Abstract
Background
Education for all physicians should include specialty-specific geriatrics-related and chronic disease-related topics.
Objective
We describe the development, implementation, and evaluation of a chronic disease/geriatric medicine curriculum designed to teach Accreditation Council for Graduate Medical Education core competencies and geriatric medicine competencies to residents by using longitudinal encounters with a standardized dementia patient and her caregiver daughter.
Intervention
Over 3 half-day sessions, the unfolding standardized patient (SP) case portrays the progressive course of dementia and simulates a 10-year longitudinal clinical experience between residents and a patient with dementia and her daughter. A total of 134 residents participated in the University of Cincinnati-based curriculum during 2007–2010, 72% of whom were from internal medicine (79) or family medicine (17) residency programs. Seventy-five percent of participants (100) said they intended to provide primary care to older adults in future practice, yet 54% (73) had little or no experience providing medical care to older adults with dementia.
Results
Significant improvements in resident proficiency were observed for all self-reported skill items. SPs' evaluations revealed that residents' use of patient-centered language and professionalism significantly improved over the 3 weekly visits. Nearly all participants agreed that the experience enhanced clinical competency in the care of older adults and rated the program as “excellent” or “above average” compared to other learning activities.
Conclusions
Residents found this SP-based curriculum using a longitudinal dementia case realistic and valuable. Residents improved in both self-perceived knowledge of dementia and the use of patient-centered language and professionalism.
Editor's Note: The online version of this article contains a Box describing the structure of educational sessions used in this study. (Appendix 1 (29.5KB, doc) ) (Appendix 2 (45.5KB, doc) )
What was known
The majority of primary care physicians indicate they will care for older adults in their future practice, yet more than half report little or no experience caring for patients with dementia.
What is new
A 3-day unfolding case using standardized patients simulated a 10-year experience of caring for a patient with dementia and the patient's daughter.
Limitations
Limitations include the small sample, the limited validity of the self-assessment tool, and the lack of both external assessment of residents' skills and a control group.
Bottom line
Residents reported the case presentation was realistic and improved their self-perceived knowledge of dementia and use of patient-centered language.
Introduction
Since the 1993 Institute of Medicine Report entitled Strengthening Training in Geriatrics for Physicians, it has been recognized that training for all physicians should include general medicine and specialty-specific geriatrics-related topics.1 Although much progress has been made, additional chronic disease management curriculum development is important to ensure that all physicians possess the clinical competencies necessary for providing the highest quality of care to older adults.2,3 Despite the importance of this training objective, already crowded curriculum and increasingly restrictive duty hour requirements limit time available for teaching these important competencies.
This paper describes the development, implementation, and evaluation of a unique chronic disease/geriatric medicine curriculum designed to teach Accreditation Council for Graduate Medical Education (ACGME) core competencies and geriatrics clinical competencies. Multispecialty groups of resident physicians were taught longitudinally, using a standardized patient (SP) with Alzheimer disease (AD) and her caregiver daughter.
Intervention
Setting
In 2004, a new geriatric medicine curriculum was implemented at the University of Cincinnati to teach and provide formative feedback to multi-specialty groups of residents about skills linked to ACGME core competencies and geriatric medicine clinical competencies. AD was selected as the prototype for a longitudinal chronic disease SP case, which, over 3 half-day sessions, portrayed common challenges that occur over 10 years of caring for a dementia patient. The curriculum was implemented at the University of Cincinnati's Center for Competency Development and Assessment, an instructional facility featuring 16 clinical examination rooms that permitted videotaping and observation of trainee performance via a closed-circuit television video system.
Curriculum Description
Teaching Strategies
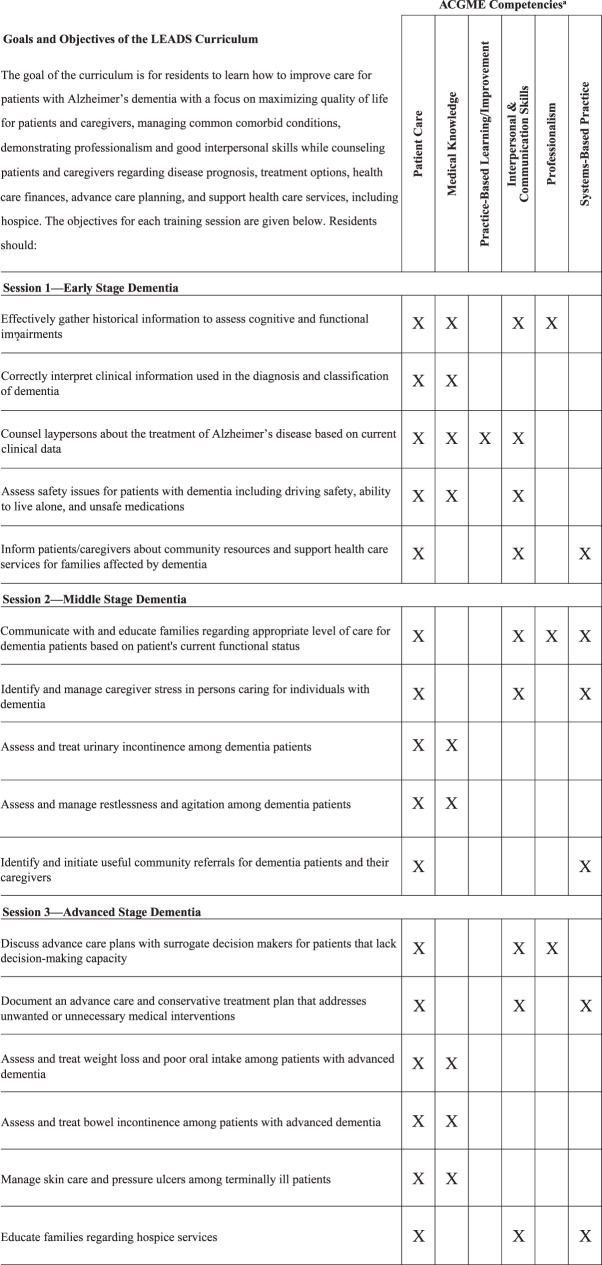
Over 3 half-day sessions, an unfolding SP case was implemented to portray the progressive course of Alzheimer dementia and simulate a 10-year longitudinal relationship between resident physicians and a dementia patient and her daughter. Learning goals and objectives for each session addressed important chronic disease/geriatric medicine competencies for primary care residents and the ACGME Core Competencies (figure).2–6 Teaching methods included lectures, videotaped longitudinal SP stations, SP feedback sessions, case discussion, and video review. Residents reviewed their own videotaped SP encounters individually and were guided in so doing by a written self-assessment containing 6 open-ended questions.7,8 Geriatrics and primary care faculty were recruited and trained to lead the sessions.
FIGURE 1.
Learning Goals and Objectives and ACGME Core Competencies Grid
Abbreviation: ACGME, Accreditation Council for Graduate Medical Education.
aEach X identifies that competency as key to the learning objective listed to the left of the X.
Structure
Teaching sessions combined didactic and experiential learning activities; didactics were organized around the SP sessions (provided as online supplemental material). The curriculum cycle repeated monthly. In groups of 2 to 6 residents, learners were scheduled for 3 consecutive weekly afternoon teaching sessions during an ambulatory elective.
Implementation
Twenty experienced SPs received 12 hours of formal on-site training. Using documentary footage of real patients, 1 of the authors (T.J.L.) instructed the SPs about realistic dementia portrayal. The SPs were also trained to elicit learners' formative self-evaluations of their performance during the verbal feedback sessions by using open-ended questions. All participating faculty also received training. An instructor's manual and faculty training program were developed to ensure a consistent instructional standard. Prior to implementing the actual curriculum, faculty instructors interviewed 10 SP pairs and elicited feedback in a pilot test to ensure validity. The pilot test provided faculty with first-hand experience with the curriculum they would be teaching and reinforced SPs' practice of new roles. The geriatric medicine program coordinator worked with participating residency program coordinators to arrange schedules.
Curriculum Evaluation
Baseline and Postintervention Geriatric Skills
Initial sessions began in July 2005. Following each session, residents completed anonymous self-ratings of their baseline (preintervention) and postintervention proficiency in 14 skill categories on a 5-point scale. Baseline skill ratings were assessed in a retrospective manner to guard against introduction of response shift bias.9,10 Initial faculty, SP, and resident physician feedback was used to revise questionnaires in 2006, and data from the academic years 2007 to 2010 were used for this evaluation.
Resident Performance as Rated by SPs
Using a written instrument, resident performance was jointly evaluated at the completion of all 3 sessions by 2 SPs (patient and daughter) assigned to each learner. The instrument included an 11-item evaluation of communication and interpersonal skills that were common to all stations (5-point scale: 1 = poor to 5 = excellent).
Resident Curricular Assessment
At the end of each teaching session, residents completed a written evaluation in which they were asked to rate the value, realism, and applicability of the experience and their confidence in providing medical care to older adults. After the final session, residents additionally used an online evaluation program to rate the educational value of course items.
Statistical Analyses
Trainees' retrospective pre-post self-ratings were compared for each skill category by using the Wilcoxon signed rank test for paired data (SPSS Inc, Chicago, IL). Session 1 and session 3 SP ratings of resident performance were compared using a paired sample t test to evaluate the change in total score of the resident's skills/observed behaviors. Effect sizes were calculated for each category, accounting for the correlation between repeated measures.11 Wilcoxon signed-rank test was used to assess the changes in specific questions in communication and interpersonal skills of the residents at the 2 time periods by both a “patient” and “daughter” evaluator.
The University of Cincinnati Institutional Review Board Social and Behavioral Sciences Division approved the project.
Results
Resident Participants
A total of 134 residents participated in the curriculum during years 2007 to 2010, of whom 72% were from general internal medicine (79) or family medicine (17). The remainder were residents from obstetrics-gynecology (17), internal medicine-pediatrics (10), and physical medicine and rehabilitation (5). Participants included 31 (23%) residents in postgraduate year (PGY)-2 and 77 (58%) PGY-3 residents and included 20 (15%) PGY-1, 5 (4%) PGY-4, and 1 PGY-5 resident(s). A total of 86% (115) of participants attended all 3 sessions of the curriculum. Seventy-five percent (100 of 134) of the participants said they intended to provide primary care to older adults in their future practice, yet 54% (73 of 134) had no or little experience with providing medical care to older adults with dementia. Only 51% (68 of 134) previously had an interaction with an SP as a part of their training.
Baseline and Postintervention Resident Self-Skill Ratings
During academic years 2007 to 2010, statistically significant improvements in self-reported proficiency were observed for all pre- and post-skill items (table 1). No differences were revealed by subanalysis of resident self-skill ratings as related to PGY, previous SP experience, specific residency program, or intention to provide primary care to older adults in future practice.
TABLE 1.
Resident Retrospective Pre- and Postintervention Self-Rating of Skills (N = 134)a
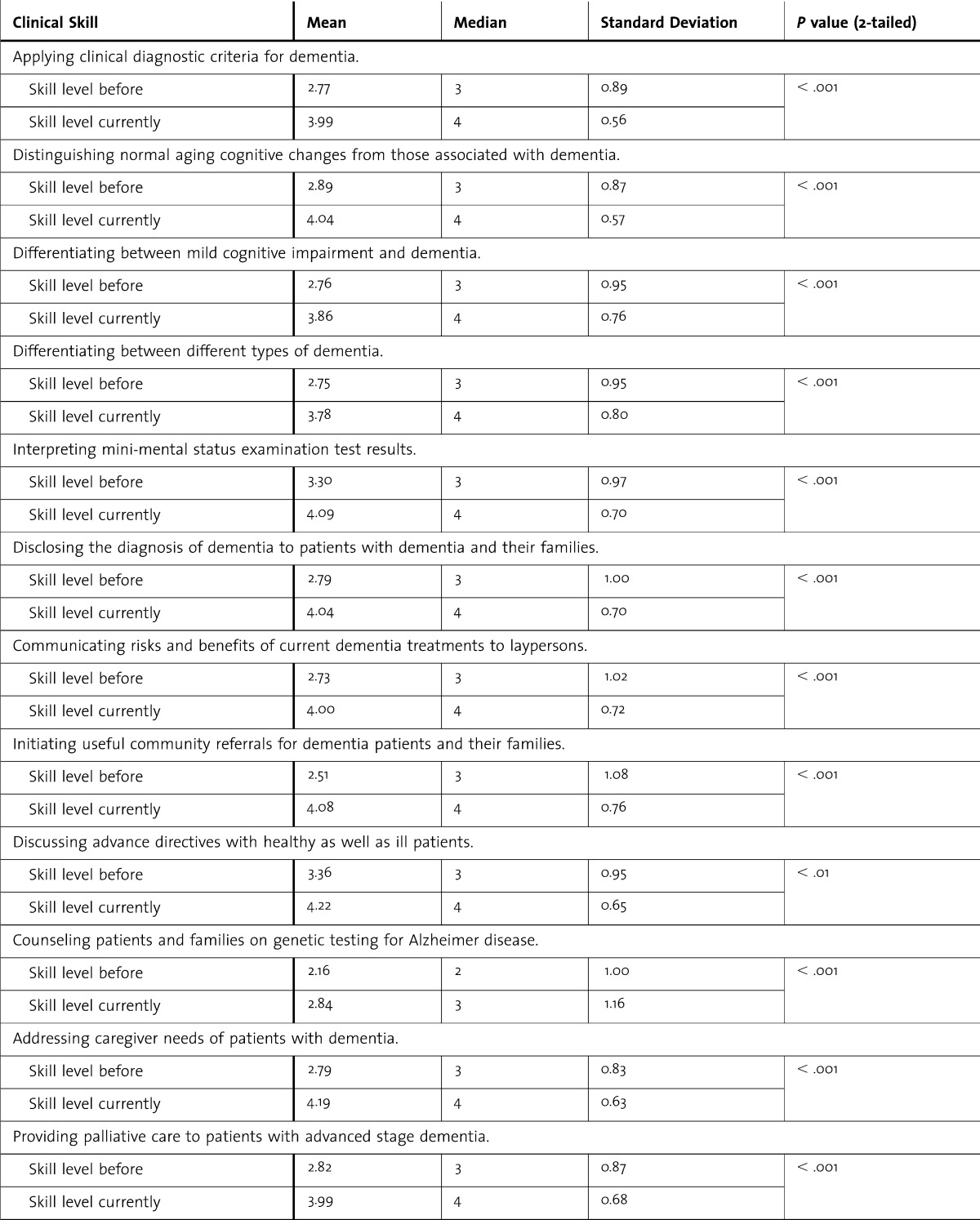
TABLE 1.
Continued
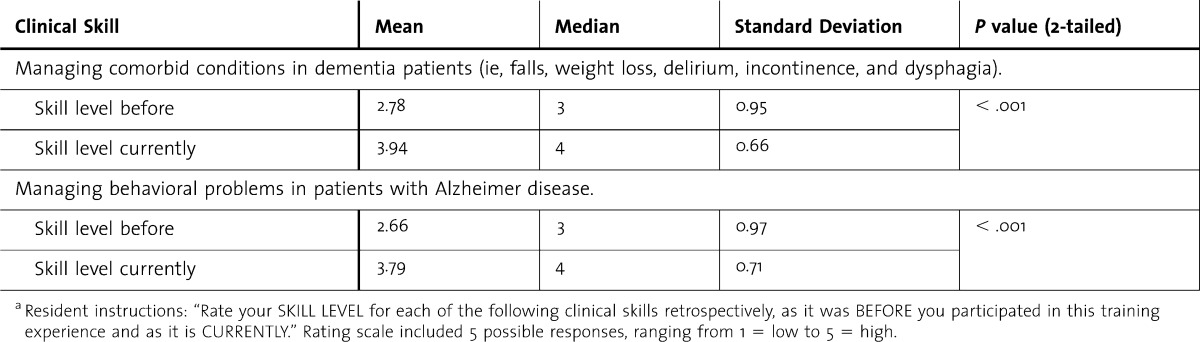
SP Ratings of Resident Performance at Sessions 1 and 3
Patient SP Role
There was a statistically significant positive change in the total score from session 1 (mean 43.31, SD = 6.72) to session 3 (mean 49.28, SD = 6.49); P < .005. Significant improvement was also seen in 6 items as rated by the “patient” SP (table 2). Of note, the only rating that decreased from the initial to the final session was related to whether the resident “included me in the discussion.” These results may be explained by the nature of the portrayed clinical scenario; in the third session, the patient is portrayed as having advanced AD, and the residents accordingly take the most of the history from the caregiver, in contrast with session 1, where the patient's cognition is more intact and she is typically the principal historian. This portrayed disease progression may explain the finding that residents were rated as less likely to include the patient in the discussion in the third session.
TABLE 2.
Selected Standardized Patient Ratings of Resident Performance at Sessions 1 and 3
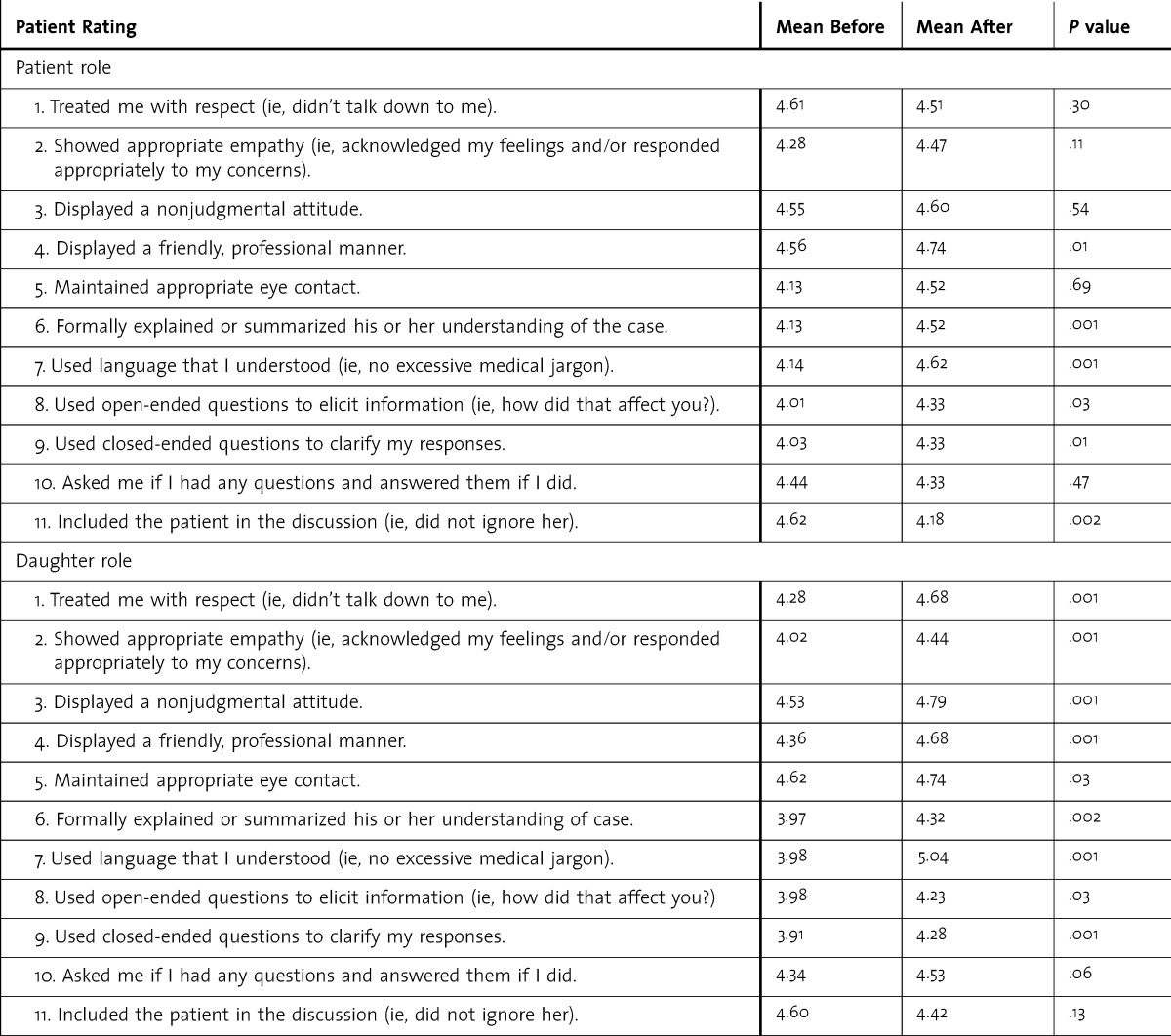
Daughter SP Role
There was a statistically significant positive change in the total score from session 1 (mean, 46.78; SD, 6.18) to session 3 (mean, 50.20; SD, 7.76) (P < .005). Significant improvement was also seen in 8 individual items as rated by the “daughter” SP (table 2).
Participants' Evaluation of the Curriculum
During academic years 2007 to 2010, 98% (131 of 134 residents) rated this training program as either “excellent” or “above average” compared to other learning activities and “agreed” or “strongly agreed” that the SPs' portrayals of the clinical scenario appeared realistic, and 96% (129 of 134 residents) “agreed” or “strongly agreed” that the experience “has helped to enhance my clinical competency in the care of older adults.”
Residents' mean ratings of the educational value of each curriculum component (where n = 134, 4 = “extremely valuable”) were as follows: SP clinical encounters, 3.56, SD = 0.64; SP verbal feedback sessions, 3.45, SD = 0.74; faculty case discussions, 3.47, SD = 0.69; video review activities, 2.99, SD = 1.18; printed handouts, 3.22, SD = 0.83; and lectures, 3.3, SD = 0.77. No statistical differences were revealed by subanalysis of educational value ratings as related to PGY, previous SP experience, specific residency program, or intention to provide primary care to older adults in future practice.
Implementation Costs
The primary cost of developing the curriculum is creation of the cases and faculty training manual. The ongoing costs for the SPs and teaching faculty for teaching are relatively small and have been supported by the participating residency programs and ongoing support of the Office of Geriatric Medicine. Options exist for “lower tech” implementation of this curriculum, such as forgoing videotaped monitoring of the SP stations. That change could preserve the opportunity for residents to receive feedback from the SPs on their performance while eliminating the lesser-valued video review exercises. Further evaluation of the effects of this approach and research into its applications for teaching and assessing chronic disease/geriatric medicine competencies are needed.
Discussion
We describe the successful implementation of a new chronic disease management/geriatric medicine curriculum using SPs. Participating resident physicians found this SP curriculum using a longitudinal dementia case to be both realistic and valuable compared to other learning activities in residency. Residents improved in both self-perceived dementia knowledge and communication abilities, as perceived by both self-report and SP evaluation. The SPs' evaluations revealed that residents' use of patient-centered language and professionalism improved.
Other educators have used SPs to assess geriatric medicine skills among residents.12–14 Our curriculum has the distinguishing feature of a longitudinal clinical experience between learners and SPs/daughters over multiple SP sessions representing a single unfolding dementia case. Studies have shown that SPs are at least as effective as faculty in teaching the medical interview to first-year medical students15 and that SP encounters can be a useful tool in teaching medical students the art of communicating.16 There are few published studies of using SPs for providing formative evaluation of residents' chronic disease or geriatric clinical skills. SP encounters have been used to evaluate residents' skills in end-of-life discussions before and after a single intervention consisting of lecture, discussion, and SP interaction demonstrating statistically significant improvements in delivery of bad news.17,18 A study of an intervention using an unfolding SP case across 4 years of medical school elicited positive ratings from students; however, no data exist for the value of such an experience for residents.19 Our educational intervention's blend of a simulated 10-year clinical experience with an SP and caregiver to teach geriatric competencies with the provision of formative feedback to resident physicians on communication skills is unique in the literature.
Our curriculum and SP intervention were effective in teaching professionalism, use of patient-centered language, and effective use of open-ended questions, as rated by SPs. The effect of our curriculum was small mainly because of an observed ceiling effect with the data. Future instruments could potentially be redesigned for upper level residents who are more advanced in communication skills. Our curriculum targets specific geriatric competencies and additional competencies critical to the professional development of resident physicians. SPs' performance ratings of residents' observed interpersonal skills were highly favorable and significantly improved from the first to third sessions, indicating a potentially efficacious method for teaching these critically important skills. The residents valued their SP clinical encounters over all the other teaching methods used in this curricular innovation. This result, combined with the favorable ratings the SPs received from the residents for the realism of their case portrayal, reinforces the authors' impression that the strong performance of the SPs, both as patients and teachers, contributed substantively to this program's educational value. Residents found the video reviews least valuable, and we speculate including multiple video reviews in a curriculum that already featured highly valued SP feedback provided only marginal added educational value.
Our finding that 54% (72 of 134) of resident participants had little or no experience with providing medical care to older adults with dementia suggests that despite increasing residency geriatric training requirements, progress may have been limited since a 2001 study found that only half of internal medicine and family medicine residents reported feeling prepared to care for older adults at the time of graduation.20
Limitations of our intervention include lack of formal validity testing for the tools used to self-evaluate resident performance and SPs feedback, although faculty and SP feedback from the first year of experience was incorporated into revised tools in 2006. The self-efficacy results in this study should be interpreted with caution as they are subjective, and we did not include a control group.
Conclusion
Resident physicians found this SP-based curriculum using a longitudinal dementia case both realistic and valuable. Residents improved in both self-perceived knowledge of dementia as well as communication abilities, as perceived by both self-report and SP evaluation. The use of SPs in a longitudinal clinical encounter can be an effective way to teach about chronic disease management and core residency communication skills competencies.
Footnotes
Jeffrey D. Schlaudecker, MD, is Assistant Professor, Department of Family and Community Medicine, University of Cincinnati College of Medicine; Timothy J. Lewis, MD, is Geriatrician, Post-Acute and Senior Services, Health Services Research and Education Institute, Summa Health System; Irene Moore, MSW, is Professor, Geriatric Medicine Program, University of Cincinnati College of Medicine; Harini Pallerla, MS, is Senior Research Assistant, Department of Family and Community Medicine, University of Cincinnati College of Medicine; Anna M. Stecher, BS, is a medical student, University of Cincinnati College of Medicine; Nathan D. Wiebracht, BA, is a medical student, University of Cincinnati College of Medicine; and Gregg A. Warshaw, MD, is Martha Betty Semmons Professor of Geriatric Medicine and Professor of Family and Community Medicine, University of Cincinnati College of Medicine.
Funding: This work was supported by the Bureau of Health Professions Geriatric Academic Career Award (J.D.S., T.J.L.) and the Donald W. Reynolds Foundation grant Strengthening Geriatric Education and Care of the Elderly in the Greater Cincinnati Tri-State Area.
The authors thank Patricia Hatchett and Maureen Asebrook for assistance in working with the University of Cincinnati's Center for Competency Development and Assessment. Sharon Harding provided valuable administrative support. Karthikeyan Meganathan provided valuable statistical analysis and oversight. The authors also acknowledge our profoundly dedicated group of standardized patients, who brought the unfolding case to life with passion, conviction, and credibility. The standardized patient training materials, instructor's manual, assessment instruments, and trainees' written exercises are available from the authors upon request.
References
- 1.Institute of Medicine, Committee on Strengthening the Geriatrics Content of Medical Training. Strengthening Training in Geriatrics for Physicians. Washington, DC: National Academies Press; 1993. [Google Scholar]
- 2.Bragg EJ, Warshaw GA. ACGME requirements for geriatrics medicine curricula in medical specialties: progress made and progress needed. Acad Med. 2005;80(3):279–285. doi: 10.1097/00001888-200503000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Williams BC, Warshaw G, Fabiny AR, Lundebjerg Mpa N, Medina-Walpole A, Sauvigne K, et al. Medicine in the 21st century: recommended essential geriatrics competencies for internal medicine and family medicine residents. J Grad Med Educ. 2010;2(3):373–383. doi: 10.4300/JGME-D-10-00065.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas DC, Leipzig RM, Smith LG, Dunn K, Sullivan G, Callahan E. Improving geriatrics training in internal medicine residency programs: best practices and sustainable solutions. Ann Intern Med. 2003;139(7):628–634. doi: 10.7326/0003-4819-139-7-200310070-00037. [DOI] [PubMed] [Google Scholar]
- 5.American Geriatrics Society. Curriculum guidelines on the care of the elderly for internal medicine residency training programs. New York, NY: American Geriatrics Society; 1996. [Google Scholar]
- 6.Core competencies for the care of older patients: recommendations of the American Geriatrics Society. The Education Committee Writing Group of the American Geriatrics Society. Acad Med. 2000;75(3):252–255. [PubMed] [Google Scholar]
- 7.Swenson SL, Chou C, Satterfield JM, Frankel RM. Using Videotapes as Tools for Teaching Patient-Centered Care. Workshop F10, Society of General Internal Medicine, Chicago, IL, Saturday, May 15, 2004. [Google Scholar]
- 8.Edwards A, Tzelepis A, Klingbeil C, Melgar T, Speece M, Schubiner H, et al. Fifteen years of a videotape review program for internal medicine and medicine-pediatrics residents. Acad Med. 1996;71(7):744–748. doi: 10.1097/00001888-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Howard GS, Ralph KM, Gulanick NA, Maxwell SE, Nance DW, Gerber SK. Internal invalidity in pretest-posttest self-report evaluations and a re-evaluation of retrospective pretests. Appl Psych Meas. 1979;3:1–23. [Google Scholar]
- 10.Skeff KM, Stratos GA, Bergen MR. Evaluation of a medical faculty development program: a comparison of traditional pre/post and retrospective pre/post self-assessment ratings. Eval Health Prof. 1992;15:350–366. [Google Scholar]
- 11.Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychol Methods. 1996;1:170–177. [Google Scholar]
- 12.Ainsworth MA, Rogers LP, Markus JF, Dorsey NK, Blackwell TA, Petrusa ER. Standardized patient encounters. A method for teaching and evaluation. JAMA. 1991;266(10):1390–1396. doi: 10.1001/jama.266.10.1390. [DOI] [PubMed] [Google Scholar]
- 13.Nagoshi M, Williams S, Kasuya R, Sakai D, Masaki K, Blanchette PL. Using standardized patients to assess the geriatrics medicine skills of medical students, internal medicine residents, and geriatrics medicine fellows. Acad Med. 2004;79(7):698–702. doi: 10.1097/00001888-200407000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Karani R, Leipzig RM, Callahan EH, Thomas DC. An unfolding case with a linked Objective Structured Clinical Examination (OSCE): a curriculum in inpatient geriatric medicine. J Am Geriatr Soc. 2004;52(7):1191–1198. doi: 10.1111/j.1532-5415.2004.52321.x. [DOI] [PubMed] [Google Scholar]
- 15.Vannatta JB, Smith KR, Crandall S, Fischer PC, Williams K. Comparison of standardized patients and faculty in teaching medical interviewing. Acad Med. 1996;71(12):1360–1362. doi: 10.1097/00001888-199612000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Rose M, Wilkerson L. Widening the lens on standardized patient assessment: what the encounter can reveal about the development of clinical competence. Acad Med. 2001;76(8):856–859. doi: 10.1097/00001888-200108000-00023. [DOI] [PubMed] [Google Scholar]
- 17.Alexander SC, Keitz SA, Sloane R, Tulsky JA. A controlled trial of a short course to improve residents' communication with patients at the end of life. Acad Med. 2006;81(11):1008–1012. doi: 10.1097/01.ACM.0000242580.83851.ad. [DOI] [PubMed] [Google Scholar]
- 18.Szmuilowicz E, el-Jawahri A, Chiappetta L, Kamdar M, Block S. Improving residents' end-of-life communication skills with a short retreat: a randomized control trial. J Palliat Med. 2010;13(4):439–452. doi: 10.1089/jpm.2009.0262. [DOI] [PubMed] [Google Scholar]
- 19.Rull G, Rosher RB, McCann-Stone N, Robinson SB. A simulated couple aging across the four years of medical school. Teach Learn Med. 2006;18(3):261–266. doi: 10.1207/s15328015tlm1803_12. [DOI] [PubMed] [Google Scholar]
- 20.Blumenthal D, Gokhale M, Campbell EG, Weissman JS. Preparedness for clinical practice: reports of graduating residents at academic health centers. JAMA. 2001;286(9):1027–1034. doi: 10.1001/jama.286.9.1027. [DOI] [PubMed] [Google Scholar]