Abstract
Nevus comedonicus is an uncommon skin abnormality characterized by an aggregation of dilated follicular orifices filled with keratinous material. Nevus comedonicus is occasionally complicated with other conditions including cataracts, skeletal defects, central nervous system abnormalities or other extra-cutaneous diseases (nevus comedonicus syndrome). Although most cases of nevus comedonicus occur unilaterally on the face, neck and chest, the lesions occasionally show a bilateral distribution (bilateral nevus comedonicus). We report here an unusual case of bilaterally disseminated nevus comedonicus with various systemic complications. A 62-year-old Japanese man presented with a 50-year history of numerous keratotic papules and comedo-like lesions, which gradually worsened with time. Physical examination revealed that the papules were skin-colored and 1–4 mm in diameter. Some papules had dark-black keratinous materials on their surface, giving them a comedo-like appearance. The lesions were located predominantly on the face, head, neck and trunk with symmetric distribution, following Blaschko’s lines. The patient’s past medical history was noteworthy; he had undergone surgical treatments for thyroid cancer, pneumothorax and schwannoma in the cauda equina. He also suffered from scoliosis, cervical spondylosis and atrial fibrillation. Histopathologic examination revealed dilated and invaginated follicular structures filled with lamellar keratin, compatible with nevus comedonicus. Our patient’s case did not fit with any previously reported diseases, and we thought a diagnosis of “bilateral nevus comedonicus syndrome” was the most appropriate for our patient’s condition. He was treated with topical retinoic acid and activated vitamin D3 ointment for 3 months each, but the lesions remained unchanged.
Keywords: nevus comedonicus, nevus comedonicus syndrome, schwannoma, thyroid tumor
Nevus comedonicus is an uncommon skin abnormality characterized by an aggregation of dilated follicular orifices filled with keratinous material.1 In some cases, nevus comedonicus is complicated with other conditions, such as cataracts, skeletal defects, central nervous system abnormalities or various other non-cutaneous conditions (nevus comedonicus syndrome).2 Although most cases of nevus comedonicus occur unilaterally on the face, neck and chest, they occasionally show a bilateral distribution (bilateral nevus comedonicus).3 We report here an unusual case of bilaterally disseminated nevus comedonicus with various systemic complications.
PATIENT REPORT
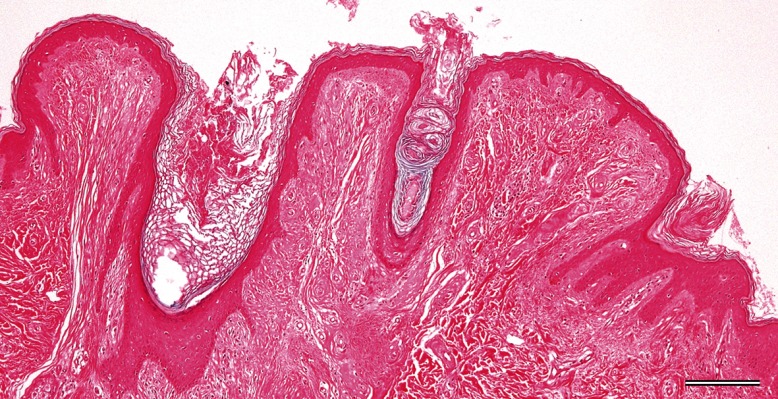
A 62-year-old Japanese man was referred to our hospital with a 50-year history of numerous keratotic papules and comedo-like lesions, which gradually worsened with time. Physical examination revealed that the papules were skin-colored and 1–4 mm in diameter. Some papules had dark-black keratinous materials on their surface, giving them a comedo-like appearance. The lesions were located predominantly on the face, head, neck and trunk with symmetric distribution, following Blaschko’s lines (Fig. 1). Extremities, including hands, feet and nails, as well as mucous membranes were spared. The patient did not complain of any symptoms. Family history and routine laboratory studies were unremarkable, while his past medical history was noteworthy; he had undergone surgical treatments for thyroid cancer, pneumothorax and schwannoma in the cauda equina. He has also suffered from scoliosis, cervical spondylosis and atrial fibrillation. We performed punch biopsy of the lesion on the neck. Histopathologic examination revealed dilated and invaginated follicular structures filled with lamellar keratin, in accordance with the features of nevus comedonicus (Fig. 2). Based on these findings, we thought a diagnosis of “bilateral nevus comedonicus syndrome” was the most appropriate for our patient’s condition. He was treated with topical retinoic acid and activated vitamin D3 ointment for 3 months each, but the lesions remained unchanged.
Fig. 1.
Many skin-colored papules and comedo-like lesions on the neck.
Fig. 2.
Dilated and invaginated follicular structures filled with lamellar keratin (hematoxylin and eosin staining). Bar = 1000 µm.
Discussion
Since the first description by Kofmann,1 about 200 cases of nevus comedonicus have been reported, though bilateral nevus comedonicus and nevus comedonicus syndrome have been reported only sporadically. Our patient’s case is of interest in that it showed bilaterally disseminated comedo-like lesions with various systemic complications. The skin lesions were clinically and histopathologically compatible with bilateral nevus comedonicus. To our knowledge, bilateral nevus comedonicus accompanied by systemic complications as found in our patient has not been reported in the English literature.
To make a diagnosis of “bilateral nevus comedonicus syndrome”, we should rule out other diseases showing multiple comedo-like lesions or skin-colored papules such as acne vulgaris, chloroacne, Favre-Racouchot disease, familial dyskeratotic comedones, idiopathic disseminated comedones, disseminated congenital comedones, multiple congenital comedones, verruca vulgaris and Apert syndrome.
Acne vulgaris is a common disease that should be considered as a differential diagnosis. The diagnosis of acne vulgaris is usually made from the clinical finding of a mixture of acne lesions such as comedones, papules, pustules, nodules and hypertrophic scars.4 It is seen primarily in adolescents and usually lacks systemic complications. Therefore, acne vulgaris is not the perfect diagnosis for our patient. Chloracne, caused by halogenated chemical compounds, is a well-known dermatosis consisting of diffuse acneiform lesions with diffuse grayish skin pigmentation,5 but our patient had no history of exposure to halogenated chemical compounds or other acnegenic substances. Favre-Racouchot disease is a cutaneous disorder with grouped comedones in sun-damaged skin.6 The lesions are usually symmetrically distributed without developing inflammation, but the locations of this disease are confined to sun-exposure areas. Familial dyskeratotic comedones is a rare abnormality characterized by symmetrically scattered comedo-like hyperkeratotic papules.7 It is inherited as an autosomal dominant condition, which can distinguish it from our case. Idiopathic disseminated comedones is a good candidate diagnosis for our patient. It is a rare entity clinically characterized by symmetrically scattered comedo-like hyperkeratotic papules on the trunk, arms and legs.8 Histopathologically, crateriform cysts containing hyperkeratotic debris and peri-infundibular inflammatory infiltrate are seen. These histopathologic features, however, were not evident in our patient. Moreover, there has been only one case report of this disease so far. Disseminated congenital comedones was described by Galvan in a 3-month-old boy who had congenital and extensive skin comedones confined to the upper half of the body.9 Our case can be differentiated from this disease because of the distribution and onset age of comedones. Multiple congenital comedones is a recently described condition showing congenital bilateral comedones and some systemic complications.10 Our case does not fit with this disease because of the onset of comedones. Verruca vulgaris sometimes occurs as multiple skin-colored lesions,11 but this disease can be clearly discriminated from ours histopathologically. Apert syndrome, characterized by craniosynostosis, mid-facial malformations, symmetrical syndactyly and severe acne vulgaris, does not accord with the features of our patient.12 After excluding the diseases mentioned above, we concluded that “bilateral nevus comedonicus syndrome” is the most appropriate term reflecting our patient’s condition.
The authors declare no conflict of interest.
REFERENCES
- 1.Kofmann S. Ein fall von seltener localisation und verbreitung von komedonen. Arch Dermatol Syphilol. 1895; 32: 177 [Google Scholar]
- 2.Engber PB. The nevus comedonicus syndrome: a case report with emphasis on associated internal manifestations. Int J Dermatol. 1978; 17: 745-749 [DOI] [PubMed] [Google Scholar]
- 3.Paige TN, Mendelson CG. Bilateral nevus comedonicus. Arch Dermatol. 1967; 96: 172-175 [PubMed] [Google Scholar]
- 4.Thiboutot DM, Stauss JS Diseases of the sebaceous glands In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's Dermatology in General Medicine. New York: McGraw-Hill; 2003. p. 672-687 [Google Scholar]
- 5.Passarini B, Infusino SD, Kasapi E. Chloracne: Still cause for concern. Dermatology. 2010; 221: 63-70 [DOI] [PubMed] [Google Scholar]
- 6.Patterson WM, Fox MD, Schwartz RA. Favre-Racouchot disease. Int J Dermatol. 2004; 43: 167-169 [DOI] [PubMed] [Google Scholar]
- 7.Caneiro SJC, Dickson JE, Knox JM. Familial dyskeratotic comedones. Arch Dermatol. 1972; 105: 249-251 [PubMed] [Google Scholar]
- 8.Zhang RZ, Zhu WY. Idiopathic disseminated comedones in a child. Pediatr Dermatol. 2006; 23: 163-166 [DOI] [PubMed] [Google Scholar]
- 9.Veno-Galvan S, Hernandez-Martin A, Colmenero I, Torrelo A. Disseminated congenital comedones. Pediatr Dermatol. 2011; 28: 58-59 [DOI] [PubMed] [Google Scholar]
- 10.Ito T, Yoshida Y, Furue M, Yamamoto O. Multiple congenital comedones, hearing impairment and intellectual disability: a new syndromic association?. Eur J Dermatol. 2012; 22: 807-808 [DOI] [PubMed] [Google Scholar]
- 11.Ito T, Yoshida Y, Adachi K, Furue M, Yamamoto O. Wart with depigmented halo and generalized vitiligo. Yonago Acta Medica. 2012; 55: 81-82 [PMC free article] [PubMed] [Google Scholar]
- 12. Harper JI, Trembath RC Genetics and genodermatoses In: Burns T, Bresthnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Massachusetts: Blackwell Publishing; 2004. p. 12.75 [Google Scholar]