey. Compared with euthyroid women, women with suppressed TSH scored significantly lower in the domains “physical functioning” (84 vs. 89, p=0.013) and “general health” (67 vs. 72, p=0.036). Women with markedly elevated TSH (>10 mU/L) had a score in all HR-QOL domains that was similar to that of women with normal TSH values. There were no differences in the physical component score and the mental component score between any of the TSH groups. Physical component score and mental component score were mainly determined by smoking status, co-morbidity, and body mass index or waist circumference.
Conclusions
In this population-based study, HR-QOL scores of subjects with suppressed TSH values or markedly elevated TSH values were generally not significantly lower than those of subjects with normal or mildly elevated TSH values.
Introduction
Thyroid disease is a common endocrine disorder; however, only a limited number of studies have described the health-related quality of life (HR-QOL) in thyroid patients (1–3). While subjects found to have primary hypothyroidism may have specific complaints, such as fatigue, feeling cold, constipation, and weight increase, it has been suggested that symptoms are less pronounced or even absent in specific subgroups such as elderly people (3). Moreover, many subjects are found to have hypothyroidism by chance, when thyroid hormone values are measured in the context of nonspecific symptoms, or during screening.
HR-QOL refers to how the well-being of an individual can be influenced by a disease or multiple diseases, and describes the impact of a disease on all relevant dimensions of human life, including mental and social well-being and physical function (2). In recent decades, assessment of the impact of disease on a patient's life has become an increasingly important therapeutic component, especially in patients with chronic disease. Besides, as the goal for thyroid patients becomes longevity in good health, rather than survival of a life-threatening illness, a major focus of treatment will be to optimize HR-QOL (1,2). Both the measurement and improvement of HR-QOL are currently becoming an increasingly important part of patient-centered care (4).
According to the available literature, HR-QOL is reduced in patients with benign thyroid disorders, both in those with thyroid dysfunction and those with normal levels of thyroid hormones (1–3). However, as reviewed by Watt et al. (2), most of these studies are generally small, or use questionnaires that lack thorough validation. A recent review has mentioned that patients with subclinical hypothyroidism may have alterations in clinical features such as quality of life, cognitive function, and memory, although contrasting findings have been reported (5).
HR-QOL can be measured by two types of questionnaires: disease-specific and generic. The first type of questionnaire shows great sensitivity to detect differences among affected patients and to monitor the result of treatment, whereas the generic questionnaire allows for good comparison between patients and the general population.
As far as we know, no data about the effect of thyroid status on the HR-QOL measured in a large general population have yet been published. Here we make use of the LifeLines Cohort Study, a prospective population-based study in The Netherlands, as part of which the thyroid hormone status was measured in a subset of participants between December 2009 and August 2010. We hypothesize that HR-QOL is more severely impaired in subjects with more abnormal thyroid hormone function tests. The aim of this study therefore was to investigate the association between thyroid hormone status and HR-QOL, and to assess whether the HR-QOL perceived by participants with abnormal thyrotropin (TSH) values was different from that of subjects with normal TSH values.
Materials and Methods
Subjects
In this cross-sectional study, we used data from subjects participating in the LifeLines Cohort Study between December 2009 and August 2010. The LifeLines Cohort Study is a multidisciplinary prospective population-based cohort study with a unique three-generation design that examines the health and health-related behaviors of 165,000 participants living in the northeastern region of The Netherlands (6). It employs a broad range of investigative procedures to assess the biomedical, sociodemographic, behavioral, physical, and psychological factors that contribute to the health and disease of the general population, with a focus on multimorbidity. All survey participants were between 18 and 90 years old at the time of enrollment. All participants provided written informed consent before participating in the study. The study protocol was approved by the medical ethics review committee of the University Medical Center Groningen. In the present survey, we excluded subjects who were not of Western European descent, who had current or previous thyroid disorders, who had current or former use of medication for thyroid disorders, or in whom thyroid function tests were not available.
Clinical examination
Subjects were asked to complete a self-administered questionnaire on medical history, current diseases, use of medication, and health behavior at home. Height, waist, and hip circumference were measured to the nearest 0.1 cm. Waist circumference was measured at a level midway between the lower rib margin and iliac crest with the tape all around the body in horizontal position. Body weight was measured without shoes with a 0.1 kg precision. Systolic and diastolic blood pressures were measured every minute for a period of 10 minutes using a DINAMAP Monitor. The size of the cuff was chosen according to the arm circumference. The average of the last three measurements was reported for each of the blood pressure levels.
Questionnaires
The RAND 36-Item Health Survey (RAND-36) (7) is the Dutch version of the SF-36 (8), a questionnaire developed from the Medical Outcome Study General Health Survey Instrument (9,10). It is a generic questionnaire with eight health-status subscales: physical functioning, role limitations because of physical health problems, bodily pain, general health perception, vitality, social functioning, role limitations because of emotional health, and general mental health. Moreover, the general mental component score (MCS) and the physical component score (PCS) can be computed. Before visiting one of the research locations, all participants filled in the same self-administered questionnaire at home. Only 24 participants did not fill in the RAND-36 questionnaire, and were therefore excluded from the analysis. The research assistants were trained to check the completeness of the questionnaire and—if needed—to interview subjects on missing data without forcing answers from them. They also conducted a mental test (Mini-Mental State Examination, MMSE) (11) in all participants aged above 65, and in those participants aged 65 or under for whom there were doubts about the quality of answers or the status of self-administration, for instance, because of a cognitive disorder. Scores on the MMSE range from 0 to 30, and scores of 25 or higher are traditionally considered normal. The answers of the RAND-36 questionnaire were not used if participants had an MMSE score of 24 or less, because in those cases there would be considerable doubt about the quality of answers obtained by a self-administered questionnaire. This was the case in 137 participants, who were also excluded. In total, HR-QOL data from 9491 participants were available, and this group was used for all analyses.
Analyses
Blood samples were collected the morning after an overnight fast, directly into tubes containing heparin, and centrifuged. Measurement of the thyroid hormone status of all participants was performed at the clinical chemistry laboratory of the University Medical Center Groningen. TSH, free thyroxine (FT4), and free triiodothyronine (FT3) were assayed by electrochemiluminescent immunoassay on the Roche Modular E170 Analyzer using kits provided by the manufacturer (Roche, Basel, Switzerland). Tests to measure anti–thyroid peroxidase (anti-TPO) antibody levels were not performed. Total cholesterol and high-density lipoprotein cholesterol were measured with an enzymatic colorimetric method and triglycerides with a colorimetric UV method, on a Roche Modular P chemistry analyzer. Fasting blood glucose was measured with a hexokinase method. HbA1c was measured with HPLC (Roche).
Data description and statistical analyses
The RAND-36 questionnaire has 36 items that measure health perception across eight domains. Continuous scores for each of these domains were calculated as recommended by the RAND co-operation (12). In this method, the scores for the answer to each item are totaled to generate a score from 0 to 100, with 100 being the best score for HR-QOL (7,10). Since men generally have a higher HR-QOL score than women, data are provided separately for both sexes. The MCS and the PCS were determined from the RAND-36 by taking the individual domains and performing a Z-score transformation, using the mean and standard deviation (SD) derived from the Dutch general population (13). A standardized score with a mean of 50 and an SD of 10 is the average for the Dutch population (13). Diagnosis of earlier myocardial infarction or hypertension was self-reported. Diagnosis of diabetes mellitus was based on self-report, or the finding of an elevated fasting blood glucose >7 mmol/L at examination. The number of different medications used was considered as a proxy for multimorbidity (14). Participants were subdivided according to smoking status as never smoker, former smoker, or current smoker. Study participants were divided into subgroups according to serum TSH values (1st: suppressed, TSH<0.50 mU/L; 2nd: euthyroid, TSH=0.50–4.0 mU/L; 3rd: mildly elevated, TSH=4.01–10.0 mU/L; 4th: markedly elevated, TSH >10.0 mIU/L). The group with TSH between 0.5 and 4.0 mU/L was used as the reference group. Normal values for FT4 are 11–20 pmol/L. The general Dutch population is iodine sufficient.
All analyses were conducted using PASW Statistics (Version 20, IBM, Armonk, NY). Data are presented as mean±SD, or median and interquartile range when not normally distributed. Means were compared between TSH groups with analysis of variance. When variables were not normally distributed, medians were compared with a nonparametric Kruskal–Wallis test. Chi-square test was used to analyze categorical variables. Since men have a higher HR-QOL than women (15–18), group comparisons were corrected for sex. A backward linear regression analysis was performed to assess whether thyroid hormone status, baseline disease state, use of medication, smoking status, and laboratory variables were independently associated with MCS and PCS as an integrated score for HR-QOL. To adjust for multiple comparisons, a p-value <0.01 was considered statistically significant.
Results
Demographic data
The clinical and laboratory parameters of our population are depicted in Table 1. We divided the whole cohort into four groups according to TSH: 114 subjects (1.2%) had serum TSH values below the normal range; 8334 had TSH within the normal range; 973 subjects (10.3%) had mildly elevated TSH values (4.0–10.0 mU/L); and 70 subjects (0.7%) had markedly elevated TSH values (>10 mU/L). Of the subjects with suppressed TSH, 19 (16%) had elevated FT4 values above 20 pmol/L (range 20.1–47.0 pmol/L). Of all subjects with TSH >10 mU/L, 30 (43%) had FT4 values below 11 pmol/L, the lower limit of normal for our assay. There was a significantly higher number of women in the groups with TSH 4–10 mU/L (68%) and >10 mU/L (75%) than in the group with normal TSH values (57%, p<0.01).
Table 1.
Clinical and Laboratory Parameters of the Participants
| TSH<0.5 mU/L (N=114) | TSH 0.5–4.0 mU/L (N=8334) | TSH 4.0–10.0 mU/L (N=973) | TSH>10.0 mU/L (N=70) | |
|---|---|---|---|---|
| Males:females | 49:65 | 3615:4719 | 311:662* | 18:52* |
| Age (years) | 49±13** | 44±13 | 45±15 | 48±11 |
| BMI (kg/m2) | 27.2±4.4* | 26.1±4.2 | 26.2±4.6 | 25.8±3.7 |
| WHR | 0.93±0.08* | 0.91±0.08 | 0.90±0.08** | 0.90±0.07 |
| Systolic BP (mm Hg) | 132±17** | 127±15 | 127±16 | 128±16 |
| Diastolic BP (mm Hg) | 77±11* | 74±9 | 74±9 | 75±10 |
| Heart rate (b/min) | 73±12 | 72±11 | 72±11 | 72±11 |
| TSH (mU/L) | 0.34 (0.001–0.49) | 2.02 (0.50–4.0) | 4.89 (4.01–10.0) | 13.8 (10.1–170) |
| FT4 (pmol/L) | 17.6±5.6** | 15.8±2.0 | 15.0±2.1** | 11.4±2.7** |
| FT3 (pmol/L) | 6.2±2.2** | 5.2±0.7 | 5.1±0.7** | 4.7±0.8** |
| Glucose (mmol/L) | 5.3±0.8* | 5.0±0.8 | 5.0±0.8 | 5.0±0.6 |
| HbA1c (%) | 5.6±0.4* | 5.5±0.4 | 5.5±0.4 | 5.6±0.4 |
| Total cholesterol (mmol/L) | 4.9±0.9 | 5.0±1.0 | 5.1±1.1* | 5.5±1.0*** |
| HDL cholesterol (mmol/L) | ||||
| Males | 1.31±0.32 | 1.25±0.30 | 1.25±0.31 | 1.34±0.27 |
| Females | 1.49±0.37 | 1.55±0.37 | 1.56±0.39 | 1.60±0.39 |
| LDL cholesterol (mmol/L) | 3.1±0.8 | 3.2±0.9 | 3.2±0.9 | 3.6±1.0** |
| Triglycerides (mmol/L) | 1.20±0.65 | 1.20±0.80 | 1.29±0.91** | 1.18±0.63 |
| Use of BP-lowering drugs (%) | 19.3 | 11.3 | 11.8 | 7.1 |
| Use of statins (%) | 10.5 | 5.3 | 4.7 | 5.7 |
TSH groups were defined as: 1st, <0.50 mU/L; 2nd, ≥0.50 and ≤4.0 mU/L; 3rd, >4.0 and ≤10.0 mU/L; 4th, >10.0 mU/L.
Data represent mean±standard deviation and were evaluated by analysis of variance (p-values vs. group with TSH 0.5–4.0 mU/L: *p<0.01, **p<0.001) or χ2-test (*p<0.01).
BMI, body mass index; WHR, waist–hip ratio; BP, blood pressure; FT3, free triiodothyronine; FT4, free thyroxine; HbA1c, hemoglobin A1c; TSH, thyrotropin; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Compared with subjects with normal TSH values, participants with suppressed TSH were older (Fig. 1), had a higher body mass index (BMI) and waist–hip ratio, as well as higher systolic and diastolic blood pressure, despite the fact that a higher percentage of them used blood pressure–lowering medication. Also, their values of fasting blood glucose and HbA1c were slightly, but significantly, higher. Overall, subjects with mildly elevated TSH levels had slightly higher total cholesterol, but similar low-density lipoprotein (LDL) cholesterol levels as subjects with normal TSH. When we analyzed men and women separately, men with mildly elevated TSH had similar total and LDL cholesterol levels. However, women with mildly elevated TSH had higher total cholesterol (5.1±1.1 vs. 4.9±1.1 mmol/L, p=0.001) and LDL cholesterol (3.1±0.9 vs. 3.0±0.9 mmol/L, p=0.011) than women with normal TSH, but the absolute differences were small. Compared with subjects with normal TSH, both men and women with markedly elevated TSH >10 mU/L had considerably elevated values of total and LDL cholesterol. Their age did not differ significantly from those with normal TSH (Table 1).
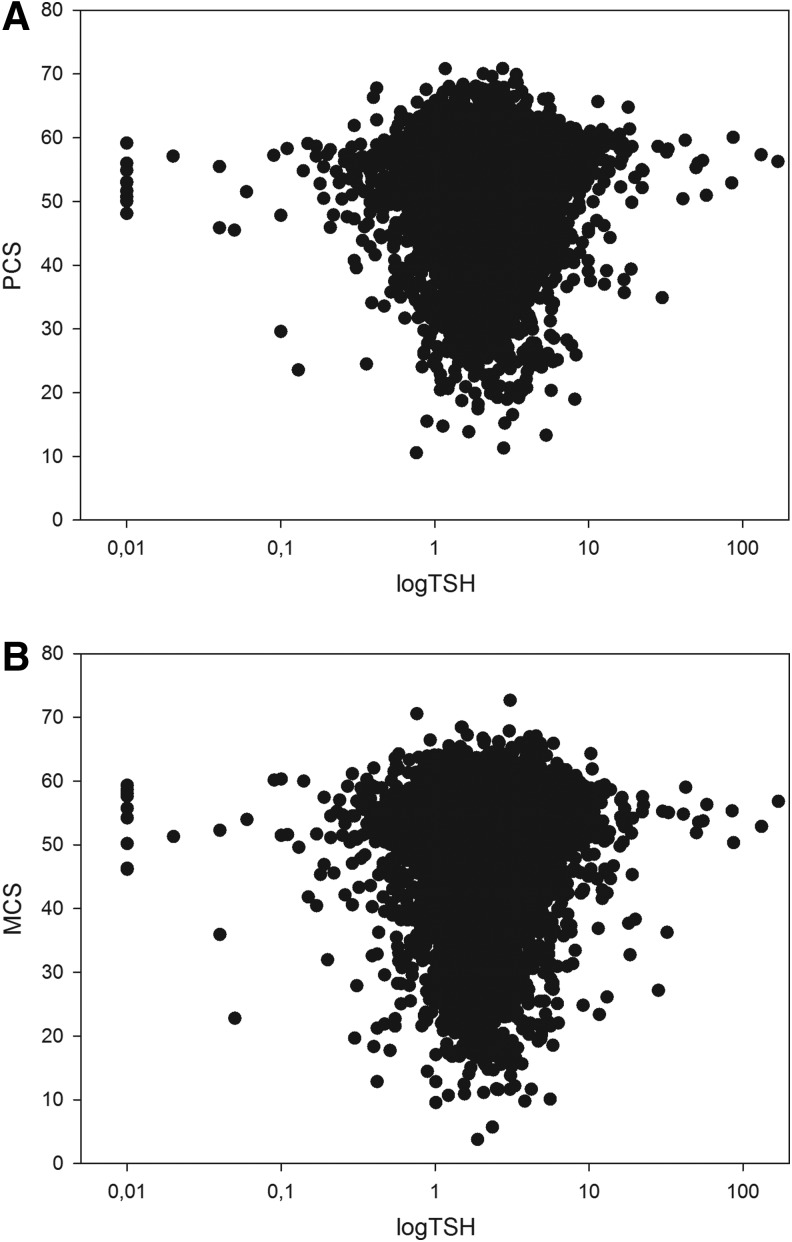
FIG. 1.
Graphical representation of the relationship between log TSH and the PCS (A) and MCS (B), as derived from the RAND-36 questionnaire. TSH, thyrotropin; PCS, physical component score; MCS, mental component score; RAND 36, RAND 36-Item Health Survey.
Health-related quality of life
All HR-QOL scores of men and women are shown in Table 2 and Figures 1 and 2. In men, we observed no significant difference between the four TSH groups with regard to the various HR-QOL domains. Women with suppressed TSH values had similar HR-QOL scores compared with those of women with normal TSH, but had significantly lower median scores for the domains “general health” (70 vs. 75, p=0.036) and “physical functioning” (90 vs. 95, p=0.013). For all domains, the HR-QOL scores of women with mildly or markedly elevated TSH values were similar to those of women with normal TSH values (all comparisons p>0.05). There were no differences in the PCS and the MCS between any of the TSH groups. In the subjects with TSH >10 mU/L, PCS and MCS were similar between subjects with normal and with reduced FT4 levels. In the subjects with TSH <0.5 mU/L, PCS and MCS were similar in subjects with normal versus subjects with elevated FT4.
Table 2.
Health-Related Quality-of-Life Scores of Men and Women
| TSH<0.5 mU/L (N=114) | TSH 0.5–4.0 mU/L (N=8334) | TSH 4.0–10.0 mU/L (N=973) | TSH>10.0 mU/L (N=70) | |
|---|---|---|---|---|
| Males:females | 49:65 | 3615:4719 | 311:662 | 18:52 |
| General health | ||||
| Males | 75 (60–85) | 75 (60–85) | 75 (60–85) | 78 (70–85) |
| Females | 70 (60–80)* | 75 (60–85) | 75 (65–85) | 75 (65–88) |
| Mental health | ||||
| Males | 84 (72–88) | 84 (76–92) | 84 (76–92) | 86 (80–88) |
| Females | 80 (72–84) | 80 (72–88) | 80 (72–88) | 84 (72–92) |
| Physical functioning | ||||
| Males | 95 (85–100) | 95 (90–100) | 95 (90–100) | 95 (95–100) |
| Females | 90 (75–100)* | 95 (85–100) | 95 (85–100) | 95 (88–100) |
| Social functioning | ||||
| Males | 100 (88–100) | 100 (88–100) | 100 (88–100) | 100 (75–100) |
| Females | 88 (62–100) | 88 (75–100) | 100 (75–100) | 94 (75–100) |
| Bodily pain | ||||
| Males | 100 (78–100) | 100 (78–100) | 90 (70–100) | 100 (78–100) |
| Females | 90 (68–100) | 90 (68–100) | 90 (68–100) | 100 (78–100) |
| Vitality | ||||
| Males | 70 (55–75) | 70 (60–85) | 75 (60–85) | 70 (55–85) |
| Females | 65 (50–75) | 65 (55–80) | 65 (55–80) | 70 (60–80) |
| Role limitation—physical | ||||
| Males | 100 (100–100) | 100 (100–100) | 100 (100–100) | 100 (100–100) |
| Females | 100 (75–100) | 100 (100–100) | 100 (100–100) | 100 (100–100) |
| Role limitation—emotional | ||||
| Males | 100 (100–100) | 100 (100–100) | 100 (100–100) | 100 (100–100) |
| Females | 100 (100–100) | 100 (100–100) | 100 (100–100) | 100 (100–100) |
| Health changing | ||||
| Males | 50 (50–50) | 50 (50–50) | 50 (50–50) | 50 (50–50) |
| Females | 50 (50–50) | 50 (50–50) | 50 (50–50) | 50 (50–50) |
| Physical component score | 53±7 | 53±8 | 53±8 | 54±7 |
| Mental component score | 50±10 | 51±9 | 52±8 | 51±8 |
N=9491. Data are expressed as median (interquartile range) or mean±standard deviation. Physical component score and mental component score are corrected for sex.
p-Values vs. euthyroid subjects: *p<0.05.
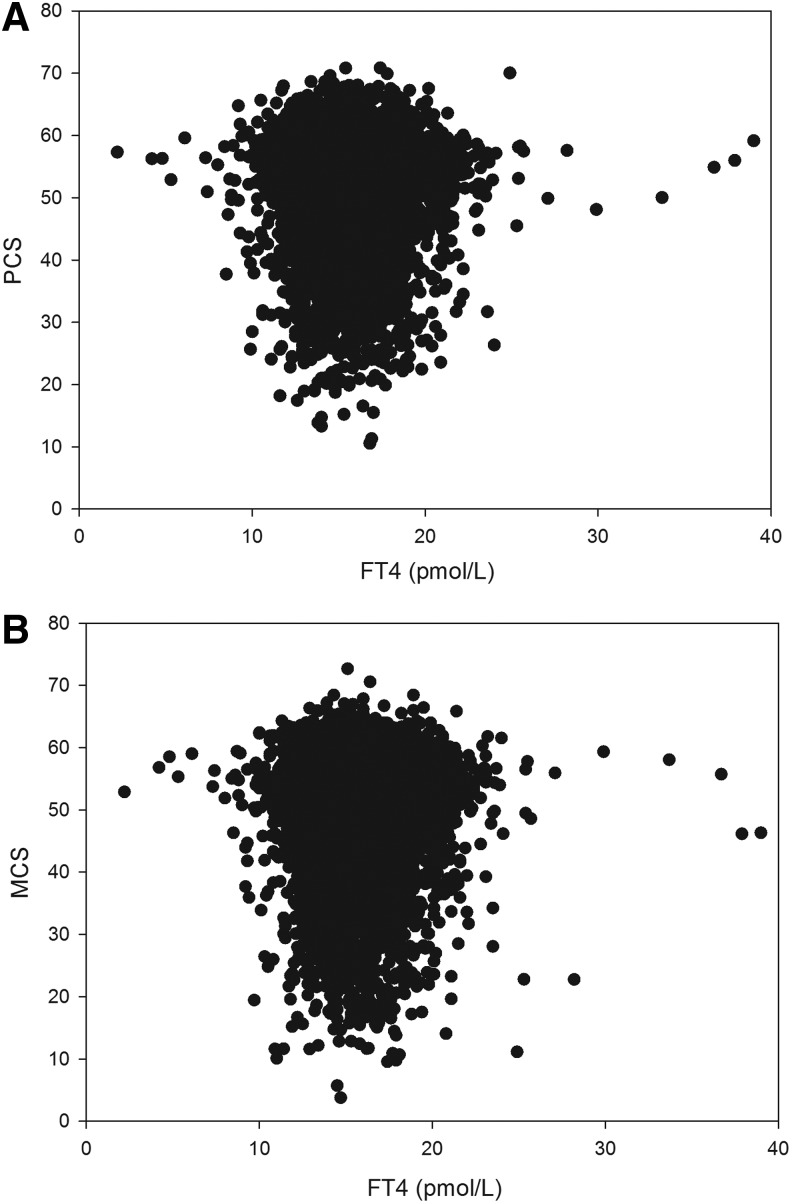
FIG. 2.
Graphical representation of the relationship between free T4 and the PCS (A) and MCS (B), as derived from the RAND-36 questionnaire. T4, thyroxine.
The same overall analyses were performed for serum levels of FT4. Compared with subjects with normal FT4, both men and women with low FT4 (<11.0 pmol/L) had a tendency toward lower scores in the domains “physical functioning” and “social functioning.” This difference was, however, not statistically significant. For the other domains, as well as for MCS and PCS, subjects with low FT4 (<11.0 pmol/L) or elevated FT4 (>20 pmol/L) had similar scores as compared to subjects with normal FT4 values (p>0.05). Figures 1 and 2 show the relationships between log TSH and the PCS and MCS, and between FT4 and the PCS and MCS. When corrected for age, current smoking, and number of medications used, there was no significant correlation between log TSH or FT4 and PCS/MCS in men or women.
In men, the number of medications used, waist circumference, and current smoking were significant negative predictors of PCS (all p<0.001), whereas in women, number of medications use, BMI, age, and current smoking were negative determinants of PCS (all p<0.001). Thyroid hormone status was not a significant predictor of PCS. In men, MCS was independently but negatively associated with current or former smoking, number of medications used, and diagnosis of hypertension, and positively associated with age. In women, MCS was negatively associated with number of medications and current smoking, and positively associated with age. No independent association was found between thyroid hormone status and MCS.
Discussion
In this large population-based survey we assessed the relationship between thyroid hormone status and HR-QOL. We did not observe a significant difference in the HR-QOL in subjects with either increased or decreased TSH or FT4 values compared with subjects with normal thyroid function. The major determinants of the PCS proved to be current smoking, BMI (in women) or waist circumference (in men), and number of medications used. Current smoking and number of medications were also the major predictors for the MCS. We were able to use information on the HR-QOL from a large number of participants, with a wide range in age, socioeconomic status, and co-morbidity. By excluding subjects with a known thyroid disorder, participants were not aware of their thyroid hormone status when they filled in the questionnaires. The outcome of the questionnaire was therefore not influenced by the knowledge of possibly having thyroid disease.
The most remarkable result of our study was that the HR-QOL of subjects with moderately or severely elevated TSH values was not lower than that of subjects with normal TSH. This is supported by the results of a large community-based study by Bell et al. (19) in Western Australia, and it supports experiences in clinical practice that many subjects with hypothyroidism are diagnosed by chance, and not because of specific symptoms (5,20–23). In agreement with our results, Bell et al. (19) reported similar scores on the SF-36 questionnaire in euthyroid subjects and in those with subclinical hypothyroidism. A study in Sweden that included subjects with subclinical thyrotoxicosis also reported no clear relationship between the HR-QOL score and thyroid hormone status, although patients with manifest Graves' disease reported lower HR-QOL (24).
Our findings contradict those of several other studies (1,25–29) in which thyroid function was found to affect the perception of health status. While some studies reported a difference that was independent of the severity of thyroid dysfunction (1,24), others described a decrease in HR-QOL with increasing severity of disease (28,29). However, these studies are limited by the small study population or by the study design, because questionnaires were filled in by patients who were already known to have thyroid dysfunction. The background of the population also determines whether or not differences between patients and controls are significant. For example, in the study by Vigario et al. (29), Brazilian women with subclinical hypothyroidism scored significantly worse than controls for five SF-36 domains. Their control group consisted of ambulatory patients attending an endocrine clinic, and had significantly lower scores for physical and social functioning, mental health, and bodily pain (29) than our normal TSH participants, who, in contrast, all originated from the general population.
The presence of typical thyroid-related symptoms plays a fundamental role in the perceived impairment of HR-QOL (26,28,29). Doctors are aware of the fact that some patients—such as those with Hashimoto thyroiditis—may present with many complaints, although their thyroid hormone status is only marginally disturbed. While a recent study in Greece conversely concluded that children and adolescents with autoimmune thyroiditis were mostly asymptomatic (23), other studies have shown that HR-QOL was decreased and remained decreased in many patients despite normalization of thyroid hormone values (26,30). While already briefly suggested by Ladenson in 2002 (31), the recent literature has also pointed to the association of autoimmunity with physical and mental symptoms and impaired quality of life: the presence of anti-TPO antibodies was a major determinant of quality of life in subjects undergoing surgery for benign thyroid disease (32). Symptoms such as chronic fatigue, dry hair, chronic irritability, nervousness, and lower quality of life were significantly associated with anti-TPO antibody levels that exceeded the cut-off point of 121 U/mL. Unfortunately, data on anti-TPO antibody levels are lacking for our participants.
TSH values are reported to be positively correlated with hypercholesterolemia and dyslipidemia (33,34), although not all studies showed this relationship. In an extensive review, Surks et al. (35) considered the scientific evidence supporting a relationship between subclinical hypothyroidism (TSH 4.5–10 mU/L) and elevations of total and LDL cholesterol as insufficient. Bell et al. (19) observed that women with subclinical hypothyroidism had similar lipid values compared with those in euthyroid women. In our study, women, but not men, with mildly elevated TSH had elevated total and LDL cholesterol levels, although the absolute differences were small. The elevations of total and LDL cholesterol in subjects with TSH >10 mU/L were more pronounced. Surprisingly, we found that the values for the other cardiovascular risk factors (body weight, blood pressure, and glucose) were significantly higher than controls in subjects with suppressed TSH values but not in subjects with increased TSH values. The reason for this is not clear. It could be because subjects with suppressed TSH values were significantly older than subjects with normal TSH. The relatively small number of subjects with suppressed TSH could also be of influence. However, subjects with markedly elevated TSH values were similar in age to the group with suppressed TSH and their number was even smaller (n=70). It is unlikely that differences in the use of medication influenced our results, as the use of blood pressure–lowering agents was also the highest in the participants with suppressed TSH.
Subclinical thyroid disease is a laboratory diagnosis rather than a clinical disease. It is characterized by levels of serum TSH below or above the reference range, and serum FT4 levels within the reference range. Individuals with subclinical thyroid disease generally have few or no clinical signs or symptoms of thyroid dysfunction (22,35,36). It remains controversial whether patients found to have subclinical thyroid disease should receive treatment, as data on the effects of treatment on patient well-being or future cardiovascular risk are conflicting (35,37,38). The data from our study and those of Bell et al. (19), in which the investigated population is unaware of their health status before answering the HR-QOL questionnaire, confirm the hypothesis that a poor HR-QOL could in part be because of the awareness of a disease state, rather than the endocrinological disturbance itself (1). This phenomenon is called the labeling effect (39) and has been observed in other asymptomatic disease states (39,40). Other authors have suggested that being aware of having a thyroid condition may make a person feel less healthy (31). Nevertheless, subclinical thyroid disease has been viewed as a risk factor for developing overt thyroid disease and its complications (41,42), especially in certain risk populations (e.g., women, subjects older than 60 years, and subjects with a history of autoimmune disease or previous thyroid dysfunction) (35).
The effectiveness of preventive screening for thyroid disorders and the positive outcomes of early treatment of subclinical thyroid disease on future co-morbidity remain inconclusive (35,41), and no data at all are available on the effects on HR-QOL. The impaired HR-QOL observed by Bianchi et al. (1) in patients with asymptomatic thyroid disease (euthyroid goiter or Hashimoto thyroiditis) argues for the fact that, while undetectable by physicians, unspecific and vague symptoms are in fact perceived by patients before the later onset of disease. Furthermore, although the SF-36 is a good instrument for the assessment of HR-QOL in the general population and measures general well-being in the community, it is debatable whether early thyroid-specific complaints affecting HR-QOL are measured properly using a generic instrument (2).
Nevertheless, more data are needed to clarify this issue and its relevance for physicians in clinical practice. It would be interesting to assess whether subjects with recently discovered thyroid dysfunction truly did not report thyroid-specific symptoms because, in retrospect, they did not recognize these symptoms as being disease related. In these subjects, a more disease-specific HR-QOL questionnaire could be helpful (2,43). It would also be very informative to follow up these subjects to investigate whether their HR-QOL remains unaffected, or whether it alters after supplementation with T4.
There are some limitations to our study. First, because of the small number of participants with overt thyroid disease, we could not compare the HR-QOL results of participants with overt thyroid disease (elevated TSH and abnormal FT4 values) with those of participants with subclinical thyroid disease (elevated TSH values only). Second, since levels of anti-TPO antibodies were not measured, we have not been able to establish the possible influence of the presence of such antibodies on HR-QOL, especially in the light of results recently published by Ott et al. (32). Third, selection bias may play a role in our study, as subjects already found to have hypothyroidism were not included. As suggested by Ladenson (31), individuals who are more aware of symptoms in general are more inclined to consult their primary care physician because of specific problems (for instance, being obese) and are more likely to be found to have hypothyroidism. Because of their underlying attitude and behavior, these subjects are more likely to have persistent complaints despite supplementation with T4.
In conclusion, we have demonstrated that alterations in thyroid hormone status, especially elevated TSH values, are highly prevalent in the general population. The HR-QOL scores of subjects with suppressed TSH values or markedly elevated TSH values were generally not significantly lower than those of subjects with normal or mildly elevated TSH values. Current smoking, co-morbidity, and BMI were the major predictors of HR-QOL. Prospective follow-up studies are needed to assess the necessity of population-based screening for thyroid disorders and the possible benefits of early intervention by supplementation of T4.
Acknowledgments
The LifeLines Cohort Study is supported by The Netherlands Organization of Scientific Research (NWO; Grant 175.010.2007.006); the Economic Structure Enhancing Fund (FES) of the Dutch government; the Ministry of Economic Affairs; the Ministry of Education, Culture and Science; the Ministry for Health, Welfare and Sports; the Northern Netherlands Collaboration of Provinces (SNN); the Province of Groningen; University Medical Center Groningen; the University of Groningen; the Dutch Kidney Foundation; and the Dutch Diabetes Research Foundation.
We thank Rob Bieringa, Joost Keers, René Oostergo, Rosalie Visser, and Judith Vonk (University of Groningen, University Medical Center Groningen) for data collection and validation. We also thank Sally Hill (Zwolle, The Netherlands) for critical reading and editing of the manuscript. The authors are grateful to the study participants, the staff of the LifeLines Cohort Study and Medical Biobank Northern Netherlands, and the participating general practitioners and pharmacists.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Bianchi GP. Zaccheroni V. Solaroli E. Vescini F. Cerutti R. Zoli M. Marchesini G. Health-related quality of life in patients with thyroid disorders. Qual Life Res. 2004;13:45–54. doi: 10.1023/B:QURE.0000015315.35184.66. [DOI] [PubMed] [Google Scholar]
- 2.Watt T. Groenvold M. Rasmussen AK. Bonnema SJ. Hegedus L. Bjorner JB. Feldt-Rasmussen U. Quality of life in patients with benign thyroid disorders. A review. Eur J Endocrinol. 2006;154:501–510. doi: 10.1530/eje.1.02124. [DOI] [PubMed] [Google Scholar]
- 3.Biondi B. Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008;29:76–131. doi: 10.1210/er.2006-0043. [DOI] [PubMed] [Google Scholar]
- 4.Sloan JA. Cella D. Frost MH. Guyatt G. Osoba D. Quality of life III: translating the science of quality-of-life assessment into clinical practice-an example-driven approach for practicing clinicians and clinical researchers. Clin Ther. 2003;25(Suppl D):D1–D5. doi: 10.1016/s0149-2918(03)80244-8. [DOI] [PubMed] [Google Scholar]
- 5.Cooper DS. Biondi B. Subclinical thyroid disease. Lancet. 2012;379:1142–1154. doi: 10.1016/S0140-6736(11)60276-6. [DOI] [PubMed] [Google Scholar]
- 6.Stolk RP. Rosmalen JG. Postma DS. de Boer RA. Navis G. Slaets JP. Ormel J. Wolffenbuttel BH. Universal risk factors for multifactorial diseases: LifeLines: a three-generation population-based study. Eur J Epidemiol. 2008;23:67–74. doi: 10.1007/s10654-007-9204-4. [DOI] [PubMed] [Google Scholar]
- 7.VanderZee KI. Sanderman R. Heyink JW. de HH. Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med. 1996;3:104–122. doi: 10.1207/s15327558ijbm0302_2. [DOI] [PubMed] [Google Scholar]
- 8.McHorney CA. Ware JE., Jr Lu JF. Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Tarlov AR. Ware JE., Jr Greenfield S. Nelson EC. Perrin E. Zubkoff M. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA. 1989;262:925–930. doi: 10.1001/jama.262.7.925. [DOI] [PubMed] [Google Scholar]
- 10.Ware JE., Jr Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 11.Folstein MF. Folstein SE. McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 12.www.rand.org/content/dam/rand/www/external/health/surveys_tools/mos/mos_core_36item_scoring.pdf. [Jan 5;2013 ]. www.rand.org/content/dam/rand/www/external/health/surveys_tools/mos/mos_core_36item_scoring.pdf.
- 13.Aaronson NK. Muller M. Cohen PD. Essink-Bot ML. Fekkes M. Sanderman R. Sprangers MA. te Velde A. Verrips E. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51:1055–1068. doi: 10.1016/s0895-4356(98)00097-3. [DOI] [PubMed] [Google Scholar]
- 14.Schubert CC. Boustani M. Callahan CM. Perkins AJ. Carney CP. Fox C. Unverzagt F. Hui S. Hendrie HC. Comorbidity profile of dementia patients in primary care: are they sicker? J Am Geriatr Soc. 2006;54:104–109. doi: 10.1111/j.1532-5415.2005.00543.x. [DOI] [PubMed] [Google Scholar]
- 15.Zahran HS. Kobau R. Moriarty DG. Zack MM. Holt J. Donehoo R. Health-related quality of life surveillance—United States, 1993–2002. MMWR Surveill Summ. 2005;54:1–35. [PubMed] [Google Scholar]
- 16.Groessl EJ. Ganiats TG. Sarkin AJ. Sociodemographic differences in quality of life in rheumatoid arthritis. Pharmacoeconomics. 2006;24:109–121. doi: 10.2165/00019053-200624020-00002. [DOI] [PubMed] [Google Scholar]
- 17.Johansson P. Dahlstrom U. Brostrom A. Factors and interventions influencing health-related quality of life in patients with heart failure: a review of the literature. Eur J Cardiovasc Nurs. 2006;5:5–15. doi: 10.1016/j.ejcnurse.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Gallicchio L. Hoffman SC. Helzlsouer KJ. The relationship between gender, social support, and health-related quality of life in a community-based study in Washington County, Maryland. Qual Life Res. 2007;16:777–786. doi: 10.1007/s11136-006-9162-4. [DOI] [PubMed] [Google Scholar]
- 19.Bell RJ. Rivera-Woll L. Davison SL. Topliss DJ. Donath S. Davis SR. Well-being, health-related quality of life and cardiovascular disease risk profile in women with subclinical thyroid disease—a community-based study. Clin Endocrinol (Oxf ) 2007;66:548–556. doi: 10.1111/j.1365-2265.2007.02771.x. [DOI] [PubMed] [Google Scholar]
- 20.Tunbridge WM. Evered DC. Hall R. Appleton D. Brewis M. Clark F. Evans JG. Young E. Bird T. Smith PA. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf ) 1977;7:481–493. doi: 10.1111/j.1365-2265.1977.tb01340.x. [DOI] [PubMed] [Google Scholar]
- 21.Hollowell JG. Staehling NW. Flanders WD. Hannon WH. Gunter EW. Spencer CA. Braverman LE. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III) J Clin Endocrinol Metab. 2002;87:489–499. doi: 10.1210/jcem.87.2.8182. [DOI] [PubMed] [Google Scholar]
- 22.Canaris GJ. Manowitz NR. Mayor G. Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160:526–534. doi: 10.1001/archinte.160.4.526. [DOI] [PubMed] [Google Scholar]
- 23.Skarpa V. Kappaousta E. Tertipi A. Anyfandakis K. Vakaki M. Dolianiti M. Fotinou A. Papathanasiou A. Epidemiological characteristics of children with autoimmune thyroid disease. Hormones (Athens) 2011;10:207–214. doi: 10.14310/horm.2002.1310. [DOI] [PubMed] [Google Scholar]
- 24.Abraham-Nordling M. Wallin G. Lundell G. Torring O. Thyroid hormone state and quality of life at long-term follow-up after randomized treatment of Graves' disease. Eur J Endocrinol. 2007;156:173–179. doi: 10.1530/eje.1.02336. [DOI] [PubMed] [Google Scholar]
- 25.Biondi B. Palmieri EA. Fazio S. Cosco C. Nocera M. Sacca L. Filetti S. Lombardi G. Perticone F. Endogenous subclinical hyperthyroidism affects quality of life and cardiac morphology and function in young and middle-aged patients. J Clin Endocrinol Metab. 2000;85:4701–4705. doi: 10.1210/jcem.85.12.7085. [DOI] [PubMed] [Google Scholar]
- 26.Elberling TV. Rasmussen AK. Feldt-Rasmussen U. Hording M. Perrild H. Waldemar G. Impaired health-related quality of life in Graves' disease. A prospective study. Eur J Endocrinol. 2004;151:549–555. doi: 10.1530/eje.0.1510549. [DOI] [PubMed] [Google Scholar]
- 27.Razvi S. Ingoe LE. McMillan CV. Weaver JU. Health status in patients with sub-clinical hypothyroidism. Eur J Endocrinol. 2005;152:713–717. doi: 10.1530/eje.1.01907. [DOI] [PubMed] [Google Scholar]
- 28.Gulseren S. Gulseren L. Hekimsoy Z. Cetinay P. Ozen C. Tokatlioglu B. Depression, anxiety, health-related quality of life, and disability in patients with overt and subclinical thyroid dysfunction. Arch Med Res. 2006;37:133–139. doi: 10.1016/j.arcmed.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Vigario P. Teixeira P. Reuters V. Almeida C. Maia M. Silva M. Vaisman M. Perceived health status of women with overt and subclinical hypothyroidism. Med Princ Pract. 2009;18:317–322. doi: 10.1159/000215731. [DOI] [PubMed] [Google Scholar]
- 30.Fahrenfort JJ. Wilterdink AM. Van der Veen EA. Long-term residual complaints and psychosocial sequelae after remission of hyperthyroidism. Psychoneuroendocrinology. 2000;25:201–211. doi: 10.1016/s0306-4530(99)00050-5. [DOI] [PubMed] [Google Scholar]
- 31.Ladenson PW. Psychological wellbeing in patients. Clin Endocrinol (Oxf ) 2002;57:575–576. doi: 10.1046/j.1365-2265.2002.01682.x. [DOI] [PubMed] [Google Scholar]
- 32.Ott J. Promberger R. Kober F. Neuhold N. Tea M. Huber JC. Hermann M. Hashimoto's thyroiditis affects symptom load and quality of life unrelated to hypothyroidism: a prospective case-control study in women undergoing thyroidectomy for benign goiter. Thyroid. 2011;21:161–167. doi: 10.1089/thy.2010.0191. [DOI] [PubMed] [Google Scholar]
- 33.Duntas LH. Thyroid disease and lipids. Thyroid. 2002;12:287–293. doi: 10.1089/10507250252949405. [DOI] [PubMed] [Google Scholar]
- 34.Walsh JP. Bremner AP. Bulsara MK. O'Leary P. Leedman PJ. Feddema P. Michelangeli V. Thyroid dysfunction and serum lipids: a community-based study. Clin Endocrinol (Oxf ) 2005;63:670–675. doi: 10.1111/j.1365-2265.2005.02399.x. [DOI] [PubMed] [Google Scholar]
- 35.Surks MI. Ortiz E. Daniels GH. Sawin CT. Col NF. Cobin RH. Franklyn JA. Hershman JM. Burman KD. Denke MA. Gorman C. Cooper RS. Weissman NJ. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. 2004;291:228–238. doi: 10.1001/jama.291.2.228. [DOI] [PubMed] [Google Scholar]
- 36.Vanderpump MP. Tunbridge WM. Epidemiology and prevention of clinical and subclinical hypothyroidism. Thyroid. 2002;12:839–847. doi: 10.1089/105072502761016458. [DOI] [PubMed] [Google Scholar]
- 37.Vanderpump MP. How should we manage patients with mildly increased serum thyrotrophin concentrations? Clin Endocrinol (Oxf ) 2010;72:436–440. doi: 10.1111/j.1365-2265.2009.03720.x. [DOI] [PubMed] [Google Scholar]
- 38.Asvold BO. Bjoro T. Platou C. Vatten LJ. Thyroid function and the risk of coronary heart disease: 12-year follow-up of the HUNT Study in Norway. Clin Endocrinol (Oxf ) 2012;77:911–917. doi: 10.1111/j.1365-2265.2012.04477.x. [DOI] [PubMed] [Google Scholar]
- 39.Rodger AJ. Jolley D. Thompson SC. Lanigan A. Crofts N. The impact of diagnosis of hepatitis C virus on quality of life. Hepatology. 1999;30:1299–1301. doi: 10.1002/hep.510300504. [DOI] [PubMed] [Google Scholar]
- 40.Wenger NK. Quality of life issues in hypertension: consequences of diagnosis and considerations in management. Am Heart J. 1988;116:628–632. doi: 10.1016/0002-8703(88)90561-3. [DOI] [PubMed] [Google Scholar]
- 41.Helfand M. Screening for subclinical thyroid dysfunction in nonpregnant adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:128–141. doi: 10.7326/0003-4819-140-2-200401200-00015. [DOI] [PubMed] [Google Scholar]
- 42.Asvold BO. Vatten LJ. Midthjell K. Bjoro T. Serum TSH within the reference range as a predictor of future hypothyroidism and hyperthyroidism: 11-year follow-up of the HUNT Study in Norway. J Clin Endocrinol Metab. 2012;97:93–99. doi: 10.1210/jc.2011-1724. [DOI] [PubMed] [Google Scholar]
- 43.Watt T. Hegedus L. Groenvold M. Bjorner JB. Rasmussen AK. Bonnema SJ. Feldt-Rasmussen U. Validity and reliability of the novel thyroid-specific quality of life questionnaire, ThyPRO. Eur J Endocrinol. 2010;162:161–167. doi: 10.1530/EJE-09-0521. [DOI] [PubMed] [Google Scholar]