Abstract
Body dysmorphic disorder (BDD) is a debilitating disorder characterized by an excessive pre-occupation with an imagined or very slight defect in one’s physical appearance. Despite the overall success of cognitive behavioural therapy (CBT) in treating BDD, some people do not seem to benefit as much from this approach. Those with high overvalued ideation (OVI), for instance, have been shown to not respond well with CBT. The purpose of this study was to evaluate the efficacy of an inference-based therapy (IBT) in treating BDD. IBT is a cognitive intervention that was first developed for obsessive–compulsive disorder with high OVI, but whose focus on beliefs can also apply to a BDD population. IBT conceptualizes BDD obsessions (e.g., ‘I feel like my head is deformed’) as idiosyncratic inferences arrived at through inductive reasoning processes. Such primary inferences represent the starting point of obsessional doubt and the treatment focuses on addressing the faulty inferences that maintain the doubt. Thirteen BDD participants, of whom 10 completed, underwent a 20-week IBT for BDD. The participants improved significantly over the course of therapy, with large diminutions in BDD and depressive symptoms. OVI also decreased throughout therapy and was not found to be related to reduction in BDD symptoms. Although a controlled-trial comparing CBT with IBT is needed, it is proposed that IBT constitutes a promising treatment alternative for BDD especially in cases where OVI is high.
Keywords: Body Dysmorphic Disorder, Inference-Based Approach, Inference-Based Therapy, Overvalued Ideation, Cognitive Therapy
Body dysmorphic disorder (BDD) is characterized by an excessive pre-occupation with an imagined or very slight defect in physical appearance. Although concerns can relate to body weight or shape, they should not be better accounted for by another mental disorder such as anorexia nervosa or bulimia (American Psychiatric Association, 2000). Any body part can become the focus of concern but the most common parts are the skin, hair, nose, weight and stomach (Phillips, 2005). BDD is associated with markedly poor psychosocial functioning and low quality of life (Phillips, Menard, Fay, & Pagano, 2005) and with high levels of suicidal ideation (57.8%) and suicide attempts (2.6%) (Phillips & Menard, 2006). The prevalence of the disorder in the general population appears to range between 0.7% and 2.4% (Faravelli, Salvatori, Galassi, & Aiazzi, 1997; Koran, Abujaoude, Large, & Serpe, 2008) but rates are much higher in certain groups such as students (2–13.1%) (Grant, Kim, & Crow, 2001; Mayville, Katz, Gipson, & Cabral, 1999) as well as in those presenting in dermatology (8.5–21.1%) and cosmetic surgery settings (2.9–16.6%) (Bellino etal., 2006; Bowe, Leyden, Crerand, Sarwer, & Margolis, 2007; Castle, Molton, Hoffman, Preston, & Phillips, 2004; Vulink et al., 2006).
BDD is currently classified under somatoform disorders in DSM-IV-TR, but many experts conceptualize it as an obsessive–compulsive spectrum disorder given its similarities with obsessive–compulsive disorder (OCD) in phenomenology, epidemiology, comorbidity, familial aggregation and response to treatment (Hollander, 1993). Cognitive behavioural therapy (CBT) is currently considered the psychological treatment of choice for both OCD (March, Frances, Carpenter, & Kahn, 1997) and BDD (Williams, Hadjistavropoulos, & Sharpe, 2006). The meta-analysis of Williams et al. on treatments for BDD reveals large effect sizes for CBT and supports its superiority over pharmacological treatment with selective serotonin re-uptake inhibitors.
Although encouraging, these results must be interpreted with caution as over 30% of the participants abandon treatment, and asymptomatic criteria are very rarely reached following CBT. One variable linked with poorer response to CBT in patients with BDD is overvalued ideation (OVI) (Neziroglu, Stevens, McKay, & Yaryura-Tobias, 2001). OVI refers to the strength of a particular belief along a continuum from rational thought to delusional belief and occurs in a variety of disorders. An idea is considered over-valued when the person strongly invests in the objective reality of their belief, without it reaching the level of certainty typical of a delusional belief. BDD patients have been found to show particularly high levels of OVI (McKay, Neziroglu, & Yaryura-Tobias, 1997), which makes it a pertinent variable to address in trying to improve treatment options.
Inference-based therapy (IBT) is a form of cognitive intervention originally developed for OCD with high OVI. In a recent study, IBT was shown to be as effective as behavioural or cognitive therapy as usual in treating OCD patients. Moreover, it was found to be more effective than cognitive therapy in people with OCD with high obsessional investment (O’Connor et al., 2005a). As BDD shares many similarities with OCD and as it is characterized by high levels of OVI, IBT appears a viable treatment for clients with BDD. The next section briefly presents how IBT applies to BDD obsessions.
IBT in BDD
Traditional cognitive behavioural models propose that unwanted intrusive thoughts are a universal experience, but that if they are appraised as holding negative implications for the person (e.g., ‘People will reject me because I look hideous’), the person will become preoccupied and try to ‘neutralize’ or otherwise suppress the thought, consequently maintaining the preoccupation. On the other hand, IBT conceptualizes obsessions as doubts that are supported by an inductively generated and purely idiosyncratic narrative. In fact, IBT considers that there is a subjective narrative that precedes and supports the obsessional doubt before the intrusion is even appraised. The reasoning process hypothesized to be common to OCD and BDD and to lead to obsessions is termed inferential confusion (O’Connor, Aaderna, & Pelissier, 2005b). Those whose reasoning processes are characterized by inferential confusion have a tendency to distrust their senses and common sense and to invest in remote and often imaginary possibilities at the expense of reality. See Table 1 for a list of inferential reasoning errors with examples applied to BDD. The aim of IBT is to modify the reasoning narrative producing the doubt, and to return the person to the world of common sense perception.
Table 1.
Overview of reasoning errors in BDD
| Reasoning error | Definition | Example |
|---|---|---|
| Category errors | Confusing two logical distinct properties or objects. | My sister had a nose job and got a lot of compliments. This procedure is therefore also justified for me. |
| Apparently comparable events | Confusing two distinct events separated by time or place. | Teenagers with acne get mocked, which means that I can also be laughed at if my skin is imperfect. |
| Selective use of out-of-context facts | Inappropriately applying abstract facts to specific personal contexts. | Actors with physical flaws don’t get as many contracts. |
| Purely imaginary sequences | Making up convincing stories and living them. | When people look at me I feel my nose grow even bigger and I become even uglier. |
| Distrust of normal perception | Disregarding the senses in favour of going deeper into reality. | People say I look ok but it doesn’t mean that I actually do. |
| Inverse inference | Inferences about reality precede it rather than follows from observation. | People in the room have laughed, which might mean I look ugly. |
In IBT, obsessions are conceptualized as a two-step process. The person first arrives at one or more primary inferences through a subjective narrative (inferential confusion) that leads them to confuse reality in the here and now with remote possibilities. In BDD, primary inferences are often held with great conviction, that is, the beliefs are overvalued. The primary inference is generally followed by one or more secondary inferences. Secondary inferences refer to negative anticipated consequences of primary inferences, such as ‘Nobody will ever love me because of my hideous nose’. Contrary to traditional cognitive behavioural approaches, IBT therefore addresses the initial content of the obsession through the process of inferential confusion that led to it, rather than the negative consequences arising from its appraisal. The rationale behind IBT is that even though addressing the initial doubt or primary inferences may not be necessary to dispel distress, it should be sufficient to dispel distress because it is ultimately the trigger for the secondary distressing appraisals (Aardema & O’Connor, 2003).
Objectives
The main objective of this study was to evaluate the application and effectiveness of IBT in treating BDD. Predictions were: (1) IBT would lead to a statistically significant improvement in BDD symptoms, anxiety and depressive symptoms, inferential confusion and OVI; and (2) IBT would be equally or more effective than CBT in reducing BDD symptoms (as reflected by a larger effect size than in a recent meta-analytic study). An additional research question was: Is the strength of conviction in obsessional beliefs (that is, more OVI) related to treatment outcome?
METHOD
Participants
Participants were recruited through a mixture of self-referrals and referrals from other professionals to our research clinic between 2006 and 2010. Entry criteria were: (1) a diagnosis of BDD; (2) age between 18 and 65 years; and (3) all medications were stabilized 3months prior to participation. The study excluded patients with current substance abuse, current or past schizophrenia, bipolar disorder or organic mental disorder, or those with suicidal intent. Patients with other comorbid diagnoses were included in the study as long as their primary diagnosis was BDD. Written informed consent approved by the local ethics committee was obtained from all participants.
Measures
The Yale-Brown Obsessive–Compulsive Scale Modified for BDD (BDD-YBOCS) (Phillips, Hollander, Rasmussen, & Aronowitz, 1997). The BDD-YBOCS is the clinician-administered instrument of choice for assessing the severity of BDD obsessions and compulsions (frequency, interference, distress, resistance and control). The total score ranges from 0 to 48 with higher scores indicating greater symptom severity. Scores ranging from 32 to 40 on the obsessions and compulsions subscales are considered ‘extreme’, whereas scores from 24 to 32 are considered ‘severe’; 16 to 23 ‘moderate’; 8 to 15 ‘mild’; and 0 to 7 ‘subclinical’. The scale is a modified version of the Y-BOCS (Goodman et al., 1989a; Goodman et al., 1989b), a scale assessing the severity of OCD symptoms.
The Overvalued Ideas Scale (Neziroglu, McKay, Yaryura-Tobias, Stevens, & Todaro, 1999; Neziroglu, et al., 2001) is an 11-item clinician-administered scale assessing over-valued ideas; that is, the extent to which a person hold their obsessional belief to be true. Score ranges from 0 to 10 with higher total scores indicating greater OVI.
The Beck Depression Inventory II (BDI-II) (Beck, Steer, & Brown, 1996) is a 21-item measure of cognitive and vegetative symptoms of depression for the past 2 weeks. Total score ranges from 0 to 63 with higher scores indicating greater severity of depression.
The Beck Anxiety Inventory (BAI) (Beck, Epstein, Brown, & Steer, 1988) is a 21-item anxiety rating anxiety symptom intensity for the past 2 weeks. Total score ranges from 0 to 63 with higher scores indicating greater severity of anxiety.
The Inferential Confusion Questionnaire – Expanded Version (ICQ-EV) (Aardema et al., 2010) is a 30-item questionnaire measuring inferential confusion. Scores range from 30 to 180 with higher scores signifying greater inferential confusion.
Procedure
Assessment included a two-stage process involving telephone screening interviews followed by initial questionnaires returned by mail and a face-to-face diagnostic interview with a trained independent psychologist. Baseline diagnosis used three structured interviews to provide adequate description of clinical features. In order to confirm the diagnosis of BDD and to screen for Axis I comorbid conditions, the participants were first assessed with the Structured Clinical Interview for DSM-IV Axis I Disorders (First, Spitzer, Gibbon, & Williams, 1996). Severity of BDD symptoms was then assessed using the BDD-YBOCS (Phillips, et al., 1997), as was the strength of OVI which was measured with the Overvalued Ideas Scale (OVIS) (Neziroglu, et al., 1999; Neziroglu, et al., 2001).
Treatment Protocol
Treatment consisted of 20 weekly 1hour sessions delivered by a licensed psychologist at the Fernand–Seguin Research Centre. IBT is organized in a series of 10 cumulative stages: (1) establish the nature of imaginary doubt and how it differs from real doubt (that is, a doubt being supported by sense information in the here and now); (2) familiarize the person with the reasoning process behind the doubt and emphasize that this reasoning is not incorrect in itself but rather used in out-of-context situations; (3) illustrate how the doubt goes against perception in the here and now and detracts from common sense; (4) highlight the power of imagination, unravel the subjective ‘story’ (reasoning narrative) behind the primary inference and construct an alternative realistic narrative in order to ground the person in reality sensing; (5) help the person identify a cross-over point when reality and sense information are left behind and imagination takes over; (6–7) reveal how reasoning devices (see Table 1) lead to, and renders unfounded, an arbitrary doubting inference; (8) introduce the person to the selectivity of the imaginary doubt by exploring situations where they do not experience doubts; (9) explore why the person with BDD experiences doubts in one area but not in others by targeting the vulnerable self-theme; and (10) help the person to tolerate the void that comes with the proper trust of their senses in BDD situations.
Clinical Vignette: Jim’s case1
Jim is a 31 year old single man who works full time as a fireman. He presented to our clinic complaining of disabling pre-occupations concerning his muscle mass and bone structure that have been present for the past 18 years. Jim stated that he was deeply marked by experiences of being mocked as a child, when he recalled being called ugly and scrawny. Jim’s main obsession was that if he was not ‘bigger’, he would not be attractive and as a consequence would be unable to attract women and find a girlfriend. In response to his obsession, Jim engaged in a series of compulsive and re-assuring behaviours such as working out excessively (2 hours a day, 5 days a week), eating large amounts of food, checking his appearance in the mirror (approx. 20minutes, 4–5 times a day) and comparing his appearance to people around him and people on the internet (approx. 2–3 hours a day). His social network and daily functioning was however not so impaired: he had a few friends and was functional in most areas of his life. Jim avoided going to bars and gyms (he worked out at home) and had refrained from weighing himself for over 8years. Apart from a primary diagnosis of BDD (in this case what is known as ‘muscle dysmorphia’), Jim also met criteria for social anxiety disorder and presented borderline and avoidant personality traits. He was not taking any medication. Prior to commencing therapy, Jim’s total BDD-YBOCS score was 28, which falls within the severe range of symptoms. Severity of obsessions and compulsions was equivalent and insight was fair. Associated depressive and anxiety symptoms were mild.
Jim’s first four sessions with his therapist were used for assessment purposes. Obsessions and compulsions were listed and clarified (see above). Obsessions were then explored further and dismantled in terms of IBA’s primary and secondary inferences. The question ‘What do you fear would happen if you were prevented from engaging in your compulsive and reassuring behaviours?’ will often permit to specify the person’s secondary inference. In Jim’s case, he feared that if he did not perform his rituals (e.g., working out), then he ‘Would not find a girlfriend’ and ‘Would be less attractive and popular’. Jim was 90% convinced that these consequences would come true if he did not perform his compulsions. Starting from the identified feared consequences or secondary inferences, the therapist can then work back to the initial obsessional doubt by asking ‘Which doubt would have to be eliminated for you to be able to resist the compulsions?’. In Jim’s case, the primary inference or initial doubt was ‘Perhaps I am not big enough to get noticed/respected/loved’. Jim rated this doubt as 100% probable. Having carefully specified the person’s primary and secondary inferences, the therapist can then start the IBT per se.
As mentioned earlier, the first part of the treatment aims at clarifying the distinction between imaginary and real doubt. Real doubt is justified by new sense-based information (e.g., wondering if it is cold outside after seeing people wearing jackets and scarves), whereas imaginary doubt is not based on any new information that signals problems in the here and now (e.g., Jim worrying whether he is attractive enough to be loved when waking up in the morning).There may be an external trigger (e.g., seeing one’s reflection in the mirror) but the content of the doubt is still not justified by new sense-based information in the present (e.g., someone telling Jim that he is ugly). In this sense, Jim’s reaction to the doubt (e.g., mirror gazing) does not elicit further information allowing to resolve the doubt but rather pushes him to go beyond his senses and deeper into the imagination.
The next stage of therapy familiarizes the person with the reasoning behind their imaginary doubts. The justification can appear quite logical and the main reason for this apparent ‘logicity’ is that the arguments supporting the doubt are not necessarily incorrect by themselves (e.g., ‘People sometimes get rejected because of their looks’). In other words, it is often not the content of the justification which renders the doubt ‘illogical’ but rather the context in which it occurs. For instance, Jim came up with the following arguments to justify his doubt: ‘In movies, it’s always the attractive guy that ends up with the pretty girl’ and ‘There are always women lining up at male strip clubs, therefore this is the kind of men (attractive and muscular) that women are attracted to’. These arguments were not based on realistic information in the present but rather on previous experiences and biassed logical calculation that had nothing to do with Jim’s own situation in the here and now. Jim was able to recognize this although he still found it difficult not to give credit to these justifications.
The objective of the IBT’s third stage is for the person to recognize that their imaginary doubt originates from them rather than from their senses. Here, it is important that the person understands that the term ’imagined’ does not refer to impossibility, but rather highlights the 100% lack of sense data in the here and now that could possibly justify the obsessional inference. IBT therefore does not rely on convincing the person of the unlikelihood of the doubt, but proposes its irrelevancy to the context in which it arises. This was illustrated by Jim’s therapist using an OCD example which was neutral for him: someone doubting that their hands might be dirty without any sense-based information justifying such a doubt (e.g., seeing dirt on their hands or smelling a bad odour from their hands).
The next stage of IBT aims at highlighting the power of the imagination and explaining how the imaginary doubt gets its strength from a convincing story which leads the person logically to the doubt. The person’s subjective story behind the doubt is unravelled, and an alternative story exclusively based on information present in the here and now is also created. This exercise should be introduced to the person as an attempt to come up with an alternative story rather than an attempt to ‘disproof’ the BDD story. Although Jim was able to recognize that both stories were equally possible, he still continued to invest more in the BDD story:
Jim’s BDD story: Maybe I am not big enough to get noticed/respected/loved. In the past, I have elicited positive reactions from women because I was in good shape. This proves that I must continue working out. The bigger I will be, the more I will get noticed, just as dancers in the clubs. These men look good and there are always women lining up at clubs to see them. This is therefore the kind of men that attracts women. […]Also, in movies, it is always the guy with the good looks that ends up with the pretty girl. It is not surprising that men who are in shape feel better, have more confidence and are more popular.
Jim’s alternative story: I don’t need to be big to get noticed/respected/loved. I can very well be loved, noticed and respected no matter my appearance or physical condition. I am a good listener, I have good communication skills and I am respectful of others. I enjoy helping people; in fact that’s what I chose to do as a job. I have a good sense of humour and I don’t take myself too seriously. I am easy to approach and I enjoy being with people, talk to them and reassure them. I am more than a weight or a body. All these qualities contribute much more to the love and respect that people can have for me.
The aim of the IBT’s step 5 is to help the person create distance from their obsession by learning to identify a cross-over point when they leave reality behind and get caught up in a ‘BDD bubble’, where imagination takes over. A metaphor of a bridge can be useful here: the therapist asked Jim to picture himself crossing a bridge. On one side was reality, his senses and his normal everyday reactions. On the other side was the BDD doubt. The therapist asked Jim to move across the bridge towards the doubt and identify the specific moment when imagination started to jump in. Although Jim understood the principle, he found it difficult to identify a precise moment when his BDD took over. This exercise had to be practiced repeatedly at home and in sessions before Jim was able to identify the cross-over point.
The next two steps of IBT are used to cover the reasoning devices (see Table 1) in the person’s narrative which invalidly convince them to believe in the doubt. In Jim’s case, the principal devices were category errors and selective use of out-of-context facts. Jim had a good understanding of this stage and participated well.
In step 8, the therapist introduces the person to the selectivity of the obsessional doubt by exploring situations where they do not experience such doubts. The idea here is that if the person can become aware of other situations where they adopt a ‘normal’ type of reasoning, it will highlight the irrelevance of obsessional doubts in BDD situations. The example of crossing the street was used by Jim’s therapist to illustrate this point. Jim agreed that in this situation, he did trust his senses to decide whether it is ok to cross the street (e.g., looking left and right to see if there are any cars, waiting for the green light, etc.). He did not resort to arguments based on far-fetched possibilities such as ‘A car may cross the corner suddenly’ or ‘I could be blinded by the sunlight’ that would prevent him from ever crossing the street. Jim was able to see that his reasoning differed in BDD and ‘neutral’ situations and that there was no valid reason not to trust his senses when it came to BDD situations.
The next stage of IBT is probably the one that led to the most change in Jim. The objective of step 9 is to target the person’s vulnerable self-theme by exploring why the person experiences doubts in one area, but not in others. Jim was quite able to realize that in his eyes, muscularity was directly linked with the idea of being strong and a ‘real man’ and that not being big enough made him feel weak and without character. With the help of his therapist, he was gradually able to develop a more balanced view of himself by exploring and challenging his definition of being ‘strong’ and by taking into account his other personal attributes that illustrated strength of character.
The objective of IBT’s last step is to train the person in the proper use of their senses in obsessional situations. Jim spent a lot of time each day gazing and scrupulously analyzing his reflection in the mirror. Rather than illustrating a proper use of the senses, these behaviours in fact reflect a complete distrust of the information given by the senses. In order to help Jim understand what a ‘proper use of the senses’ meant, his therapist used the neutral example of combing his hair in the morning. However, as Jim gradually learned to look at his body and trust his senses in the same fashion as he did when placing his hair, he reported feeling that he was ‘not doing enough’ or that he was ‘missing something’. People with BDD often report this feeling but as Jim’s therapist told him, it is temporary and should disappear over time as they learn to trust their senses again.
Overall, Jim collaborated well in therapy and was compliant with homework and sessions attendance. Although his symptoms improved consistently through the weeks, working on his vulnerable self-theme (IBT’s step 9) appeared to have the most impact in reducing the strength of conviction in his obsession. In fact Jim’s score on the OVIS went from 6 at pre-treatment to 2 at post-treatment. At the end of the therapy, a 79% diminution was observed in Jim’s total BDD-BOCS score, with obsessions slightly more severe than compulsions. This score (6) falls within the sub-clinical range of symptoms for BDD. Although already low at the beginning of treatment, depressive and anxiety symptoms also decrease considerably (from 14 to 3 on the BDI-II and from 12 to 3 on the BAI).
Treatment of other cases followed this pattern although there were differences in reaction to each step. For instance in another case, Julie was excessively pre-occupied with the shape of her head which she thought was hideous and deformed. She did not report a lot of compulsive behaviours, but her conviction in the reality of her defect was quite high and avoidance extremely severe. Therapy was more of a challenge with Julie. Her theoretical understanding of the model was particularly good and in therapy sessions she was able to identify errors in her reasoning. However, once she left the therapist’s office, her anxiety levels climbed up so high that she was often unable to avoid being caught up in the ‘BDD bubble’. Julie’s symptoms did decrease throughout the course of therapy but it remained a struggle for her to apply what she had learned into her daily life. Another participant, Caroline, was concerned with the look of her skin and engaged in skin picking behaviour and mirror checking in response to her obsession. For Caroline, it was realizing that she did not use the same logic in and out of BDD situations that was the most helpful: Why should she think differently when it comes to her skin than when it comes to her eyes or her hair?
Design and Data Analyses
The study design is an open-label, uncontrolled clinical trial. Treatment outcome was established with a series of paired samples t-tests for statistical significance, whereas clinical significance was defined as a 30% or greater decrease on the BDD-YBOCS total score, an empirically derived cut-point established by Phillips et al. (1997). Furthermore, an effect size statistic, d (Hedges & Olkin, 1985), was calculated for each pertinent outcome by subtracting the mean score for the pre-test from the mean score for the post-test and dividing the result by the pooled standard deviation. To assess whether IBT was equal to or more effective than CBT in treating BDD, the effect size found in the present study for BDD symptoms was compared with the standardized mean effect size reported for the five CBT interventions in the latest meta-analysis on BDD treatments. This was achieved by converting d to r (r=d/√(d2 +4), converting r to Fisher’s z, and then comparing z values using z1− z2/√((1/(N1−3))+(1/(N2−3))) as indicated by Rosenthal & Rosnow (1991). The resulting value is a Z value for which a p level is obtained in a Z table of probabilities. The sample size for the meta-analysis was obtained by adding up samples from the five CBT studies (n=125). Finally, a Pearson’s correlation was used to calculate the link between strength of OVI at pre-test and decrease in symptomatology over the course of therapy. For all analyses, an alpha level of 0.05 was considered statistically significant.
RESULTS
Eighteen participants were initially recruited and assessed for the study. One was excluded after initial assessment on the basis of comorbid substance abuse and another four never showed up again after assessment and did not return our calls. In total, 13 participants were seen by a therapist from our team and 10 of them completed the treatment. Two participants dropped out because of difficulties adhering to the protocol, whereas the other one abandoned because of a scheduling conflict. One other participant had to discontinue therapy after the 11th session because she moved to another city. We decided to carry forward her mid-treatment scores in our analyses (as post-treatment scores) as the client mentioned that she felt a lot better and that she was ready to terminate the therapy.
For those 17 participants who met the criteria for participating in the study, mean score on the BDD-YBOCS prior to therapy was 27.9 (standard deviation [SD=2.2]), which falls within the severe range of symptoms. Current comorbid disorders were: major depression (n=6), panic disorder with agoraphobia (n=1), generalized anxiety disorder (n=2) and social anxiety disorder (n=1). Locations of perceived defects were: hair (n=5), stomach (n=1), skin (n=8), ears (n=1), eyes (n=2), smell (n=1), teeth (n= 1), breasts (n=1), head (n=1) and muscle mass (n=1). Multiple concerns were seen in 24% (n=4) of the sample. The participants’ age ranged from 20 to 54years (M=34.1; SD=9.1). Fourteen were single (never married), one was married and two were separated/divorced. Two had attended high school, six had a college-level education and nine attended university. Four were on a stabilized dose of medication while participating in the study: Fluoxetine (Eli Lilly Company, IN, USA) (n=2), Quetiapine (AstraZeneca Pharmaceuticals, LP) (n =1) and Clonazepam (Roche, Basel, Switzerland) (n=1). Number of years suffering from BDD ranged from 5 to 44 (M=20.4; SD=12.4). The participants who abandoned therapy were more depressed (BDI-II M=27.7; SD=12.7) compared with treatment completers (BDI-II M=17.0; SD=3.3), but no other noteworthy differences in demographic or clinical characteristics was found.
For the 10 participants who completed the treatment, paired samples t-tests were conducted on symptom and cognitive measures. Means and standard deviations before and after treatment are shown in Table 2. In line with our first hypothesis, there was a significant decrease in BDD obsessive and compulsive symptomatology from pre- to post-treatment. This decrease in scores on both the BDD-YBOCS Obsessions (M=44.7%; SD=23.9) and Compulsions (M=51.1%; SD=21.6) subscales is also clinically significant according to the recommendations of Phillips et al. (1997). While at pre-test, 9 participants fell into the ‘severe’ range of symptoms and one in the ‘moderate’ range, at post-test none were in the ‘severe’ range of symptoms, five fell into the ‘moderate’ range, three in the ‘mild’ range and two had scores that can be considered subclinical. We also found a significant reduction in scores on the BDI-II and the OVIS (respectively measuring depressive symptoms and OVI). All changes yielded large effect sizes. However, no significant improvement was observed on the BAI and the ICQ-EV (respectively measuring anxiety and inferential confusion). The mean pre-test score on the ICQ-EV (M=58.3; SD=19.6) is quite low and in fact resembles scores found in community (M=66.5) and student (M=75.74) samples (Aardema, et al., 2010).
Table 2.
Differences pre- and post-treatment on measures
| BDD-YBOCS | M Pre | SD | M Post | SD | t | d |
|---|---|---|---|---|---|---|
|
| ||||||
| Obsessions | 14.0 | 1.9 | 7.8 | 3.5 | 6.36** | 2.2 |
| Compulsions | 13.9 | 1.5 | 6.7 | 2.8 | 6.91** | 3.2 |
| Total | 27.9 | 2.2 | 14.5 | 6.1 | 6.97** | 2.9 |
| Depression (BDI-II) | 16.7 | 3.4 | 10.9 | 4.4 | 2.82* | 1.5 |
| Anxiety (BAI) | 12.2 | 5.9 | 10.1 | 6.4 | 1.13 | 0.3 |
| Inferential confusion (ICQ-EV) | 58.3 | 19.6 | 61.7 | 24.1 | −0.56 | 0.2 |
| Overvalued ideation (OVIS) | 6.5 | 0.9 | 3.7 | 1.6 | 8.21** | 2.2 |
Note. BDD-YBOCS=Yale-Brown Obsessive–Compulsive Scale Modified for BDD; BDI=Beck Depression Inventory II; BAI=Beck Anxiety Inventory; ICQ-EV=Inferential Confusion Questionnaire – Expanded Version; OVIS= Overvalued Ideas Scale.
p<0.001.
p<0.05.
Figures 1a and b present individual results at pre- and post-treatment on the BDD-YBOCS Obsessions and Compulsions subscales and shows that although severity and degree of improvement varied between participants, all benefited from IBT. Follow-up data also suggest that therapeutic gains were sustained 6 months following the intervention, although such data is missing for four participants who failed to show up for follow-up assessments. Participant #10 terminated therapy only 2 months ago but follow-up telephone screenings with his psychologist indicate that therapeutic improvements are stable.
Figure 1.
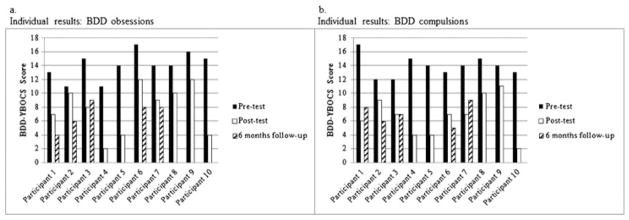
Individual results: BDD obsessions
Consistent with our second hypothesis, IBT yielded a d=2.9 effect size on the BDD-YBOCS total score, whereas the mean effect size for CBT interventions in the meta-analysis of Williams et al. was Md=1.78. However, this difference was not statistically significant, d=2.9 (r=0.82; z=1.16; n=10) vs Md=1.78 (r =0.66; z =0.79; n =125): Z = 0.95, p=0.349, NS.
Finally, we were interested in exploring the link between initial strength of OVI and treatment outcome. A Pearson product-moment correlation coefficient was computed to assess the relationship between pre-test score on the OVIS and change score on the BDD-YBOCS total score from pre- to post-treatment. There was no significant correlation between the two variables (r=−0.17, p=0.630), suggesting that OVI does not negatively impact treatment outcome with IBT. However, when one particular participant’s atypical scores were withdrawn from analyses, the correlation and alpha level increased considerably (r=−0.52, p=0.151). Also, analyses revealed a link between initial score on the OVIS and decrease in scores on the BDI-II. That is, more OVI was associated with less improvement in depressive symptoms through the course of therapy (r=−0.82, p=0.007). There was a tendency for initial score on the OVIS to be associated with decrease in scores on the anxiety measure (r=−0.65, p=0.057, NS).
DISCUSSION
The purpose of this study was to evaluate the efficacy of IBT in treating BDD. Although a recent meta-analysis reveals fair results with CBT, the current study is the first to test a psychological intervention that was specifically designed for people with high obsessional investment, a factor that has been linked with poorer response to CBT in BDD samples. Our findings indicate that IBT is not only effective in reducing BDD symptoms but also aids in reducing depressed mood that often accompanies BDD. Comparison of our effect sizes with those obtained with CBT in previously published studies failed to confirm the superiority of IBT, but the absence of a significant difference here might be attributable to our small sample size. Interestingly, no significant pre-post change was observed on anxiety or the inferential confusion questionnaire. This is contrary to our predictions. However, in BDD anxiety may not always be the dominant emotion. As for inferential confusion, in IBT it is hypothesized to be the reasoning process leading to obsessions and maintaining the preoccupation and distress. Therefore, it would be expected to decrease as obsessions subside or at least show a certain diminution at the end of therapy. Our results did not support this and it will be crucial to further investigate if inferential confusion, a concept initially developed in the context of OCD, might be manifested—and measured—in a slightly different way in BDD. For instance, the fact that our participants scored so low on the ICQ-EV might suggest that they are so confused between reality and imagination that they fail to realize it and consequently do not endorse items illustrating inferential confusion. Then, it could be that therapy does reduce inferential confusion, but in such a way that it increases the participants’ awareness of it, which makes them endorse more items than they otherwise would, thus cancelling out the pre-post improvement. If this is true, then the ICQ-EV score before and after treatment reflects two different phenomena. It is also possible that in BDD, inferential confusion is mostly characterized by a distrust of the senses and less so by an overreliance on possibility and imagination, which might be more characteristic of OCD. If so, it would be essential to modify questionnaires of inferential confusion so that they accurately target and measure the particular reasoning processes at play in BDD.
The focus of IBT on faulty inferences and overinvestment in obsessional doubts is in line with the recommendation of Labuschagne, Castle, Dunai, Kyrios and Rossell (2010) to include techniques from models of delusional thinking in the treatment of BDD. This particular focus on reasoning processes occurring before—and leading to—overinvested primary inferences fundamentally differentiates IBT from traditional CBT interventions which typically target the feared consequences of the initial doubts (that is, secondary appraisals). We believe that this quality of IBT plays a part in accounting for the absence of a significant link between OVI and decrease in BDD symptomatology in the current study. On the other hand, we did find a link between OVI and decrease in depressive symptoms during treatment. This might be due to IBT’s exclusive focus on reasoning processes underlying BDD beliefs and the absence of techniques specifically aimed at modifying cognitive processes associated with depression. It would be interesting with larger samples to identify specific factors predicting poorer response to IBT (including both BDD symptoms per se but also depressive symptomatology). For instance, there may be value in adding a module addressing depression. Overall, our findings suggest that IBT may offer a certain advantage over traditional CBT in cases where obsessional conviction is high, but more research with larger samples is needed to better understand the specificity of IBT and how it impacts OVI, BDD symptomatology and depression.
Given the chronic nature of BDD, Sarwer, Gibbons and Crerand (2004) underlined the importance of studies investigating the maintenance of treatment gains at long-term follow up. It is noteworthy that with IBT, therapeutic gains appear to be maintained—or in some cases even improved—6months following treatment, suggesting that changes in reasoning processes and inferences are enduring throughout time. It will be interesting to see if improvements are sustained at 1 year follow-up when our participants will be re-assessed.
The major limitation of this study was the small sample size. However, given the exploratory nature of the study and the large effects sizes that were found, the data and conclusions presented here still provide coherent and solid empirical support for the use of IBT in BDD and are of relevance to the field of psychological interventions for obsessive–compulsive spectrum disorders. Finally, the lack of a control group prevents attributing improvements exclusively to the IBT intervention. Notwithstanding these limitations, findings this study have several clinical implications. They highlight the relevance of assessing and addressing reasoning processes and obsessional doubts in BDD. They also suggest that IBT be considered a promising alternative to traditional CBT especially when OVI is high. Finally, they underline the importance of examining the long-term outcome of interventions.
In conclusion, results from the current study are promising but clearly a randomized-controlled trial is needed confirm IBT’s efficacy and effectiveness. It will also be crucial to explore even more how inferential confusion manifests itself in BDD and how the IBT protocol can consequently be further adapted to BDD pre-occupations.
Key Practitioner Message.
An inference-based therapy (IBT) may be effective in treating BDD.
Unlike CBT, in IBT, overvalued ideation does not appear to negatively impact decrease in BDD symptomatology.
Acknowledgments
The authors wish to thank treating psychologists Geneviève Goulet and Natalia Koszegi; Ariane Fontaine, Dominic Julien and Monique Lahoud for assessing the participants for the study; and Frederick Aardema for his feedback. This study was supported by a doctoral research scholarship awarded to the first author and by an operating grant to the second author, by the Canadian Institutes of Health Research (CIHR).
Footnotes
Certain details of the client are disguised to maintain confidentiality.
References
- Aardema F, O’Connor K. Seeing white bears that are not there: inference processes in obsessions. Journal of Cognitive Psychotherapy. 2003;17:23–37. [Google Scholar]
- Aardema F, Wu K, Careau Y, O’Connor K, Julien D, Dennie S. The expanded version of the Inferential Confusion Questionnaire: further development and validation in clinical and non-clinical samples. Journal of Psychopathology and Behavioral Assessment. 2010;32(3):448–462. doi: 10.1007/s10862-009-9157-x. [DOI] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington: APA; 2000. Text Revised. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown G. Manual for Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bellino S, Zizza M, Paradiso E, Rivarossa A, Fulcheri M, Bogetto F. Dysmorphic concern symptoms and personality disorders: a clinical investigation in patients seeking cosmetic surgery. Psychiatry Research. 2006;144(1):73–78. doi: 10.1016/j.psychres.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Bowe WP, Leyden JJ, Crerand CE, Sarwer DB, Margolis DJ. Body dysmorphic disorder symptoms among patients with acne vulgaris. Journal of the American Academy of Dermatology. 2007;57(2):222–230. doi: 10.1016/j.jaad.2007.03.030. [DOI] [PubMed] [Google Scholar]
- Castle DJ, Molton M, Hoffman K, Preston NJ, Phillips KA. Correlates of dysmorphic concern in people seeking cosmetic enhancement. The Australian and New Zealand Journal of Psychiatry. 2004;38(6):439–444. doi: 10.1111/j.1440-1614.2004.01381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faravelli C, Salvatori S, Galassi F, Aiazzi L. Epidemiology of somatoform disorders: a community survey in Florence. Social Psychiatry and Psychiatric Epidemiology. 1997 Jan;32(1):24–29. doi: 10.1007/BF00800664. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis 1 disorders – Patient edition (SCID-I/P) 2. New-York, NY: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Archives of General Psychiatry. 1989a;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischman RL, Hill CL, Charney DS. The Yale-Brown Obsessive Compulsive Scale. I. Development, use and reliability. Archives of General Psychiatry. 1989b;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW, Crow SJ. Prevalence and clinical features of body dysmorphic disorder in adolescent and adult psychiatric inpatients. The Journal of Clinical Psychiatry. 2001 Jul;62(7):517–522. doi: 10.4088/jcp.v62n07a03. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Olkin I, editors. Statistical methods for meta-analysis. New-York: Academic Press; 1985. [Google Scholar]
- Hollander E. Obsessive-compulsive spectrum disorders: an overview. Psychiatric Annals. 1993;23(7):355–358. [Google Scholar]
- Koran L, Abujaoude E, Large M, Serpe R. The prevalence of body dysmorphic disorder in the United States adult population. CNS Spectrums. 2008;13(4):316–322. doi: 10.1017/s1092852900016436. [DOI] [PubMed] [Google Scholar]
- Labuschagne I, Castle DJ, Dunai J, Kyrios M, Rossell S. An examination of delusional thinking and cognitive styles in body dysmorphic disorder. The Australian and New Zealand Journal of Psychiatry. 2010;44(8):706–712. doi: 10.3109/00048671003671007. [DOI] [PubMed] [Google Scholar]
- March JS, Frances A, Carpenter LL, Kahn D. Expert consensus treatment guidelines for obsessive-compulsive disorder: a guide for patients and families. The Journal of Clinical Psychiatry. 1997;58(suppl 4):65–72. [Google Scholar]
- Mayville S, Katz RC, Gipson MT, Cabral K. Assessing the prevalence of body dysmorphic disorder in an ethnically diverse group of adolescents. Journal of Child and Family Studies. 1999;8(3):357–362. [Google Scholar]
- McKay D, Neziroglu F, Yaryura-Tobias JA. Comparison of clinical characteristics in obsessive-compulsive disorder and body dysmorphic disorder. Journal of Anxiety Disorders. 1997;11(4):447–454. doi: 10.1016/s0887-6185(97)00020-0. [DOI] [PubMed] [Google Scholar]
- Neziroglu F, McKay D, Yaryura-Tobias JA, Stevens KP, Todaro J. The overvalued ideas scale: development, reliability and validity in obsessive-compulsive disorder. Behaviour Research and Therapy. 1999;37(9):881–902. doi: 10.1016/s0005-7967(98)00191-0. [DOI] [PubMed] [Google Scholar]
- Neziroglu F, Stevens KP, McKay D, Yaryura-Tobias JA. Predictive validity of the Overvalued Ideals Scale: outcome in obsessive-compulsive and body dysmorphic disorders. Behaviour Research and Therapy. 2001;39(6):745–756. doi: 10.1016/s0005-7967(00)00053-x. [DOI] [PubMed] [Google Scholar]
- O’Connor K, Aardema F, Bouthillier D, Fournier S, Guay S, Robillard S, Pitre D. Evaluation of an inference-based approach to treating obsessive-compulsive disorder. Cognitive Behaviour Therapy. 2005a;34(3):148–163. doi: 10.1080/16506070510041211. [DOI] [PubMed] [Google Scholar]
- O’Connor K, Aardema F, Pélissier M-C. Beyond reasonable doubt: reasoning processes in obsessive-compulsive disorder and related disorders. Chichester, UK: John Wiley & Sons, Ltd; 2005b. [Google Scholar]
- Phillips KA. The broken mirror: understanding and treating body dysmorphic disorder. New-York: Oxford University Press; 2005. [Google Scholar]
- Phillips KA, Hollander E, Rasmussen S, Aronowitz B. A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacology Bulletin. 1997;33(1):17–22. [PubMed] [Google Scholar]
- Phillips KA, Menard W. Suicidality in body dysmorphic disorder: a prospective study. The American Journal of Psychiatry. 2006 Jul;163(7):1280–1282. doi: 10.1176/appi.ajp.163.7.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Menard W, Fay C, Pagano ME. Psychosocial functioning and quality of life in body dysmorphic disorder. Comprehensive Psychiatry. 2005;46(4):254–260. doi: 10.1016/j.comppsych.2004.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R, Rosnow RL. Essentials of behavioral research: methods and data analyses. 2. McGraw-Hill Publishing Company; 1991. [Google Scholar]
- Sarwer DB, Gibbons LM, Crerand CE. Treating body dysmorphic disorder with cognitive-behavior therapy. Psychiatric Annals. 2004;34(12):934–941. [Google Scholar]
- Vulink NCC, Sigurdsson V, Kon M, Bruijnzeel-Koomen CAFM, Westenberg HGM, Denys D. Body dysmorphic disorder in 3–8% of patients in outpatient dermatology and plastic surgery clinics [English abstract] Nederlands Tijdschrift voor Geneeskunde. 2006;150(2):97–100. [PubMed] [Google Scholar]
- Williams J, Hadjistavropoulos T, Sharpe D. A meta-analysis of psychological and pharmacological treatments for body dysmorphic disorder. Behaviour Research and Therapy. 2006;44(1):99–111. doi: 10.1016/j.brat.2004.12.006. [DOI] [PubMed] [Google Scholar]


