Abstract
Smartphone apps can provide real-time, interactive self-management aid to individuals with diabetes. It is currently unclear whether existing diabetes self-management apps follow evidence-based guidelines. The purpose of this study was to evaluate the extent to which existing diabetes self-management apps address the seven self-management behaviors recommended by the American Association of Diabetes Educators (the AADE7™). The term “diabetes” identified relevant self-management apps via the Apple App Store search engine in March 2012. Ratings were based on app descriptions and downloads. Chi-square analyses assessed differences in apps based on developer type. Apps promoted a median of two AADE7™ skills. Overall reliability between description and download ratings was good (kappa = .66). Reliability of individual skills was variable (kappa = .25 to .91). Most diabetes apps do not conform to evidence-based recommendations, and future app reviews would benefit from testing app performance. Future apps may also benefit from theory-based designs.
Keywords: Diabetes, mHealth, Apps, Self-management, Smartphone, Technology
More than 25 million American adults over the age of 20 have diabetes, and its prevalence is on the rise [1]. Diabetes represents a major public health concern, as its complications, which include cardiovascular disease, kidney failure, blindness and amputations, greatly affect patients’ health, quality of life, and ability to be active members of society. Furthermore, caring for patients with diabetes places a major strain on an already overtaxed healthcare system, costing USA’s healthcare system US$174 billion in 2007 [2]. As with most forms of chronic illness, patients with diabetes shoulder the majority of the treatment burden, which includes lifestyle changes (e.g., diet and physical activity) and medication. Also similar to most chronic illnesses, adherence to diabetes treatment regimens is poor [3, 4] with some estimates placing it as low as 50 % [5]. Low adherence rates are troubling as non-adherence is associated with worse health outcomes, including mortality [6].
Leveraging mobile technologies may be one way to improve patient adherence to diabetes self-management regimens. Lim and colleagues [7] compared the effects of three diabetes self-management regimens: (1) care as usual, (2) self-monitoring of blood glucose (SMBG) with standard blood glucose meters, and (3) “U-Health,” which consisted of SMBG with Bluetooth-enabled meters linked to a cell phone text messaging service that provided real time self-management prompts based on SMBG results. After 3 months of treatment, glycemic control improved in both the standard SMBG and U-Health conditions, but only participants using U-Health maintained those improvements at 6 months. These results are especially promising in light of the fact that technological advancements have made U-Health and other diabetes self-management applications (apps) available to any patient who has access to a smartphone.
Indeed, as of April 22, 2012, Apple’s iPhone, one of the best selling smartphones in the USA [8], provided access to almost 8,000 health-related apps. Given that 80 % of Internet users report searching for health information online [9] and that 30 % of American adults reported downloading health apps in 2011 [10], it is critical for health care providers and the public to be aware of which apps promote empirically supported health behavior change techniques. Unfortunately, while Apple’s App Store includes apps with empirical support (e.g., U-Health), it does not provide users with a way to search for empirically supported apps. Further, while mobile application management companies such as Happtique.com may soon provide catalogs of evidenced-based apps, app certification standards have not been finalized and such catalogs are not easily accessed by consumers through Apple’s App Store. The limited research on this topic has shown, for example, that the majority of apps for weight loss are not based on empirically supported techniques [11] nor are the majority of apps for diabetes self-management that include SMBG [12].
Building upon previous work by Breton et al. [11] and Chomutare [12], the goal of the current study was to describe and review iPhone apps that were promoted as diabetes self-management tools and available as of March 2012 in Apple’s App Store. To describe apps, information was collected on price, user ratings, developer type, Bluetooth compatibility, and social networking capabilities from individual apps’ App Store description pages. These description pages were also reviewed to determine whether apps promoted any of the seven self-management behaviors recommended by the American Association of Diabetes Educators (AADE7™) [13]. The AADE7™ provide an evidence-based framework for diabetes self-management and include: (1) healthy eating, (2) being active, (3) monitoring, (4) taking medications, (5) problem solving, (6) reducing risks, and (7) healthy coping. As information from description pages may differ from actual app content, we extended previous app review methodology [11] by downloading, using, and rating 10 % of eligible apps to assess the reliability between ratings of the AADE7™ behaviors based on description pages and ratings based on actual use.
Given the lack of empirically based apps for SMBG and weight loss, it was hypothesized that most apps would not adhere to the majority of the AADE7™ Self-Care Behaviors. It was also hypothesized that apps developed by non-profit, education, or government institutions would promote more AADE7™ behaviors and have higher user ratings than those made by other developers, as non-profit, education, or government institutions may be more likely than other app programmers to be aware of existing guidelines, which would both increase the number of skills promoted and potentially increase the face validity of apps. Further, it was hypothesized that apps developed by non-profit, education, or government institutions would cost the least, as they were not developed for profit. Finally, it was hypothesized that there would be good reliability between description-based and download-based ratings of the AADE7™ behaviors.
METHODS
The search for and analysis of diabetes self-management iPhone apps was based in part on previous reviews of mHealth apps [e.g., 11]. Apps were identified by entering the term “diabetes” in the Apple App Store search engine on March 17, 2012. iPhone apps were chosen, as Apple products may be used more often than Android products in medical settings [14]. Content and descriptive analyses were used to report on the apps’ specific characteristics. Chi-square analyses were used to compare apps created by non-profit, education, or government institutions and other developers. The study was exempt from review by the authors’ institutional review board, as all information was available and retrieved from the public domain.
Search protocol
The protocol by Breton et al. [11] served as the model for diabetes self-management app identification. On March 17, 2012, the authors (JYB, VMY, JY) logged onto the Apple App Store, at www.apple.com/itunes, and entered the term “diabetes” in the store’s search engine. A total of 411 apps were identified. Each author assumed responsibility for downloading the description pages for one third of the apps. The description page for each app included an overall description of the app and its features, user ratings, customer reviews, and visual displays of the app. Description pages were saved as web archive files on the authors’ MacBook Pros and served as the basis for this review.
In order to choose apps for the reliability screen, the names of eligible apps were placed individually in rows in alphabetical order, and each row was assigned a non-repeating integer. The Random Integer Set Generator from www.random.org was used to identify a random set of integers that represented the rows of the 10 % of apps to download and review for reliability. These apps were downloaded and reviewed in September 2012.
App review
Each author reviewed the app descriptions she downloaded and one other author’s apps, such that each of the 411 identified apps was reviewed twice. Initial review of descriptions occurred independently. Once all apps were reviewed, the two authors responsible for a particular app met to verify and discuss ratings. In the case of any discrepant ratings, the two authors together re-reviewed the app to come to a consensus rating. If a consensus could not be reached, the first author (JYB) made a final decision. Consensus between the two authors responsible for a particular app was reached for over 99 % of ratings and JYB made a final decision in five cases. The specifics of the app review process are described below.
Review of downloaded apps for reliability was conducted by JYB and JY in a similar manner 5 months after the initial review of description pages. To reduce potential bias, the initial ratings of app descriptions were not referenced during this process. Each author downloaded all of the randomly selected apps and independently reviewed each app. In order to ensure that all app features were explored, the authors clicked all possible links and entered data into all possible fields. Once all apps were reviewed, the authors met to verify and discuss ratings. After re-review of discrepant ratings, consensus was met for all ratings.
Applicability
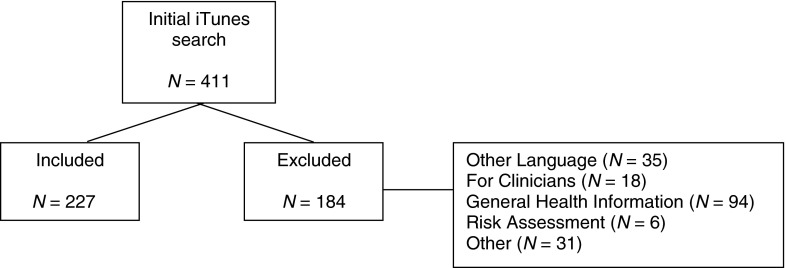
Applicability was broadly defined as any app intended to help an individual manage his or her diabetes and its complications. Apps that were produced in languages other than English, served as medical guides specifically for clinicians, or offered general health and/or nutrition information were considered not applicable (Fig. 1).
Fig 1.
Consort diagram of app inclusion
Adherence to AADE7™ guidelines
Apps were rated on a binary scale (0 = No, 1 = Yes) according to whether they adhered to or promoted each of the seven behaviors considered essential by the AADE for diabetes self-management: (1) healthy eating, (2) being active, (3) monitoring, (4) taking medications, (5) problem solving, (6) reducing risks, and (7) healthy coping. Descriptions provided by the AADE were used as the basis of ratings and can be found at http://www.diabeteseducator.org/ProfessionalResources/AADE7/. Specifically, healthy eating was rated as “1” if the app included information on diabetic-friendly food and meals or provided a means of tracking food and nutrition. Being active was rated as “1” if the app included exercise recommendations or an activity tracker. Monitoring, as described by the AADE7™, differs from the general definition of self-monitoring that may be familiar to many psychologists (e.g., keeping track of meals or behaviors) as it refers only to the monitoring of biomarkers. As such, for the purposes of reviewing AADE7™-defined monitoring, monitoring was rated as “1” if the app allowed users to save and track their blood glucose levels, weight, blood pressure, and/or urine ketones over time. Taking medications was rated as “1” if the app allowed users to save and track their medication dosages or if the app provided reminders for taking medication. Problem solving was rated as “1” if the app met the broad AADE7™ guidelines of helping users make decisions about their self-management and/or promoted the problem-solving steps commonly taught in evidence-based cognitive behavioral therapy [e.g., 15]. Examples of problem solving include color-coded charts or graphs that alerted users to out-of-range blood glucose levels, providing feedback to individuals on the effectiveness of their problem solving solution. Reducing risks was rated as “1” if the app provided education or the ability to track complications of diabetes (e.g., heart rate, blood pressure, foot injuries). Healthy coping was rated as “1” if the app provided information regarding self-care and seeking support.
Additional features
The following information was captured directly from the web archive descriptions: developer name, app price, date of last update, rating (from 1 to 5 stars, per iTunes, with 1 indicating customers “hate it” and 5 indicating customers think “it’s great”); number of ratings for the most recent app version; and the overall rating and number of ratings for all app versions. In addition to capturing developer name, the following developer codes were created to review the different types of app developers: (1) individual, (2) health industry, (3) website, (4) general app developer, (5) health app developer, and (6) non-profit, education, or government institution.
The apps were also rated on a binary scale (0 = No, 1 = Yes) according to whether they were interactive: to be used in conjunction with a website, to be used in conjunction with a Bluetooth-enabled blood glucose meter, allowed for social networking, and were specific to diabetes. Specifically, apps were considered interactive if they allowed the user to do more than passive searching or entering of data (e.g., if they allowed for tracking progress over time). Apps were considered to be used in conjunction with a website if the app provided additional features on a specific website. Apps were considered to be used in conjunction with a Bluetooth-enabled meter if such a meter could be synced with the app. Apps were considered as allowing for social networking if they provided links to Facebook, Twitter, or similar forums. Finally, apps were considered specific to diabetes if “diabetes” came up in the web archive description. In order to simulate the way patients and/or providers might use the app store, we included all apps listed under the search term “diabetes,” which resulted in both diabetes-specific and broader health-related apps.
Statistical analyses
Descriptive statistics of all variables and chi-square analyses to assess associations between AADE7™ behaviors and developer type were run with IBM SPSS Statistics 19 (2010). Given the small sample size of apps developed by non-profit, education, and government institutions, a median split was used in chi-square analyses of differences in the number of AADE7™ behaviors promoted by different developer types. Tests of reliability between description-based and download-based ratings of the AADE7™ behaviors were conducted with Cohen’s Kappa using the guidelines described by Cicchetti [15]: 0.75–1.00 = excellent; 0.60–0.74 = good; 0.40–0.59 = fair; and <0.40 = poor.
RESULTS
As seen in Fig. 1, 227 out of 411 apps were eligible for review. Among the 184 apps ineligible for review, the most common reasons for exclusion were that the apps provided general health information rather than diabetes-specific information (N = 94; 51.1 %) and that the apps were produced in languages other than English (N = 35; 19.0 %). Descriptive statistics of the remaining 227 apps were examined to investigate adherence to the AADE7™ guidelines and the additional features of interest. In general, the number of AADE7™ skills referenced in each app was low (Mdn = 2; range, 0–6), and the data were positively skewed (Table 1). No app promoted all seven skills recommended by the AADE7™. As seen in Table 2, apps most commonly featured the AADE7™ skills of healthy eating (44.9 %), monitoring of the biomarkers specified by the AADE7™ (48 %), and medication (46.7 %). The least commonly featured AADE7™ skill was healthy coping (5.7 %). Of the additional features catalogued, the most common was insulin delivery (39.2 %) and the least common was Bluetooth compatible monitoring (1.8 %).
Table 1.
Number of AADE7™ skills by developer type
| Number of AADE7™ skills | Developer type (N; %) | ||||||
|---|---|---|---|---|---|---|---|
| Individual (27; 11.9 %) | Health industry (23; 10.1 %) | Website (1; 0.4 %) | General developer (92; 40.5 %) | Health developer (71; 31.3 %) | Non-profit, education, or government (13; 5.7 %) | All (227; 100 %) | |
| 0 | 1 | 2 | 0 | 16 | 10 | 4 | 33 (14.5 %) |
| 1 | 9 | 10 | 0 | 38 | 14 | 4 | 75 (33.0 %) |
| 2 | 9 | 2 | 1 | 15 | 8 | 0 | 35 (15.4 %) |
| 3 | 5 | 4 | 0 | 9 | 11 | 3 | 32 (14.1 %) |
| 4 | 1 | 2 | 0 | 10 | 11 | 0 | 24 (10.6 %) |
| 5 | 1 | 2 | 0 | 4 | 16 | 2 | 25(11.0 %) |
| 6 | 1 | 1 | 0 | 0 | 1 | 0 | 3 (1.3 %) |
Table 2.
Number of apps promoting each AADE7™ guideline and other diabetes self-management tools
| AADE7™ guideline | N (%) |
| Healthy eating | 102 (44.9 %) |
| Being active | 56 (24.7 %) |
| Self-monitoring | 109 (48.0 %) |
| Medication | 106 (46.7 %) |
| Problem solving | 67 (29.5 %) |
| Reducing risks | 27 (11.9 %) |
| Healthy coping | 13 (5.7 %) |
| Other self-management tools | |
| Insulin delivery | 89 (39.2 %) |
| Companion website | 20 (8.8 %) |
| Bluetooth compatible monitoring | 4 (1.8 %) |
| Social networking | 20 (8.8 %) |
The number of skills referenced in each app is listed by developer type in Table 1. Apps were most frequently released by general developers (40.5 %) and health-specific developers (31.3 %). The results of the chi-square test to examine whether apps developed by non-profit, education, or government institutions were more likely to present at least the average number of AADE7™ skills (i.e., two or more skills), was not significant. Only five (38.5 %) out of 13 apps developed by non-profit, education, or government institutions referenced two or more AADE7™ skills. Roughly half (56.3 %) of the apps created by other developers referenced two or more AADE7™ skills.
Price was heavily skewed such that app costs were low. The median price for all diabetes self-management apps was US$0.99 and, most commonly, apps were free. The most expensive app was US$24.99. Chi-square analyses indicated that apps developed by non-profit, education, or government institutions (Mdn = $0; range, US$0–24.99) were significantly less expensive than apps developed by other groups (Mdn = $.99, range, US$0–19.99), χ2 (1, N = 227)= 59.18, p < .001).Information on ratings was present for approximately half of the 227 apps relevant to diabetes self-management (47.14 %). Possible ratings ranged from 1 star (“hate it”) to 5 stars (“it’s great”). Ratings and number of ratings for the most recent and overall app versions were similar. Most ratings were 3 stars, indicating “it’s okay,” for the most recent version (M = 3.20, SD = 1.07) and overall (M = 3.13, SD = 1.05). The number of reviews per app ranged widely for the most recent version (5–1,520) and overall (5–4,500) and were positively skewed. The median number of reviews was 13 for the most recent version and 19 for the overall app. Ratings (overall and most current) for apps developed by non-profit, education, or government institutions were not significantly different from other developer types.
Reliability
Of the 23 apps chosen for download and full review in September 2012, two were no longer available and three had been updated since March 2012. These apps were considered ineligible for reliability review, and the five apps in the rows directly succeeding the ineligible apps were chosen for review instead. One of these apps was no longer available and two had been updated since March 2012. These apps were also considered ineligible for reliability review, and the three apps in the rows directly succeeding the ineligible apps were chosen for review. All three apps were eligible.
Table 3 provides a comparison of the additional features of all 227 apps and the 23 downloaded apps. There were no statistically significant differences between the two groups in terms of developer type, price, ratings, or number of reviews, indicating that the 23 downloaded apps were representative of all available and eligible self-management apps.
Table 3.
Comparison of additional features of all reviewed apps (N = 227) and downloaded apps (N = 23)
| Feature | All reviewed apps | Downloaded apps | Significance |
|---|---|---|---|
| Developer type | N (%) | N (%) | |
| Individual | 27 (11.9 %) | 0 (0 %) | p = .513 |
| Health industry | 23 (10.1 %) | 4 (17.4 %) | |
| Website | 1 (0.4 %) | 0 (0 %) | |
| General developer | 92 (40.5 %) | 8 (34.8 %) | |
| Health developer | 71 (31.3 %) | 10 (43.5 %) | |
| Non-profit, education, or government | 13 (5.7 %) | 1 (4.3 %) | |
| Ratings | Mean (SD) | Mean (SD) | |
| Most recent | 3.2 (1.07) | 3.3 (1.07) | p = .734 |
| Overall | 3.1 (1.04) | 3.2 (1.0) | p = .880 |
| Price | Median (range) | Median (range) | |
| US$ | 0.99 (0–24.99) | 1.99 (0–4.99) | p = .976 |
| Number of reviews | |||
| Most recent | 13 (5–1,525) | 14 (7–1,214) | p = .161 |
| Overall | 19 (5–4,500) | 14 (7–4,500) | p = .056 |
Reliability was assessed for all of the AADE7™ skills. Overall reliability between description-based and download-based ratings of the AADE7™ skills was good (kappa = 0.66). However, reliability for ratings of individual skills was mixed. Reliability was excellent for being active (kappa = 0.81) and monitoring (kappa = 0.91), good for healthy eating (kappa = 0.65), fair for taking medication (kappa = 0.55), and poor for problem solving (kappa = 0.31), reducing risks (kappa = 0.25) and healthy coping (kappa = 0.28). These data are presented in Table 4.
Table 4.
Agreement and reliability of AADE7™skills based on description pages versus downloads
| AADE7™ skill | Agreement between description page and downloaded app on skill promotiona | Under-reporting of skill based on description pageb | Over-reporting of skill based on description pagec | Kappa |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Healthy eating | 19 (82.6 %) | 2 (8.7 %) | 2 (8.7 %) | 0.65 |
| Being active | 21 (91.3 %) | 2 (8.7 %) | 0 (0 %) | 0.81 |
| Monitoring | 22 (95.7 %) | 1 (4.4 %) | 0 (0 %) | 0.91 |
| Taking Medication | 19 (82.6 %) | 3 (13.0 %) | 1 (4.4 %) | 0.55 |
| Problem solving | 15 (65.2 %) | 6 (26.1 %) | 2 (8.7 %) | 0.31 |
| Reducing risks | 19 (82.6 %) | 3 (13.0 %) | 1 (4.4 %) | 0.25 |
| Healthy coping | 19 (82.6 %) | 4 (17.4 %) | 0 (0 %) | 0.28 |
aAgreement refers to the number and percentage of times the presence or absence of the AADE7™ skill was rated identically in the initial review of the app description page and review of the downloaded app
bUnder-reporting of skill refers to the number and percentage of times the AADE7™ skill was rated as absent during review of the app description page but present during review of the downloaded app
cOver-reporting of skill refers to the number and percentage of times the AADE7™ skill was rated as present during review of the app description page but absent during review of the downloaded app
Specific methods of self-management
Downloading apps for review allowed for a detailed post hoc assessment of the specific means and methods of self-management. In order to capture the array of skills present in apps, we recorded specific methods for promoting AADE7™ skills within the four most complex categories: (1) healthy eating, (2) being active, (3) monitoring of biomarkers, and (4) problem solving. This was unrelated to reliability as it was impossible to rate apps at this level of detail from description pages. These data are presented in Table 5. Thirty percent of the apps downloaded for review monitored diet and 35 % monitored physical activity. Half of these apps allowed users to track diet or physical activity in relation to target values (e.g., out of range glucose levels) or other activities (e.g., physical activity). Almost 60 % of apps monitored biomarkers, most commonly in the form of blood glucose monitoring and never in the form of urine ketone monitoring. A little over half of the biomarker monitoring apps allowed users to monitor biomarkers in relation to target values or activities. Forty-eight percent of apps provided problem solving assistance, usually in the form of graphing monitoring results in relation to target ranges or activities. Only two apps guided users through an interactive action plan to manage their diabetes.
Table 5.
Specific methods for promoting healthy eating, being active, monitoring, and problem solving in downloaded apps
| Behavior | N (%) | Item tracked | Number | Specific method of tracking behavior | Number |
|---|---|---|---|---|---|
| Monitoring of healthy eating | 7 (30.4 %) | Carbohydrates only | 3 | Graph or list only Graph or list in relation to target values or activities | 3 4 |
| Combination (e.g., protein, fats, and carbs) | 2 | ||||
| Categorical rating (e.g., fatty foods) | 2 | ||||
| Monitoring of being active | 8 (34.8 %) | Minutes only | 3 | Graph or list only Graph or list in relation to target values or activities | 5 3 |
| Level (e.g., easy, moderate, hard) only | 3 | ||||
| Minutes and level | 2 | ||||
| Monitoring of biomarkers | 13 (56.5 %) | Blood glucose | 13 | Graph or list only Graph or list in relation to target values or activities | 8 7 |
| Blood pressure | 2 | ||||
| Urine ketones | 0 | ||||
| Weight | 3 | ||||
| Problem solving | 11 (47.8 %) | N/A | Graph only Graph with indicators (e.g., target glucose range) Graph and action plan | 3 6 2 |
N/A not applicable
DISCUSSION
The apps reviewed herein represent a tentative beginning to enhancing diabetes self-management with mobile applications. Our search resulted in over 200 diabetes self-management apps, suggesting that app developers realize that the high prevalence of diabetes and the complex nature of diabetes self-management may make diabetes especially amenable to mobile intervention. As patients with diabetes must engage in and respond to numerous behaviors over the course of a single day (e.g., checking and responding to blood glucose levels, eating healthfully, engaging in physical activity, administering medication), a well-crafted app could provide a convenient portal for reminders, self-monitoring, and problem solving. Yet few such apps exist, indicating that much work is necessary to improve the quality of available apps.
Few apps promoted more than two AADE7™ behaviors and none promoted all seven behaviors. This suggests a disconnect between clinical guidelines and app features. The finding held for apps developed by non-profit, education, and government institutions, indicating that patients may need to take on the burden of and initiative in downloading multiple apps in order for apps to be an effective component of diabetes self-management. Indeed, one app, Glucose Buddy 3.6.5, that focuses on the monitoring of biomarkers, instructs users to download two additional apps related to diet and activity for best results. It should be noted, however, that it is also likely that not all patients may need or want to use apps to manage all of the AADE7™ behaviors; for example, some patients may simply want to track carbohydrate consumption, while others may want to keep track of medications.
Self-monitoring (most often in the form of the self-monitoring of blood glucose; SMBG) was the most commonly promoted AADE7™ behavior. The variety of ways in which SMBG was promoted provided excellent examples of the strengths and weaknesses of current apps. Strengths included the ability to track blood glucose readings over time and apps that could guide users in interpreting blood glucose readings, for example, by alerting them to values outside of a predefined range. Fewer apps helped users respond to specific readings and those that did were generally limited to helping patients calculate the proper dose of insulin based on meals and activities. These data are supported by the results of the post hoc analyses of specific methods of self-management in the apps downloaded for review. Calculating insulin dosages is an important component of diabetes self-management, if users are prescribed insulin. However, many patients with type 2 diabetes do not use insulin and might benefit from apps that help them respond to out of range readings with suggestions for changes in diet or activity. That is, most apps did not embed monitoring within an action framework that could help patients understand how to interpret and respond to blood glucose readings across a variety of settings, as suggested by the theoretical model most closely aligned with the effective use of SMBG, the Common Sense Model of Self-Regulation (CSM) [16–18].
Similar to apps focused on monitoring, apps that promoted problem solving often made use of the iPhone’s (and other smartphones’) unique technical capabilities; for example, by using data visualization techniques to demonstrate out of range glucose levels (e.g., color coded graphs). However, while apps that promoted problem solving tended to alert patients to potential problems, they did not necessarily guide patients in potentially helpful responses, as evidenced by the fact that only two of the downloaded apps allowed for the use of action plans as part of problem solving. Further, few apps presented problem solving in its empirically tested form, that is, by leading users through the entirety of the seven steps delineated by D’Zurilla and Nezu [19]. Most apps presented just the solution implementation phase of problem solving (i.e., monitoring outcomes and evaluating solution effectiveness through color coded charts and graphs that indicated when food, exercise, or biomarker levels were out of range). The use of structured problem solving exercises may be especially important to include in future applications as a problem solving-based intervention has been shown to improve glycemic control in patients with type 2 diabetes [20].
The data also suggest that the promotion of healthy eating and/or medication adherence might benefit from fuller use of the novel components of smartphones. These skills were promoted in almost half of all apps’ description pages, most commonly through lists of healthy recipes or medication alarms. Some apps allowed users to sync recipes with shopping lists or provided automatic refill reminders, but the majority did not leverage the unique aspects of smartphones; for example, fewer than 20 % of apps downloaded for review allowed users to graph the results of diet and activity monitoring in relation to target ranges or activities. Future apps may benefit from the ability to sync information across computers or websites or use recipes and Bluetooth-enabled meters to create graphs or logs of foods/calories/grams of fat or carbohydrates consumed. Apps promoting physical activity made better use of some of the iPhone’s novel components, like the phone’s built-in accelerometer.
Healthy coping and reducing risks were the least commonly promoted AADE7™ behaviors, most likely because they are the most difficult to promote in mobile settings (e.g., there are few ways to treat depression or provide a comprehensive interpretation of a metabolic panel via smartphone). However, some aspects of these skills are promoted in separate apps (e.g., those that promote relaxation training) and could be integrated into existing programs. Further, research on cell phone therapy is ongoing and may result in stand-alone mobile treatments for emotional and motivational issues [21, 22]. Increasing the use of the reducing risks skill set may be more difficult as it is a broader category, but future diabetes self-management apps could be integrated with existing apps that address risky behaviors (e.g. smoking cessation). However, it should be noted that, like current diabetes apps, apps promoting smoking cessation do not necessarily adhere to established guidelines and are in need of further development [23].
Methodological considerations
Prior research [11] relied solely on Apple’s App Store’s description pages to supply information on app capabilities. We tested the reliability of this approach by downloading a random 10 % of eligible apps for use and review. Overall reliability between app review by description page and app review by download was good; however, the data suggest that the reliability of obtaining accurate data for each individual AADE7™ behavior from Apple’s App Store’s description pages is mixed. The excellent–good reliabilities for being active, monitoring biomarkers and healthy eating suggest that data pulled from description pages regarding these skills are likely to be accurate. The high reliabilities for these skills are most likely due to a combination of the high prevalence of these skills and the relatively straightforward nature of the skills. Similarly, reliabilities were low for skills that were uncommon and more difficult to operationalize (i.e., reducing risks and healthy coping). Indeed, the low prevalence of reducing risks and healthy coping makes the results inconclusive. The fair–poor reliabilities for taking medication and problem solving are most concerning, as these skills are commonly promoted. For both of these skills, descriptions pages were more likely to underreport the availability of these skills and as such, some apps may actually promote more of these behaviors than described in the data presented above.
These data highlight the importance of downloading all apps for review in future research. Downloading all apps related to medication and problem solving may be especially important for future work on apps related to diabetes self-management or other chronic conditions where these tools might be useful. It will be important for future studies to report information based on both description pages (i.e., what patients and clinicians most likely use to choose apps) and downloaded apps (i.e., information on the apps’ full capabilities). In this way, research can make statements about what kinds of apps are backed by research as well as users’ ability to determine this information from description pages (i.e., how most consumers decide on app purchases). This kind of app review process will not only provide useful information for clinicians, patients and scientists, but can give developers ideas for app improvement.
Linking cutting edge technology and theory
Diabetes is a relatively silent condition and research suggests that it is more difficult for patients to adhere to treatments for conditions that do not provide clear or “noisy” somatic cues [24–26]. Therefore, patients with diabetes cannot rely on “common sense” information from their bodies to help them manage their disease; rather, they must rely on external methods (e.g., SMBG). It is possible that mobile phone apps, especially if they are based on empirically supported theories of health beliefs and behaviors (like the Common Sense Model [16]), can provide additional ways for patients with diabetes to make use of external self-management methods intended to make their silent condition noisy. One way apps could make diabetes noisier is by using Bluetooth-enabled meters to transmit data directly to a smartphone, which could then alert the user if a reading is out of range and suggest corrective action. Given the empirical success of such methods [7] and the ubiquity of Bluetooth-enabled devices, it was surprising that only four apps made use of this technology. Similarly, the dearth of apps using social networks and/or gamification was unexpected given their popularity in the media and scientific communities [27].
Some notable exceptions to this trend are apps like Gmate SMART and DF Diary. The former consists of a small blood glucose meter that can be attached to the iPhone and used to track blood glucose levels and their relationship to foods, activities, and medications. The ability to view changes in blood glucose levels with respect to specific behaviors is an especially important feature, as the CSM suggests it is critical for effective glucose management [28]. DF Diary provides an interactive food and restaurant database that allows users to track nutritional information and save entries for later use. Users can track glucose levels, medication, and meals on graphs that can be viewed on the phone or sent directly to their physicians. The app also includes a diabetes forum in which other patients can discuss daily life with diabetes. As such, DF Diary allows patients to use concrete feedback (from the graphing and nutrition functions) to interact with their clinicians and peers all of which can inform their personal understanding of diabetes (i.e., their common sense models).
We found one example of a diabetes self-management app using gamification, Health Garden: Diabetic edition. This app links users’ blood glucose, blood pressure, weight and other health variables to the growth of a virtual garden: the better the monitoring and results, the more the garden flourishes. This app does not in and of itself improve users understanding of diabetes, but it may motivate patients to use already acquired skills to improve their health. Indeed, pilot work suggests that the gamification of diabetes self-management improves the frequency of SMBG in adolescents [29]; however, it remains to be seen whether gamification can improve health outcomes and additional research is necessary.
Given the sheer number of diabetes self-management apps currently available, we believe more will follow. Partnerships between academics and app developers may be an important component of future mHealth endeavors. Researchers can provide information on empirically based theories to inform app development, and developers can provide information on the practical limitations of technology. These efforts must take into account the increased costs associated with such collaboration; for example, integrating theories into apps may require complex data algorithms that are expensive to produce. However, our data indicate that apps developed by non-profit, education, or government institutions are less expensive than other apps, suggesting that this collaboration need not be costly for consumers, despite development costs. Research could also help determine the optimal number of AADE7™ behaviors to include in apps, further limiting app complexity and cost.
Dissemination
Apps developed in a collaborative manner will not be useful or able to affect health outcomes if patients do not use them. Patients may be more likely to use apps if recommended by a trusted source, like a health care provider. Providers, however, do not have time to independently evaluate apps on their own. Further, this study demonstrates that app turnover is rapid, making it difficult for busy clinicians and researchers to keep track of an ever-changing landscape. Independent app reviewers, such as Happtique [http://www.happtique.com], could address these problems by providing clinicians with information on the empirical basis of apps and, most importantly, by finding effective means of disseminating these findings to providers (e.g., by offering CE credits for reading app reviews). In this way, health care providers and independent app reviewers like Happtique [http://www.happtique.com] can play a critical role in disseminating effective and evidence-based apps. Collaboration between health professionals and app reviewers could also protect consumers from dangerous misinformation. For example, potential for harm is especially great in insulin dosage apps, as insulin overdose can lead to severe hypoglycemia and coma—physician review of such apps could decrease the likelihood of such occurrences.
Limitations
A limitation of this study is that no apps were tested by patients with diabetes. However, the methods with which the authors chose and reviewed apps was intended to mimic the way consumers and patients might choose apps for diabetes self-management. Not all apps were downloaded and reviewed, and the reliability between downloaded apps and all reviewed apps was low for some criteria. Specifically, the low reliabilities for problem solving, reducing risks, and healthy coping prevent strong conclusions regarding the ways that apps address these skills. Further, as mentioned above, the small sample of apps developed by non-profit, education, or government institutions affected the power of analyses used to determine whether there were differences in the number of AADE7™ skills promoted by those or other applications.
CONCLUSION
Diabetes mHealth is an area ripe for future research. Apps are a promising method of diabetes self-management and unlike paper and pencil self-management tools, can be flexibly tailored to individual health requirements through a routinely carried item (i.e., a smartphone). Most available apps, however, do not fully adhere to evidence based guidelines. Much work is needed to promote the development of evidence-based apps. This research should focus on integrating theories of health and health behavior change into diabetes self-management apps, empirically testing apps and providing patients and clinicians with the results of these endeavors. Additionally, future app review studies should download and test all apps to address reliability concerns and to ensure that apps that appear evidence-based follow recommend guidelines. Recent research suggests that mobile health apps may save US$6 billion in yearly medical costs worldwide [30]. Given the preliminary success of diabetes self-management programs like U-Health, there is reason to believe that with continued research it may be possible to integrate responsive feedback from mobile applications into diabetes self-management to improve patients’ control over a silent and costly condition.
Footnotes
Implications
Practice: Most diabetes apps do not adhere to more than two AADE7™ self-care behaviors, therefore, clinicians should exercise caution when recommending such apps.
Policy: There are no regulations regarding the empirical and/or theoretical basis of apps and, as such, developers and/or app stores should note whether apps are empirically based so that consumers can make informed decisions.
Research: Future research should address whether and which apps are most effective in helping patients achieve glycemic control.
Contributor Information
Jessica Y. Breland, Phone: +1-415-2650571, FAX: +1-732-9321253, Email: Jessica.breland@gmail.com.
Vivian M. Yeh, Email: Vvn.yeh@gmail.com.
Jessica Yu, Email: jessica.yu@rutgers.edu.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. 2011.
- 2.Association AD. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31(3):596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 3.Hernández-Ronquillo L, Téllez-Zenteno JF, Garduño-Espinosa J, et al. Factors associated with therapy noncompliance in type-2 diabetes patients. Salud Publica Mex. 2003;45(3):191–197. doi: 10.1590/S0036-36342003000300008. [DOI] [PubMed] [Google Scholar]
- 4.Kirk A, Mutrie N, MacIntyre P, et al. Increasing physical activity in people with type 2 diabetes. Diabetes Care. 2003;26(4):1186–1192. doi: 10.2337/diacare.26.4.1186. [DOI] [PubMed] [Google Scholar]
- 5.Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med. 2005;118(Suppl 5A):27S–34S. doi: 10.1016/j.amjmed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166(17):1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 7.Lim S, Kang SM, Shin H, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care. 2011;34(2):308–313. doi: 10.2337/dc10-1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.As smartphone prices fall, retailers are leaving money on the table, according to The NPD Group. Available at: http://www.npdgroup.com/wps/portal/npd/us/news/pressreleases/pr_111114a. Accessed 29 July 2012.
- 9.Pew Internet and American Life Project. The social life of health information and the Internet. Available at: http://www.chcf.org/publications/2012/07/social-life-health-information. Accessed 29 July 2012
- 10.Purcell K. Half of adult cell phone owners have apps on their phones.Pew Research Center’s Internet and American Life Project; 2011. Available at: http://pewinternet.org/Reports/2011/Apps-update.aspx. Accessed 29 July 2012
- 11.Breton E, Fuemmeler B, Abroms L. Weight loss—there is an app for that! But does it adhere to evidence-informed practices? Transl Behav Med. 2011;1(4):523–529. doi: 10.1007/s13142-011-0076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chomutare T, Fernandez-Luque L, Årsand E, et al. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res. 2011;13(3):e65. doi: 10.2196/jmir.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Association of Diabetes Educators. AADE7, Self-Care Behaviors. Available at: http://www.diabeteseducator.org/ProfessionalResources/AADE7/. Accessed on 29 July 2012
- 14.Franko OI, Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Syst. 2012;36(5):3135–3139. doi: 10.1007/s10916-011-9798-7. [DOI] [PubMed] [Google Scholar]
- 15.Cicchetti D. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–290. doi: 10.1037/1040-3590.6.4.284. [DOI] [Google Scholar]
- 16.Leventhal H, Bodnar-Deren S, Breland JY, et al. Modeling health and illness behavior: the approach of the commonsense model. In: Baum AS, Revenson TA, Singer J, et al., editors. The Handbook of Health Psychology. Second. New York: Erlbaum; 2011. pp. 3–35. [Google Scholar]
- 17.Clar C, Barnard K, Cummins E, et al. Aberdeen Health Technology Assessment G. Self-monitoring of blood glucose in type 2 diabetes: systematic review. Health Technol Assess. 2010;14(12):1–140. doi: 10.3310/hta14120. [DOI] [PubMed] [Google Scholar]
- 18.Malanda UL, Welschen LM, Riphagen II, Dekker JM, Nijpels G, Bot SD. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. In: Cochrane Database of Systematic Reviews. Wiley;2012.Available at: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005060.pub3/abstract. Accessed 3 June 2012 [DOI] [PubMed]
- 19.D’Zurilla TJ, Nezu AM. Problem-solving Therapy. 3. New York: Springer; 2007. [Google Scholar]
- 20.Hill-Briggs F, Lazo M, Peyrot M, et al. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J Gen Intern Med. 2011;26(9):972–978. doi: 10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dimeff L, Paves AP, Skutch JM, et al. Shifting paradigms in clinical psychology: How innovative technologies are shaping treatment delivery. In: Barlow DH, et al., editors. The Oxford Handbook of Clinical Psychology. New York: Oxford University Press; 2001. pp. 618–648. [Google Scholar]
- 22.Morris ME, Kathawala Q, Leen TK, et al. Mobile therapy: case study evaluations of a cell phone application for emotional self-awareness. J Med Internet Res. 2010;12(2):e10. doi: 10.2196/jmir.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abroms LC, Padmanabhan N, Thaweethai L, et al. iPhone apps for smoking cessation. Am J Prev Med. 2011;40(3):279–285. doi: 10.1016/j.amepre.2010.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leventhal H, Leventhal EA, Breland JY. Cognitive science speaks to the “Common-Sense” of chronic illness management. Ann Behav Med. 2011;41(2):1–12. doi: 10.1007/s12160-010-9246-9. [DOI] [PubMed] [Google Scholar]
- 25.Halm EA, Mora P, Leventhal H. No symptoms, no asthma: the acute episodic disease belief is associated with poor self-management among inner-city adults with persistent asthma. Chest. 2006;129(3):573–580. doi: 10.1378/chest.129.3.573. [DOI] [PubMed] [Google Scholar]
- 26.Baumann LJ, Cameron LD, Zimmerman RS, et al. Illness representations and matching labels with symptoms. Health Psychol. 1989;8(4):449–469. doi: 10.1037/0278-6133.8.4.449. [DOI] [PubMed] [Google Scholar]
- 27.Anderson J, Rainie L. The Future of Gamification.Pew Research Center’s Internet & American Life Project; 2012. Available at: http://www.pewinternet.org/topics/Future-of-the-internet.aspx. Accessed July 29, 2012.
- 28.McAndrew L, Schneider SH, Burns E, et al. Does Patient Blood Glucose Monitoring Improve Diabetes Control? Diabetes Educator. 2007;33(6):991–1010. doi: 10.1177/0145721707309807. [DOI] [PubMed] [Google Scholar]
- 29.Cafazzo JA, Casselman M, Hamming N, et al. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res. 2012;14(3):e70. doi: 10.2196/jmir.2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cox A. Mobile Healthcare Opportunities: Smartphone Apps, Monitoring, and mHealth Strategies 2011–2016. Hampshire: Juniper Research; 2011. [Google Scholar]