Abstract
Objective
To determine whether the rates of nontraumatic dental condition (NTDC)-related emergency department (ED) visits are higher during the typical working hours of dental offices and lower during night hours, as well as the associated factors.
Methods
We analyzed data from the National Hospital Ambulatory Medical Care Survey for 1997 through 2007 using multivariate binary and polytomous logistic regression adjusted for survey design to determine the effect of predictors on specified outcome variables.
Results
Overall, 4,726 observations representing 16.4 million NTDC-related ED visits were identified. Significant differences in rates of NTDC-related ED visits were observed with 40%–50% higher rates during nonworking hours and 20% higher rates on weekends than the overall average rate of 170 visits per hour. Compared with 19–33 year olds, subjects < 18 years old had significantly higher relative rates of NTDC-related ED visits during nonworking hours [relative rate ratio (RRR) = 1.6 to 1.8], whereas those aged 73 and older had lower relative rates during nonworking hours (RRR = 0.4; overall P = 0.0005). Compared with those having private insurance, Medicaid and self-pay patients had significantly lower relative rates of NTDC visits during nonworking and night hours (RRR = 0.6 to 0.7, overall P < 0.0003). Patients with a dental reason for visit were overrepresented during the night hours (RRR = 1.3; overall P = 0.04).
Conclusion
NTDC-related visits to ED occurred at a higher rate during nonworking hours and on weekends and were significantly associated with age, patient-stated reason for visit and payer type.
Keywords: dental health services, dental care, emergency service, toothache
Introduction
Nontraumatic dental condition-related emergency department (ED) visits have increased substantially over time in the United States.1–3 Information on the time of day and day of week that patients visit EDs for nontraumatic dental conditions (NTDCs) is scanty and poorly documented. Ladrillo et al4 reported that 27% of patients visited the ED during regular working hours for dental care, but, this study was based on a convenience sample of children obtained from a single teaching facility. Most dental practices are open to the public during regular working hours that typically run from 8 am to 5 pm daily (excluding Saturdays and Sundays); nonworking hours or after-hours coverage for emergencies are usually restricted to existing practice patients. The time of day and day of week during which dental practices are open could pose a challenge to many patients with unmet dental needs, thereby leading such patients to seek care in EDs.
Emergency departments do not have general dental practitioners on staff to provide routine dental care to patients, but many have maxillofacial surgeons on call for trauma cases that are considered to be life-threatening. Therefore, patients with nontraumatic dental conditions mainly receive temporary care in the form of a prescription for analgesics and antibiotics, without the opportunity for continuity of care.5,6 Definitive care for such patients is best provided by trained dental care providers, the majority of whom work in private offices.
From a public health perspective, EDs serve as a link between the health care system, population health, and access to care, and provide the opportunity to collect data related to social and behavioral problems.7 Schoenfeld and McKay reported that in Nebraska, more patients with non-urgent conditions were cared for in EDs on weekends than on weekdays, based on the National Health Care Utilization data.8 Understanding and monitoring the different times of day and days of the week when nontraumatic dental condition-related ED visits occur is important for assessing the health needs of a community as well as for program planning and development.9–12 In addition, the rising number of nontraumatic dental condition-related ED visits is a public health concern that could be addressed through the development of appropriate intervention strategies.
Our study examined the rates of nontraumatic dental condition-related visits to EDs and the effect of predictors on the likelihood of visits during nonworking hours, as well as working hours versus night hours. We hypothesized that the rates of nontraumatic dental condition-related visits to EDs would be higher outside the typical working hours of dental offices and lower during night hours. It must be noted that our study emphasis was not about the decision on whether to use an ED for an NTDC-related ED visit, but rather on the choice of the timing of such a visit, given that the patient had made a decision to go to an ED for dental care.
Methods
Data source
This study used 1997–2007 data from the National Hospital Ambulatory Medical Care Survey – Emergency Departments (NHAMCS-ED). This is a publicly available national database that is tailored toward understanding the utilization of ambulatory care in noninstitutional general and short-stay hospitals within the fifty US states and the District of Columbia. Detailed information about the data source, characteristics, and data gathering procedures are described in the Ambulatory Health Care Data–Survey Instruments.13 Specially trained interviewers visited selected emergency departments to facilitate the execution of the survey and to minimize or eliminate potential hitches in its administration. A four-stage probability sampling design was used. Included in the NHAMCS-ED database were sections pertinent to race/ethnicity, financing of care, information regarding clinical presentation, diagnosis, and treatment, as well as the times and dates when the sampled patients presented in the emergency facilities.
Based on NTDC-related ED visit publications,1,5,6,14 the following ICD-9-CM codes were used: 521.0–521.9 (diseases of dental hard tissues of teeth), 522.0–522.9 (diseases of pulp and periapical tissues), 523.0–523.9 (gingival and periodontal diseases), 525.3 (retained dental root), and 525.9 (unspecified disorder of the teeth and supporting structures).1,5,6,14 Additional covariates included information on age, sex, insurance, patient-stated reason for visit, calendar year, region, location in a Metropolitan Statistical Area, and hospital ownership. The NHAMCS-ED database contains information on the expected source of payment for ED visits, which would typically refer to medical insurance. For example, patients with private insurance are more likely to be employed, whereas self-pay patients are likely uninsured and unlikely to have dental insurance, and patients on Medicaid have lower income. The Medical College of Wisconsin and Marquette University Institutional Review Boards approved the study as exempt.
Conceptual framework and visit time categories
The categorization of the time of visit was guided by our conceptual model relating the timing of NTDC-related visits to EDs to the availability of alternative care options and patient factors. The descriptors were carefully chosen after multiple consultations with research experts, dental/health advocates, and other stakeholders. These descriptors are closely aligned with current understanding of the issue and with commonly accepted terminology in this area of study.12,15–17 The typical working hours or hours of operation, defined as 8 am to 5 pm on weekdays, correspond to both the operating hours of most dental offices and the work or school day of most patients. Thus, we expected a lower rate of NTDC-related visits to EDs during these times in general, and especially for children and working age adults. On the other hand, in populations more likely to be unemployed, such as older adults or patients on Medicaid, we expected that this barrier would be less relevant. During nighttime hours, defined as 9 pm to 8 am, we also expected a low rate of visits for nontraumatic dental conditions that are typically nonemergent conditions. During the remaining nonworking hours, most dental practices would be closed, and fewer daytime barriers (such as patients having to be at work or school) would exist. We therefore anticipated that during this time, the visit rate would be the highest, especially among populations where those barriers were most relevant.
Statistical analysis
All analyses were adjusted for survey design using the weights and cluster variables provided in the NHAMCS-ED survey. Hourly visit rates were obtained by estimating the total number of visits in the US for each category of interest and dividing by the corresponding number of hours. For example, the visit rate during working hours was calculated as (weighted total frequency of visits over the study period)/(11 × 365.24 × 24 × [45/168]), to give the number of working hours during this period (45 hours of every 168-hour week). To enable comparison of the effect of covariates on the timing of the visits while eliminating the effect of these covariates on the overall rate of visits (due in part to the sizes of the corresponding population), we present relative rates (RR) normalized to the hourly visit rates during working hours.
The conversion values from weighted frequencies to rates do not depend on the observed data, so the comparison procedure is mathematically equivalent to rescaling the survey weights in inverse proportion to the length of the time period. We used this weight rescaling in multivariate polytomous survey-adjusted logistic regression to model the effect of predictors on the ratio of the rate of NTDC-related visits to EDs during nonworking and nighttime hours to that during working hours. The results of the model are presented as relative rate ratios (RRR), which is the ratio of the relative rate of visits in each subgroup to that in a reference group.
Results
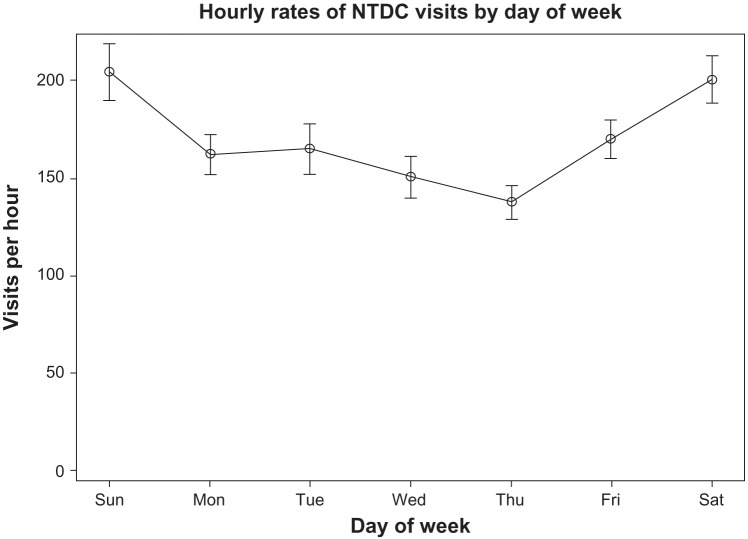
Overall, 4,726 NTDC-related ED visits were identified in the database during the study period (Table 1), which is equivalent to approximately 16.4 million NTDC-related ED visits in the United States. Based on the weighted frequency, on average about 4,080 NTDC-related ED visits occurred per day, equivalent to an average of 170 NTDC-related ED visits every hour during the study period in the United States. Significant time-related variabilities in the rates of NTDC-related ED visits were observed with 40%–50% higher rates during nonworking hours and 20% higher rates on weekends than the overall average rate (170 visits per hour). The rates of NTDC-related ED visits at night were significantly lower (20%–30%) than the overall average rate. Figure 1 shows the estimated hourly rate of NTDC-related ED visits on different days of the week. NTDC-related ED visits were highest on Sundays and Saturdays (202 visits per hour).
Table 1.
Frequency, weighted frequency and weighted hourly rate of NTDC-related visits to emergency departments by day of week, time of day (working and nonworking hours): National Hospital Ambulatory Medical Care Survey, United States,1997–2007
| Predictor/category | Frequency | Weighted frequency (millions) | Weighted visits/hour (SE) | Group/overall rate ratio | P-value |
|---|---|---|---|---|---|
| Overall | 4,726 | 16.4 | 170 (8) | ||
| Joint | <0.0001 | ||||
| Weekday (working hours >8 am–5 pm) | 1,418 | 4.7 | 182 (10) | 1.08 | |
| Weekday/weekend (nonworking hours, weekend daytime hours) | 1,847 | 6.5 | 245 (14) | 1.45 | |
| Night hours (9 pm–8 am) | 1,408 | 5.1 | 115 (6) | 0.68 | |
| Day of week | <0.0001 | ||||
| Weekday | 3,144 | 10.8 | 157 (8) | 0.92 | |
| Weekend | 1,582 | 5.6 | 202 (11) | 1.19 |
Note:P-values are from a Rao-Scott Chi-square test for matching the expected proportions.
Abbreviation: NTDC, nontraumatic dental condition; SE, standard error.
Figure 1.
Hourly rates of nontraumatic dental condition-related visits to emergency departments by day of week: National Hospital Ambulatory Medical Care Survey, United States,1997–2007.
Note: Calculated by estimating the total number of visits in the United States for each category of interest and dividing by the corresponding number of hours.
Abbreviation: NTDC, nontraumatic dental condition.
Table 2 shows the bivariate analysis of factors associated with NTDC-related ED visits separated into working hours, nonworking hours, and night hours. It is important to note that results from this analysis are relative to overall visit rates, which are strongly influenced by the size of the population. For example, non-Hispanic Whites, who comprise the largest proportion of the US population, had the highest proportion of visits, at 115 per hour out of the overall 170 visits per hour. To eliminate this effect on our main outcome of interest, the timing of NTDC-related ED visits and the relative rate of visits, which is the ratio of visit rates during nonworking hours or night hours to that during working hours, is also shown. Compared to working hours, the relative rate (RR) of visits was higher during nonworking hours (RR, 1.1– 2.5) for all the independent variables examined, except for those aged 73 years and older and for those identified as “other” payment type. This difference in visit rates is particularly pronounced in subjects aged 18 years and younger, who had more than 2-times higher visit rates during nonworking hours than working hours. The reverse was the case for night hours, when the visit rate was lower than during working hours in all subgroups (unadjusted RR, 0.3– 0.9).
Table 2.
Bivariate analysis for NTDC-related visits to emergency departments stratified by weekday and night hours based on weighted number of visits/hour: National Hospital Ambulatory Medical Care Survey, United States, 1997–2007
| Category | Weighted number of visits per hour (SE)
|
Unadjusted relative rate
|
P-value | |||
|---|---|---|---|---|---|---|
| Time of day
|
Nonworking vs working hours | Night vs working hours | ||||
| Working hours (weekday 8 am–5 pm) | Nonworking hours (other) | Night hours (9 pm–8 am) | ||||
| Age group (years) | <0001 | |||||
| 0–4 | 6.5 (1.2) | 15.9 (1.9) | 4.6 (0.7) | 2.45 | 0.71 | |
| 5–18 | 12.0 (1.5) | 25.3 (2.4) | 11.3 (1.4) | 2.11 | 0.94 | |
| 19–33 | 84.9 (6) | 111.8 (8.4) | 59.0 (4.4) | 1.32 | 0.69 | |
| 34–52 | 62.8 (4.9) | 74.0 (5) | 32.8 (2.2) | 1.18 | 0.52 | |
| 53–72 | 10.7 (1.5) | 14.5 (1.7) | 5.6 (0.8) | 1.36 | 0.52 | |
| 73 over | 5.0 (1.1) | 3.5 (0.8) | 1.6 (0.5) | 0.70 | 0.32 | |
| Metropolitan statistical area | 0.2687 | |||||
| MSA | 150.5 (11.2) | 196 (14.9) | 91.4 (6.9) | 1.30 | 0.61 | |
| Non-MSA | 31.3 (5.8) | 49.1 (8.7) | 23.6 (4.3) | 1.57 | 0.75 | |
| ED ownership | 0.0605 | |||||
| Government, non-federal | 37.2 (3.7) | 40.3 (4.8) | 20.4 (2.8) | 1.08 | 0.55 | |
| Proprietary | 22.8 (4) | 25.8 (4.2) | 12.3 (1.8) | 1.13 | 0.54 | |
| Voluntary non-profit | 121.7 (9) | 179 (11.7) | 82.2 (5.4) | 1.47 | 0.68 | |
| Payer type | <0.0001 | |||||
| Medicaid | 51.2 (4.6) | 70 (5.3) | 26.9 (2.3) | 1.37 | 0.53 | |
| Medicare | 11.1 (1.6) | 14.6 (2.1) | 5.7 (0.9) | 1.32 | 0.51 | |
| Other | 7.0 (1.2) | 4.8 (1) | 4.1 (0.7) | 0.69 | 0.59 | |
| Private insurance | 36.1 (3.3) | 69.2 (5.4) | 31.0 (2.4) | 1.92 | 0.86 | |
| Self-pay | 63.8 (4.7) | 70.6 (5.5) | 39.3 (3.2) | 1.11 | 0.62 | |
| Unknown | 12.6 (2.1) | 15.8 (2.3) | 7.9 (1.1) | 1.25 | 0.63 | |
| Race/ethnicity | 0.4320 | |||||
| Hispanic | 15.5 (1.9) | 21.5 (2.6) | 10.3 (1.2) | 1.39 | 0.66 | |
| Non-Hispanic Black | 47.8 (3.8) | 53.7 (4.6) | 28.4 (2.6) | 1.12 | 0.59 | |
| Non-Hispanic White | 114.8 (8.7) | 163.6 (11.5) | 73.6 (5) | 1.43 | 0.64 | |
| Other | 3.6 (0.8) | 6.3 (1.3) | 2.7 (0.6) | 1.75 | 0.75 | |
| Region | 0.1646 | |||||
| Midwest | 40.9 (5.6) | 59.6 (7.4) | 28.6 (3) | 1.46 | 0.70 | |
| Northeast | 38.7 (6) | 52.7 (4.8) | 20.0 (2) | 1.36 | 0.52 | |
| South | 72.8 (5.7) | 94.7 (9.8) | 49.8 (4.9) | 1.30 | 0.68 | |
| West | 29.4 (2.5) | 38.1 (5.7) | 16.5 (1.8) | 1.30 | 0.56 | |
| Patient-stated reason for visit | 0.0235 | |||||
| Dental reason | 119 (7.8) | 150.8 (10.2) | 77.3 (5.1) | 1.34 | 0.68 | |
| Non-dental reason | 68.9 (4.5) | 94.2 (6.1) | 37.7 (2.6) | 1.37 | 0.55 | |
| Sex | 0.4294 | |||||
| Female | 99 (6.3) | 134.6 (9) | 60.0 (4) | 1.36 | 0.61 | |
| Male | 82.8 (5.7) | 110.4 (6.8) | 55 (3.7) | 1.33 | 0.66 | |
| Year | 0.4255 | |||||
| 1997 | 130.7 (24.3) | 157.7 (23.5) | 83 (13.2) | 1.21 | 0.64 | |
| 1998 | 90.7 (17.2) | 176.4 (21.9) | 88.3 (16.6) | 1.94 | 0.97 | |
| 1999 | 122.1 (19.6) | 160.8 (22.2) | 70.2 (11.9) | 1.32 | 0.57 | |
| 2000 | 132.8 (18.9) | 237.9 (35.5) | 117.9 (17.9) | 1.79 | 0.89 | |
| 2001 | 182.4 (27.9) | 230.8 (30) | 99.2 (12.5) | 1.27 | 0.54 | |
| 2002 | 208.1 (29) | 269.8 (44.8) | 119.2 (16) | 1.30 | 0.57 | |
| 2003 | 193.7 (21.3) | 248.8 (31.3) | 126 (14.4) | 1.28 | 0.65 | |
| 2004 | 173.9 (22.3) | 305.6 (42) | 115.2 (18.1) | 1.76 | 0.66 | |
| 2005 | 238.3 (39.2) | 292.6 (35.2) | 144.3 (17.9) | 1.23 | 0.61 | |
| 2006 | 254.8 (36.8) | 311.8 (37.4) | 168.2 (21.6) | 1.22 | 0.66 | |
| 2007 | 272.4 (33.5) | 303.3 (41.4) | 132.8 (17.8) | 1.11 | 0.49 | |
Note:P-values are from a Rao-Scott Chi-square test.
Abbreviations: SE, standard error; MSA, Metropolitan Statistical area; NTDC, nontraumatic dental condition; ED, emergency department.
Payer type was significantly associated with the timing of NTDC-related ED visits with privately insured patients standing out as having high visit rates during nonworking hours compared to working hours. Patient-stated reason for visit was also a significant predictor: patients with a dental versus nondental reason for visit had similar relative rates for nonworking hours, but the nighttime relative visit rate was relatively higher among patients with a dental reason for visit. NTDC-related ED visit rates per hour increased substantially in all three time periods over the study period, but there were no consistent changes in the timing of the visits. These findings aligned well with expectations based on our conceptual framework of the effect of barriers on the timing of the visits.
Table 3 shows results from the multivariate polytomous logistic regression analysis of NTDC-related ED visits by comparing working hours to nonworking and night hours. Results from this analysis are consistent with those of the bivariate analysis after adjustment in the regression analysis and with our expectations from the conceptual framework. Compared with 19 to 33 year olds, patients <18 years old had higher relative rates of NTDC-related ED visits during nonworking hours only (relative rate ratio [RRR], 1.6–1.8). Patients aged 34–72 years had lower nighttime relative rates only (both RRR = 0.7), whereas those 73 years old and older had lower relative rates for both nonworking and nighttime hours (for both, RRR = 0.4; overall P = 0.0005). Compared to those with private insurance, patients with Medicare, self-pay patients and those with other/unknown sources of payment had significantly lower adjusted relative rates of NTDC-related ED visits during both nonworking hours and nights (RRRs, 0.4–0.7, overall P < 0.0003). Although only marginally significant, compared to voluntary (nonprofit) hospital EDs, government and proprietary EDs had lower adjusted relative rates of NTDC-related ED visits during nonworking hours and nighttime hours (RRs 0.7–0.8, overall P = 0.059). Compared to those with non-dental patient-stated reasons for ED visits, those who stated dental reasons for ED visits had higher adjusted relative rates of NTDC-related ED visits during nonworking hours only (RRR = 1.3, overall P = 0.0397). Race/ethnicity, calendar year, sex, region, and location in a Metropolitan Statistical Area were not significant predictors of the timing of NTDC-related ED visits during nonworking and nighttime hours compared to working hours.
Table 3.
Multivariate polytomous logistic regression analysis of factors associated with NTDC-related visits to EDs comparing nonworking and night hours with working hours: National Hospital Ambulatory Medical Care Survey, United States, 1997–2007
| Predictor/comparison | Adjusted relative rate ratio (95% CI)
|
P-value | |
|---|---|---|---|
| Nonworking vs working hours | Night vs working hours | ||
| Metropolitan statistical area | 0.5688 | ||
| Non-MSA vs MSA | 1.13 (0.84–1.52) | 1.15 (0.88–1.52) | |
| Payer type | 0.0003 | ||
| Medicaid vs private insurance | 0.71 (0.55–0.91) | 0.58 (0.44–0.77) | |
| Medicare vs private insurance | 0.92 (0.55–1.52) | 0.79 (0.48–1.32) | |
| Other vs private insurance | 0.40 (0.23–0.69) | 0.70 (0.45–1.11) | |
| Self-pay vs private insurance | 0.61 (0.47–0.79) | 0.68 (0.53–0.87) | |
| Unknown vs private insurance | 0.66 (0.43–1.00) | 0.68 (0.46–1.01) | |
| Region | 0.0777 | ||
| Midwest vs Northeast | 1.08 (0.82–1.42) | 1.39 (1.02–1.89) | |
| South vs Northeast | 1.10 (0.86–1.42) | 1.51 (1.16–1.97) | |
| West vs Northeast | 1.04 (0.74–1.48) | 1.23 (0.88–1.73) | |
| Sex | 0.5665 | ||
| Female vs male | 1.00 (0.84–1.20) | 0.92 (0.74–1.13) | |
| Calendar year | 0.98 (0.95–1.01) | 0.97 (0.94–1.00) | 0.2326 |
| Age group (years) | 0.0005 | ||
| 0–4 vs 19–33 | 1.76 (1.11–2.78) | 1.08 (0.69–1.70) | |
| 5–18 vs 19–33 | 1.58 (1.15–2.17) | 1.40 (0.96–2.03) | |
| 34–52 vs 19–33 | 0.87 (0.72–1.05) | 0.73 (0.59–0.90) | |
| 53–72 vs 19–33 | 0.96 (0.65–1.42) | 0.74 (0.48–1.16) | |
| 73 and older vs 19–33 | 0.41 (0.21–0.81) | 0.45 (0.19–1.07) | |
| Hospital ownership | 0.0592 | ||
| Government, non-federal vs voluntary nonprofit | 0.78 (0.63–0.96) | 0.78 (0.63–0.96) | |
| Proprietary vs voluntary nonprofit | 0.77 (0.56–1.04) | 0.73 (0.51–1.03) | |
| Race/ethnicity | 0.3943 | ||
| Hispanic vs NHW | 0.99 (0.73–1.35) | 1.17 (0.86–1.60) | |
| Non-Hispanic Black vs NHW | 0.78 (0.61–1.00) | 0.94 (0.75–1.19) | |
| Other vs NHW | 1.16 (0.59–2.30) | 1.18 (0.63–2.22) | |
| Patient-stated reason for visit | 0.0397 | ||
| Dental reason vs nondental reason | 1.10 (0.90–1.34) | 1.33 (1.06–1.67) | |
Note:P-values are from the Wald test.
Abbreviations: NTDC, nontraumatic dental condition; ED, emergency department; CI, confidence interval; MSA, Metropolitan Statistical Area; NHW, non-Hispanic White.
Discussion
This study is based on a nationally representative sample and shows that on average about 4,080 NTDC-related ED visits (the equivalent of 170 visits per hour) occurred per day from 1997 through 2007. The highest rates of NTDC-related ED visits occurred on weekends (202 visits per hour) and during nonworking hours (245 visits per hour). These visit rates are somewhat concerning, given that ED physicians are not sufficiently trained to manage preventable dental conditions. In addition, compared with the observed average rate, the higher NTDC-related ED visit rates of 40%–50% during nonworking hours were not completely unexpected, given that most people have difficulty leaving their workplace for dental care during normal working hours. This result is also consistent with our findings for age and insurance. In both the bivariate and multivariable analysis, age was significantly associated with of the timing of NTDC-related ED visits. Compared with 19–33 year olds, children were more likely to visit EDs during adult nonworking hours (RRR 1.6–1.7), whereas older adults arrived during working hours (RRR 0.4–0.7, P < 0.001). This result suggests that working adults with NTDCs might be waiting until nonworking hours to seek care for themselves and their children when needed.
We found that NTDC-related ED visits were highest on Saturdays and Sundays, with approximately 202 visits per hour. This trend of higher rates of visits is consistent with a study by Manski et al,18 which was based only on Medicaid data from a large teaching hospital in Baltimore. That study reported that compared with other days of the week, the number of visits for dental conditions was highest on Saturdays (21%) and Sundays (22%). Whereas our study did not specifically examine the reasons for higher visit rates in EDs during weekends, possible reasons could include a lack of work-schedule flexibility during the week among patients on hourly pay (who are incidentally also more likely to use EDs for NTDC care), and the limited availability of open dental offices on Saturdays and Sundays.14 Compared with privately insured enrollees, all other payer-type enrollees had lower relative rates of NTDC-related ED visits at the different times (RRR 0.4–0.9, overall P < 0.0003), which is consistent with the expectation that most privately insured patients are employed or have employed parents. These findings have potential program, public policy, economic and workforce implications in the quest for strategies to reduce NTDC-related visits to emergency departments.19,20 A possible program improvement could include the establishment of on-call or rotational schedules for private practitioners to manage patients in urgent care clinics.
Another interesting finding from our study relates to ownership of emergency departments. This factor was marginally associated with NTDC-related visits at the different time periods (P = 0.06). After adjustment for potential covariates, we found that compared with voluntary ED ownership, NTDC-related visits to EDs were less likely to occur in government- and proprietary ED-owned hospitals. This finding is consistent with the perceptions of health advocates, including health care providers and researchers that patients find it easier to seek care in voluntary EDs, especially when they are located in inner cities. In terms of race/ethnicity, compared with Whites, Blacks and Hispanics had somewhat lower relative rates of NTDC-related ED visits during working and night hours, except for Hispanics visiting during night hours. This was not statistically significant. Nonetheless, our findings are unexpected, given that prior studies have reported that racial and ethnic minorities are more likely to use EDs for NTDC-related ED visits, are disproportionately affected by dental disease, and have inadequate access to dental care.14 Our study suggests that decisions on the timing of visits are not influenced by the same factors as the decision to make a visit.
The potential limitations of our study must be noted. First, we are unable to determine repeat ED users for NTDC visits from our database. Second, there exists a potential for coding errors associated with the use of an administrative database. Third, the payer type information available in the database does not differentiate between medical and dental insurance. Finally, we are unable to make any distinctions between the different state variations in Medicaid coverage for dental care. Despite these limitations, the major strengths of this study include the fact that our findings are generalizable and that they include adjustments for potential confounders. Such confounders include ED ownership, regional versus metropolitan statistical area; these are important control variables linked to nontraumatic dental condition-related visits to EDs by time of day and day of week.
Conclusion
Nationally, NTDC-related visits to EDs occurred at a higher rate during nonworking hours and weekends and at lower rates during nights. Age, patient-stated reason for visit, and payer type were significantly associated with the timing of NTDC-related ED visits. Possible ways to reduce NTDC-related ED visits could include the establishment of clinics with longer hours and the provision of incentives for dental providers to work on weekends.
Acknowledgments
This study was supported by the National Institute of Dental and Craniofacial Research grant #1R15DE021196-01.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Okunseri C, Okunseri E, Thorpe JM, Xiang Q, Szabo A. Patient characteristics and trends in nontraumatic dental condition visits to emergency departments in the United States. Clin Cosmet Investig Dent. 2012;16(4):1–7. doi: 10.2147/CCIDEN.S28168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wall T. Recent trends in dental emergency department visits in the United States: 1997/1998 to 2007/2008. J Public Health Dent. 2012;72(3):216–220. doi: 10.1111/j.1752-7325.2012.00339.x. [DOI] [PubMed] [Google Scholar]
- 3.Anderson L, Cherala S, Traore E, Martin NR. Utilization of Hospital Emergency Departments for non-traumatic dental care in New Hampshire, 2001–2008. J Community Health. 2011;36(4):513–516. doi: 10.1007/s10900-010-9335-5. [DOI] [PubMed] [Google Scholar]
- 4.Ladrillo TE, Hobdell MH, Caviness AC. Increasing prevalence of emergency department visits for pediatric dental care, 1997–2001. J Am Dent Assoc. 2006;137(3):379–385. doi: 10.14219/jada.archive.2006.0188. [DOI] [PubMed] [Google Scholar]
- 5.Okunseri C, Okunseri E, Thorpe JM, Xiang Q, Szabo A. Medications prescribed in emergency departments for nontraumatic dental condition visits in the United States. Med Care. 2012;50(6):508–512. doi: 10.1097/MLR.0b013e318245a575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okunseri C, Pajewski NM, Jackson S, Szabo A. Wisconsin Medicaid enrollees’ recurrent user of emergency departments and physicians’ offices for nontraumatic dental conditions. J Am Dent Assoc. 2012;142(5):540–550. doi: 10.14219/jada.archive.2011.0224. 2011. [DOI] [PubMed] [Google Scholar]
- 7.Hirshon JM, Warner M, Irvin CB, et al. Research using emergency department-related data sets: current status and future directions. Acad Emerg Med. 2009;16(11):1103–1109. doi: 10.1111/j.1553-2712.2009.00554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schoenfeld EM, McKay MP. Weekend emergency department visits in Nebraska: higher utilization, lower acuity. J Emerg Med. 2010;38(4):542–545. doi: 10.1016/j.jemermed.2008.09.036. [DOI] [PubMed] [Google Scholar]
- 9.Lasker RD. Medicine and Public Health: the Power of Collaboration. New York, NY: Academy of Medicine; 1997. [Google Scholar]
- 10.Rhodes KV, Pollock DA. The future of emergency medicine public health research. Emerg Med Clin North Am. 2006;24(4):1053–1073. doi: 10.1016/j.emc.2006.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirshon JM. The rationale for developing public health surveillance systems based on emergency department data. Acad Emerg Med. 2000;7(12):1428–1432. doi: 10.1111/j.1553-2712.2000.tb00503.x. [DOI] [PubMed] [Google Scholar]
- 12.Varney SM, Hirshon JM. Update on public health surveillance in emergency departments. Emerg Med Clin North Am. 2006;24(4):1035–1052. doi: 10.1016/j.emc.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Ambulatory Health Care Data Survey Instruments Available from: http://www.cdc.gov/nchs/ahcd/ahcd_survey_instruments.htm#nhamcsAccessed 15 July, 2013
- 14.Okunseri C, Pajewski N, Brousseau D, Tomany-Korman S, Snyder A, Flores G. Racial and ethnic disparities in nontraumatic dental condition visits to emergency departments and physicians’ offices: a study of the Wisconsin Medicaid program. J Am Dent Assoc. 2008;139(12):1657–1666. doi: 10.14219/jada.archive.2008.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE, Myocardial Infarction Data Acquisition System (MIDAS 10) Study Group Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356(11):1099–1109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 16.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekend as compared with weekdays. N Engl J Med. 2001;345:663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 17.Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117:151–157. doi: 10.1016/j.amjmed.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 18.Manski R, Cohen LA, Hooper FJ. Use of hospital emergency rooms for dental care. Gen Dent. 1998;46(1):44–47. [PubMed] [Google Scholar]
- 19.Davis EE, Deinard AS, Maiga EW. Doctor, my tooth hurts: the costs of incomplete dental care in the emergency room. J Public Health Dent. 2010;70:205–210. doi: 10.1111/j.1752-7325.2010.00166.x. [DOI] [PubMed] [Google Scholar]
- 20.Cohen LA, Manski RJ, Madger LS, Mullins CD. Dental visits to hospital emergency departments by adults receiving Medicaid: assessing their use. J Am Dent Assoc. 2002;133:715–724. doi: 10.14219/jada.archive.2002.0267. [DOI] [PubMed] [Google Scholar]