Abstract
Purpose
Evidence suggests that expressing emotions related to cancer and receiving interpersonal support can promote psychological and physical health in women diagnosed with breast cancer. However, adaptive expression of feelings and communication with one's social network can pose challenges for patients with cancer. We report on a randomized controlled trial of an intervention, Project Connect Online, for patients with breast cancer to create personal Web sites to chronicle their experience and communicate with their social network.
Patients and Methods
Women (N = 88) diagnosed with breast cancer (any stage, any interval since diagnosis) were randomly assigned to participate in a 3-hour workshop for hands-on creation of personal Web sites with a follow-up call to facilitate Web site use, or to a waiting-list control. Assessed before randomization and 6 months after the intervention, dependent variables included depressive symptoms, positive and negative mood, cancer-related intrusive thoughts, and perceived cancer-related benefits in life appreciation and strengthened relationships.
Results
Relative to control participants, women randomly assigned to Project Connect Online evidenced significant benefit 6 months later on depressive symptoms, positive mood, and life appreciation, but not negative mood, perceived strengthened relationships, or intrusive thoughts. Treatment status moderated the intervention effects, such that women currently undergoing medical treatment for cancer benefitted significantly more from the intervention on depressive symptoms and positive mood than did women not receiving treatment.
Conclusion
Findings suggest the promise of an intervention to facilitate the ability of women diagnosed with breast cancer to chronicle their experience and communicate with their social network via the Internet.
INTRODUCTION
Most commonly, breast cancer is not experienced in isolation, but rather within an interpersonal nexus. Supportive relationships can serve as crucial resources during the cancer experience, whereas social constraint and isolation bode ill for psychological and physical health (eg,1–7). Communication can pose challenges, however, both for the cancer survivor and supportive others. The woman may want to keep others apprised of her status, but may lack the energy, fear becoming a burden, or anticipate unhelpful reactions. Friends and family may want to gain information and provide support, but might not know what to ask or how to offer effective support. Providing a channel for communication might not only facilitate interpersonal support, but also present a vehicle for expressing emotions and bolstering a sense of self-efficacy, factors that can promote adjustment.8,9 Our aim was to develop and test in a randomized controlled trial an Internet-based platform, Project Connect Online (PCO), for chronicling the experience and promoting communication by women with cancer.
Most psychosocial interventions that include an interpersonal component have been directed toward enhancing the patient–caregiver relationship or fostering relationships with other patients with cancer (eg,10,11). Promoting communication within the broader interpersonal circle also might carry benefit. Some evidence demonstrates that patients with breast cancer receive more support from friends than from male partners,12 and friends/family can offset the negative effects of partners' unsupportive behaviors.5 Peer discussion groups are particularly effective for women with unsupportive partners.10 Family and friends also desire information and support.13 Such findings suggest that interventions to enhance communication within the interpersonal network could promote well-being for both the survivor and others.
Personal Web sites are of interest to cancer survivors, as evidenced by several such platforms.14,15 A qualitative study of 50 personal Web sites of patients with breast cancer16 demonstrated that they frequently provided detailed accounts of women's experiences, provided a way to connect with others, and offered help to other patients with cancer. The researchers16 suggested that the Web sites offered a vehicle for expressing emotion and bolstering a sense of efficacy/control. Whether such Web sites are effective in bolstering psychological and physical health-related adjustment of cancer survivors is unknown, however.
To our knowledge, ours is the first research to evaluate an intervention to teach patients with cancer personal Web site development. The primary hypothesis was that, relative to women assigned to a waiting-list control condition, women trained to create a personal Web site would improve in general psychological adjustment (depressive symptoms, negative/positive mood) and cancer-specific adjustment (cancer-related intrusive feelings/thoughts, perceived cancer-related benefits of strengthened relationships and life appreciation) 6 months later. With the rationale that women undergoing medical treatment would have a greater need to manage communication and express emotions than women who had completed treatment, we also hypothesized that PCO would be more effective for the former.
PATIENTS AND METHODS
Patients
Participants were recruited from a community medical oncology practice specializing in breast cancer. Eligibility criteria included the following: age at least 18 years; diagnosis of invasive or metastatic breast cancer (any interval since diagnosis); ability to complete the intervention and questionnaires in English; no existing personal Web site (any comfort/skill level with computers allowed). Participants also had to return the baseline questionnaire within 1 month of receipt. This preliminary trial was designed to establish whether effect sizes were sufficient to pursue a larger trial and to detect large effects (d = 0.80) in an analysis of covariance with 80% power, two-sided P < .05, and 20% attrition, which required 33 participants per group. Sample size was expanded to 44 per group because of available resources.
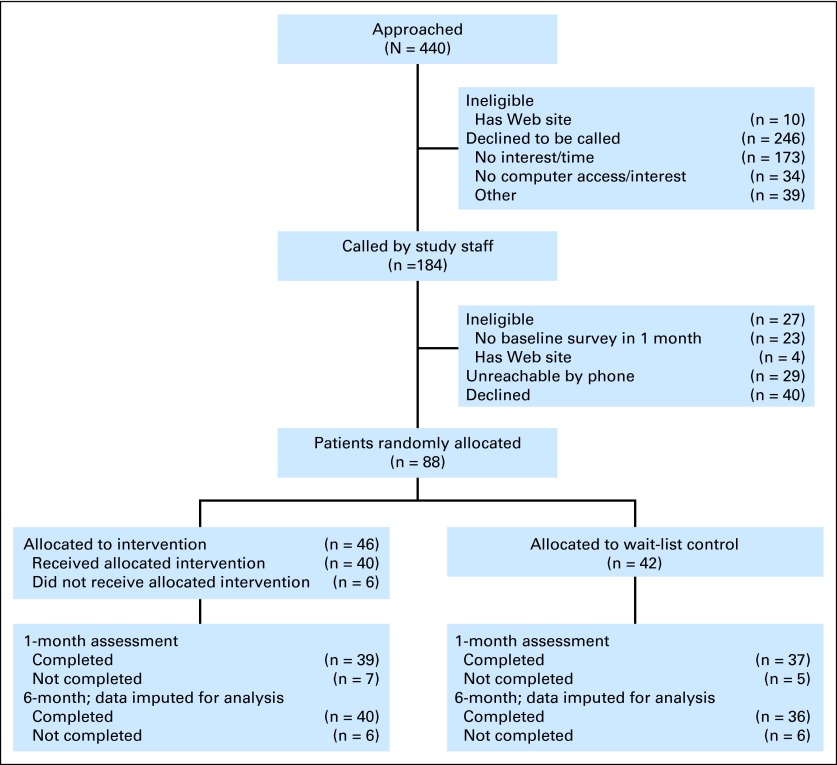
Of 440 women approached, 8% (n = 37) were ineligible, 72% (n = 315) declined to hear more about the study or were unreachable by telephone, and 20% (n = 88) were randomly assigned and included in analyses (Fig 1). Of the 88 women randomly assigned, 86% (n = 76) completed the 1-month assessment, and 86% (n = 76) completed the 6-month assessment.
Fig 1.
Project Connect Online accrual and retention.
Procedure
On institutional review board approval, within clinic scheduling constraints, consecutive potentially eligible patients were approached at a medical appointment by the clinic's research coordinator, following a standard verbal script. Women were informed that the purpose of the research was “to evaluate a workshop held here to create your own personal Web site to communicate with friends and loved ones about your experience.” Treating physicians were unaware of patients' participation.
With verbal consent, the research coordinator provided contact information to research staff, who called potentially eligible women to describe the study and confirm eligibility. Interested and eligible women were mailed informed consent forms and questionnaires, which they returned by mail. After packet return, each participant's assigned condition was revealed to research staff from a random allocation sequence generated by a biostatistician uninvolved in the trial, whereupon staff called to schedule the intervention session or inform the participant that she would continue assessments and be offered the workshop in 6 months. One and 6 months after the intervention, women completed and returned additional questionnaires by mail. Timing of assessments was designed to capture change in potential mediators at 1 month (not reported here) and mediators and effects of PCO after sufficient time to use the Web site (6 months). Data entry personnel were unaware of participants' condition assignment. Participants were compensated $50 per returned questionnaire.
PCO intervention.
Three phases informed the development of PCO: semistructured interviews of eight patients with breast cancer who had created cancer-related personal Web sites; focus groups of seven patients with breast cancer to evaluate barriers, facilitators, and preferences for creating Web sites (Appendix, online only); and, once the Web site template, manual, and workshop protocol were developed, a pilot intervention session with four patients with breast cancer to elicit feedback, with resulting slight modifications before launching PCO.
The researchers collaborated with a Web site development firm,17 using the WordPress multisite Web site and blogging platform,18 to develop a design that allowed for personalization of esthetics and content (eg, Web site template, links). Each template contained six identical functions (1): a journal (blog) that could contain photos; (2) a section for Web site links, to be populated by each participant (a list of potential Web sites was provided by the researchers [eg, the oncology clinic, National Cancer Institute, American Society of Clinical Oncology public site]); (3) a How You Can Help page, in which participants could convey actions visitors could undertake (eg, meal provision, written cards); (4) choice of privacy settings; (5) instructions for visitors to post messages and subscribe for automatic notification of Web site updates; and (6) an online survey to assess visitors' reactions to PCO (data not reported here). The researchers and Web site development firm also created a 48-page manual with written and visual instructions for Web site creation and maintenance and online step-by-step video tutorials for creating/maintaining Web site functions (eg, adding a link or photo).
Once a minimum of three women were randomly assigned to the intervention, two members of the research team (A.L.S., E.H.T., postbaccalaureate research staff) conducted a 3-hour intervention session in a conference room of the medical oncology practice. Participants could use a researcher-provided laptop computer or bring their own. Delivered in groups of one to five participants (along with significant others), the intervention, accompanied by the take-home manual, involved (1) a description of potential functions of personal Web sites (eg, keep others informed, manage communication, chronicle the experience); (2) proactive discussion of common concerns about maintaining a Web site (eg, perceived pressure to post frequent updates or to convey only positive content; see Appendix); (3) demonstration of all Web site functions (ie, privacy settings, journal, photo posting, links, How You Can Help page, visitor survey); (4) discussion of how to introduce the Web site to others; (5) demonstration of online tutorials; and (6) hands-on creation of the Web site, which involved selecting one of 11 templates, creating a Web site title, and initiating the first journal post to introduce others to the Web site. A toll-free phone number was provided for technical support from the Web site development firm. As scheduled during the intervention session, a researcher (E.H.T.) called each participant 1 week later to respond to questions. Conversations were less than 15 minutes. Wireless access was available during oncology clinic hours for participants to update Web sites, and cameras and laptops were available for check-out.
Waiting-list control.
Patients in the control condition completed the baseline and follow-up assessments and otherwise received standard medical care. Participation in PCO was offered once women had completed the 6-month assessment; eight patients participated.
Measures
At baseline, participants self-reported sociodemographic (ie, age, education, race/ethnicity, employment, partner status, familial/social network data) and cancer-related variables (ie, diagnosis date, stage, treatment status, specific treatments).
Outcomes were measured at each assessment. Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale.19 Internal consistency reliability was high at all assessments (α = 0.89 to 0.91). Participants completed the Profile of Mood States20 with regard to their feelings in the past week. As in other studies with samples of patients with cancer,21–25 we constructed a negative mood index from items (eg, sad, tense) on the highly correlated anger, depression, tension, fatigue, and confusion subscales and a positive mood index with the vigor subscale items (eg, cheerful, lively). Internal consistency reliabilities were high for negative (α = 0.96 to 0.97) and positive (α = 0.79 to 0.93) mood. Within assessment points, correlations between these dependent variables ranged in absolute value from r = 0.48 to 0.79, all P < .01.
Participants also completed cancer-related outcome measures. On the 7-item Impact of Event–Intrusion subscale,26 which assesses cancer-related intrusive thoughts and feelings, women rated how frequently each item (eg, “I had waves of strong feelings about it”) was true for them during the past 7 days with regard to their cancer experience (α = 0.87 to 0.89). With the rationale that PCO could bolster perceived cancer-related benefits in specific domains, Posttraumatic Growth Inventory (PTGI)27 subscales selected for assessment were Appreciation of Life (eg, “I can better appreciate each day”; α = 0.83 to 0.83) and Relating to Others (eg, “I more clearly see that I can count on people in times of trouble”; α = 0.87 to 0.89). Women rated items for the degree to which each change had occurred as a result of the cancer experience. Within assessment points, correlations of PTGI subscales with Impact of Event–Intrusion ranged from r = −0.02 to 0.14, all P > .10.
Fidelity to the PCO workshop protocol (ie, evidence that the intervention was delivered as intended) was assessed on a 20-item author-constructed measure by two research staff uninvolved in PCO performance. With informed consent, intervention sessions were audio recorded. Each yes/no item (eg, “discussed common concerns about using a Web site and how these can be proactively addressed,” “explained privacy settings and demonstrated how to change them”) was rated independently by raters while listening to each tape.
Data Analysis
All analyses were preplanned. The randomized groups were compared on all baseline variables using χ2 for categorical variables and t tests for continuous variables. Treatment fidelity was calculated as the percentage of workshop protocol elements covered, as judged by two independent raters. Outcome analyses were conducted using analysis of covariance, with the 6-month measure as the dependent variable and group assignment, current medical treatment (radiotherapy, chemotherapy, biologic therapy [endocrine therapy not counted]: yes/no), their interaction, and the baseline measure as independent variables. No adjustment was made to correct for multiple statistical comparisons. Main effects were estimated as adjusted mean differences between levels of each factor. When the interaction was significant, we estimated differences in adjusted means among pairs of the four cells defined by the interaction. Intent-to-treat analyses were conducted using Markov chain Monte Carlo multiple imputation28–30 of missing outcomes under a missing at random assumption, as implemented in SAS PROC MI; 30 imputed data sets were analyzed and estimates combined using PROC MI ANALYZE (see Appendix for details). Analyses were repeated with data of participants retained at 6 months. Cohen d effect sizes were obtained as differences in adjusted means using standardized variables in analyses. Analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC).
RESULTS
Sample Characteristics
Most participants were married, non-Hispanic white, college graduates, and employed outside the home (Table 1). On average, participants were 56 years old and had been diagnosed with breast cancer more than 5 years earlier. Twenty-one women were in medical treatment, and 17 had metastatic disease.
Table 1.
Characteristics of Participants at Baseline (N = 88)
| Characteristic | Control Group Participants (n = 42) |
Project Connect Online Participants (n = 46) |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| Age, years | ||||
| Mean | 56 | 55 | ||
| SD | 10 | 12 | ||
| Range | 37-76 | 28-76 | ||
| Race | ||||
| Non-Hispanic white | 33 | 83 | 39 | 87 |
| African American | 2 | 5 | 1 | 2 |
| Asian American | 4 | 10 | 0 | 0 |
| Latina | 0 | 0 | 5 | 11 |
| American Indian | 1 | 3 | 0 | 0 |
| College graduate | 30 | 71 | 29 | 63 |
| Employed ≥ 30 h per week outside home | 24 | 57 | 21 | 46 |
| Married/living as married | 25 | 60 | 34 | 74 |
| Time since first breast cancer diagnosis, years | ||||
| < 2 | 14 | 33 | 7 | 15 |
| 2-5 | 9 | 21 | 18 | 39 |
| 5-10 | 14 | 33 | 16 | 35 |
| ≥ 10 | 5 | 12 | 5 | 11 |
| Metastatic breast cancer diagnosis | 8 | 22 | 9 | 21 |
| Current primary medical treatment | 11 | 26 | 10 | 22 |
| Dependent variables at baseline | ||||
| CES-D | ||||
| Mean | 12 | 11 | ||
| SD | 10 | 9 | ||
| Range | 0-36 | 0-34 | ||
| POMS-Negative Mood | ||||
| Mean | 35 | 30 | ||
| SD | 34 | 27 | ||
| Range | −7-119 | −4-92 | ||
| POMS-Vigor | ||||
| Mean | 18 | 16 | ||
| SD | 6 | 8 | ||
| Range | 5-30 | 0-32 | ||
| Impact of Event Scale (Intrusion) | ||||
| Mean | 11 | 8 | ||
| SD | 9 | 7 | ||
| Range | 0-35 | 0-25 | ||
| PTGI Relating to Others Subscale | ||||
| Mean | 24 | 22 | ||
| SD | 7 | 8 | ||
| Range | 6-34 | 3-35 | ||
| PTGI Life Appreciation Subscale | ||||
| Mean | 11 | 11 | ||
| SD | 3 | 3 | ||
| Range | 3-15 | 3-15 | ||
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; POMS, Profile of Mood States; PTGI, Posttraumatic Growth Inventory; SD, standard deviation.
The randomized groups did not differ significantly (all P > .05) at baseline on any demographic, cancer-related, or outcome measure, nor was treatment status or the interaction of condition with treatment status associated with significant differences on any baseline variable. Although not statistically significant, women in current medical treatment had somewhat worse status on all outcomes at baseline. Baseline variables did not differ significantly at P < .05 between participants who completed (n = 76) or did not complete (n = 12) the 6-month assessment.
Treatment Fidelity
Eight of 15 sessions were audio taped in full. On the measure of treatment fidelity, two independent raters agreed that there was 100% fidelity to the workshop protocol.
Outcome Analyses
General measures of psychological adjustment.
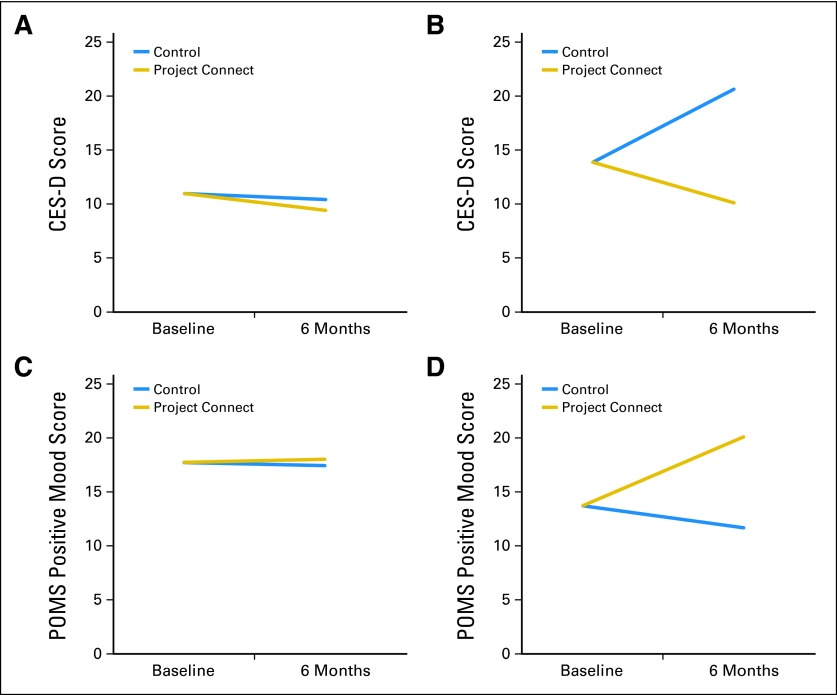
Intent-to-treat results for depressive symptoms and negative and positive mood are presented in Table 2, with additional results pertinent to the significant interactions displayed in Table 3. All effect sizes for statistically significant effects were moderate to large. Women in medical treatment reported more depressive symptoms at 6 months than did those not in treatment (P = .04), and PCO produced a significant benefit on depressive symptoms (P = .009). These main effects were qualified by a significant interaction (P = .03; Fig 2), whereby PCO buffered the increase in depressive symptoms experienced by women in medical treatment who were assigned to the control condition. Specifically, for PCO participants, 6-month depressive symptoms did not differ significantly as a function of medical treatment, and they were significantly lower than depressive symptoms of control patients in medical treatment (all P < .006). Control participants in medical treatment demonstrated a significant increase in depressive symptoms compared with women not in treatment (P = .004). Effects on negative mood were not statistically significant, although the pattern of cell means mirrored that for depressive symptoms.
Table 2.
Results of Intent-to-Treat Outcome Analysis for Project Connect Online (N = 88)
| Outcome | Main Effect of Group Assignment |
Main Effect of Medical Treatment Status |
Interaction, P | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PCO (n = 46) |
Control (n = 42) |
P | Cohen d | 95% CI | Current Treatment (n = 21) |
Not in Treatment (n = 67) |
P | Cohen d | 95% CI | ||||||
| Adjusted Mean | SE | Adjusted Mean | SE | Adjusted Mean | SE | Adjusted Mean | SE | ||||||||
| CES-D | 9.7 | 1.6 | 15.5 | 1.7 | .009 | 0.6 | 0.1 to 1.1 | 15.7 | 1.7 | 10.1 | 1.0 | .04 | 0.6 | 0.0 to 1.1 | .03 |
| POMS-Negative Mood | 22.4 | 3.8 | 30.1 | 3.8 | .14 | 0.3 | −0.1 to 0.7 | 29.5 | 4.7 | 22.9 | 2.6 | .20 | 0.3 | −0.2 to 0.8 | .16 |
| POMS-Vigor | 18.2 | 1.2 | 14.7 | 1.2 | .03 | 0.5 | 0.1 to 0.9 | 15.4 | 1.5 | 17.4 | 0.8 | .42 | 0.2 | −0.3 to 0.7 | .04 |
| Impact of Event Scale (Intrusion) | 8.5 | 1.0 | 11.6 | 1.0 | .13 | 0.4 | −0.1 to 0.8 | 11.7 | 1.3 | 8.5 | 0.7 | .12 | 0.4 | −0.1 to 0.8 | .89 |
| PTGI Relating to Others Subscale | 23.0 | 1.1 | 23.2 | 1.1 | .45 | 0.2 | −0.3 to 0.6 | 22.9 | 1.4 | 23.3 | 0.8 | .41 | 0.2 | −0.3 to 0.7 | .37 |
| PTGI Life Appreciation Subscale | 9.8 | 0.5 | 8.7 | 0.5 | .03 | 0.5 | 0.1 to 0.9 | 8.3 | 0.6 | 10.2 | 0.3 | .15 | 0.3 | −0.1 to 0.7 | .09 |
NOTE. Estimates are from general linear models with measurement at 6-month assessment as dependent variable and baseline measurement, group assignment, current medical treatment status, and the interaction between group assignment and current treatment status as independent variables. Means are adjusted for other effects in the model by holding such effects constant at their marginal means. Cohen d effect sizes provide the effects on a pooled standard deviation scale. Results are based on 30 multiply imputed data sets.
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; PCO, Project Connect Online; POMS, Profile of Mood States; PTGI, Posttraumatic Growth Inventory.
Table 3.
Effect Sizes for Outcomes With Significant Interaction Effects, Intent-to-Treat Analysis (N = 88)
| Outcome | Adjusted Cell Mean |
Cohen d Effect Sizes, Differences in Adjusted Cell Means |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A. PCO and Current Medical Treatment (n = 10) | B. Control and Current Medical Treatment (n = 11) | C. PCO and Not in Medical Treatment (n = 36) | D. Control and Not in Medical Treatment (n = 31) | PCO v Control for Participants in Treatment (A v B) | PCO v Control for Participants Not in Treatment (C v D) | Current Treatment v Not in Treatment for Control Group Assignees (B v D) | Current Treatment v Not in Treatment for PCO Group Assignees (A v C) | PCO Assignees in Treatment v Control Assignees Not in Treatment (A v D) | Control Assignees in Treatment v PCO Assignees Not in Treatment (B v C) | |
| CES-D | ||||||||||
| Mean | 10.1 | 20.6 | 9.4 | 10.4 | 1.1 | 0.1 | 1.1 | 0.1 | 0.0 | 1.2 |
| SE | 2.9 | 3.1 | 1.5 | 1.6 | ||||||
| 95% CI | 0.3 to 1.9 | −0.3 to 0.5 | 0.3 to 1.8 | −0.6 to 0.7 | −0.7 to 0.7 | 0.5 to 1.9 | ||||
| P | .006 | .64 | .004 | .84 | .91 | .001 | ||||
| POMS-Vigor | ||||||||||
| Mean | 20.1 | 11.6 | 18.0 | 17.4 | 0.9 | 0.1 | 0.6 | 0.2 | 0.3 | 0.7 |
| SE | 2.8 | 2.6 | 1.3 | 1.5 | ||||||
| 95% CI | 0.2 to 1.7 | −0.4 to 0.5 | 0.0 to 1.3 | −0.5 to 0.9 | −0.4 to 1.0 | 0.1 to 1.3 | ||||
| P | .02 | .78 | .05 | .52 | .43 | .03 | ||||
NOTE. Estimates are from general linear models with measurement at 6-month assessment as dependent variable and baseline measurement, group assignment, current medical treatment status, and the interaction between group assignment and current treatment status as independent variables. Means are adjusted for other effects in the model by holding such effects constant at their marginal means. Cohen d effect sizes provide the effects on a pooled standard deviation scale. Results are based on 30 multiply imputed data sets.
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; PCO, Project Connect Online; POMS, Profile of Mood States.
Fig 2.
Adjusted mean scores on (A, B) depressive symptoms (Center for Epidemiologic Studies Depression Scale [CES-D]) and (C, D) positive mood (Profile of Mood States [POMS]) for patients (A, C) with no current medical treatment and (B, D) in current medical treatment, as a function of intervention (Project Connect Online v waiting-list control) and current medical treatment (yes v no).
PCO produced a significant improvement in positive mood (P = .03), which was qualified by a significant interaction (P = .04; Fig 2). Again, the intervention buffered the effect of being in medical treatment on positive mood. Control participants receiving medical treatment declined in positive mood over time, relative to improved positive mood in the other three groups (all P < .05), which did not differ from each other.
When analyses were repeated on data from the 75 participants retained at 6 months, all statistically significant effects remained (see Appendix). In addition, PCO had a significant effect on negative mood (P = .02) qualified by a significant interaction (P = .03), with the pattern of results mirroring that for depressive symptoms.
Cancer-related psychological adjustment.
In intent-to-treat analyses, PCO produced a significant effect on deepened life appreciation relative to the control condition (P = .03). The interaction was not statistically significant (P = .09), although the means conformed to the same pattern as that for the general adjustment measures. No significant main or interaction effects emerged on cancer-related intrusion or on perceived strengthened relationships.
When analyses were repeated for participants retained at 6 months, the significant effect on PTGI life appreciation remained (P = .002), and the interaction was statistically significant (P = .03). Again, control participants who were receiving medical treatment had significantly lower life appreciation at 6 months compared with the other three groups (all P < .004). In addition, PCO had a marginally significant effect on cancer-related intrusive thoughts and feelings (P = .06), with a decline in cancer-related intrusions in PCO compared with the control condition.
DISCUSSION
PCO demonstrated positive, statistically significant effects on depressive symptoms, positive mood, and life appreciation. These effects are notable in that they were obtained through intent-to-treat analyses of all randomized participants, including six of 46 assigned to PCO who did not attend the workshop, were evident 6 months after participation in a brief intervention, and emerged on both general and cancer-related measures of psychological adjustment. In addition, these effects were moderate to large in magnitude.31 These effects, however, were conditioned by significant interactions, which revealed benefits of PCO particularly (or solely) for women in active medical treatment, most of whom had metastatic disease. Motivations to tell one's story, express cancer-related emotions, garner support, and keep others informed likely are stronger during active medical treatment and the often uneven course of metastatic disease than when treatment is complete. Anecdotally, several longer term survivors stated they participated more for altruistic than personal reasons. Approaches are needed to reduce potential barriers to personal Web site use for patients in active medical treatment (eg, engaging a loved one to manage some Web site functions) and to promote effective use among survivors not in current treatment (eg, address remaining needs for support).
Several limitations of the trial are apparent. This preliminary study had sufficient statistical power to detect only moderate to large effects, and it did not include multiple-test adjustment. In light of trends on some dependent variables, it is possible that PCO has the potential for positive effects on a broader range of general and cancer-related outcomes. The waiting-list control condition did not control for attention. Generalizability of findings to men, individuals with diverse cancer diagnoses, and disadvantaged groups (eg, low education) awaits future research. Effects on outcomes other than self-reported adjustment (eg, return to work) require study, as does sustainability of effects beyond 6 months.
To our knowledge, the current research represents the first experimental study of an innovative intervention with high potential for dissemination. Several questions remain, however, including whether the enhanced benefit for individuals in current medical treatment and/or with metastatic disease is a reproducible effect; potential ethnic/cultural and sex-related variation in effects, in light of nuances in support processes (eg,12,32); effects on other outcomes, including physical health; and comparative effects of this intervention versus other online or in-person approaches.33,34 Such continued research is warranted in light of the promising findings of this preliminary trial.
Supplementary Material
Acknowledgment
We thank the women who took part in the Project Connect Online trial, Kevin Durr and Not Sold Separately, Cheryl Jacobs and Lisa Donley of Breastlink Medical Group, and Lauren Gyllenhammer, Delana Parker, and Orly Weltfreid, who aided in performance of the research.
Appendix
Project Connect Online Intervention Development
Development of the Project Connect Online intervention was informed by two preliminary phases of the research involving semistructured interviews of eight patients with breast cancer who had created personal Web sites to communicate about the cancer experience and focus groups of seven patients with breast cancer to evaluate barriers, facilitators, and preferences for creating personal Web sites. First, semistructured interviews of approximately 60 minutes were conducted with eight women diagnosed with breast cancer who had created their own personal Web sites to communicate with their social network about the cancer experience (phase 1). They were recruited from community clinical oncology practices and listservs for women with cancer (eg, bcmets.org). The principal investigator (A.L.S.) conducted the interviews in person or by telephone with the goals of learning about the intended purposes, benefits, challenges, and consequences associated with Web site use. Second, the researchers (A.L.S. and E.H.T.) conducted two 90-minute focus groups with a total of seven patients with breast cancer from the community medical oncology practice who were interested in the creation of personal Web sites (phase 2). Focus group members discussed perceived barriers, facilitators, and preferences for creating personal Web sites and reviewed sample Web sites volunteered by the phase 1 participants. The researchers prompted suggestions for functions of the Web sites and the format and content of the Project Connect Online intervention.
Review of the recorded phase 1 and 2 sessions by the researchers informed the development of Web site functions and esthetics, as well as intervention content and format. Specifically, suggestions from phase 1 and 2 participants resulted in decisions to (1) offer the intervention to all interested women diagnosed with breast cancer regardless of diagnosis duration or treatment status rather than only to women in active medical treatment (consequently, medical treatment status was examined as a moderator of the intervention's effects); (2) allow attendance at intervention sessions by significant others (eg, partners, offspring); (3) proactively address participants' concerns about Web site use, including perceived pressure to post frequent Web site updates, perceived expectation to adopt a particular tone in journal entries (eg, cheerful, wise, eloquent, positive), discomfort requesting help, perceived responsibility to respond individually to Web site visitors, disappointment arising from the lack of or content of responses from particular individuals in the social network; and (4) provide options for Web site privacy settings (no individual Web site was accessible through general search engines; participants could elect password protection for entry to their Web sites).
Incorporating these decisions, the researchers collaborated with a Web site development firm,17 using the WordPress personal publishing platform,18 to develop a Web site design that allowed for personalization with regard to esthetics and content (eg, Web site template, title, links). Each of the 11 potential WordPress Web site templates selected by the researchers were designed to contain six identical functions (1): a journal (blog) into which photos could be inserted; (2) Web site links chosen by the women, with a list of cancer information Web sites also offered by the researchers (eg, Web sites of the oncology clinic, National Cancer Institute, American Society of Clinical Oncology public site); (3) a How You Can Help page, in which participants could convey actions Web site visitors could undertake for the participant (eg, meal provision, written cards, transportation); (4) choice of privacy settings; (5) instructions for visitors to subscribe to receive automatic notification of updates to the Web site and to post personal messages to the participant; and (6) an online survey to assess visitors' reactions to the Web site (data not reported here). The researchers and Web site development firm created a 48-page manual with written and visual instructions for creating and maintaining the Web sites. In addition, the Web site development firm created online tutorials for managing several Web site functions (eg, adding a link or photo, writing a post, changing templates). The researchers (A.L.S. and E.H.T.) conducted a pilot intervention session with four phase 2 participants to elicit feedback on the online interface, the instructional manual, and session content; slight modifications were made before launching the intervention.
Details of the Multiple Imputation Procedures
The purpose of the multiple imputation was to support an intent-to-treat analysis that included all randomly assigned subjects in the presence of missing outcomes for some participants. Missingness on baseline variables was negligible, whereas outcomes at 6 months were missing for 12 participants (14% of the total of 88 randomly assigned patients) owing to dropout and partially missing data for one participant owing to incomplete assessments.
Missing data were imputed using Markov chain Monte Carlo (MCMC) full-data imputation28 as implemented in the MI procedure in SAS software version 9.3. This method assumes multivariate normal data and uses a Bayesian approach and MCMC to create draws from the posterior distribution of the missing data. Technical details are provided in Schafer28 and in SAS/STAT(R) 9.3 User's Guide, available online at http://support.sas.com/documentation/cdl/en/statug/63,962/HTML/default/viewer.htm#mi_toc.htm. Although the MCMC method assumes multivariate normality, inferences are robust to departures from multivariate normality if the amount of missing information is not large.28
Variables selected for the imputation model included variables in the complete data model and variables correlated with the target missing variables. These included both variables that were collected only at baseline and variables that were collected at all three assessments. Longitudinal data were in the wide format (one row per subject) for purposes of the imputation. Variables included in the imputation model included sociodemographic characteristics (education, age, race/ethnicity, income, employment status), cancer-related and medical variables (diagnosis duration, stage, surgery, chemotherapy, radiotherapy, Herceptin, tamoxifen, whether currently in medical treatment), familial/social network data (marital status, years married, whether had children, whether had children living at home, living parent, living sibling, close living relatives, support group attendance ever, current support group attendance), outcome measures at all available time points, that is, baseline, 1 month, and 6 months (Center for Epidemiologic Studies Depression, Profile of Mood States–Negative Mood, Profile of Mood States–Vigor, Impact of Events Scale [Intrusion], Posttraumatic Growth Inventory Relating to Others Subscale, Posttraumatic Growth Inventory Life Appreciation Subscale), additional psychosocial variables potentially related to outcomes or missingness (seen mental health professional ever, seeing mental health professional now, loneliness, social support, coping self-confidence), and group assignment.
We obtained 30 imputations of missing values after burn-in of 1,000 iterations. The relative efficiency of using 30 imputations rather than an infinite number for fully efficient imputation exceeded 0.993 for all parameters. Convergence was checked by examining trace plots and autocorrelations for parameter values.
The analytic approach was an analysis of covariance, with the 6-month measure as dependent variable and group assignment (Project Connect Online or control group), current medical treatment (radiotherapy, chemotherapy, biologic therapy [endocrine therapy not counted]: yes/no), their interaction, and the baseline measure as independent variables. Main effects were estimated as adjusted mean differences between levels of each factor. When the interaction was significant, we estimated differences in adjusted means among pairs of the four cells defined by the interaction. Because sample sizes among the cells defined by Project Connect versus control condition and current medical treatment (yes/no) were unequal, we used type III sums of squares and the parameters of interest for inference were adjusted means, also known as least square means. Adjusted means are a type of linear combination of regression parameter estimates, and as such, point estimates and SEs can be obtained for them, and the point estimates and SEs obtained from multiply imputed data sets can be combined using Rubin rules.29,30 In SAS, these results can be obtained using the MIXED procedure; syntax is provided at http://support.sas.com/kb/30/698.html and http://support.sas.com/kb/30/715.html. After the 30 complete data sets were analyzed using the MIXED procedure, the MIANALYZE procedure was used to combine the results from the 30 analyses using Rubin rules.
To validate the multiple imputation results, the process was repeated with different starting values for the random number generator, and sensitivity analyses were conducted by repeating the multiple imputation using different model specifications. All procedures gave similar results.
Table A1.
Results of Outcome Analysis for Project Connect Online Based on Data of Participants Retained at 6 Months (n = 75)
| Outcome | Main Effect of Group Assignment |
Main Effect of Current Treatment Status |
Interaction, P | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PCO (n = 40) |
Control (n = 35) |
P | Cohen d | 95% CI | Current Treatment (n = 16) |
Not in Treatment (n = 59) |
P | Cohen d | 95% CI | ||||||
| Adjusted Mean | SE | Adjusted Mean | SE | Adjusted Mean | SE | Adjusted Mean | SE | ||||||||
| CES-D | 9.6 | 1.5 | 16.0 | 1.5 | .004 | 0.7 | 0.2 to 1.2 | 15.6 | 1.9 | 10.0 | 1.0 | .01 | 0.6 | 0.1 to 1.1 | .02 |
| POMS-Negative Mood | 22.1 | 3.8 | 35.1 | 3.9 | .02 | 0.5 | 0.1 to 0.9 | 32.3 | 4.9 | 25.0 | 2.5 | .19 | 0.3 | −0.1 to 0.7 | .03 |
| POMS-Vigor | 18.9 | 1.3 | 14.4 | 1.3 | .02 | 0.5 | 0.1 to 1.0 | 15.6 | 1.6 | 17.7 | 0.8 | .27 | 0.2 | −0.2 to 0.7 | .06 |
| Impact of Event Scale (Intrusion) | 8.4 | 1.1 | 11.5 | 1.2 | .06 | 0.4 | 0.0 to 0.9 | 11.3 | 1.4 | 8.6 | 0.7 | .10 | 0.4 | −0.1 to 0.8 | .90 |
| PTGI Relating to Others Subscale | 23.5 | 1.1 | 21.4 | 1.1 | .18 | 0.3 | −0.1 to 0.7 | 21.7 | 1.4 | 23.1 | 0.7 | .38 | 0.2 | −0.2 to 0.6 | .20 |
| PTGI Life Appreciation Subscale | 10.5 | 0.4 | 8.5 | 0.4 | .002 | 0.6 | 0.2 to 0.9 | 8.9 | 0.5 | 10.1 | 0.3 | .05 | 0.4 | 0.0 to 0.7 | .03 |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; PCO, Project Connect Online; POMS, Profile of Mood States; PTGI, Posttraumatic Growth Inventory.
Table A2.
Effect Sizes for Outcomes With Significant Interaction Effects
| Outcome | Adjusted Cell Mean |
Cohen d Effect Sizes, Differences in Adjusted Cell Means |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A. PCO and Current Treatment (n = 8) | B. Control and Current Treatment (n = 8) | C. PCO and Not in Treatment (n = 32) | D. Control and Not in Treatment (n = 27) | PCO v Control for Participants in Treatment (A v B) | PCO v Control for Participants Not in Treatment (C v D) | Current Treatment v not in Treatment for Control Group Assignees (B v D) | Current Treatment v Not in Treatment for PCO Group Assignees (A v C) | PCO Assignees in Treatment to Control Assignees Not in Treatment (A v D) | Control Assignees in Current Treatment to PCO Assignees Not in Treatment (B v C) | |
| CES-D | ||||||||||
| Mean | 9.8 | 21.4 | 9.3 | 10.6 | 1.3 | 0.1 | 1.2 | 0.0 | 0.1 | 1.3 |
| SE | 2.8 | 2.6 | 1.3 | 1.4 | ||||||
| 95% CI | 0.4 to 2.1 | −0.3 to 0.6 | 0.5 to 1.8 | −0.7 to 0.6 | −0.6 to 0.8 | 0.7 to 1.9 | ||||
| P | .003 | .53 | .0006 | .89 | .80 | .0001 | ||||
| POMS-Negative Mood | ||||||||||
| Mean | 19.6 | 44.9 | 24.5 | 25.4 | 1.0 | 0.0 | 0.7 | 0.2 | 0.2 | 0.8 |
| SE | 6.8 | 6.9 | 3.4 | 3.7 | ||||||
| 95% CI | 0.2 to 1.7 | −0.3 to 0.4 | 0.1 to 1.3 | −0.4 to 0.8 | −0.4 to 0.8 | 0.2 to 1.4 | ||||
| P | .01 | .86 | .02 | .52 | .46 | .01 | ||||
| PTGI Life Appreciation Subscale | ||||||||||
| Mean | 10.6 | 7.2 | 10.4 | 9.8 | 1.0 | 0.2 | 0.8 | 0.0 | 0.2 | 0.9 |
| SE | 0.8 | 0.8 | 0.4 | 0.4 | ||||||
| 95% CI | 0.3 to 1.6 | −0.2 to 0.5 | 0.3 to 1.2 | −0.4 to 0.5 | −0.3 to 0.7 | 0.4 to 1.4 | ||||
| P | .003 | .31 | .004 | .85 | .40 | .0004 | ||||
NOTE. Estimates are from general linear models with measurement at 6-month assessment as dependent variable and baseline measurement, group assignment, current medical treatment status, and the interaction between group assignment and current treatment status as independent variables. Means are adjusted for other effects in the model by holding such effects constant at their marginal means. Cohen's d effect sizes provide the effects on a pooled standard deviation scale.
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; PCO, Project Connect Online; POMS, Profile of Mood States; PTGI, Posttraumatic Growth Inventory.
Footnotes
Supported by funding from Breast Cancer Research Foundation, Susan G. Komen for the Cure Foundation (Grant No. BCTR0707901 to A.L.S.), and National Institutes of Health (Grant No. CA016042 to C.M.C.).
Presented in part at the Annual Meeting of the American Psychosomatic Society, March 9-12, 2011, San Antonio, TX, and the Annual Meeting of the Society of Behavioral Medicine, April 27-30, 2011, Washington, DC.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Annette L. Stanton, John S. Link, James R. Waisman
Provision of study materials or patients: John S. Link, James R. Waisman
Collection and assembly of data: Annette L. Stanton, Elizabeth H. Thompson
Data analysis and interpretation: Annette L. Stanton, Elizabeth H. Thompson, Catherine M. Crespi
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Helgeson VS, Cohen S. Social support and adjustment to cancer: Reconciling descriptive, correlational, and intervention research. Health Psychol. 1996;15:135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 2.Alferi SM, Carver CS, Antoni MH, et al. An exploratory study of social support, distress, and life disruption among low-income Hispanic women under treatment for early stage breast cancer. Health Psychol. 2001;20:41–46. doi: 10.1037//0278-6133.20.1.41. [DOI] [PubMed] [Google Scholar]
- 3.Nosarti C, Roberts JV, Crayford T, et al. Early psychological adjustment in breast cancer patients: A prospective study. J Psychosom Res. 2002;53:1123–1130. doi: 10.1016/s0022-3999(02)00350-1. [DOI] [PubMed] [Google Scholar]
- 4.Cordova MJ, Cunningham LL, Carlson CR, et al. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychol. 2001;20:176–185. [PubMed] [Google Scholar]
- 5.Widows MR, Jacobsen PB, Fields KK. Relation of psychological vulnerability factors to posttraumatic stress disorder symptomatology in bone marrow transplant recipients. Psychosom Med. 2000;62:873–882. doi: 10.1097/00006842-200011000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Lutgendorf SK, Sood AK. Biobehavioral factors and cancer progression: Physiological pathways and mechanisms. Psychosom Med. 2011;73:724–730. doi: 10.1097/PSY.0b013e318235be76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt JE, Andrykowski MA. The role of social and dispositional variables associated with emotional processing in adjustment to breast cancer: An internet-based study. Health Psychol. 2004;23:259–266. doi: 10.1037/0278-6133.23.3.259. [DOI] [PubMed] [Google Scholar]
- 8.Howsepian BA, Merluzzi TV. Religious beliefs, social support, self-efficacy and adjustment to cancer. Psychooncology. 2009;18:1069–1079. doi: 10.1002/pon.1442. [DOI] [PubMed] [Google Scholar]
- 9.Stanton AL, Danoff-Burg S, Cameron CL, et al. Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. J Consult Clin Psychol. 2000;68:875–882. [PubMed] [Google Scholar]
- 10.Helgeson VS, Cohen S, Schulz R, et al. Group support interventions for women with breast cancer: Who benefits from what? Health Psychol. 2000;19:107–114. doi: 10.1037//0278-6133.19.2.107. [DOI] [PubMed] [Google Scholar]
- 11.Manne S, Ostroff J, Sherman M, et al. Buffering effects of family and friend support on associations between partner unsupportive behaviors and coping among women with breast cancer. J Soc Person Relat. 2003;20:771–792. [Google Scholar]
- 12.Wellisch D, Kagawa-Singer M, Reid SL, et al. An exploratory study of social support: A cross-cultural comparison of Chinese-, Japanese-, and Anglo-American breast cancer patients. Psychooncology. 1999;8:207–219. doi: 10.1002/(SICI)1099-1611(199905/06)8:3<207::AID-PON357>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 13.Marcus AC, Garrett KM, Kulchak-Rahm A, et al. Telephone counseling in psychosocial oncology: A report from the Cancer Information and Counseling Line. Patient Educ Couns. 2002;46:267–275. doi: 10.1016/s0738-3991(01)00163-x. [DOI] [PubMed] [Google Scholar]
- 14.Caring Bridge. www.caringbridge.org.
- 15.MyLifeLine.org Cancer Foundation. MyLifeLine. www.mylifeline.org.
- 16.Høybye MT, Johansen C, Tjørnhøj-Thomsen T. Online interaction. Effects of storytelling in an internet breast cancer support group. Psychooncology. 2005;14:211–220. doi: 10.1002/pon.837. [DOI] [PubMed] [Google Scholar]
- 17.Not Sold Separately. www.notsoldseparately.com.
- 18.WordPress. www.wordpress.org.
- 19.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 20.McNair DM, Lorr M, Droppleman LF. EITS Manual for the Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 21.Sears SR, Stanton AL, Danoff-Burg S. The Yellow Brick Road and the Emerald City: Benefit-finding, positive reappraisal coping, and posttraumatic growth in women with early-stage breast cancer. Health Psychol. 2003;22:487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- 22.Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psychooncology. 2002;11:93–102. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- 23.Stanton AL, Danoff-Burg S, Sworowski LA, et al. Randomized, controlled trial of written emotional expression and benefit-finding in breast cancer patients. J Clin Oncol. 2002;20:4160–4168. doi: 10.1200/JCO.2002.08.521. [DOI] [PubMed] [Google Scholar]
- 24.Stanton AL, Estes MA, Estes NC, et al. Treatment decision making and adjustment to breast cancer: A longitudinal study. J Consult Clin Psychol. 1998;66:313–322. doi: 10.1037//0022-006x.66.2.313. [DOI] [PubMed] [Google Scholar]
- 25.Stanton AL, Snider PR. Coping with a breast cancer diagnosis: A prospective study. Health Psychol. 1993;12:16–23. doi: 10.1037//0278-6133.12.1.16. [DOI] [PubMed] [Google Scholar]
- 26.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J Traumatic Stress. 1996;9:455–472. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 28.Schafer JL. New York, NY: Chapman and Hall; 1997. Analysis of Incomplete Multivariate Data. [Google Scholar]
- 29.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. [Google Scholar]
- 30.Rubin DB. New York, NY: John Wiley & Sons; 1987. Multiple Imputation for Nonresponse in Surveys. [Google Scholar]
- 31.Cohen J. ed 2. Hillsdale, NJ: Erlbaum; 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 32.Taylor SE, Sherman DK, Kim HS, et al. Culture and social support: Who seeks it and why? J Pers Soc Psychol. 2004;87:354–362. doi: 10.1037/0022-3514.87.3.354. [DOI] [PubMed] [Google Scholar]
- 33.Leykin Y, Thekdi SM, Shumay DM, et al. Internet interventions for improving psychological well-being in psycho-oncology: Review and recommendations. Psychooncology. 2012;21:1016–1025. doi: 10.1002/pon.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hong Y, Peña-Purcell NC, Ory MG. Outcomes of online support and resources for cancer survivors: A systematic literature review. Patient Educ Couns. 2012;86:288–296. doi: 10.1016/j.pec.2011.06.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.