Between 1.5% and 7.5% of school aged children (6-12) experience encopresis, a medical disorder more recently labeled constipation with fecal incontinence (Doleys, 1989; Rasquin et al., 2006). Constipation, with and without fecal incontinence, accounts for 25% of pediatric gastroenterology clinic visits (Levine, 1975; Youssef & Di Lorenzo, 2001) and 3% of general pediatric clinic visits (Loening-Baucke, 1993). Although primary care providers typically self-report high success rates when treating constipation alone, these same providers indicate that encopresis is often difficult to treat, with only 19% of providers surveyed indicating a more than 80% success rate with encopresis (Philichi & Yuwono, 2010). One possible reason for the differential rates of success is the heavy educational and behavioral component that is integral to effective encopresis treatment, adding to the burden already placed on providers in demanding primary care settings.
Despite evidence that both medical and behavioral management of encopresis have been found to be at least partially effective (McGrath, Mellon, & Murphy, 2000), especially when they are combined (Cox, Sutphen, Borowitz, Kovatchev, & Ling, 1998), encopresis remains difficult to treat in most primary care settings. The relatively poor success rate is what prompts many primary care providers to refer their encopretic patients to a pediatric gastroenterologist (Philichi & Yuwono, 2010). One treatment that has been found to be especially effective for fecal incontinence with constipation is Enhanced Toilet Training (ETT) (Cox et al., 1998). ETT incorporates intensive medical management (defined by use of enemas or high dose laxatives for cleanout, followed by sufficient dose of laxatives or stool softeners to ensure regular bowel movements) and combines it with proven behavioral techniques for encopresis. The behavioral components include: 1) education on psychophysiology and mechanisms of bowel movements; 2) description and explanation of paradoxical constriction of the external anal sphincter (EAS) and how this impedes defecation; 3) instructions, modeling, and practicing effective straining (proper defecation dynamics); 4) strategies for reducing parent-child conflicts; 5) treating phobic reactions to the toilet and defecation; and 6) addressing social isolation and other related difficulties (i.e., problems at school).
ETT leads to significantly greater symptom reduction compared to more intense medical management alone (Cox et al., 1998). However, there are barriers to its routine use, particularly a lack of professionals trained in both the medical and behavioral elements of ETT. And, even when clinicians are trained to incorporate the behavioral strategies into their treatment offering, the intervention takes time, thereby adding expense and time as two additional barriers to delivering and receiving ETT. In sum, clinician training, clinician fees, transportation and travel to these specialty clinics, and time away from both work for the parent and school for the child all impede access to comprehensive encopresis care.
To address these treatment barriers, an Internet intervention, called UCanPoopToo, was developed to enable parents and children with encopresis to access the primary components of ETT from anywhere with a computer and Internet access. An early version of UCanPoopToo was evaluated and found to be an effective adjunct (improvement) to standard medical care (Ritterband et al., 2003). In the initial testing, 24 children diagnosed with chronic encopresis were enrolled in a randomized controlled trial. All participants received routine care from their primary care physician (PCP); however, half of the subjects also had a computer placed in their homes (Web group) and half (No-Web group) were not given access to the Internet intervention while continuing to receive care from their PCP. Children who received the Internet version of ETT improved significantly more than those in routine medical care. More specifically, the Web parents reported that their children were having on average 6.0 (SD = 6.3) accidents each week before the intervention and 0.5 (SD = .9) accidents following the 3-week intervention, while the No-Web participants reported having 8.2 (SD = 7.3) accidents at pre-assessment and 8.3 (SD = 13.8) at post-assessment. Success, defined as ≤1 accident/week, differed by group; 80% in the Web group had success, whereas only 55% had success in the No-Web group. The cure rate, defined as the proportion of children who had zero accidents/week at post-assessment, was 70% for the Web group and 45% for the No-Web group.
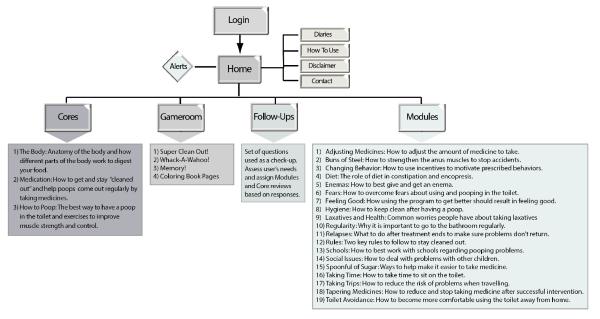
Building on this first trial, the UCanPoopToo program was revised in preparation for a larger trial to include children recruited from across the U.S. in order to determine whether findings generalized as well as to examine the stability of these outcomes over time. The specifics on the updates to the program are reported elsewhere (Magee, Ritterband, Thorndike, Cox, & Borowitz, 2009). In brief, this UCanPoopToo version 2 is structurally similar to the original, but enhanced with additional content, online assessment and online diaries, and a game room that included web-based arcade-style games for the children to play as rewards for completing components of the program (see Figure 1 which includes the child-friendly descriptions of the Cores and Modules as presented to the users). The number of Core content components remained the same (three), but the number of Modules was reduced from 27 to 22 (19 plus 3 Core review Modules), in part because some Modules were combined. An additional weekly Follow-Up was also added, lengthening the intervention by one week for a total of four weeks.
Figure 1.
Schematic of UCanPoopToo version 2 with Core and Module descriptions.
With this version 2 of UCanPoopToo, we hypothesized that, with a larger sample, children with encopresis receiving the Internet intervention in addition to treatment-as-usual would have significantly fewer accidents at post intervention (Weeks 4-6) and one year post compared to those receiving routine care only. Secondary hypotheses were that 1) children and parents receiving the Internet intervention in addition to treatment-as-usual would increase their encopresis-specific knowledge (including information about treatment strategies) and 2) would show greater reductions in bowel-specific problems related to encopresis and constipation (e.g., avoidance of the toilet) more than families who only received routine care. Although these secondary hypotheses were not supported in the previous trial of UCanPoopToo, we believed that with a revised measure of encopresis knowledge and an improved intervention, these hypotheses should be re-evaluated with a larger sample.
PARTICIPANTS AND METHODS
Participants
Participants for this randomized control trial were recruited nationally (U.S.) through clinicians, both MDs (primarily pediatricians) and PhDs/PsyDs (primarily psychologists) treating the patient for encopresis, between 2004 and 2006. Clinicians were solicited through professional organization meetings, mailings, and email. One hundred and seventy-eight clinicians indicated interest by responding to the notices. Clinicians were then contacted and provided with additional study details. Ninety-eight clinicians enrolled in the study by faxing in a signed agreement form indicating their understanding of the study and assumptions made by the Internet intervention. Of the other 80, 29 declined and 51 either did not respond to subsequent contacts or were placed on an “unsure or wait” list. Of the 98 clinicians enrolled, 50 were MDs and 48 were PhD/PsyD.
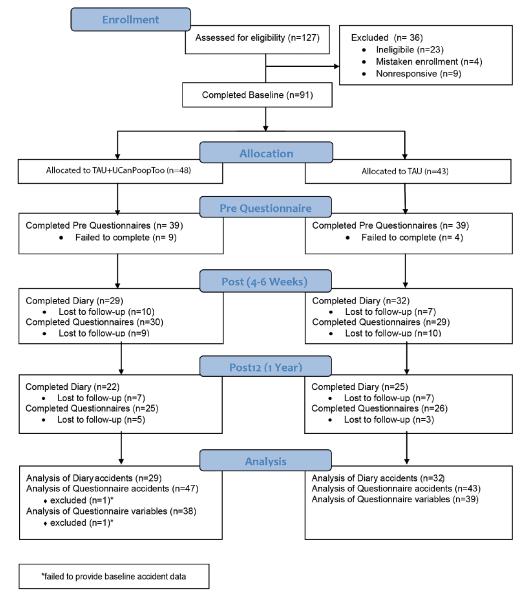
These clinicians referred 127 potential participants (see CONSORT Figure 2). Ninety-one met eligibility, agreed to participate, and completed the telephone screen and telephone assessment (see Measures below); 23 were ineligible because they did not meet inclusion criteria, 4 were mistakenly enrolled but then not included due to age, and 9 were nonresponsive when initial contact was attempted. Inclusion criteria included 6-12 years of age, symptoms of encopresis (fecal soiling) for more than 3 months, had more than one accident in the previous two weeks, had a home computer and Internet access, indicated the ability to complete the Internet intervention over the subsequent 4 weeks, willing to be randomized, and willing to track bowel activity for 14 days at post and one year post assessment. Exclusion criteria included medical conditions that could be the cause (i.e., Short Bowel Syndrome, Hirschsprung’s) or treatment obstacle (i.e., pull through procedure, Cerebral Palsy) of the encopresis, or significant developmental delay (i.e., Pervasive Development Delay, Autism) that might impede treatment success.
Figure 2.
CONSORT
Measures
Parents responded to a series of questions at Pre, Post (Day 42), and one year Post (Day 365) after the intervention period regarding their child’s encopretic symptoms (bowel/accident patterns) and associated problems, caregiver information, computer/Internet usage, previous treatment history, demographics, parental knowledge of encopresis, cost items, and program evaluation. Specifically, the following measures were used in this study:
Encopresis Knowledge Scale-Revised (EKS-R)
A revised version of the EKS was administered to test the parent’s knowledge about encopresis. The EKS-R consists of 25 true/false questions, covering three main areas: anatomy/pathophysiology, laxative/medication use, and behavior treatment techniques. Significant correlations between pre- and post- scores using an earlier version of the knowledge scale demonstrated adequate test-retest reliability (Ritterband et al., 2006).
Virginia Encopresis Constipation Apperception Test (VECAT)
The VECAT was administered to assess bowel-specific problems related to the process of encopresis and constipation, such as avoidance of the toilet, non-responsiveness to rectal distention cues, and fear of defecation pain. In this study, only the bowel-specific items were used, resulting in a range of scores from 9 to 36. For mothers’ responses, the Cronbach alpha for the bowel-specific items is .68, (p<.001) and test-retest reliability after six months, with no treatment, is reliable (r=.60, p<.001)(Cox et al., 2003).
Internet Intervention Utility Questionnaire (IIUQ)
To gather subjects’ experiences using UCanPoopToo, those who received UCanPoopToo were asked about issues of usability, likeability, usefulness, understandability, and convenience. There are 12 items, 10 requiring responses on a five point scale from 0 being “not at all” to 4 being most positive, and 2 additional items asking what the most and least helpful aspects of the Internet program were. A similar 8 item Likert scale was shown to have good internal reliability with an alpha coefficient of .69 (Ritterband et al., 2008).
In addition to these validated measures, several other forms of data were collected, including:
Diary data
We utilized DCSI (Data Collection System on the Internet), a web-based diary data collection tool we developed, to collect fourteen sequential days of diary data at post and one year post assessment. Six questions track symptoms and behaviors (parental prompting and self-prompting for toilet use, fecal accidents, defecation pain, number of BMs in the toilet, and stool consistency). An earlier version of DCSI demonstrated strong reliability and validity as well as convincing sensitivity and specificity (Ritterband et al., 2001).
Website usage data
Usage was tracked via three primary metrics: Completion of Cores, Follow-Ups, and Modules. Intervention users were instructed to complete three Cores during the initial week and then three Follow-Ups, one for each of the subsequent three weeks. Based on feedback from the Follow-Ups, users were encouraged to complete specific Modules identified based on their responses to the Follow-Up.
Cost data
For an exploratory cost analysis, participants were asked at Pre and Post to quantify items and events that incurred costs related to encopresis. Items relevant to the present analysis include number of diapers used, number of school days missed, trips to school by parents, and clean-out procedures. The per unit cost estimates assigned to the quantified items/events were derived from health economic analysis practices recommended by Finkelstein and colleagues (Tate, Finkelstein, Khayjou, & Gustafson, 2009).
Procedure
Enrolled clinicians were sent recruitment packets that included study related information sheets for possible participants, a participant interest and clinician treatment form that the clinician filled out and faxed in when a potential patient was identified and agreed to learn more about the study, informed consent and assent packets, a few small gifts for the participants (magnets, pencils and post-it notes with study contact information on them), and a stamped return envelope for the participants to mail back completed forms. The clinician or designee received a $50 gift certificate for each participant considered for inclusion as compensation for the time taken to discuss the study with the participant and faxing the subject interest form.
Once a participant’s interest form was received, the patient was entered into a data tracking system and called within one business day. A brief phone screening was conducted to ensure the patient met eligibility. If the patient met inclusion criteria and was still interested in participation, the full phone assessment was administered and the individual was randomized to either continued clinical care (treatment-as-usual, TAU) or continued clinical care plus the Internet intervention (TAU+UCanPoopToo). At the conclusion of the phone assessment, the participant was emailed a “welcome” email with instructions on how to access the study website. At the participant’s first login, s/he was directed to the online Assessment Pre questionnaires. Once complete, the participant was notified of his/her group condition, and if in the experimental condition, instructions on how to use UCanPoopToo were provided.
During the first week, TAU+UCanPoopToo participants were instructed to complete the three main Cores of UCanPoopToo. One week following the completion of the intervention Cores, participants completed a “Follow-Up” questionnaire within UCanPoopToo that, based on their answers, assigned additional Modules. This same step of completing a “Follow-Up” questionnaire and assigning subsequent tailored Modules occurred for the next two weeks (for a total of three Follow-Ups). TAU participants were instructed to continue to follow the care of their clinician. Twenty-eight days after completing the Pre Assessment, all participants were instructed to complete two weeks of online diary data (see Measures section). At the end of this two week diary collection, participants were instructed to complete the Post Assessment questionnaires (Day 42). Once the diaries and questionnaires were completed for a given assessment period, participants received a $40 gift certificate. All participants were asked to complete the same 14 days of diaries and questionnaires (Day 365) one year from completing the Pre Assessment (Post12), and received a $60 gift certificate at that time. This study was approved by the institutional review board for human subjects at the University of Virginia Health System.
Statistical Analyses
Descriptive statistics were computed on the baseline characteristics outlined in Table 1. To compare groups at baseline, t-tests and Wilcoxon rank-sum tests were used for normal and skewed data, respectively. Fisher’s Exact Test (FET) was used for comparing groups on dichotomous variables. To evaluate efficacy of the intervention on the reduction of accidents, an outcome variable was created using diary entries completed at Post. Daily diary entries completed over two weeks (range = 8-14 entries) were averaged by participant. An ANCOVA was used to test the difference between groups at Post controlling for number of accidents reported retrospectively by telephone interview at Pre. To test whether groups changed at different rates from Post to Post12, a variable for accidents at Post12 was calculated from diaries as described above (range=12-14 entries), and a 2 × 2 repeated-measures (RM) ANOVA (Group × Time period) was conducted. To supplement analyses on the diary-based accident variables, RM ANOVAs were also conducted on retrospective accident data collected at Pre, Post and Post12. Both diary and retrospective accident variables were positively skewed and were logarithmically transformed in order to meet assumptions of normality. Effect sizes were calculated at each time point as the difference between the estimated marginal means (controlling for values at Pre) standardized using the TAU group standard deviation at Post. Because accident data was transformed, effect sizes were computed from the transformed statistics.
Table 1.
Descriptive Data at Baseline
| TAU+UCanPoopToo (n=47) |
TAU (n=43) |
Significance | |
| Gender | 81% male | 81% male | FET, p = 1.00 |
| Age | 8.47 (1.92) | 8.66 (1.72) | t(1,88) = .51, p = .61 |
| Race1 | 85% White | 95% White | FET, p = .16 |
| High School degree or less (Parent) | 53% | 50%* | FET, p = .83 |
| Age of toilet training (months) | 31.00 (12.17) | 27.05 (17.01) | t(1,75) = 1.26, p = .21 |
| Accident history (months) | 42.55 (30.79) | 47.14 (33.73) | t(1,88) = .67, p = .50 |
| # of accidents per 2 weeks (median(range)) | 8.00 (2-70) | 9.00 (2-70) | z =1.02, p=.31 |
| # previous medical visits (median(range))2 | 3.00 (0-15)* | 3.00 (0-35) | z = .53, p = .60 |
| # previous mental health visits (median(range))2 | 0.00 (0-120) | 1.00 (0-24) | z= 1.28, p = .20 |
| “Very comfortable using Internet” (Parent)3 | 79% | 81% | FET, p = .80 |
| Check email daily (Parent)4 | 68% | 61% | FET, p = .51 |
Note: FET = Fisher’s Exact Test
One case missing.
Race is coded as white vs. all other races.
% visits were related to encopresis
For comfort with the Internet, the percentage show represents those who selected “very comfortable” or “I’m an expert” as compared to those who selected “somewhat comfortable” or “comfortable.”
% who check email daily is compared to % who check email less than daily.
Missing data analysis was conducted to test whether diary outcome data was missing completely at random (MCAR). The last observation carried forward (LOCF) approach to missing data could not be used with Post diary data because diary data was not collected at Pre. Little’s MCAR test was used for continuous variables; continuous variables with a skewed distribution were logarithmically transformed prior to analysis. For dichotomous variables, FET was used to compare groups (missing vs. non-missing Post diary data). Regarding missing Post12 diary data, as well as retrospective accident data, an intent-to-treat approach using LOCF was used. Success and cure rates for accident outcomes were calculated using only those who had non-missing Post diary data.
For analyses of the secondary outcomes of knowledge and bowel specific problems, derived from the EKS-R and VECAT measures respectively, we conducted 2 × 3 RM ANOVA (Group by Assessment period). Because the EKS-R is a proportion, a logit transformation was performed prior to analysis. Again, an intent-to-treat approach using LOCF was used since Pre data was available.
Cost analysis was performed by calculating the difference in Pre-Post changes between the TAU and TAU+UCanPoopToo group for each item. The per unit cost estimate for each item/event was then applied to the difference in changes over time between groups. The cost differences for each item were summed to provide a total weekly difference in savings between groups.
Among TAU+UCanPoopToo participants, usage of the Internet program and satisfaction with the program were evaluated using descriptive statistics. All analyses were conducted with SPSS 19.
RESULTS
Baseline Characteristics
Groups did not differ significantly at baseline (see Table 1). Descriptive statistics show the two groups to be similar in composition by demographics, fecal accident history, number of previous clinician visits related to encopresis, and frequency of Internet/email use. Thirty-seven percent of participants were referred by an MD, while 63% were referred by a PhD/PsyD with no significant difference in referring clinician type between treatment groups (FET, p=.51).
Primary Outcome Results
Fecal accident outcomes with online diary data
Table 2 provides test statistics for group differences at Pre, Post and Post12 for participants who provided outcome data at Post. Group differences at Pre in retrospective accidents were not significant. At Post, the ANCOVA predicting number of online diary fecal accidents showed a significant difference between groups, controlling for retrospective accidents at baseline. At Post12, the ANCOVA revealed a trend between groups, with the TAU+UCanPoopToo group still showing a lower rate of accidents compared to the TAU group. From Post to Post12, the median number of online diary fecal accidents of the TAU+UCanPoopToo group decreased from 3.0 to 1.0, while the TAU group median decreased from 8.0 to 4.5 (see Figure 3). The groups did not differ significantly in their rates of change from Post to Post12, F(1, 59)=0.05, p=.833. However, when three individuals who had provided Post data but never used the online program (i.e., completed 0 Cores) were excluded, a post-hoc ANCOVA indicated significant group differences at both Post (F(1,55)=6.64, p=.013) and Post12 (F(1,55)=4.38, p=.041).
Table 2.
DCSI Accidents per 2 Weeks at Pre, Post, Post12
| Time | TAU+UCanPoopToo Median(range) (n=29) |
TAU Median(range) (n=32) |
F | df | p | ES |
|---|---|---|---|---|---|---|
| Accidents – Pre (retro) | 7.0 (2-70) | 8.5 (2-45) | 0.65 | 1,59 | .423 | |
| Accidents – Post (diary) | 3.0 (0-26.8) | 8.0 (0-38) | 5.28 | 1,58 | .025 | .52 |
| (Accidents – Post 12 ITT (diary) | 1.0 (0-27) | 4.5 (0-45) | 3.03 | 1,58 | .087 | .46 |
Figure 3.
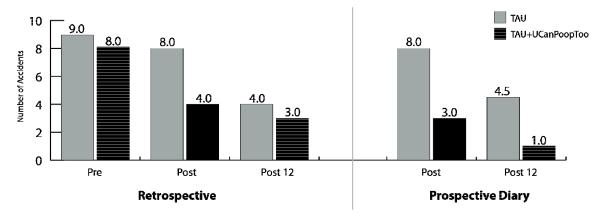
Number of Accidents per Two Weeks
Success and cure rates
Success and cure rates by group are presented in Table 3. Success is defined as having zero or one fecal accidents over the course of two weeks. Cure is defined as having zero accidents over the previous two weeks. At Post (based on diary data), there is a non-significant trend for a greater percentage of TAU+UCanPoopToo children to achieve “success” compared to TAU children. This difference in success rates favoring TAU+UCanPoopToo children becomes significant at the one year assessment. With respect to “cure” rates, there are no group differences at Post (again based on diary data). However, at one year assessment, a greater percentage of TAU+UCanPoopToo children become “cured” compared to TAU children.
Table 3.
Success and Cure rates
| Success (≤1 accident/two weeks) | Cure (0 accidents/two weeks) | |||||
|---|---|---|---|---|---|---|
| TAU+ UCanPoopToo |
TAU | FET | TAU+ UCanPoopToo |
TAU | FET | |
| Post | ||||||
| Prospective (n=61) | 31% | 13% | p=.073 | 14% | 9% | p=.443 |
| Post 12 | ||||||
| Prospective (n=47) | 64% | 28% | p=.015 | 50% | 20% | p=.031 |
Missing data analysis
Baseline variables were examined for patterns relating to missing post-diary data. Child’s age, months of fecal accidents, baseline accidents, and number of times child had seen for encopresis by a medical professional and a mental health professional were insignificant predictors of missing data for the diary accident variable at Post when entered into a logistic regression. There were also no significant differences on FETs between groups (missing Post diary vs. non-missing) on the dichotomous variables: group, sex, race, parent’s degree, whether the parent worked outside the home, child treatment for depression, child treatment for ADHD, or parent’s comfort with the Internet. However, among the missing Post diary group, the parent was significantly more likely to be under treatment for depression at Pre (FET, p=.009), as well as less likely to check their email daily at Pre (FET, p=.019). These two variables, though, were not significant predictors of Post diary accidents within either the TAU or TAU+UCanPoopToo group (controlling for accidents at Pre).
Secondary Outcomes
Fecal accident outcomes with retrospective data
Analysis was also conducted on retrospective parent-report data to examine changes in number of fecal accidents across time. Prospective (online diary) and retrospective data for accidents were highly correlated at Post (n=57, r=.89, p<.001) and at Post12 (n=47, r=.87, p<.001). Retrospective data on accidents was available at all three time points, allowing for a 2 × 3 (Group × Time) RM ANOVA. Using an intent-to-treat approach, a trend for the 2 Group × 3 Time interaction was found, F(2, 87)=2.93, p=.059. Post-hoc RM ANOVAs were conducted and showed a trend for the Pre-Post Group × Time interaction, F(1,88)=3.44, p=.067. The TAU group did not improve significantly from Pre to Post, F(1,42)=1.09, p=.303, while the TAU+UCanPoopToo group improved significantly from Pre to Post, F(1,46)=14.45, p<.001. For the Post-Post12 post-hoc ANOVA, the Group × Time interaction revealed a significant interaction, F (1,88)=4.05, p=.047. Broken down by group, the TAU group improved significantly from Post to Post 12 (F(1,42)=13.21, p=.001), and the TAU+UCanPoopToo group showed a trend in improvement from Post to Post 12 (F(1,46)=2.86, p=.098). From Pre to Post to Post12, the median number of accidents of the TAU+UCanPoopToo group decreased from 8.0 to 4.0 to 3.0 while the TAU group median decreased from 9.0 to 8.0 to 4.0 (see Figure 3).
Knowledge
The 2 × 3 RM ANOVA conducted on the EKS measure revealed a significant Group × Time interaction, F(2,74)=8.43, p=.001. Post-hoc ANOVAs revealed a significant Pre-Post, Group × Time interaction, F(1,75)=17.06, p<.001, but not a significant Post-Post12 interaction, F(1,75)=2.26, p=.137. From Pre to Post, both groups improved significantly, F(1,37)=35.23, p<.001 and F(1,38)=4.55, p=.040 for the TAU+UCanPoopToo and TAU, respectively. The TAU+UCanPoopToo group improved from a mean score of 51% at Pre to 67% at Post, while the TAU group mean score changed from 56% at Pre to 59% at Post.
VECAT
The 2 × 3 RM ANOVA conducted on the VECAT revealed a significant Group × Time interaction, F(2,74)=3.68, p=.030. Post-hoc ANOVAs revealed a significant Pre-Post, Group × Time interaction, F(1,75)=5.72, p=.019, but not a significant Post-Post12 interaction, F(1,75)=0.40, p=.532. From Pre to Post, the TAU+UCanPoopToo group improved significantly, F(1,37)=14.68, p<.001, but the TAU group did not, F(1,38)=2.19, p=.147. The TAU+UCanPoopToo group improved from a mean score of 23.76 at Pre to 21.05 at Post, while the score for the TAU group changed from a mean score of 22.95 at Pre to 22.26 at Post.
Cost Analysis
On average, TAU+UCanPoopToo participants indicated a reduction in number of diapers used, number of school days missed, trips to school by parents, and clean-out procedures. The TAU group indicated an increase in number of diapers used and clean-out procedures, and a reduction in number of school days missed and trips to school by parents. When per unit costs were applied to the differences between groups and summed, the total weekly dollar difference between groups was $13.37 U.S. dollars, with the TAU+UCanPoopToo participants incurring less encopresis-related cost than the TAU group.
Usage and Satisfaction
Usage
Of the 47 TAU+UCanPoopToo participants, 27 (57%) completed all three Cores, 3 (6%) completed one or two Cores, and 17 (36%) did not complete any Cores. Of those 17 participants who did not complete any Cores, 14 (82%) did not provide online diary data at Post. Among those 27 participants who completed three Cores, only 3 (11%) did not provide diary data at Post. Accordingly, of the 29 participants who completed Post diary data, 26 (90%) had completed at least one Core, and 24 (83%) had completed all three Cores.
Among the participants who completed at least one Core, 24 (80%) completed at least one intervention Follow-Up, and 20 (67%) completed three or more Follow-Ups (range: 0-8 Follow-Ups completed). Among those who completed at least one Follow-Up, between 3 and 44 Modules were assigned, with a median of 16. 27 participants (57%) completed at least one Module (including some who did not complete a Core and/or did not complete a Follow-Up). Among those who completed at least one Follow-Up, 22 (92%) completed at least one Module. Among those who completed at least one Module, the median number completed was 9 (range 1-36 Modules completed).
Satisfaction
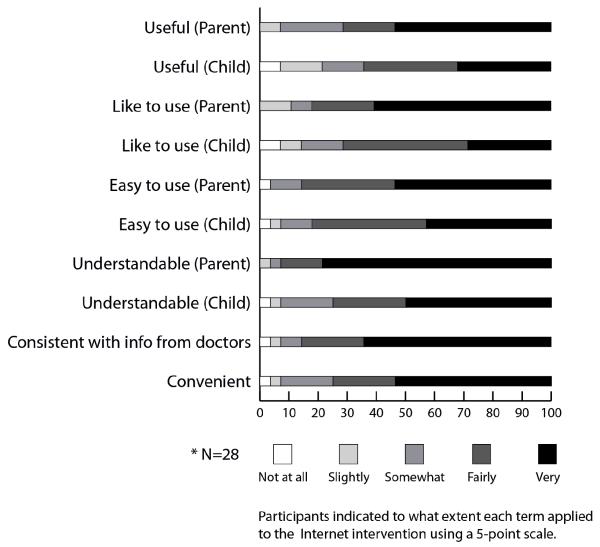
Parents of children in the TAU+UCanPoopToo group rated their satisfaction with the Internet intervention on a 5-point scale: 0 (not at all), 1 (slightly), 2 (somewhat), 3 (fairly) or 4 (very). As shown in Figure 4, a majority of parents indicated that they and their children found the intervention to be useful, easy, understandable, convenient, and that they liked it overall.
Figure 4.
Findings from the Internet Intervention Utility Questionnaire.
DISCUSSION
This paper reports on the first trial to evaluate a fully automated Internet intervention for pediatric encopresis with a US national sample of participants recruited through clinicians. Related to the primary hypothesis, this larger sample of children with encopresis who used the Internet intervention had significantly fewer accidents at both post and one year post intervention compared to those children who received routine care only. In particular, the difference at post, assessed four to six weeks from baseline using either prospective or retrospective data, showed a 50% or greater decline in frequency of accidents (depending on which type of data is used) for those receiving UCanPoopToo. This is a meaningful change clinically given that these children had an almost four year history of bowel accidents. Those who received regular ongoing clinician treatment did experience improvements, as would be expected of those receiving clinical care, but it appeared to take longer to achieve those improvements (observed at one year post). As an adjunct to care intervention, UCanPoopToo made a substantive impact in reducing accidents more quickly. In addition, those who received UCanPoopToo increased their encopresis-specific knowledge and showed greater reductions in bowel-specific problems related to encopresis and constipation than those in the TAU group, providing support for the secondary hypotheses.
These findings are similar to those found in the first trial of UCanPoopToo (Ritterband et al., 2003). In the previous trial, means were reported for the primary outcomes, whereas in this trial, medians, a more appropriate metric for this data set but still a measure of central tendency, are reported. Although a larger magnitude of change was found in the previous study, in which the children in the TAU+UCanPoopToo group went from having approximately 12 accidents to 1 accident on average per two weeks, children in this trial reduced their median of 8 accidents to 4 accidents at post and 3 accidents at one year post (based on retrospective data). Similarly, the children in the TAU groups for both the previous and current trial had no real change from baseline to post. An examination of cure and success rates across studies shows that although both groups (TAU and TAU+UCanPoopToo) improve, the improvement is greater (and faster) among the TAU+UCanPoopToo group.
Regarding intervention usage, a majority of participants allocated to the TAU+UCanPoopToo group accessed and used the intervention. Although there were participants who dropped from the study, the participants who dropped tended to be those who never used the program rather than participants trying it and then deciding to no longer use it. This suggests that those who try UCanPoopToo, tend to continue to use it more substantively. In addition, those who use it provide positive reports and experiences in using it, including finding it useful, easy, understandable, and convenient.
The limitations of this trial and its findings should be noted. In particular, no baseline prospective diary data was collected, making the pre to post to follow-up analyses more challenging to conduct and interpret. Retrospective data was collected at each time point, but participants were not asked to provide two weeks of prospective diary data at baseline because this would delay access to treatment among a group who was already seeking care with a clinician. Although the retrospective data is relatively easy to interpret, utilizing prospective data is a much more robust approach and provides more accurate results (Shiffman, Stone, & Hufford, 2008). Therefore, future studies should carefully consider collecting prospective data at baseline as well.
Another limitation was the lack of assessment between the four to six week post and one year follow-up period to understand better what happened during this time. Participants in both conditions improved during this period, but it is difficult to specify why (and exactly when) these improvements occurred. The TAU+UCanPoopToo group could continue to access the UCanPoopToo program, and both groups were able to continue to seek treatment from their clinicians or elsewhere. However, no data was collected to help explain this change during this time. Future studies should consider additional data collection time points and questions to capture potential mediators and moderators of treatment outcomes. Specifically, the effect of continued therapy services should be examined. Finally, assessing the continued use of laxatives as an outcome variable should be addressed in future research.
In contrast to these limitations, there were a number of benefits of this study. These include the collection and use of prospective diary data at post-assessments as mentioned previously. In addition, participants were from across the US. This broader sample allows for greater generalizability of the findings. Finally, the intervention utilized in this study is a fully automated one that could easily (and readily) scale up at much lower cost than an intervention including human support. Given that all participants were able to continue seeing their referring clinician in this study, future studies should consider evaluating fully automated programs without human support to determine optimal scalability and potential cost savings.
CONCLUSIONS
Internet interventions have the potential to provide much greater access to interventions often otherwise unavailable. They can supplement the provision of treatment from clinicians who might not have the knowledge, skill set, or time to provide a necessary intervention. For example, if a child with anxiety presents to a therapist, that therapist, as a skilled provider of cognitive-behavioral therapy, can appropriately address the anxiety. However, if the child also has comorbid encopresis, and the therapist does not specialize in treating that disorder, an Internet intervention, in this case UCanPoopToo, could be used as an adjunctive component of treatment. Likewise, if a parent is searching for resources to address the needs of a child with encopresis, but lives in an area with limited treatment options, or the options are expensive, unavailable, or even inconvenient to obtain, a web-based solution may be an ideal (or only) choice. A third example may be the most common: A child presents to a primary care physician for abdominal pain, and it is determined that the child has chronic constipation with fecal incontinence. The physician has had limited success prescribing high dose laxative regimens alone, but, with the advent of Internet interventions, can now prescribe a WebIP (web-based information prescription) (Ritterband et al., 2005) to address many of the behavioral issues that co-occur with encopresis (in addition to the provision of laxative medications).
These examples highlight just a few of the many ways Internet interventions can impact direct clinical practice, and specifically how UCanPoopToo can be used to provide or supplement care for children with encopresis. Preliminary evidence shows that UCanPoopToo can be used successfully as a “real world” intervention (Ritterband et al., 2008), and, with the further positive findings presented here, showing increased generalizability and long-term success, the implications for clinical practice are expanded. Two points warrant further consideration when the program is implemented in practice. Given that children with depressed mothers were less likely to complete post assessment diaries, clinicians may want to exert additional effort with these families to confirm that these families engage with the program. This point is further stressed by the fact that most users who initially engaged with the program went on to use it in a substantive way. If clinicians can help their patients to the point of initial engagement, it appears that the program may be able to capture and maintain interest. In conclusion, the ultimate success of pediatric-based Internet interventions like UCanPoopToo will hopefully lead to greater access of interventions than have previously been possible, potentially leading to improved outcomes in these areas.
Acknowledgements
The project described was supported by Grant Number R01HD028160 from the National Institute Of Child Health And Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute Of Child Health And Human Development or the National Institutes of Health. The authors also wish to thank Michelle Hilgart for her work on the figures in this paper.
Footnotes
Disclosure: Drs. Ritterband, Thorndike, and Borowitz are equity holders of BeHealth Solutions, Inc., which has negotiated a license for the software described in this paper. Drs. Ritterband, Thorndike, Borowitz, and Cox receive a royalty share based on the intervention license. The research reported herein of this manuscript pre-date this license. The terms of the arrangement have been reviewed and approved by the University of Virginia, in accordance with their respective conflict of interest policies.
REFERENCES
- Cox DJ, Ritterband LM, Quillian W, Kovatchev B, Morris J, Sutphen J, Borowitz SM. Assessment of behavioral mechanisms maintaining encopresis: Virginia encopresis-constipation apperception test. Journal of Pediatric Psychology. 2003;28(6):375–382. doi: 10.1093/jpepsy/jsg027. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Sutphen J, Borowitz SM, Kovatchev B, Ling W. Contribution of behavior therapy and biofeedback to laxative therapy in the treatment of pediatric encopresis. Annals of Behavioral Medicine. 1998;20(2):70–76. doi: 10.1007/BF02884451. [DOI] [PubMed] [Google Scholar]
- Doleys DM. Enuresis and encopresis. In: Olendick TH, Hersen M, editors. Handbook of child psychopathology. 2nd ed Plenum Press; New York: 1989. pp. 291–314. [Google Scholar]
- Levine MD. Children with encopresis: A descriptive analysis. Pediatrics. 1975;56(3):412–416. [PubMed] [Google Scholar]
- Loening-Baucke V. Chronic constipation in children. Gastroenterology. 1993;105(5):1557–1564. doi: 10.1016/0016-5085(93)90166-a. [DOI] [PubMed] [Google Scholar]
- Magee JC, Ritterband LM, Thorndike FP, Cox DJ, Borowitz SM. Exploring the relationship between parental worry about their child’s health and usage of an internet intervention for pediatric encopresis. Journal of Pediatric Psychology. 2009;34(5):530–538. doi: 10.1093/jpepsy/jsn091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath ML, Mellon MW, Murphy L. Empirically supported treatments in pediatric psychology: Constipation and encopresis. Journal of Pediatric Psychology. 2000;25(4):225–254. doi: 10.1093/jpepsy/25.4.225. [DOI] [PubMed] [Google Scholar]
- Philichi L, Yuwono M. Primary care: Constipation and encopresis treatment strategies and reasons to refer. Gastroenterology Nursing. 2010;33(5):363–366. doi: 10.1097/SGA.0b013e3181f35020. [DOI] [PubMed] [Google Scholar]
- Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams J, Staiano A, Walker L. Childhood functional gastrointestinal disorders: Child/adolescent. Gastroenterology. 2006;130:1527–1537. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Cox DJ, Gordon T, Borowitz SM, Kovatchev B, Walker LS, Sutphen J. The inclusion of audio, graphics, and interactivity in an internet intervention for pediatric encopresis. Children’s Health Care. 2006;35(1):47–59. [Google Scholar]
- Ritterband LM, Ardalan K, Thorndike FP, Magee JC, Saylor DK, Cox DJ, Borowitz SM. Real world use of an internet intervention for pediatric encopresis. Journal of Medical Internet Research. 2008;10(2):e16. doi: 10.2196/jmir.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband LM, Borowitz SM, Cox DJ, Kovatchev B, Walker LS, Lucas V, Sutphen J. Using the internet to provide information prescriptions. Pediatrics. 2005;116(5):e643–7. doi: 10.1542/peds.2005-0404. [DOI] [PubMed] [Google Scholar]
- Ritterband LM, Cox DJ, Walker LS, Kovatchev B, McKnight L, Patel K, Sutphen J. An internet intervention as adjunctive therapy for pediatric encopresis. Journal of Consulting and Clinical Psychology. 2003;71(5):910–917. doi: 10.1037/0022-006X.71.5.910. [DOI] [PubMed] [Google Scholar]
- Ritterband LM, Cox DJ, Kovatchev BP, Borowitz SM, Ling WD, Marshall B. A telecommunication monitoring system for clinical and research practice. Professional Psychology: Research & Practice. 2001;32(6):636–641. [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Tate DF, Finkelstein EA, Khayjou O, Gustafson A. Cost effectiveness of internet interventions: Review and recommendations. Annals of Behavioral Medicine. 2009;38:40–45. doi: 10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youssef N, Di Lorenzo C. Childhood constipation: Evaluation and treatment. J Clin Gastroenterol. 2001;33:199–205. doi: 10.1097/00004836-200109000-00006. [DOI] [PubMed] [Google Scholar]