Abstract
Victimization is associated with substance use in women, but less is known about linkages between witnessing community violence and substance use, even though more women witness versus directly experience violence. Further, factors that contribute to or protect against women’s problematic substance use are less well understood. Urban female caregivers (N = 318; > 92% African American/black) living in low-income communities were interviewed annually for three waves regarding exposure to community violence, coping behaviors, substance use, and protective factors. Path analyses revealed that lifetime witnessing of violence, but not victimization, assessed at baseline, was associated with changes in avoidant coping, but not active coping, one year later; avoidant coping, in turn, was related to changes in and higher levels of problematic drug use the following year. Victimization was directly related to problematic drug use, but not to alcohol use. Regression analyses indicated that high levels of religious commitment and social support at baseline were prospectively associated with lower levels of avoidant coping. Because caregivers are important role models for their children, it is important to attend to the factors that contribute to their substance use and abuse.
Keywords: violence, coping, protective factors, alcohol use, drug use
1. Introduction
As many as 70% of individuals living in urban communities are exposed to community violence (Stein et al., 2003). Community violence (CV), defined as “violence between individuals who are unrelated, and who may or may not know each other, generally taking place outside the home” can include physical and sexual assault and neglect (Krug, Dahlberg, Mercy, Zwi, & Lozano, 2002). Community violence exposure (CVE) includes both witnessing violent acts and being victimized. Many more people are indirectly exposed to CV than are directly victimized by it (Stein et al., 2003), making it important from an attributable risk perspective (Rothman & Greenland, 1998).
Parents’ exposure to CVE is associated with maladaptive parenting practices and child outcomes (e.g., Zhang & Anderson, 2010; Zhang & Eamon, 2011). Further, links between parent substance use and negative adolescent outcomes are well-established in the literature (e.g., Hops, Duncan, Duncan, & Stoolmiller, 1996), with more recent work suggesting that maternal substance use has a greater influence on adolescent outcomes than paternal use (Ohannessian et al., 2004). Given these findings, understanding the impact of CVE on female caregivers is an important priority from a prevention standpoint. Thus, the first purpose of the present study was to document associations between both witnessing and victimization by community violence and problematic alcohol and other drug use in a sample of low-income, largely minority female caregivers.
1.1 Violence, substance use, and the role of coping
Researchers (e.g., Sher, 1996) have emphasized alternative pathways to substance abuse. One pathway focuses on the tendency toward deviant behavior generally, a second pathway focuses on the reinforcing effects of substances, and a third pathway focuses on stress and negative affect. Lazarus and Folkman’s (1984) theory of stress and coping falls in the latter category and is the perspective embraced here. Lazarus and Folkman’s theory argues that violence exposure is stressful and when particular types of coping are enacted this increases the likelihood of substance use.
In support of this perspective, a few recent models linking violence and drug use have proposed coping skills as an important factor (Merrill et al., 2001; Min et al., 2007). Although there are several ways to conceptualize coping, active or engaged versus avoidant or disengaged is one commonly used rubric (Lazarus & Folkman, 1984). Avoidant coping refers to the act of consciously denying, minimizing, or delaying interaction with a stressor. Minn et al. (2007) found that avoidant coping mediated the link between childhood trauma and substance abuse in adulthood. Other researchers have shown that more frequent use of avoidant coping strategies is associated with violence exposure (Haden & Scarpa, 2008), and with more substance use and abuse (Feil & Hasking, 2008).
A few studies to date have examined victimization by violence, coping and substance use among women within one model. This work has linked avoidant coping with greater PTSD symptoms in female victims of interpersonal violence (Krause et al., 2008) and with increased substance abuse and psychological distress in a sample of urban, primarily African-American mothers of whom more than half had suffered at least one childhood trauma (Min et al., 2007). However, we are aware of no studies to date that have tested models linking witnessing community violence, coping, and substance use among women. This is an important question to address because more women witness versus directly experience violence, and because coping is modifiable and a viable target for intervention (Brown & Lewinsohn, 1984). Further, this question is even more important to understand among parents, as caregivers are powerful role models for their children (Kliewer, 2010), and understanding the factors that contribute to their problematic substance use has implications for preventing alcohol and drug abuse in their offspring. Thus, the second purpose of the study was to test a model prospectively linking victimization and witnessing community violence, use of active and avoidant coping, and problematic alcohol and other drug use.
1.2 The role of protective factors
Not all caregivers are equally affected by violence; protective factors can attenuate the relations between violence exposure, coping, and substance use, particularly those that promote approach coping. Approach coping has been linked with less alcohol and drug use and fewer drinking problems (e.g., Forys et al., 2007). It follows then that factors that promote engagement and discourage disengagement and avoidance of stressful events may best buffer against problematic use of alcohol and illicit drugs. One protective factor that might promote approach coping, reduce avoidant coping, and buffer against substance use is religious commitment. Religiousness has been defined in various ways within the literature, but measures that have included items about the importance of religion in a person’s life – regardless of the particular religion embraced -- and its influence on a person’s decisions and daily activities have found that high religiosity buffers against past year alcohol and drug use, and past year alcohol abuse (Edlund et al., 2009). Given the empirical links between religious commitment and substance use, we felt this was an important factor to consider. Further, as noted in the 2007 U.S. Religious Landscape Survey (http://www.pewforum.org/a-religious-portrait-of-african-americans.aspx), African Americans are more religious than the general U.S. population, with 87% describing themselves as belonging to a religious group. The majority of the participants in our study were African American.
A second protective factor that might promote active coping and discourage avoidant coping is social support. Social support predicts reduced alcohol and drug use (Hamdan-Mansour et al., 2007). Research additionally has suggested that social support has both direct effects on positive adjustment outcomes and indirect effects on adjustment through approach coping (Holland & Holahan, 2003). Thus, the third and final purpose of the present study was to examine religious commitment and social support as predictors of coping and buffers of the relation between violence exposure and coping.
1.3 The Current Study
We used a prospective design to evaluate a model linking CVE, coping, and problematic substance use. We hypothesized that lifetime CVE would be associated with increases in avoidant coping and decreases in active coping, which in turn would be related to increases in problematic levels of alcohol and drug use. We also anticipated direct, positive associations between CVE and alcohol and drug use. Our study contributes to the extant literature by including a focus on the effects of witnessing violence and low-income women, which is much more common in the population than direct victimization.
Secondly, we evaluated factors that theoretically reduce the likelihood of engaging in avoidant coping and enhance the use of active coping. We hypothesized that CVE’s impact on avoidant coping would be attenuated by high levels of religious commitment and social support. By including a focus on protective factors, our study contributes to the literature in that we identify possible areas or strategies of intervention.
2. Method
2.1. Participants
Participants included 318 women (M = 39.67 yrs, SD = 7.91; range = 24–71; 92.2% African American) participating in a study of CVE, coping, and adjustment. Many (40%) had never married, 33% were married or cohabitating, 25% were separated or divorced, and 2% were widowed. Approximately a quarter of the sample (24%) had not completed high school. Another 25% completed high school or earned a GED, 25% had some college, and 26% had a vocational degree, associate’s degree or higher. Approximately half of the sample had household incomes of $400/week or less; 30% of the sample had household incomes of $601 per week or more.
2.2. Measures
2.2.1. Exposure to community violence
Caregiver lifetime victimization (10 items) and witnessing violence (16 items) was assessed with Richters and Saltzman’s (1990) Survey of Exposure to Community Violence. At baseline, caregivers reported on their lifetime exposure using a scale from (0) never to (4) every day. Richters and Saltzman’s (1990) measure has been widely used and validated.
2.2.2. Coping
Coping was assessed at baseline and Wave 2 with the 12-item avoidance coping factor and the 12-item active coping factor of the COPE (Carver, et al., 1989). Caregivers responded to items using a scale ranging from (1) I don’t do this at all to(4) I do this a lot. For this study, caregivers were asked to respond to the items on the COPE in light of how they cope with violence they have experienced, seen, or heard about (excluding media violence). Carver et al. (1989) provide extensive reliability and validity information on the COPE.
2.2.3. Alcohol and other drug use
Alcohol and drug use was assessed at Wave 2 and 3. Alcohol use was assessed with the Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 2001) to identify unhealthy patterns of alcohol consumption. Items are rated on a scale from (0) 1–2 times, no, or never to (4) 10 or more, four or more times a week, depending on the question. The AUDIT has demonstrated good reliability and validity in numerous studies. Drug use was assessed with the CAGE-AID (Brown, 1992), designed to screen for problematic drug use with four questions. Items are scored as yes/no (1/0), with higher scores indicating greater problems, and scores of two or higher considered clinically significant. Research has demonstrated good reliability (e.g., Dyson et al., 1998), with high interrater reliability (kappas of 1.0), test-retest reliability (.62), and internal consistency (.84).
2.2.4. Coping resources
Religious commitment and perceived social support from family and friends were assessed at baseline. Religious commitment was assessed with the 10-item Religious Commitment Inventory-10 (RCI-10; Worthington, et al., 2003) which is appropriate for individuals in a variety of faiths. Items are rated on a scale ranging from (1) not at all true of me to (5) totally true of me. Worthington et al. (2003) report good reliability and validity. We did not collect data on the specific faiths with which individuals were affiliated. The 12-item Multidimensional Scale Perceived Social Support (MSPSS; Zimet, et al., 1988) was used to assess perceived availability of support from family (4 items) and friends (4 items) as well as total perceived support. Responses on this measure range from (1) very strongly disagree to (7) very strongly agree, with higher scores indicating greater perceived support availability. The scale is negatively correlated with depression (r = −.25), positively correlated with self-concept (r = .42), and unrelated to social desirability (Kazarian & McCabe, 1991).
2.3. Procedures
Participants were recruited from neighborhoods within Richmond, Virginia and the neighboring counties with high levels of violence and/or poverty according to police statistics and 2000 census data. Interviews were scheduled annually for three waves, and were conducted primarily in participants’ homes. Sixty nine percent of the original sample retained across the entire study. Interviewers thoroughly reviewed the caregiver consent forms with the family. A Certificate of Confidentiality was obtained from the National Institutes of Health (NIH) to protect families’ responses. Tests for interviewer race and gender effects revealed no systematic biases, ps> .10. Interviews lasted approximately 2.5 h and participants received $50 in gift cards per family at each wave.
3. Results
3.1. Attrition analyses
At the final study wave, 246 caregivers provided data. Caregivers who completed all 3waves of interviews were compared to caregivers with baseline data only (N = 318) on exposure to violence, active and avoidance coping, alcohol and drug use, religious commitment, and social support using t-tests. There were no significant differences on any of these measures, ts(318) < 1.7, n.s.
3.2 Descriptive information on the study variables
Table 1 presents descriptive information on and correlations among the study variables. Alcohol and drug use measures were log transformed due to skewness. Consistency in reports of problematic alcohol use across the three waves of data was high, rs = .63 – .77. Consistency in reports of problematic drug use also was significant, but less robust, rs = .27 – .43.
Table 1.
Descriptive statistics on and correlations among the study variables
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | M | SD | α | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Lifetime victimization | .46*** | .03 | .08 | .21*** | .13* | −.12* | 0 | .15* | .15* | .16** | .26** | 3.96 | 3.78 | .77 |
| 2. Lifetime witnessing violence | -- | .21*** | .25*** | −.03 | .06 | −.12* | −.18*** | .20** | .24*** | .09 | .25*** | 16.82 | 11.32 | .92 |
| 3. Avoidance coping (baseline) | -- | .54*** | .16** | −.09 | −.18*** | −.05 | .21*** | .13* | .05 | .15* | 21.26 | 5.88 | .79 | |
| 4. Avoidance coping (W2) | -- | −.04 | .21** | −.26*** | −.18** | .25*** | .17** | .11 | .19** | 20.49 | 6.02 | .82 | ||
| 5. Active coping (baseline) | -- | .38*** | .26*** | .30*** | .07 | .06 | 0 | .07 | 36.09 | 7.70 | .89 | |||
| 6. Active coping (W2) | -- | .16** | .17** | .04 | 0 | .02 | .06 | 34.80 | 8.52 | .91 | ||||
| 7. Social support (baseline) | -- | .16** | −.14* | −.07 | −.09 | .04 | 66.71 | 12.53 | .90 | |||||
| 8. Religious commitment (baseline) | -- | −.24*** | −.21*** | −.04 | −.03 | 35.75 | 10.95 | .95 | ||||||
| 9. Alcohol use (W2)a | -- | .63*** | .09 | .03 | 0.53 | 0.20 | .72 | |||||||
| 10. Alcohol use (W3)a | -- | .12 | .17** | 0.52 | 0.20 | .78 | ||||||||
| 11. Drug use (W2)a | -- | .27*** | 0.04 | 0.16 | .97 | |||||||||
| 12. Drug use (W3)a | -- | 0.05 | 0.17 | .93 |
Note.
Log transformed. Ns range from 232 to 319 due to attrition. W2 = Wave 2′ W3 = Wave 3.
p < .05.
p < .01.
p < .001.
In terms of the levels of problematic alcohol and other drug use in the sample, four percent of the women in the study reported one or more indicators of problematic alcohol use, including indicators such as a greater than monthly frequency of binge drinking or failing to do what was normally expected due to drinking. Nine percent of the sample reported one or more indicators of problematic drug use including feeling she ought to cut down or control drug use or being annoyed by people criticizing her drug use. Lifetime rates of victimization and witnessing violence were fairly high. Over a third of the sample had seen someone killed, and over half of the sample had seen someone shot. One quarter of the sample had been beaten up or mugged, and 11% had been attacked with a knife.
3.3. Path model testing main hypotheses
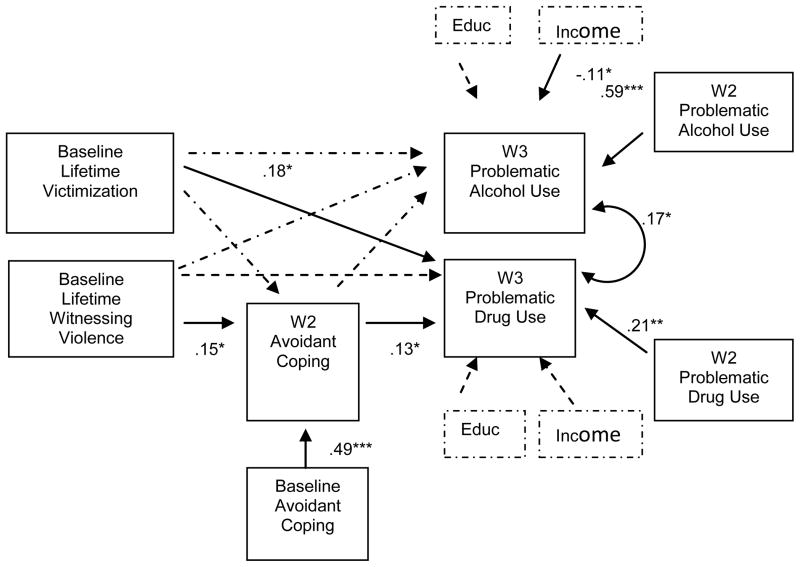
We used a path model within Mplus 6.0 (Muthen & Muthen, 2010) to evaluate the hypothesis that exposure to community violence at baseline would be associated with heightened levels of avoidant coping and reduced levels of active coping, assessed at Wave 2, which in turn would be associated with increases in alcohol and drug use, assessed at Wave 3. Baseline active and avoidant coping was controlled as was Wave 2 alcohol and drug use. The fit of the model to the data was marginal, χ2 (30) = 365.92, p < .001, CFI = .879, RMSEA = .099. Lifetime victimization was directly associated with changes in problematic drug use but not alcohol use at Wave 3. Lifetime witnessing violence but not lifetime victimization was associated with changes in avoidant coping; neither form of violence exposure was associated with changes in active coping. Avoidant but not active coping was associated with changes in problematic drug use but not problematic alcohol use.
Based on these results the model was respecified and active coping was removed (see Figure 1). Additionally, education and income were added as controls for both alcohol and drug use. In this case the data fit the model well, χ2 (8) = 19.897, p < .05, CFI =.954, RMSEA = .076. The final model indicated that exposure to violence had both direct effects on problematic drug use, and operated indirectly through an increase in avoidant coping. There was a significant negative association between income and problematic alcohol use, but no association of income and drug use or education and either alcohol or drug use.
Figure 1.
Path model linking exposure to community violence at Wave 1, avoidant coping at Wave 2, and problematic drug and alcohol use at Wave 3. N = 260. CFI = .954. RMSEA = .076. Dotted lines indicate nonsignificant paths; Solid lines indicate significant paths. * p < .05; ** p < .01; *** p < .001.
3.4. Regression analyses testing role of protecting factors
Next, hierarchical linear regression analyses were used to examine the potential protective effects of social support and religious commitment on the relation between lifetime exposure to violence and avoidance and active coping. Separate models were run for victimization and for witnessing violence, and for active and avoidant coping. We first present the models with witnessing violence as the predictor. As seen in Table 2 (model 1), the overall model was significant, F(6, 214) = 18.06, p < .001, explaining 34% of the variation in avoidant coping at Wave 2. Religious commitment was uniquely associated with changes in avoidance coping; social support was marginally associated with changes in avoidant coping. These results indicated that less religious commitment and less social support were associated with more avoidant coping. Further, none of the witnessing violence Xprotective factor interactions was significant. These results indicate that religious commitment and social support make independent contributions to changes in avoidant coping, reducing the likelihood that caregivers would engage in denial and disengagement from the problem, but do not moderate the relation between witnessing violence and changes in avoidant coping. A similar model was run predicting changes in active coping (model 2). This model also was significant, F(6, 214) = 7.06, p < .001, explaining 17% of the variation in active coping at Wave 2. However, baseline active coping was the only significant predictor.
Table 2.
Hierarchical Regression Analysis Summary for Models Predicting Coping
| Variable | B | SEB | b | R2 | cha R2 |
|---|---|---|---|---|---|
| Model 1: Dependent Variable – Avoidant Coping | |||||
| Step 1 | .30*** | .30*** | |||
| Baseline avoidant coping | 5.98 | 0.74 | 0.47*** | ||
| Baseline witnessing violence | 0.06 | 0.03 | 0.10+ | ||
| Step 2 | .33*** | .03** | |||
| Baseline religious commitment | −0.07 | 0.03 | −.13* | ||
| Baseline social support | −0.06 | 0.03 | −.11+ | ||
| Step 3 | .34*** | 0 | |||
| Witnessing X religious commitment | 0 | 0 | .01 | ||
| Witnessing X support | 0 | 0 | −.05 | ||
|
|
|||||
| Model 2: Dependent Variable – Active Coping | |||||
| Step 1 | .15*** | .15*** | |||
| Baseline active coping | 4.54 | 0.95 | 0.33*** | ||
| Baseline witnessing violence | 0.08 | 0.05 | 0.10 | ||
| Step 2 | .16*** | .01 | |||
| Baseline religious commitment | 0.06 | 0.05 | 0.07 | ||
| Baseline social support | 0.06 | 0.05 | 0.08 | ||
| Step 3 | .17*** | .01 | |||
| Witnessing X religious commitment | 0 | 0 | −.04 | ||
| Witnessing X support | 0 | 0 | −.06 | ||
|
|
|||||
| Model 3: Dependent Variable – Avoidant Coping | |||||
| Step 1 | .29*** | .29*** | |||
| Baseline avoidant coping | 6.30 | 0.73 | 0.50*** | ||
| Baseline victimization | 0.07 | 0.10 | 0.04 | ||
| Step 2 | .31*** | .04 | |||
| Baseline religious commitment | −0.09 | 0.03 | −0.16** | ||
| Baseline social support | −0.05 | 0.03 | −0.10+ | ||
| Step 3 | .31*** | 0 | |||
| Victimization X relig commitment | 0 | 0.01 | .03 | ||
| Victimization X support | 0 | 0.01 | −.04 | ||
|
|
|||||
| Model 4: Dependent Variable – Active Coping | |||||
| Step 1 | .14*** | .14*** | |||
| Baseline active coping | 4.56 | 0.97 | 0.32*** | ||
| Baseline victimization | 0.16 | 0.15 | 0.07 | ||
| Step 2 | .15*** | .01 | |||
| Baseline religious commitment | 0.03 | 0.05 | 0.04 | ||
| Baseline social support | 0.07 | 0.05 | 0.09 | ||
| Step 3 | .16*** | .01 | |||
| Victimization X relig commitment | 0 | 0.01 | .01 | ||
| Victimization X support | −0.02 | 0.01 | −.11+ | ||
Note: All values are from the final step of each regression analysis.
p < .10;
p < .05;
p < .01;
p < .001.
Next we repeated the above analyses with victimization in the model. Model 3 predicting changes in avoidant coping was significant, F(6, 213) = 17.17, p < .001, explaining 33% of the variance. In addition to avoidance coping at baseline, religious commitment was a significant predictor of changes in avoidant coping and social support a marginally significant predictor of W2 avoidance coping, indicating that less religious commitment and less social support were associated with greater use of avoidant coping. For model 4 predicting changes in active coping, the model was significant, F(6, 213) = 6.96, p < .001, explaining 16% of the variance in active coping. Baseline active coping was the only significant predictor in the model.
4. Discussion
The present study documented direct associations between lifetime victimization and witnessing CV and changes in problematic drug use even after controlling education and income, and indirect associations between lifetime witnessing of CV and changes in problematic drug use via increases in avoidant coping among low-income, largely minority caregivers. Social support and religious commitment were associated prospectively with reductions in avoidant coping but did not interact with CVE to affect changes in coping. Active coping was not predicted by nor did it predict problematic alcohol and drug use. Below we discuss the implications of coping for drug use prevention, and reasons for differences in the models predicting changes in problematic alcohol versus drug use.
Our findings are consistent with the “negative affect” pathway leading to substance use described by Sher (1996). Consistent with past research, victimization was directly associated with drug use (e.g., Merrill et al., 2001). Witnessing violence also was associated with changes in drug use via its association with avoidant coping. These analyses are robust as they control for prior substance use as well as caregiver education level and household income.
In contrast, neither victimization nor witnessing violence was associated with changes in active coping, and active coping was unrelated to alcohol or drug use. It is interesting to consider why witnessing violence was associated with avoidant but not active coping, especially since both types of coping are targeted in interventions. Active coping involves engaging with the stressor – thinking about how to solve the problem, taking steps to solve the problem, or reframing how one thinks about the problem. Avoidant coping, in contrast, involves denying the problem exists or mentally or behaviorally disengaging from it. When encountering violence, low-income women living in violent communities may come to believe that trying to change the situation or even to think about it differently is not helpful. Rather, not thinking about it may have become a way of managing the frustration surrounding the violence exposure. Substance use then becomes a way of managing affective responses to the violence around them.
Interestingly, although rates of violence exposure were quite high, rates of problematic alcohol and drug use were much lower. This suggests that exposure to violence does not inevitably lead to problematic substance use, and highlights the importance of protective mechanisms that reduce risk for substance abuse. Our findings indicate that religious commitment – regardless of religious affiliation – and to a lesser extent social support – are associated with prospective changes in avoidant coping. Caregivers with more commitment and support showed fewer increases in avoidant coping over time. This suggests that the microsystems in which caregivers are embedded shape coping responses and can contribute to a lower likelihood of problematic drug use.
4.1 Limitations
First, though we used a prospective design with well-tested measures, participants reported on their own cognitions retrospectively. Second, we did not collect data on intimate partner violence, and thus, were unable to include this as a covariate in our models. Finally, our sample endorsed low levels of substance use overall. In this study, our models predicted change in problematic drug use but not change in problematic alcohol use. Greater stability in alcohol versus drug use problems, and smaller percentages of women who endorsed problematic alcohol versus drug use likely contributed to this finding.
4.2 Implications
As noted above, strengthening caregivers’ systems of support and meaning may contribute to healthier coping, and to lower levels of problematic drug use in this population of low-income caregivers. This approach is consistent with work on resilience that emphasizes promotive processes (Wright, Masten, & Narayan, 2013), and with evidence that a sense of purpose is associated with lower levels of substance use and facilitates recovery from addiction (Grodzicki & Galanter, 2005).
A focus on bolstering promotive factors is particularly important when considering that many more individuals – especially individuals living in low-income neighborhoods – witness versus directly experience violence. Research with urban, low-income women who had both post-traumatic stress disorder (PTSD) and a substance disorder has shown that Cognitive Behavioral Therapy (CBT) is effective at reducing both PTSD and substance use (Hien et al., 2004). Thus, simultaneously addressing coping behaviors and other issues that contribute to problematic substance use appears to be an effective treatment strategy.
Highlights.
Witnessing violence is associated with increased substance use over time.
Witnessing violence is associated with increases in avoidant coping over time.
Changes in avoidant coping predict changes in drug use in female caregivers.
Religious coping is associated with decreases in avoidant coping over time.
Social support is associated with decreases in avoidant coping over time.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. Guidelines for Use in Primary Care. Geneva, Switzerland: World Health Organization; 2001. The Alcohol Use Disorders Identification Test (AUDIT) [Google Scholar]
- Brown RA, Lewinsohn PM. A psychoeducational approach to the treatment of depression: Comparison of group, individual, and minimal contact procedures. Journal of Consulting and Clinical Psychology. 1984;52:774–783. doi: 10.1037/0022-006X.52.5.774. [DOI] [PubMed] [Google Scholar]
- Brown RL. Identification and office management of alcohol and drug disorders. In: Fleming M, Barry K, editors. Addictive Disorders. St. Louis: Mosby Year Book; 1992. pp. 25–43. [Google Scholar]
- Carver C, Scheier M, Weintraub J. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Dyson V, Appleby L, Altman E, Doot M, Luchins D, Delehant M. Efficiency and validity of commonly used substance abuse screening instruments in public psychiatric patients. Journal of Addictive Diseases. 1998;17:57–76. doi: 10.1300/J069v17n02_05. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Feldman ZL. Perceived need for treatment for alcohol use disorders: Results from two national surveys. Psychiatric Services. 2009;60:1618–1628. doi: 10.1176/appi.ps.60.12.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feil J, Hasking P. The relationship between personality, coping strategies and alcohol use. Addiction Research and Theory. 2008;16:526–537. doi: 10.1080/16066350802025714. [DOI] [Google Scholar]
- Forys K, McKellar J, Moos R. Participation in specific treatment components predicts alcohol-specific and general coping skills. Addictive Behaviors. 2007;32:1669–1680. doi: 10.1016/j.addbeh.2006.11.023. [DOI] [PubMed] [Google Scholar]
- Grodzicki J, Galanter M. Spirituality and addiction. Substance Abuse. 2005;26:1–4. doi: 10.1300/J465v26n02_01. [DOI] [PubMed] [Google Scholar]
- Haden SC, Scarpa A. Community violence victimization and depressed mood: The moderating effects of coping and social support. Journal of Interpersonal Violence. 2008;23:1213–1234. doi: 10.1177/0886260508314297. [DOI] [PubMed] [Google Scholar]
- Hamdan-Mansour A, Puskar K, Sereika SM. Perceived social support, coping strategies and alcohol use among rural adolescents/USA sample. International Journal of Mental Health and Addiction. 2007;5:53–64. doi: 10.1007/s11469-006-9051-7. [DOI] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. American Journal of Psychiatry. 2004;161:1426–32. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Holland KD, Holahan CK. The relation of social support and coping to positive adaptation to breast cancer. Psychology and Health. 2003;18:15–29. doi: 10.1080/0887044031000080656. [DOI] [Google Scholar]
- Hops H, Duncan TE, Duncan SC, Stoolmiller M. Parent substance use as a predictor of adolescent use: A six-year lagged analysis. Annals of Behavioral Medicine. 1996;18:157–164. doi: 10.1007/BF02883392. [DOI] [PubMed] [Google Scholar]
- Kazarian SS, McCabe SB. Dimensions of social support in the MSPSS: Factorial structure, reliability, and theoretical implications. Journal of Community Psychology. 1991;19:150–160. doi: 10.1002/1520-6629(199104)19:2<150::AID-JCOP2290190206>3.0.CO;2-J. [DOI] [Google Scholar]
- Kliewer W. Family processes in drug use etiology. In: Scheier L, editor. Handbook of Drug Use Etiology: Theory, Methods, and Empirical Findings. Washington, D.C: American Psychological Association; 2010. pp. 365–381. [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton MA. Avoidant coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. Journal of Traumatic Stress. 2008;21:83–90. doi: 10.1002/jts.20288. [DOI] [PubMed] [Google Scholar]
- Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World report on violence and health. Geneva: World Health Organization; 2002. [DOI] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Merrill LL, Thomsen CJ, Sinclair BB, Gold SR, Milner JS. Predicting the impact of child sexual abuse on women: The role of abuse severity, parental support, and coping strategies. Journal of Consulting and Clinical Psychology. 2001;69:992–1006. doi: 10.1037//0022-006X.69.6.992. [DOI] [PubMed] [Google Scholar]
- Min M, Farkas K, Minnes S, Singer LT. Impact of childhood abuse and neglect on substance abuse and psychological distress in adulthood. Journal of Traumatic Stress. 2007;20:833–844. doi: 10.1002/jts.20250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user’s guide. Los Angeles, CA: Muthen & Muthen; 2010. [Google Scholar]
- Ohannessian CM, Hesselbrock VM, Kramer J, Bucholz KK, Schukit MA, Kuperman S, Nernberger JI., Jr Parental substance use consequences and adolescent psychopathology. Journal of Studies on Alcohol. 2004;65:725–730. doi: 10.15288/jsa.2004.65.725. [DOI] [PubMed] [Google Scholar]
- Richters J, Saltzman W. Self report version. Rockville, MD: National Institute of Health; 1990. Survey of children’s exposure to community violence. [Google Scholar]
- Rothman K, Greenland S. Modern Epidemiology. 2. New York: Lippincott, Williams & Wilkins; 1998. [Google Scholar]
- Scarpa A. Community violence exposure in young adults. Trauma, Violence, & Abuse. 2003;4:210–227. doi: 10.1177/1524838003004003002. [DOI] [PubMed] [Google Scholar]
- Sher KJ. Psychological characteristics of children of alcoholics. Alcohol Health and Research World. 1996;21:247–254. [PMC free article] [PubMed] [Google Scholar]
- Stein BD, Jaycox LH, Katoka S, Rhodes HJ, Vestal KD. Prevalence of child and adolescent exposure to community violence. Clinical Child and Family Psychology Review. 2003;6:247–264. doi: 10.1023/B:CCFP.0000006292.61072.d2. [DOI] [PubMed] [Google Scholar]
- Worthington EL, Wade NG, Hight TL, Ripley JS, et al. The Religious Commitment Inventory-10: Development, Refinement, and Validation of a Brief Scale for Research and Counseling. Journal of Counseling Psychology. 2003;50:84–96. doi: 10.1037//0022-0167.50.1.84. [DOI] [Google Scholar]
- Wright MO, Masten AS, Narayan AJ. Resilience processes in development: Four waves of research on positive adaptation in the context of adversity. In: Goldstein S, Brooks RB, editors. Handbook of resilience in children. 2. New York: Springer; 2013. pp. 15–37. [DOI] [Google Scholar]
- Zhang S, Anderson SG. Low-income single mothers’ community violence exposure and aggressive parenting practices. Children and Youth Services Review. 2010;32:889–895. doi: 10.1016/j.childyouth.2010.02.010. [DOI] [Google Scholar]
- Zhang S, Eamon MK. Parenting practices as mediators of the effect of mothers’ community violence exposure on young children’s aggressive behavior. Families in Society. 2011;92:336–342. doi: 10.1606/1044-3894.4130. [DOI] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale Perceived Social Support. Journal of Personality Assessment. 1988;52:30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]