The Accreditation Council for Graduate Medical Education (ACGME) first established national standards for resident duty hours in 2003 as part of the Common Program Requirements.1 Residents were limited to 30-hour duty periods, with a maximum 80 working hours and 1 day free from clinical responsibilities each week, averaged over a 4-week period.1 In 2008, the Institute of Medicine recommended greater supervision and additional limits on residents' hours.2
In response, an ACGME Duty Hours Task Force developed new Common Program Requirements that were released in 2010.3 The objectives of these revisions were to improve the safety and quality of patient care as well as resident education and quality of life.4 Although program directors and residents expressed some concerns that these benefits might not be realized, the new duty hours went into effect on July 1, 2011.5–12
Duty Hour Compliance
Before 2011, institution-level data from the ACGME demonstrated high rates of compliance (nearly 95%) with 2003 Common Program Requirements. However, this was contradicted by numerous published reports tracking resident work hours and anonymous resident surveys identifying frequent noncompliance and underreporting of duty hours.13–18 In 2006, a large study by Landrigan et al19 found that 83.6% of interns (N = 1068) reported duty hour violations during at least 1 month of the yearlong surveillance study.
We believe there are several potential reasons for violation of the duty hour standards. The balance of patient care and education may lead to unintentional noncompliance as residents contend with increased work density. At the same time, programs and faculty may place unrecognized pressure on residents to meet educational objectives and patient needs. Finally, trainees who disagree with the limits may actively choose to violate the rules.
Regardless of the reason for noncompliance, training programs are expected to monitor resident and fellow duty hours and maintain compliance with ACGME standards.5 New Institutional Requirements proposed for implementation in July 2014 state that “the Sponsoring Institution must provide systems to educate and monitor…accurate and honest reporting of duty hours information by residents/fellows.”20 Frequent violations place programs and institutions at risk for added scrutiny, accreditation with warning, probation, or even withdrawal of accreditation by the ACGME. Consequently, residents may feel obliged to underreport hours or violations in order to appear compliant and to avoid punitive actions on themselves or their programs.
In August 2010, a survey of more than 2500 residents on the proposed Common Program Requirements found that 84% of respondents reported compliance with the 2003 standards. In this same survey, 27% of residents speculated that it would be more difficult for them to comply with the stricter 2011 standards.6 To assess both the perceived impact of the 2011 regulations as well as self-reported compliance with the new duty hour standards, follow-up surveys of residents and program directors were conducted.21,22
Resident Survey
In December 2011, we asked designated institutional officials (DIOs) at all ACGME-sponsoring institutions to distribute an anonymous, electronic questionnaire to their residents and fellows. By February 2012, 26 581 residents had received the survey. To assess duty hour compliance, participants were asked to respond to the statement, “I comply with ALL duty hour regulations” by using a 5-point Likert scale, ranging from “never” to “always.” Each answer was provided with an estimated “percentage compliance” in an attempt to standardize responses (eg, “mostly compliant” meant approximately 75% compliance). For analytic purposes, noncompliance was defined as any response other than “always.” Residents were also asked to estimate how often they “falsely reported duty hours to appear in compliance with regulations,” by using a similar Likert scale. Falsification was likewise defined as any response other than “never.” In both cases, the outcome measured was considered a binary variable (ie, compliant versus noncompliant or falsification versus no falsification).
A total of 6202 residents (23.3%) responded to the survey. Men and women were equally represented in the sample (50.1% versus 49.9%). Most respondents were in the first 3 postgraduate years (78%) and represented internal medicine (22.2%), surgery (16.5%), or pediatrics (10.9%). The sample was generally representative of all US residents by the demographic variables measured (table 1).21
TABLE 1.
Demographic Characteristics of Respondents and Comparative ACGME Data on US Residentsa,b
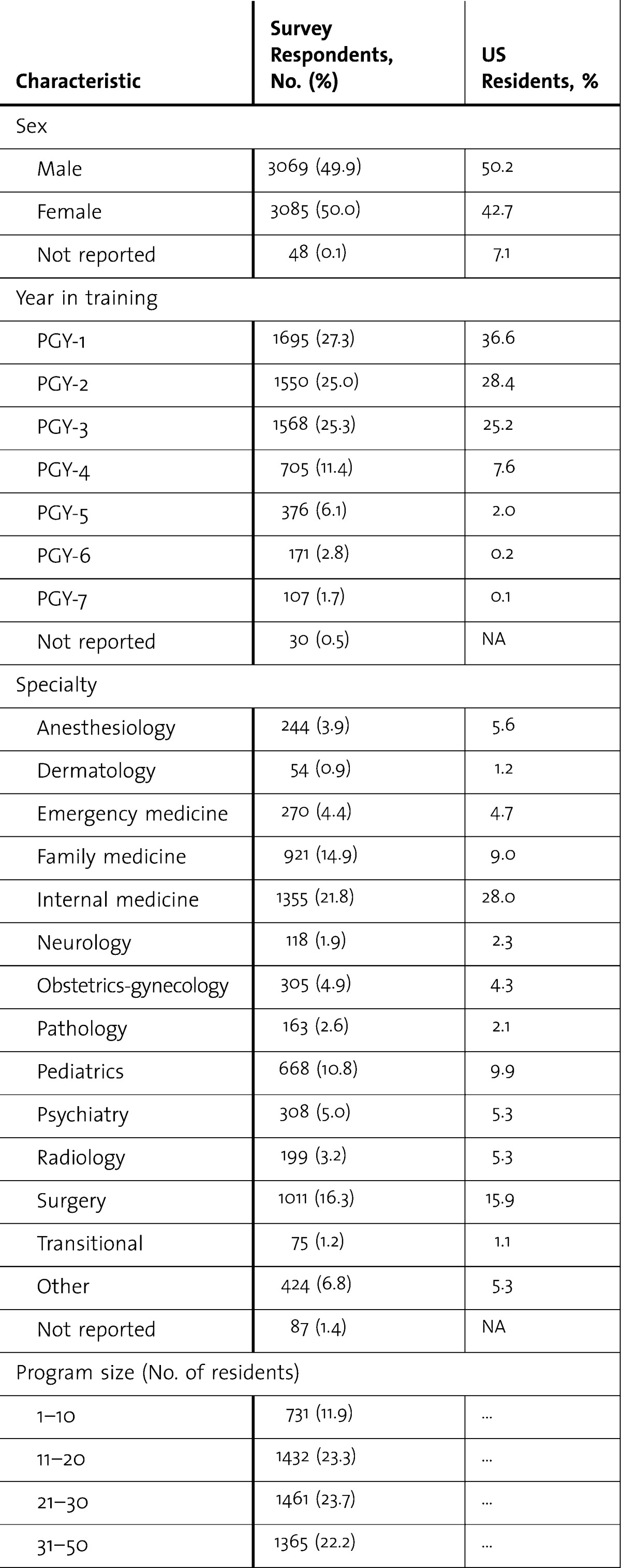
TABLE 1.
Continued
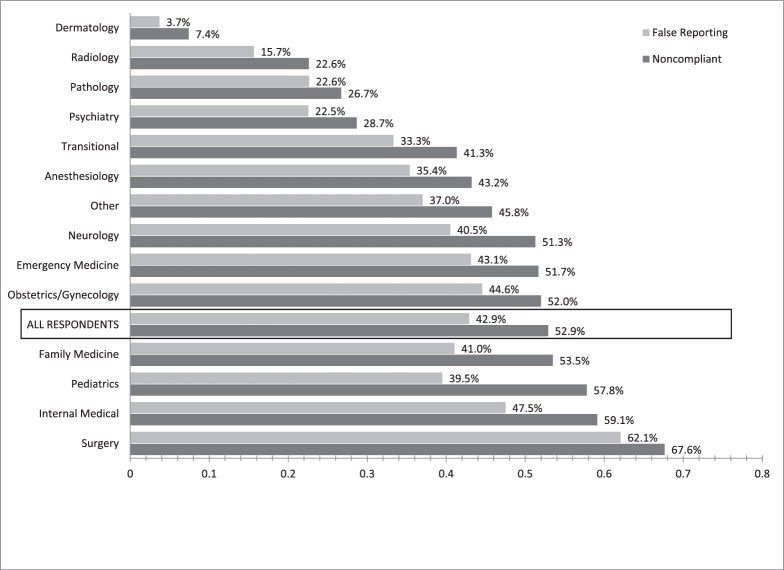
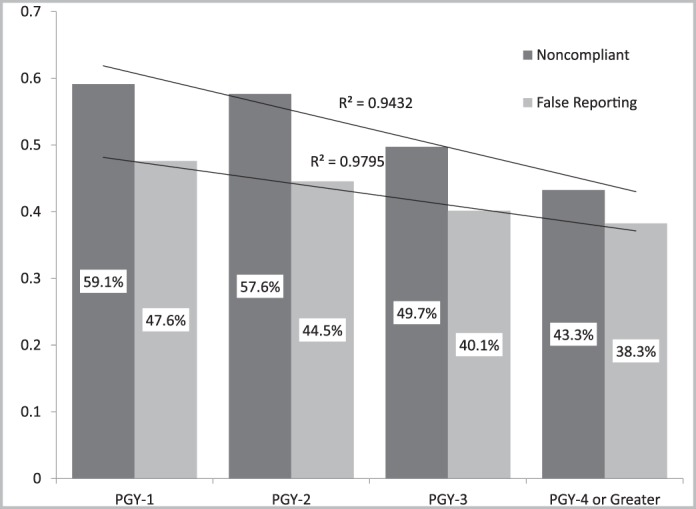
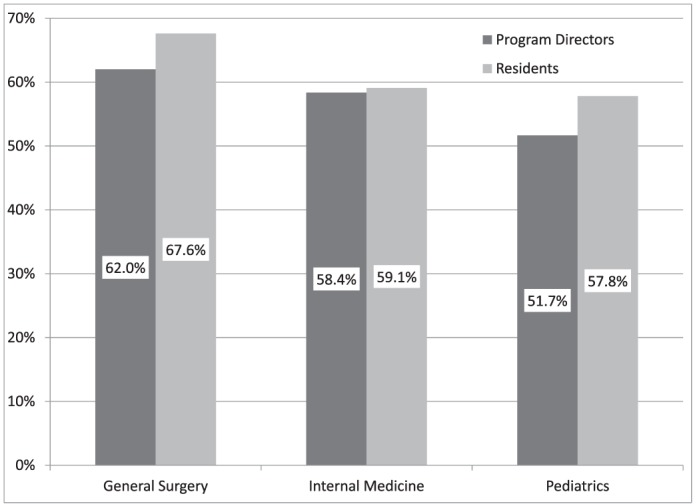
Nearly half of respondents (47.1%) reported they were “always” compliant with the 2011 duty hour standards. Of residents reporting noncompliance (52.9%), most stated that they were “mostly compliant” (82.3%; table 2). In a subgroup analysis, the highest rates of noncompliance were reported by residents in the 3 largest training groups—surgery (67.6%), internal medicine (59.1%), and pediatrics (57.8%; figure 1). Residents earlier in their training reported greater noncompliance, a linear trend demonstrated in figure 2. This correlation between postgraduate year and noncompliance remained significant (logistic regression, P < .001) after adjusting for specialty, sex, and program size in multivariate analysis.
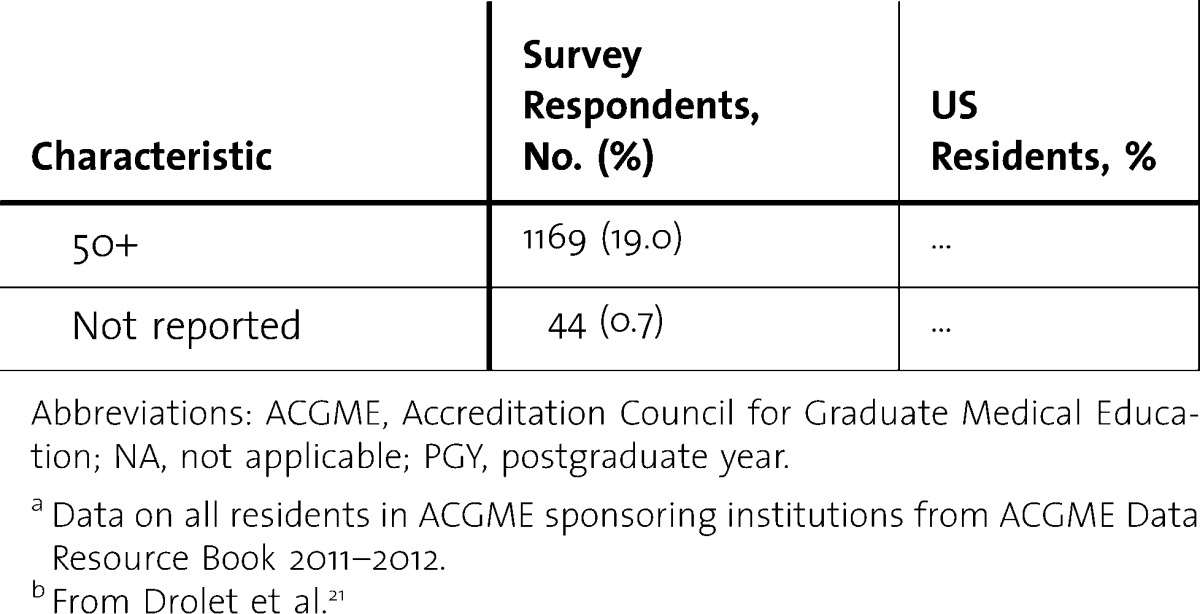
TABLE 2.
Compliance and Duty Hour False Reporting
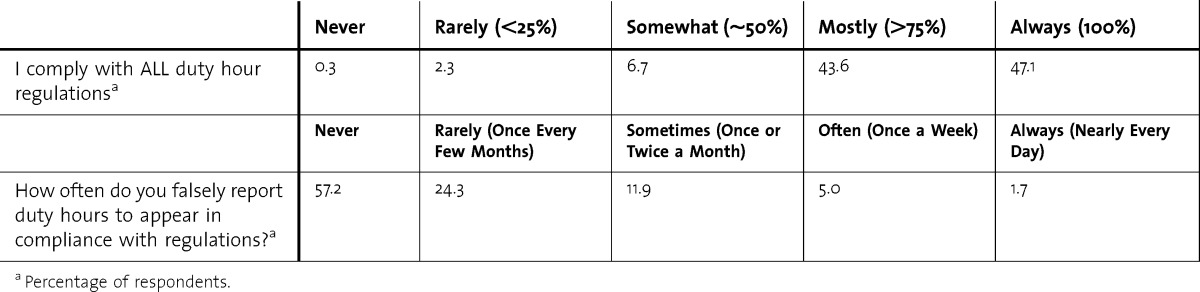
FIGURE 1.
Percentage of Trainees Reporting Noncompliance or Duty Hour Falsification in Each Specialty
Boxed area indicates averaged percentage of all respondents (n = 6202).
FIGURE 2.
False Reporting and Noncompliance by Postgraduate Year
Linear regression modeling shows a strong correlation with decreased falsification and noncompliance with increasing postgraduate year.
Nearly half of residents (42.9%) responded that they falsely reported their duty hours at some time, including 18.6% who reported falsely at least once or twice per month (table 2). Surgical residents were 2.18 times more likely to falsely report hours than all other specialties. As with noncompliance, an inverse linear association was noted between years of training and false reporting (figure 2).
Lastly, we correlated resident-reported compliance and falsification with the perceived effect of duty hour standards on patient safety, quality of education, quality of life, and residents' overall approval of the regulations. The methods for assessing perspectives and the results from this portion of the study have been previously reported.21 We found that negative perceptions were strongly associated (logistic regression, P < .001) with noncompliance and greater falsification for each of these variables. For example, residents who reported that patient safety had worsened as a result of the 2011 standards were 1.51 times more likely to report noncompliance and 1.69 times more likely to report falsification than those who stated that patient safety was unchanged or better. Similar associations between negative perceptions and noncompliance, as well as falsification, were noted for education (odds ratio [OR] 1.98 and 2.47, respectively), quality of life (OR 2.01 and 1.87, respectively), and overall disapproval of the 2011 rules (OR 1.88 and 2.17, respectively).
Program Director Survey
We also conducted a survey of residency program directors in general surgery, internal medicine, and pediatrics to assess perceptions and approval of duty hour regulations. In this study, we also asked program directors, “In general, how compliant are your residents with ACGME duty hour regulations?” We used the same 5-point Likert scale (“never” to “always”) with estimated percentage compliance for standardization. Of 730 eligible participants, 549 unique responses were received (75.2% response rate).22
Across the 3 specialties, program directors reported 57.3% noncompliance—any response other than “always” compliant. Surgeons reported their residents had the highest noncompliance rate (62.0%), followed by internists (58.4%) and pediatricians (51.7%). When we compared these data to resident responses based on training specialty, we found that there was no significant difference to residents' reported rates of noncompliance (figure 3).
FIGURE 3.
Reported Noncompliance by Program Directors and Residents by Specialty
Implications
Our study has several important implications. First, most residents (52.9%) in a large, representative sample reported some degree of noncompliance, and almost half (42.9%) admit to falsifying duty hour reports. Although we expected that senior residents would violate duty hours more frequently in order to provide patient care or to manage their teams, we found that junior residents were more likely to report noncompliance. Although this survey does not address each element of the 2011 guidelines, such as the 16-hour duty hour limit for interns, our findings suggest the stricter 2011 rules may be more difficult to follow. Alternatively, senior residents may have better efficiency and experience with duty hour regulations, which may contribute to better compliance. Second, there was a strong association between noncompliance and a negative opinion of the duty hour limits, suggesting some residents may intentionally violate duty hours owing to a disagreement on principle. Residents' concern for their education may be 1 impetus. Likewise, residents have professional obligations in caring for their patients, which they feel supersede regulations and may contribute to noncompliance, representing an “ethical dilemma” of duty hour regulations.23
This study has several limitations. First, the survey response rate from residents was low, which may indicate nonresponse bias. However, this response rate is not atypical for this type of survey study, particularly with such a large sample.24 Additionally, the study is generally representative of US residents, which may decrease the potential for selection bias.25,26 Second, these data are self-reported, which introduces the potential for recall bias. The anonymity of the web-based survey may, however, decrease social desirability bias as well as concern for potential punitive action that comes from “official” duty hour reporting.27 Finally, there may be some interpretation bias in the responses to our questions (ie, “always” versus “mostly” means something different to each person). However, the high concordance between resident and program director responses to the same question suggests similar interpretation between 2 independent samples, supporting the reliability of the question and the internal validity of the results.
Discussion
Our findings demonstrate continued problems with resident noncompliance and duty hour misrepresentation under 2011 Common Program Requirements, which were identified in studies following implementation of the 2003 standards.13–19 Before further duty hour restrictions are considered or implemented, we suggest that these issues be carefully examined and attempts are made at rectification.
We propose that the first step to improving compliance should be a nonpunitive approach that encourages accurate reporting. Although repeated violations by a resident or program would require some intervention—the standards are not voluntary guidelines—the approach could remain nonpunitive. Better awareness of noncompliance may be used to improve feedback to residents who could benefit from efficiency training. Likewise, more accurate reporting would help to identify programs in which violations are the rule rather than the exception, as well as institutions in which inadequate support is available for residents.
We believe there should be no motivation for duty hour falsification, and while occasional violations may be inevitable for residents, there should be a zero-tolerance policy for lying about duty hours. Beyond the unprofessional implications of this behavior, duty hour falsification undermines the entire system of duty hour regulation. Falsification prevents program directors and institutions from accurately assessing working conditions and from mitigating issues that result in duty hour violations. A lack of accurate data only hinders further study into determining a balanced work-life ratio for training the next generation of physicians.
We believe that increasing flexibility in the duty hour standards may be the best approach to allow for educational and patient safety goals to be met. This may involve fewer duty hour restrictions in future revisions of the Common Program Requirements or merely less strict adherence to standards. In other words, a 75% compliance requirement would have been met by 90.1% of residents in this survey, rather than only 47.1% who reported “always” (100%) compliant. Ultimately, ACGME clarification of the expectation for compliance, whether substantial or absolute, would be helpful to programs and institutions responsible for monitoring duty hours. To the authors, absolute adherence to duty hour standards seems at odds with ethical and professional standards of practicing medicine, which are explicitly reinforced in the Common Program Requirements: “Residents must demonstrate responsiveness to patient needs that supersedes self-interest [as well as] accountability to patients, society, and the profession.”5 We agree with numerous respondents in our surveys who commented that physician schedules cannot be strictly defined; flexibility is necessary to allow for inevitable patient needs.
Footnotes
Brian C. Drolet, MD, is Fifth-Year Resident, Department of Plastic Surgery, Alpert Medical School of Brown University and Rhode Island Hospital; Matthew Schwede, BA, is Third-Year Medical Student, Alpert Medical School of Brown University; Kenneth D. Bishop, MD, PhD, is Second-Year Fellow, Division of Hematology/Oncology, Department of Medicine, Alpert Medical School of Brown University and Rhode Island Hospital; and Staci A. Fischer, MD, is Designated Institutional Official, Rhode Island Hospital, and Associate Professor, Department of Medicine, Alpert Medical School of Brown University.
Funding: The authors report no external funding source for this study.
Discussed as a podium presentation at the 2013 ACGME Annual Education Conference, Orlando, FL, February 28 to March 3, 2013.
The resident perspective data from this survey were published in June 201221; the program director perspective data were published in February 2013.22
The authors wish to thank Mamoona Khokhar, MD, and Derrick Christopher, MD, MBA, for their assistance in study design and execution.
References
- 1.Philibert I, Friedmann P, Williams WT. New requirements for resident duty hours. JAMA. 2002;288(9):1112–1114. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 2.Iglehart JK. Revisiting duty-hour limits—IOM recommendations for patient safety and resident education. N Engl J Med. 2008;359(25):2633–2635. doi: 10.1056/NEJMp0808736. [DOI] [PubMed] [Google Scholar]
- 3.Nasca TJ, Day SH, Amis ES ACGME Duty Hour Task Force. The new recommendations on duty hours from the ACGME task force. N Engl J Med. 2010;363(2):e3. doi: 10.1056/NEJMsb1005800. [DOI] [PubMed] [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. Letter to the community, 2010. http://acgme-2010standards.org/pdf/Nasca_Letter_to_the_Community_June_23_2010.pdf. Accessed November 17, 2010. [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education. Common Program Requirements, 2011. http://www.acgme.org/acgmeweb/Portals/0/dh_dutyhoursCommonPR07012007.pdf. Accessed May 28, 2013. [Google Scholar]
- 6.Drolet BC, Spalluto LB, Fischer SA. Residents' perspectives on ACGME regulation of supervision and duty hours—a national survey. N Engl J Med. 2010;363(23):e34. doi: 10.1056/NEJMp1011413. [DOI] [PubMed] [Google Scholar]
- 7.Antiel RM, Thompson SM, Reed DA, James KM, Tilburt JC, Bannon MP, et al. ACGME duty-hour recommendations—a national survey of residency program directors. N Engl J Med. 2010;363(8):e12. doi: 10.1056/NEJMp1008305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fargen KM, Chakraborty A, Friedman WA. Results of a national neurosurgery resident survey on duty hour regulations. Clin Neurosurg. 2012;59:105–106. doi: 10.1227/NEU.0b013e3182698845. [DOI] [PubMed] [Google Scholar]
- 9.Mir HR, Cannada LK, Murray JN, Black KP, Wolf JM. Orthopaedic resident and program director opinions of resident duty hours: a national survey. J Bone Joint Surg Am. 2011;93(23):e1421–e1429. doi: 10.2106/JBJS.K.00700. [DOI] [PubMed] [Google Scholar]
- 10.Lo V, Ward C. 2011 ACGME duty hour week proposal—a national survey of family medicine residents. Fam Med. 2011;43(5):318–324. [PubMed] [Google Scholar]
- 11.Drolet BC, Spalluto LB, Zuckerman M, McDonnell M. New ACGME rules for supervision and duty hours: resident commentary. Med Health R I. 2011;94(6):167,171–172. [PubMed] [Google Scholar]
- 12.Drolet BC, Soh IY, Shultz PA, Fischer SA. A thematic review of resident commentary on duty hour and supervision regulations. J Grad Med Educ. 2012;4(4):454–459. doi: 10.4300/JGME-D-11-00259.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldstein MJ, Samstein B, Ude A, Widmann WD, Hardy MA. Work Hours Assessment and Monitoring Initiative (WHAMI) under resident direction: a strategy for working within limitations. Curr Surg. 2005;62(1):132–137. doi: 10.1016/j.cursur.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Sticca RP, Macgregor JM, Szlabick RE. Is the Accreditation Council for Graduate Medical Education (ACGME) Resident/Fellow survey, a valid tool to assess general surgery residency programs compliance with work hours regulations. J Surg Educ. 2010;67(6):406–411. doi: 10.1016/j.jsurg.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Macgregor JM, Sticca R. General surgery residents' views on work hours regulations. J Surg Educ. 2006;67(6):376–380. doi: 10.1016/j.jsurg.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Ladd AP. 2006;41(4):687–692. doi: 10.1016/j.jpedsurg.2005.12.010. Pediatric surgery fellowship compliance to the 80-hour work week [discussion in J Pediatr Surg. J Pediatr Surg. 2006;41(4):687–692. [DOI] [PubMed] [Google Scholar]
- 17.Tabrizian P, Rajhbeharrysingh U, Khaitov S, Divino CM. Persistent noncompliance with the work-hour regulation. Arch Surg. 2011;146(2):175–178. doi: 10.1001/archsurg.2010.337. [DOI] [PubMed] [Google Scholar]
- 18.Carpenter RO, Spooner J, Arbogast PG, Tarpley JL, Griffin MR, Lomis KD. Work hours restrictions as an ethical dilemma for residents: a descriptive survey of violation types and frequency. Curr Surg. 2006;63(6):448–455. doi: 10.1016/j.cursur.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 19.Landrigan CP, Barger LK, Cade BE, Ayas NT, Czeisler CA. Interns' compliance with Accreditation Council for Graduate Medical Education work-hour limits. JAMA. 2006;296(9):1063–1070. doi: 10.1001/jama.296.9.1063. [DOI] [PubMed] [Google Scholar]
- 20.Accreditation Council for Graduate Medical Education. Summary and impact of focused or major requirement revisions: Institutional Requirements, 2012. https://www.acgme.org/acgmeweb/Portals/0/Institutional_Requirements_Impact.pdf. Accessed March 17, 2013. [Google Scholar]
- 21.Drolet BC, Christopher DA, Fischer SA. Residents' response to duty-hour regulations—a follow-up national survey. N Engl J Med. 2012;366(24):e35. doi: 10.1056/NEJMp1202848. [DOI] [PubMed] [Google Scholar]
- 22.Drolet BC, Khokhar MT, Fischer SA. 2011 ACGME Common Program Requirements—a post-implementation study of program directors. N Engl J Med. 2013;368(8):694–697. doi: 10.1056/NEJMp1214483. [DOI] [PubMed] [Google Scholar]
- 23.Carpenter RO, Austin MT, Tarpley JL, Griffin MR, Lomis KD. Work-hour restrictions as an ethical dilemma for residents. Am J Surg. 2006;191(4):527–532. doi: 10.1016/j.amjsurg.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 24.Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805–1806. doi: 10.1001/jama.2012.3532. [DOI] [PubMed] [Google Scholar]
- 25.Krosnick JA. Survey research. Annu Rev Psychol. 1999;50:537–567. doi: 10.1146/annurev.psych.50.1.537. [DOI] [PubMed] [Google Scholar]
- 26.Dillman D. The design and administration of mail surveys. Annu Rev Sociol. 1991;17:225–249. [Google Scholar]
- 27.Joinson A. Social desirability, anonymity, and Internet-based questionnaires. Behav Res Methods Instrum Comput. 1999;31(3):433–438. doi: 10.3758/bf03200723. [DOI] [PubMed] [Google Scholar]