Abstract
A 48-year-old male patient underwent cardiac resynchronization therapy defibrillator implantation, and he was found to have atresia of the coronary sinus ostium with venous drainage occurring via a persistent left-sided superior vena cava, which was connected to the right-sided superior vena cava by the innominate vein. This is a rare benign cardiac anomaly that can pose problems when the coronary sinus needs to be cannulated. To identify the course of the coronary sinus, a coronary angiogram can be performed with attention directed to the venous phase of the angiogram. Although the technical difficulty of coronary sinus cannulation increases, various catheters, wires, and delivery systems can be utilized and this anomaly does not usually prevent successful left ventricular lead placement in cardiac resynchronization therapy via a left-sided superior vena cava approach. There however needs to be consideration regarding caliber of the left-sided superior vena cava being sufficiently large to avoid compromise of venous drainage after lead insertion.
Keywords: coronary sinus, atresia, left-sided superior vena cava, CRT
Coronary sinus ostial atresia is rare and is associated with anomalous drainage of the coronary sinus via a persistent left-sided superior vena cava1 or via venous collateral pathways to the right or left atrium. Although coronary sinus ostial atresia with a persistent left-sided superior vena cava is a benign anomaly,2 it becomes significant in situations where the coronary sinus needs to be cannulated or during cardiac surgery.3
We report a case of coronary sinus ostial atresia with persistent left-sided superior vena cava that necessitated coronary sinus lead insertion via a left-sided superior vena cava approach for cardiac resynchronization therapy.
Case Report
A 48-year-old male patient with idiopathic dilated cardiomyopathy, ejection fraction of 15% underwent cardiac resynchronization therapy defibrillator device insertion. Implantation of the bipolar atrial lead (St. Jude Medical Tendril 52 cm; St. Jude Medical, St. Paul, MN) and the ventricular lead (St. Jude Medical Durata 58 cm; St. Jude Medical, St. Paul, MN) were uneventful via the left subclavian approach. The coronary sinus could not be cannulated from the right atrium despite multiple attempts. A coronary angiogram was performed to delineate the coronary sinus, which was found to be atretic at the ostium. The coronary sinus drainage occurred via a persistent left-sided superior vena cava, which was connected to the right-sided superior vena cava by the innominate vein. There was no flow of contrast directly to the right atrium from the coronary sinus (Figs. 1 and 2)
Fig. 1.
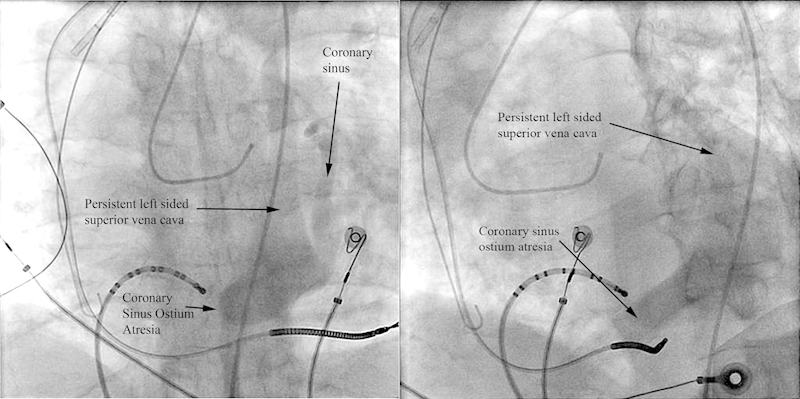
Venous phase of the left coronary angiogram from the right anterior oblique view (left) and left anterior oblique view (right). The coronary sinus is dilated. There is no flow of contrast from the coronary sinus directly to the right atrium and drains via a persistent left-sided superior vena cava.
Fig. 2.
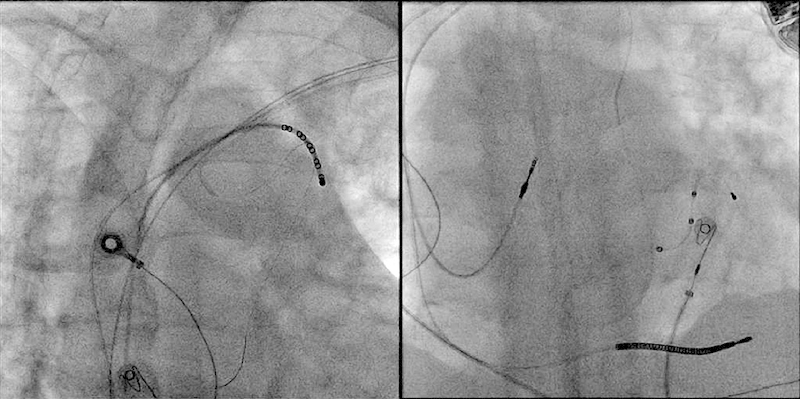
Cannulation of the persistent left-sided superior vena cava with a Judkins right coronary catheter from the left subclavian vein (left) and implantation of the left ventricular lead in the coronary sinus via the persistent left-sided superior vena cava (right).
The left-sided superior vena cava was cannulated using a Judkins right coronary catheter, and the left ventricular lead (St. Jude Quartet 86 cm; St. Jude Medical, St. Paul, MN) was positioned in a posterior branch of the coronary sinus. Thresholds and impedance readings were acceptable. The leads were connected to a Promote Quadra 3239-4OQ (St. Jude Medical, St. Paul, MN) pulse generator.
Discussion
Failure of coronary sinus cannulation occurs in 5 to 10%4 of cardiac procedures, and coronary sinus atresia is a rare cause of this.
During embryological development, the sinus venosus differentiates into right and left horns. The transverse segment of the sinus venosus shifts rightward following the separation of the left horn of the sinus venosus and the left atrium. This shift pulls the left horn of the sinus venosus along the posterior atrioventricular groove. As the residual left horn of the sinus venosus progressively undergoes degeneration, it forms the coronary sinus that drains the cardiac veins.5
Coronary sinus atresia is an anomaly described to occur at an incidence of 0.1%1 to 0.25%,6 and usually consists of a membranous occlusion at the ostium (with or without an interruption along the course of the coronary sinus),2 which prevents direct venous drainage from the coronary sinus to the right atrium. Venous return occurs via anomalous pathways and is commonly associated with a persistent left-sided superior vena cava.7 In such a situation, the coronary sinus drains retrogradely into the persistent left-sided superior vena cava, the innominate vein, then to the right-sided superior vena cava, and finally into the right atrium. Variations of this connection have been described: left-sided superior vena cava drainage to the right-sided superior vena cava via the hemiazygos vein or through a hemiazygos-azygos venous connection.8 Other instances of coronary sinus atresia have been reported to be associated with anomalous drainage via an unroofed coronary sinus into the left atrium, coronary artery fistulae, or by anomalous right atrial anastomoses.1
The embryological basis for the persistent left-sided superior vena cava is described as follows: The right and left common cardinal veins receive blood from the superior cardinal veins before entering the sinus venosus. At the 8th week of gestation, an anastomosis develops between the right and left common cardinal veins leading to the formation of the brachiocephalic vein. The portion of the left superior cardinal vein caudal to the brachiocephalic vein anastomosis involutes to become the ligament of Marshall. Failure of involution of this portion of the left superior cardinal vein leads to a persistent left-sided superior vena cava.5,9,10
Patients with coronary sinus ostial atresia are commonly asymptomatic and this anomaly is usually only diagnosed during postmortem examinations because of unobstructed venous drainage via anomalous pathways previously described.11 It however comes to attention when patients undergo invasive electrophysiological procedures that require cannulation of the coronary sinus, e.g., electrophysiologic studies12 or coronary sinus lead placement for biventricular pacing.
To identify the course of the coronary sinus, a coronary angiogram can be performed with attention directed at the venous phase of the angiogram. Alternatively, a multidetector computed tomography or magnetic resonance imaging (if leads already implanted are MRI conditional) of the heart can be performed following failure of coronary sinus intubation to delineate the coronary sinus anatomy. This also allows detection of concomitant abnormalities, such as, coronary artery fistulas or unroofed coronary sinus with left-to-right shunting. Approximately 53% of patients with coronary sinus atresia have concomitant coronary artery fistulae and coronary sinus unroofings.1
Coronary sinus ostial atresia together with a persistent left-sided superior vena cava is of great importance when cardiac surgery is performed. As the left-sided superior vena cava, in the absence of other anomalous venous pathways, can be the only conduit for venous drainage, ligation of the left-sided superior vena cava (in the Fontan or Bidirectional Glenn procedure) will result in venous congestion and myocardial ischemia.13 The pathophysiology of this has been suggested to be because of elevation of the transcapillary pressure with reduced myocardial perfusion pressure from the coronary arteries or because of direct myocardial injury from increased pressure.14
Similarly, because the left-sided superior vena cava can be small,15 during left ventricular lead implantation in the coronary sinus via the left-sided superior vena cava, the size of the left-sided superior vena cava should be assessed with a venogram to ensure that the vessel is sufficiently large to allow the lead to traverse it without causing any compromise in venous flow. Manipulation of catheters and guidewires through the venous system can also potentially cause trauma and thrombosis to the left-sided superior vena cava. In our patient, the left-sided superior vena cava caliber was sufficiently large and the left ventricular lead in situ would not have caused any venous flow compromise.
There have been few reports of coronary sinus thrombosis arising from central venous catheterization, pacemaker wire placement, cardiac surgery, or associated with atrial fibrillation or malignancy. Until now, to the best of our knowledge, there have been two cases of coronary sinus thrombosis in patients with coronary sinus atresia and persistent left-sided superior vena cava occurring spontaneously, both of which were entirely asymptomatic.3 An enlarged coronary sinus is observed in patients with coronary sinus ostium atresia,1 and it is not inconceivable that this, together with manipulation and lead insertion, may theoretically predispose to a higher risk of coronary sinus thrombosis.16 However at this point of time, there is insufficient evidence to suggest need for additional thromboprophylaxis in such patients for this indication alone.
It is technically more challenging to insert the left ventricular lead via the left-sided superior vena cava, which usually requires the use of multiple catheters and angioplasty wires, and by adopting an interventional approach to lead implantation, chances of success can be increased.17
An epicardial left ventricular lead is an alternative,18 which requires a thoracotomy or thoracoscopy under anesthesia, but it is an option when venous anatomy is not favorable for transvenous implantation.
Conclusion
Coronary sinus atresia with a persistent left-sided superior vena cava is a rare condition that usually comes to attention when there is failure to cannulate the coronary sinus from the right atrium. A coronary angiogram can be performed on table to confirm coronary sinus atresia and delineate cardiac venous anatomy. Although it increases the technical difficulty of coronary sinus cannulation, it does not commonly prevent successful left ventricular lead placement in cardiac resynchronization therapy.
Disclosures
None.
References
- 1.Shum J S, Kim S M, Choe Y H. Multidetector CT and MRI of ostial atresia of the coronary sinus, associated collateral venous pathways and cardiac anomalies. Clin Radiol. 2012;67(12):e47–e52. doi: 10.1016/j.crad.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Santoscoy R, Walters H L III, Ross R D, Lyons J M, Hakimi M. Coronary sinus ostial atresia with persistent left superior vena cava. Ann Thorac Surg. 1996;61(3):879–882. doi: 10.1016/0003-4975(95)01137-4. [DOI] [PubMed] [Google Scholar]
- 3.Stevenhagen J, Meijer A, Bracke F A, van Gelder B M. Coronary sinus atresia and persistent left superior vena cava with the presence of thrombus complicating implantation of a left ventricular pacing lead. Europace. 2007;10(3):384–387. doi: 10.1093/europace/eum291. [DOI] [PubMed] [Google Scholar]
- 4.Mak G S, Hill A J, Moisiuc F, Krishnan S C. Variations in Thebesian valve anatomy and coronary sinus ostium: implications for invasive electrophysiology procedures. Europace. 2009;11(9):1188–1192. doi: 10.1093/europace/eup179. [DOI] [PubMed] [Google Scholar]
- 5.Hugh D. Allen, David J. Driscoll. Moss and Adams' Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adult 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008 [Google Scholar]
- 6.Caetano A G, Ribeiro T C, Filho O AR, Fazan V PS. Atresia of the coronary sinus ostium to the right atrium with a persistent left superior vena cava. Int J Morphol. 2009;27(3):771–776. [Google Scholar]
- 7.Kim C, Goo H W, Yu J J, Yun T J. Coronary sinus ostial atresia with persistent left superior vena cava demonstrated on cardiac CT in an infant with a functional single ventricle. Pediatr Radiol. 2012;42(6):761–763. doi: 10.1007/s00247-011-2258-1. [DOI] [PubMed] [Google Scholar]
- 8.von Lüdinghausen M, Lechleuthner A. Atresia of the right atrial ostium of the coronary sinus. Acta Anat (Basel) 1988;131(1):81–83. doi: 10.1159/000146490. [DOI] [PubMed] [Google Scholar]
- 9.Habib A, Lachman N, Christensen K N, Asirvatham S J. The anatomy of the coronary sinus venous system for the cardiac electrophysiologist. Europace. 2009;11 05:v15–v21. doi: 10.1093/europace/eup270. [DOI] [PubMed] [Google Scholar]
- 10.Moore K Persaud T Before We Are Born: Essentials of Embryology and Birth Defects 7th ed. Philadelphia, PA: Saunders Elsevier; 2003 [Google Scholar]
- 11.Jha N K, Gogna A, Tan T H, Wong K Y, Shankar S. Atresia of coronary sinus ostium with retrograde drainage via persistent left superior vena cava. Ann Thorac Surg. 2003;76(6):2091–2092. doi: 10.1016/s0003-4975(03)01040-3. [DOI] [PubMed] [Google Scholar]
- 12.Kim J, Kim J H, Chun K J, Hong T J, Shin Y W. Left-sided accessory pathway with ostial atresia of the coronary sinus: a case report. Pacing Clin Electrophysiol. 2008;31(1):129–130. doi: 10.1111/j.1540-8159.2007.00938.x. [DOI] [PubMed] [Google Scholar]
- 13.Yokota M, Kyoku I, Kitano M. et al. Atresia of the coronary sinus orifice. Fatal outcome after intraoperative division of the drainage left superior vena cava. J Thorac Cardiovasc Surg. 1989;98(1):30–32. [PubMed] [Google Scholar]
- 14.Yeo K K, Davenport J, Raff G, Laird J R. Life-threatening coronary sinus thrombosis following catheter ablation: case report and review of literature. Cardiovasc Revasc Med. 2010;11(4):e1–e5. doi: 10.1016/j.carrev.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Gerlis L M, Gibbs J L, Williams G J, Thomas G D. Coronary sinus orifice atresia and persistent left superior vena cava. A report of two cases, one associated with atypical coronary artery thrombosis. Br Heart J. 1984;52(6):648–653. doi: 10.1136/hrt.52.6.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morani G, Bergamini C, Toniolo M, Vassanelli C. How many leads through persistent left superior vein cava and coronary sinus? J Electrocardiol. 2010;43(6):663–666. doi: 10.1016/j.jelectrocard.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 17.Worley S J, Gohn D C, Pulliam R W. Interventional approach to CRT in a patient with drainage of the superior vena cava into the coronary sinus. Pacing Clin Electrophysiol. 2008;31(4):506–508. doi: 10.1111/j.1540-8159.2008.01023.x. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura T, Otomo K, Kawai S, Igawa O. Coronary sinus atresia complicating cardiac resynchronization therapy. J Cardiovasc Electrophysiol. 2010;21(10):1178. doi: 10.1111/j.1540-8167.2010.01810.x. [DOI] [PubMed] [Google Scholar]


