Abstract
A cross-sectional, community-based study was performed in 2012 with 428 residents of periurban shantytowns in Lima, Peru to study risk factors for and changes in latent tuberculosis infection in age-stratified groups compared with our data from the same region in 1990 (N = 219) and 2005 (N = 103). Tuberculin skin test positivity in these communities was highly prevalent at 52% overall, increased with age (P < 0.01) and was similar to 2005 (53%) and 1990 (48%). From 1990 to 2012, the prevalence of tuberculin positivity decreased in 5–14 and 15–24 year old groups (to 17% and 34%, respectively, both P < 0.05). However, this may be explained by cessation of Bacille Calmette-Guérin revaccination during this period, because Bacille Calmette-Guérin revaccination doubled tuberculin positivity. Over the same 22-year period, tuberculin positivity in the ≥ 25 year old group remained high (71%, P = 0.3), suggesting that prevalent latent tuberculosis infection persists in the adult population despite improving medical care and socioeconomic development in this region.
Introduction
The World Health Organization (WHO) estimates that the global tuberculosis (TB) mortality is 1.4 million persons per year and developing countries account for 98% of these deaths.1,2 After human immunodeficiency virus (HIV) infection, TB causes more deaths worldwide than any other infectious disease.3 Globally, one-third of the world population, more than two billion people, are estimated to have acquired latent Mycobacterium tuberculosis infection and 8.9 million people each year become ill with TB disease.1,3
The main risk factor for TB infection is exposure to someone infected with active M. tuberculosis disease. Poor living and health conditions increase the risk of such exposure causing TB infection and of this latent infection progressing to active TB disease.3 Without treatment, patients with active TB disease are estimated to infect 10–15 people per year on average.4 In Peru, strengthening of the national tuberculosis control program, universalization of directly observed treatment short course and socioeconomic development were associated with a reduction in the estimated incidence of TB disease per 100,000 people5 from 317 in 1990 to 106 in 2010.1 Despite this, Peru is among the highest three countries in the Americas for TB incidence, mortality, and drug resistance rates.1,6
One aspect of the TB burden in Peru that has not been addressed adequately is the prevalence of latent TB infection as indicated by the Mantoux tuberculin skin test (TST) positivity. The community prevalence of TST positivity is an important indicator of TB control because it is not confounded by changes in TB case finding that can considerably increase or decrease estimates of the incidence of TB disease.5 In TB-endemic countries such as Peru, the TST is the only widely used method for diagnosing latent infection, especially in children7–10 despite difficulty interpreting results in subjects who have received the Bacille Calmette-Guérin (BCG) vaccine. The great majority of children in Peru receive the BCG vaccine at birth. Pelly and others found that 90% of Peruvians had BCG scars (many with multiple scars) in two areas of Peru,11 consistent with studies elsewhere.12–14 Several previous studies have suggested that the prevalence of TST positivity in Lima was comparable with impoverished communities in other countries.12,13
To address this knowledge gap concerning changes in latent TB infection associated with apparent reductions in TB disease rates we completed a cross-sectional study in periurban shantytowns in Lima, Peru, determining the prevalence of TST positivity. We then compared our results to two previous cross-sectional studies in the years 199013 and 200511 in the same study location.
Methods
Study design and setting.
We conducted a community-based cross-sectional study and our goals were to characterize:
-
1)
changes in the age-stratified prevalence of TST positivity over 20 years; and
-
2)
risk factors for TST positivity.
Participants were 5 years of age and older and lived in Pampas de San Juan de Miraflores, in Southern Lima, Peru, an impoverished cluster of periurban shantytowns with an approximate population of 57,000 people according to a recent census. The population has grown consistently because of internal migration in Peru from rural to urban areas in recent decades.15 This migration principally of the Andean peoples to Lima contributed to a greater genetic mixture than other cities.16 Pampas is very crowded, potentially increasing the risk of M. tuberculosis transmission. Residents of this region generally live in small, cramped houses, and there is limited access to medical care compared with other areas of Lima.
Participants.
Potential participants were identified using the information from a census performed in the year 2000 by a local non-governmental organization Asociacion Benefica Proyectos en Informatica, Salud, Medicina, y Agricultura (AB PRISMA), from which an age-stratified sample was drawn (three age strata were considered: 5–14, 15–24, and ≥ 25 years of age). Pregnant women were excluded from the study.
Sample size.
Sample size for the study was calculated for each of the age-strata based on the pre-specified hypotheses regarding the magnitude of the variation of the prevalence of TST positivity since 1990. Specifically, for the age group of 5–14 years, we hypothesized a reduction in the prevalence of TST positivity by at least half (from 23% to 12%),13 at least 25% for the other two age groups (15–24 and ≥ 25 years).13 These hypotheses are based on improvements in several risk factors for TB in Peru, including decreasing rates of diagnosed TB disease, and probable decreases in poverty, malnutrition, and crowding. All sample size calculations considered a significance level of 0.05, and a power of 0.8. Based on these parameters, the sample size needed for the 5–14 years age group was 100 children; whereas for the other two age groups, the combined sample size needed was 296 persons. Predicting a 15% rejection rate, we therefore enrolled 460 participants.
Of the 460 participants enrolled in the study, 28 (6%) reported a prior diagnosis of active TB and 4 (1%) could not be located for reading the result of the TST. After excluding these groups, there were 428 (93%) participants available for analysis.
Data collection.
The study took place between July 2011 and January 2012, through a minimum of four home visits to each participant. If the participant was not available at any of the scheduled visits, a field worker visited the participant daily until he or she was found or until it was determined that he or she no longer wished to participate in the study.
Socio-demographic and health questionnaires.
Socio-demographic and health questionnaires were completed by all participants during the first visit. The questionnaire took 15–20 minutes to complete and assessed risk factors including current health, prior TB exposure, living conditions, occupation, socioeconomic status, length of time residing in this community, history of a positive TST, and prior TB treatment. The number of BCG scars on both arms was counted. Weight and height were measured, body mass index (BMI) was categorized for adults17 and for children z-scores were calculated.18
TST and tetanus toxoid control.
The TST and tetanus toxoid procedures were based on those used in Getchell and others (1992). The TST positivity was determined using purified protein derivative (PPD, Aplisol, JHP Pharmaceuticals, LLC, Rochester, MI) that was administered on the volar surface of the forearm during the second visit. The 1992, 2005, and this study used 5 tuberculin units (TU) in 0.1 mL. At the same time, a similar intradermal test using 0.1 mL tetanus toxoid (1 Lf, Sanofi Pasteur, product no. 49281-820-10) was administered on the volar surface of the opposite arm to test for immune anergy. This dose is one-fifth of the recommended dose for immunization, and was the same as the 1992 study but half the dose used in the 2005 study.11,13 To prevent observer bias, all syringes were identical except for color-coded stickers and field workers were blinded as to the content of the syringes and which antigen and where the antigen was injected. The color code was assigned daily by a study investigator, who pre-loaded the 25-guage syringes and stored them at 4°C until use.
TST and tetanus toxoid test readings.
The TST and tetanus toxoid test readings were done by both a trained nurse and a field worker on the third study visit 48–72 hours after injection. The results were measured as the horizontal diameter of induration around the test application site in each arm, using the ball-point pen method, and were recorded to the nearest millimeter. This method has been proven accurate and has little discrepancy between observers.19
The fourth visit, to each participating household, involved delivering and explaining the results of the evaluation. All participants with positive TST results and two or more symptoms (unintentional weight loss, cough for greater than 2 weeks, fever, or night sweats) were further investigated and were referred for a chest x-ray and sputum sample as part of the follow-up. The sputum sample was tested with microscopy and the microscopic-observation drug-susceptibility (MODS) culture.20–23 Because of the known low specificity of the TST for TB disease, subjects with a positive TST result but with fewer than two symptoms were not further investigated.
In accordance with Peruvian policies and the Centers for Disease Control and Prevention (CDC) recommendations for the diagnosis of latent TB infection in immune-competent individuals from a country with a high prevalence of TB, we defined a positive TST result as a horizontal induration diameter ≥ 10 mm.24 Furthermore, for additional comparisons with previous reports, we divided less reactive TST results (< 10 mm), into negative (0–4 mm induration) and borderline (5–9 mm induration).2,11,13
Ethical approval.
This study received ethical approval by Institutional Review Board committees of Tulane University, New Orleans, LA and AB PRISMA, Lima, Peru. Adult participants gave verbal and written consent and participants < 18 years of age gave assent supported by written consent from a parent or guardian.
Data analysis.
All analyses were performed using STATA/IC 11.0 for Windows (StataCorp LP, College Station, TX, 2010). For univariate analyses, we computed the central tendency and dispersion summary statistics, and evaluated the distribution and presence of outliers using graphical and numerical methods. For bivariate analyses, we compared the distribution of socio-demographic and clinical characteristics by categories of TST size. We used analysis of variance and the Kruskal-Wallis test for continuous variables, and the χ2 test and Fisher's exact test for categorical variables. For multivariate analyses, we used a binary logistic regression model (TST positive versus negative), to estimate the odds ratio (OR) of TST positivity by socio-demographic and clinical characteristics, after adjusting for potential confounders. We modeled data using graphical methods, and assessed the model fit using the normal approximation of the Pearson's χ2 statistic and the Hosmer-Lemeshow goodness-of-fit statistic.25 We centered all continuous predictors to enhance the interpretability of the logistic regression models. Age-specific prevalences of TST positivity was calculated from a binary logistic regression model. Annual risk of infection was calculated using a standard formula.26,27 The adjusted population attributable fraction of TST positivity from two or more BCG vaccinations were calculated using the methods proposed by Rockhill and others28 and Zhang and others.29 All tests were two-sided and considered 95% confidence intervals (CIs) and a significance level of 5%.
Results
Table 1 shows the socio-demographic and clinical characteristics of the 428 participants. 67 (16%) were from the 15–24 age group, 103 (24%) aged 5–14 years, and 258 (60%) ≥ 25 years of age. Fifty-one percent (51%) were female and were a median of 33 years of age (semi-interquartile range: 19 years). The majority of our study had a high school education and had low socio-economic position. Nearly all of the participants had a BCG scar (99%), and most shared their bedroom with another person (53%). A minority were overweight (32%) or obese (19%), lived in a poorly ventilated house (21%), and had lived in the past 5 years with a person diagnosed with TB (9%).
Table 1.
Characteristics of the study population, 2012 (N = 428)
| Characteristic | n | Proportion (95% CI)* |
|---|---|---|
| Gender | ||
| Male | 208 | 48.9 (43.8, 53.4) |
| Female | 220 | 51.4 (46.6, 56.2) |
| Age (years)† | 32.7 (18.9) | |
| Age category | ||
| 5–14 years | 103 | 24.1 (20.1, 28.4) |
| 15–24 years | 67 | 15.7 (12.3, 19.4) |
| ≥ 25 years | 258 | 60.3 (55.5, 64.9) |
| BCG scars | ||
| 0 | 2 | 0.5 (0.1, 2.0) |
| 1 | 196 | 45.8 (41.0, 50.6) |
| 2 | 131 | 30.6 (26.3, 35.2) |
| 3+ | 99 | 23.1 (19.2, 27.4) |
| BMI category - adults‡ | ||
| Underweight | 3 | 1.0 (0.2, 2.9) |
| Normal weight | 88 | 29.5 (24.4, 35.1) |
| Overweight | 130 | 43.6 (37.9, 49.5) |
| Obese | 77 | 25.8 (21.0, 31.2) |
| BMI category - children§ | ||
| Underweight | 3 | 2.3 (0.5, 6.6) |
| Normal weight | 79 | 61.2 (52.3, 69.7) |
| Overweight | 31 | 24.0 (16.9, 32.3) |
| Obese | 16 | 12.4 (7.3, 19.4) |
| Education level | ||
| None | 18 | 4.2 (2.5, 6.6) |
| Primary | 128 | 29.9 (25.6, 34.5) |
| Secondary | 192 | 44.9 (40.1, 49.7) |
| Superior | 90 | 21.0 (17.3, 25.2) |
| Basic service monthly expenditure (nuevos soles)†¶ | 168.5 (39.5) | |
| Persons/room ratio∥ | 2.0 (0.1) | |
| Reported house ventilation | ||
| Poor | 89 | 20.8 (17.0, 25.0) |
| Good | 339 | 79.2 (75.0, 83.0) |
| Lived with a person with TB in the past 5 years | ||
| Yes | 39 | 9.1 (6.6, 12.2) |
| No | 389 | 90.9 (87.8, 93.4) |
95% binomial exact confidence intervals (95% CI).
Median (semi-interquartile range).
BMI categories for adults were based on the WHO Classification.
BMI child categories were based on CDC 2000 Growth Reference (z-scores for age and sex).
Basic service expenditure was calculated as the sum of the monthly expenditure on electricity, water supply, and food (in nuevos soles).
Ratio (standard error), otherwise N.
TST= tuberculin skin test; BCG = Bacille Calmette-Guérin; BMI = body mass index; TB = tuberculosis.
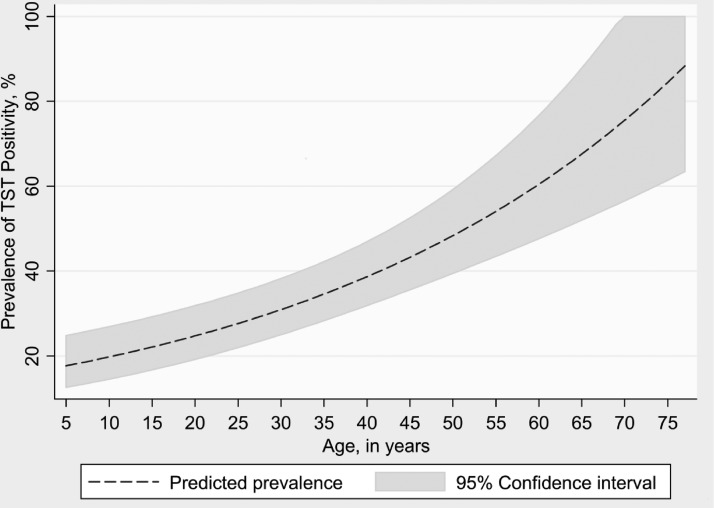
The overall prevalence of TST positivity in 2012 was 52% (95% CI: 48, 57%). The prevalence of TST positivity increased with age (P < 0.01, Figure 1 ), and the age-specific prevalence of TST positivity for the 5–14, 15–24, and ≥ 25 age groups were 17% (95% CI: 9.9, 25), 34% (95% CI: 23, 47), and 72% (95% CI: 65, 76), respectively. In 2012 the prevalence of borderline and positive TST results was higher than 1990 (P < 0.01, Table 2), but the prevalence of clearly positive TST results (≥ 10 mm) did not change significantly (52% versus 48%, P = 0.2). In 1990 only 33% of the population was aged > 25 years versus 60% in 2012 (P < 0.0001). From 1990 to 2012, TST positivity in the 5–14 age group decreased from 22% to 17% (P = 0.04, Table 2). From 1990 to 2005 TST positivity in the 15–24 age group decreased from 60% to 34% (P < 0.01), and remained at 34% in 2012 (Table 2). In the older age group (≥ 25 years of age) there were no significant changes in TST positivity prevalence (increased from 68% in 1990 to 71% in 2012, P = 0.3, Table 2).
Figure 1.
Prevalence of tuberculin skin test (TST) positivity by age among participants with one or no Bacille Calmette-Guérin (BCG) scars.
Table 2.
Comparison of TST results: 1990 and 2005 vs. 2012
| TST Result | Getchell and others, 199213 | Pelly and others, 200511 | Martinez and others, 2013 (Reference) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Negative(0–4 mm) | Borderline(5–9 mm) | Positive(≥ 10 mm) | P value vs. 2012† | n | Negative(0–4 mm) | Borderline(5–9 mm) | Positive(≥ 10 mm) | P value vs. 2012† | n | Negative(0–4 mm) | Borderline(5–9 mm) | Positive(≥ 10 mm) | ||
| Age group | |||||||||||||||
| 5–14 years | 89 | 56 (62.9) | 13 (14.6) | 20 (22.4) | 0.04* | – | – | – | – | – | 103 | 55 (53.4) | 31 (30.1) | 17 (16.5) | |
| 15–24 years | 58 | 16 (27.6) | 7 (12.1) | 35 (60.4) | < 0.01** | 35 | 23 (65.7) | 0 (0.0) | 12 (34.3) | < 0.01** | 67 | 25 (37.3) | 19 (28.4) | 23 (34.3) | |
| ≥ 25 years | 72 | 16 (22.2) | 7 (9.7) | 49 (68.1) | 0.25 | 68 | 18 (26.5) | 7 (10.3) | 43 (63.2) | 0.08 | 258 | 38 (14.7) | 36 (14.0) | 184 (71.3) | |
| All | 219 | 88 (40.1) | 27 (12.3) | 104 (47.5) | < 0.01** | 103 | 41 (39.8) | 7 (6.8) | 55 (53.4) | < 0.01** | 428 | 118 (25.6) | 86 (20.1) | 224 (52.3) | |
Figures are number of participants per age category (%).
P < 0.05.
P < 0.01.
P values refer to the comparison between the age-specific prevalences of each of the tuberculin skin test (TST) result categories reported by Martinez and others, 2012 (reference) and those reported by Getchell and others, 199213 and Pelly and others, 2005,11 respectively.
TST= tuberculin skin test.
Only two participants did not have Bacille Calmette-Guérin (BCG) scars (0.05%), of whom one had a negative TST (50%) and the other had a positive TST (50%). Because of the small number of observations, we did not further stratify the TST results by number of BCG scars (0 vs. ≥ 1 BCG scar).
There were few differences in TST results between data from our study and 2005,11 when the 5–14 age group was not studied. Thirty-four percent (34%) of the 15–24 age group were TST positive in 2005 and 2012, whereas 71% of the ≥ 25 age group were positive in 2012 compared with 63% in 2005 (P = 0.08). In 2012 there were 28% and 14% borderline TST results for the 15–24 age group and ≥ 25 age group, more than in 2005 (0% and 9.9%, respectively).
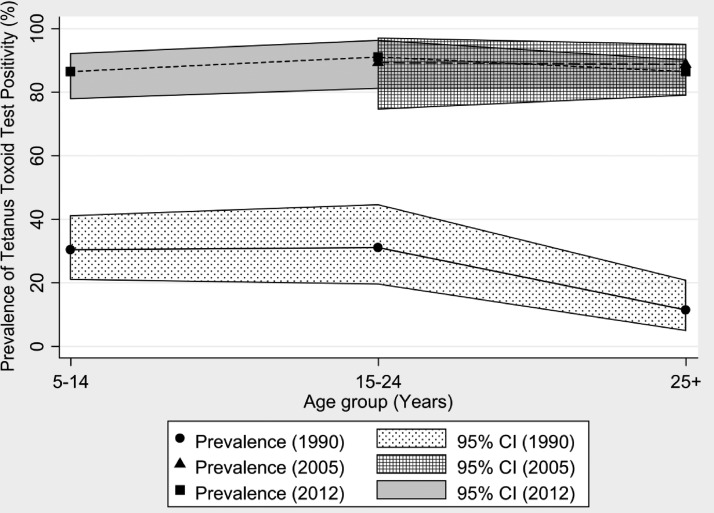
Tetanus skin test positivity rates increased from 1990 to 2012 (24–87%, P < 0.01, Table 3). The 2012 data were similar to 2005, when a higher dose of tetanus toxoid was used (Table 3). Tetanus skin test positivity was not significantly associated with participant age (Figure 2).
Table 3.
Comparison of tetanus toxoid test results: 1990 and 2005 vs. 2012
| Tetanus Toxoid Test Result | Getchell and others, 199213 | Pelly and others, 200511 | Martinez and others, 2012 (Reference) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Negative(0–4 mm) | Borderline(5–9 mm) | Positive(≥ 10 mm) | P value† | n | Negative(0–4 mm) | Borderline(5–9 mm) | Positive(≥ 10 mm) | P value† | n | Negative(0–4 mm) | Borderline(5–9 mm) | Positive(≥ 10 mm) | ||
| Age group | |||||||||||||||
| 5–14 years | 89 | 35 (39.3) | 27 (30.3) | 27 (30.3) | < 0.01** | – | – | – | – | – | 103 | 2 (1.9) | 12 (11.7) | 89 (86.4) | |
| 15–24 years | 58 | 30 (51.7) | 10 (16.3) | 18 (31.0) | < 0.01** | 35 | 1 (2.9) | 3 (8.6) | 31 (88.6) | 0.52 | 67 | 0 (0.0) | 6 (9.0) | 61 (91.0) | |
| ≥ 25 years | 72 | 48 (67.1) | 16 (21.4) | 8 (11.4) | < 0.01** | 68 | 3 (4.4) | 5 (7.4) | 60 (88.2) | 0.28 | 258 | 5 (1.9) | 30 (11.6) | 223 (86.4) | |
| All | 219 | 113 (51.6) | 53 (24.2) | 53 (24.2) | < 0.01** | 103 | 4 (3.9) | 8 (7.8) | 91 (88.4) | 0.23 | 428 | 7 (1.6) | 48 (11.2) | 373 (87.2) | |
Figures are number of participants per age category (%).
P < 0.05.
P < 0.05.
Figure 2.
Relationship between age and tetanus toxoid positivity.
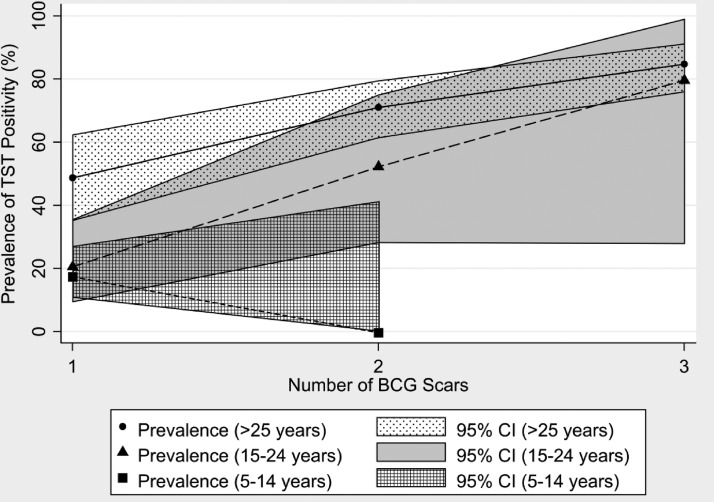
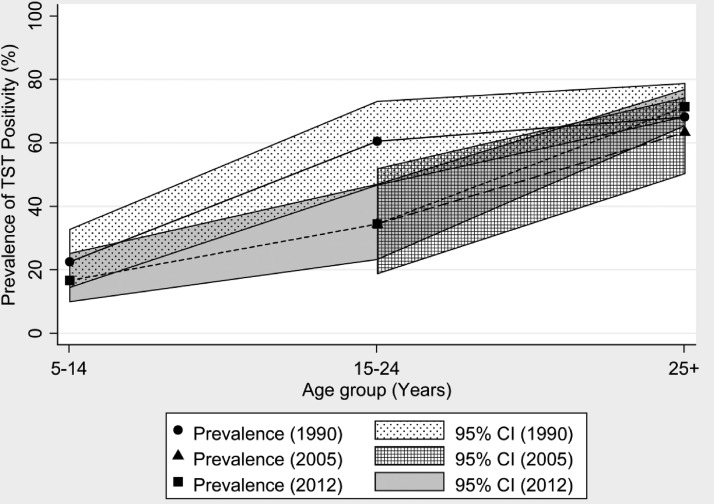
Table 4 shows the associations with a higher category of TST positivity that included education level (P = 0.04), number of BCG scars (P < 0.01, Figure 3 ), age (P < 0.01, Figure 4 ), and having lived in the last 5 years with a person diagnosed with TB (P = 0.02). No significant differences were noted in the categories of TST positivity with gender, BMI category, basic service monthly expenditure, number of persons per room, or the reported house ventilation.
Table 4.
TST positivity by socio-demographic and clinical characteristics, 2012
| Variable | TST result | P value | ||
|---|---|---|---|---|
| Negative(0–4 mm) | Borderline(5–9mm) | Positive(≥ 10 mm) | ||
| Gender | ||||
| Male | 52 (25.0) | 38 (18.3) | 118 (56.7) | 0.21 |
| Female | 66 (30.0) | 48 (21.8) | 106 (48.2) | |
| Age (years)† | 15.0 (9.5) | 21.0 (13.5) | 42.5 (13.3) | < 0.01** |
| Age category | ||||
| 5–14 years | 55 (53.4) | 31 (30.1) | 17 (16.5) | < 0.01** |
| 15–24 years | 25 (37.3) | 19 (28.4) | 23 (34.3) | |
| ≥ 25 years | 38 (14.7) | 36 (14.0) | 184 (71.3) | |
| BCG scars | ||||
| 0 | 1 (50.0) | 0 (0.0) | 1 (50.0) | < 0.01** |
| 1 | 83 (42.4) | 59 (30.1) | 54 (27.5) | |
| 2 | 26 (19.8) | 20 (15.3) | 85 (64.9) | |
| 3+ | 8 (8.1) | 7 (7.1) | 84 (84.8) | |
| BMI category - adults‡ | ||||
| Underweight | 1 (33.3) | 1 (33.3) | 1 (33.3) | 0.52 |
| Normal weight | 12 (13.6) | 14 (15.9) | 62 (70.5) | |
| Overweight | 26 (20.0) | 20 (15.4) | 84 (64.6) | |
| Obese | 10 (13.0) | 13 (16.9) | 54 (70.1) | |
| BMI category - children§ | ||||
| Underweight | 2 (66.7) | 0 (0.0) | 1 (33.3) | 0.39 |
| Normal weight | 44 (55.7) | 24 (30.4) | 11 (13.9) | |
| Overweight | 12 (38.7) | 11 (35.5) | 8 (25.8) | |
| Obese | 10 (62.5) | 3 (18.8) | 3 (18.8) | |
| Education level | ||||
| None | 5 (27.8) | 6 (33.3) | 7 (38.9) | 0.04* |
| Primary | 46 (35.9) | 28 (21.9) | 54 (42.2) | |
| Secondary | 49 (25.5) | 37 (19.3) | 106 (55.2) | |
| Superior | 18 (20.0) | 15 (16.7) | 57 (63.3) | |
| Basic service expenditure†¶ | 167.3 (38.8) | 170.0 (44.0) | 169.0 (38.5) | 0.84 |
| Persons/room ratio¶ | 2.0 (0.1) | 2.3 (0.1) | 2.0 (0.1) | 0.21 |
| Reported house ventilation | ||||
| Poor | 32 (36.0) | 19 (21.4) | 38 (42.7) | 0.08 |
| Good | 86 (25.4) | 67 (19.8) | 186 (54.9) | |
| Lived with TB contact in past 5 years | ||||
| Yes | 4 (10.3) | 8 (20.5) | 27 (69.2) | 0.02* |
| No | 114 (29.3) | 78 (20.1) | 197 (50.6) | |
P < 0.05; ** P < 0.01.
Median (semi-interquartile range), Ratio (standard error), otherwise N (%).
BMI categories for adults were based on the WHO Classification.
BMI categories for children were based on CDC 2000 Growth Reference (based on BMI z-scores for age and sex).
Basic service expenditure was calculated as the sum of the monthly expenditure on electricity, water supply and food (in nuevos soles).
TST= tuberculin skin test; BCG = Bacille Calmette-Guérin; BMI = body mass index; TB = tuberculosis.
Figure 3.
Relationship between number of Bacille Calmette-Guérin (BCG) scars and tuberculin skin test (TST) positivity.
Figure 4.
Relationship between age and tuberculin skin test (TST) positivity.
Table 5 shows the crude and adjusted associations with TST positivity analyzed with a binary logistic regression model. Adjusting for potential confounders (gender, age, number of BCG scars, BMI category, education level, basic service monthly expenditure, and TB contact) changed the OR for most of the variables in the model. In multiple regression analysis, three characteristics were independently associated with the TST positivity: female gender (OR = 0.6, 95% CI: 0.4, 1.0), increasing age (OR per additional year = 1.1, 95% CI: 1.0, 1.1), and more BCG scars. Compared with one scar, persons with two scars had twice the odds of having a positive TST result (OR = 2.7, 95% CI: 1.5, 4.8), whereas people with three or more scars had more than five times the odds of having a positive TST (OR = 5.7, 95% CI: 2.7, 12, Table 5).
Table 5.
Crude and adjusted odds ratios (OR) and 95% confidence intervals (95% CI) of a positive TST# by socio-demographic and clinical characteristics using binary logistic regression, 2012
| Characteristic | Crude model | Adjusted model† | ||
|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | |
| Gender | ||||
| Male | 1.00 | Reference | 1.00 | Reference |
| Female | 0.71 | (0.48, 1.04) | 0.59 | (0.36, 0.96)* |
| Age (years) | ||||
| 5 years | 1.00 | Reference | 1.00 | Reference |
| Each additional year of age | 1.06 | (1.05, 1.08)** | 1.05 | (1.03, 1.06)** |
| BCG scars | ||||
| 0 | 2.63 | (0.16, 42.79) | 2.19 | (0.12, 37.11) |
| 1 | 1.00 | Reference | 1.00 | Reference |
| 2 | 4.86 | (3.02, 7.82)** | 2.72 | (1.54, 4.78)** |
| ≥ 3 | 14.73 | (6.80, 23.25)** | 5.66 | (2.68, 11.93)** |
| BMI category§ | ||||
| Underweight | 0.64 | (0.11, 3.61) | 0.52 | (0.05, 5.18) |
| Normal weight | 1.00 | Reference | 1.00 | Reference |
| Overweight | 1.72 | (1.11, 2.66)* | 0.83 | (0.47, 1.45) |
| Obese | 2.04 | (1.22, 3.42)** | 0.86 | (0.44, 1.67) |
| Education level | ||||
| Primary or less | 0.52 | (0.35, 0.79)** | 0.86 | (0.51, 1.45) |
| Secondary or greater | 1.00 | Reference | 1.00 | Reference |
| Basic service expenditure¶ | ||||
| 100 nuevos soles | 1.00 | Reference | 1.00 | Reference |
| Each additional 50 nuevos soles | 0.99 | (0.87, 1.14) | 0.85 | (0.72, 1.02) |
| Persons/room ratio | ||||
| 1.0 | 1.00 | Reference | 1.00 | Reference |
| Each additional person/room | 0.94 | (0.84, 1.05) | 0.98 | (0.86, 1.12) |
| Reported house ventilation | ||||
| Poor | 0.61 | (0.38, 0.98)* | 1.31 | (0.73, 2.35) |
| Good | 1.00 | Reference | 1.00 | Reference |
| Lived with TB contact in last past 5 years | ||||
| Yes | 2.19 | (1.08, 4.45)* | 1.50 | (0.63, 3.57) |
| No | 1.00 | Reference | 1.00 | Reference |
P < 0.05; ** P < 0.01.
#TST results were classified as follows: Negative: 0–9 mm; and Positive: ≥ 10 mm induration.
Adjusted for gender, age, number of BCG scars, body mass index, education level, basic service expenditure, and having lived with a person with TB in the last 5 years.
BMI categories for adults were based on the WHO Classification, whereas BMI categories for children were based on CDC 2000 Growth Reference (based on BMI z-scores for age and sex).
Basic service expenditure was calculated as the sum of the monthly expenditure on electricity, water supply, and food (in nuevos soles).
TST= tuberculin skin test; BCG = Bacille Calmette-Guérin; BMI = body mass index; TB = tuberculosis.
The annual increase in the age-specific prevalence of a positive TST result was 2.2% (95% CI: 1.9, 2.5) for all participants, and 1.5% (95% CI: 1.1, 1.9) for participants with no or one BCG vaccination. The relationship between increased age and TST positivity was statistically significant P < 0.001, (Table 6). The TST positivity in participants with no or one BCG scar was 28%. There was large variability depending on age as seen in Figure 1. Similar to findings in 1990, there was a statistically significant (P < 0.01) association between age and TST positivity for participants who had no or one BCG scar.
Table 6.
Age-specific prevalences of TST positivity and annual risk of infection, 2012*
| Age (years) | n | Prevalence (%) | 95% confidence interval | Annual risk of infection (%) | 95% confidence interval |
|---|---|---|---|---|---|
| 5–14 | 103 | 16.5 | (10.7, 25.5) | 1.75 | (1.08, 2.77) |
| 15–24 | 67 | 34.3 | (24.6, 47.8) | 2.08 | (1.36, 3.07) |
| 25–34 | 64 | 60.9 | (50.1, 74.2) | 3.14 | (2.23, 4.24) |
| 35–44 | 64 | 62.5 | (51.7, 75.6) | 2.43 | (1.73, 3.27) |
| 45–54 | 62 | 79.0 | (38.8, 58.2) | 3.10 | (2.22, 4.09) |
| ≥ 55 | 68 | 82.4 | (73.8, 91.9) | 2.71 | (1.97, 3.54) |
| All | 428 | 52.3 | (47.5, 57.2) | 2.21 | (1.92, 2.53) |
TST = tuberculin skin test; ARI = annual risk of infection.
Figure 3 shows the relationship between TST positivity and number of BCG scars. The number of BCG scars per participant increased considerably with increasing age: 7% of 5–14 years of age had multiple BCG scars; 36% for 15–24 years of age; and 77% of participants aged ≥ 25 years of age (P < 0.01). The adjusted population attributable fraction of multiple BCG scars (compared with one BCG scar) causing TST positivity was 40% (95% CI: 28, 47), increased from 26% when assessed in 2004 in this population.2
Discussion
Global TB control is hampered by the high prevalence of latent TB infection because it constitutes a reservoir of individuals capable of developing TB disease and subsequently transmitting the infection to others. Despite evidence of decreasing numbers of diagnosed TB disease cases in Peru, objective data concerning changes in TB infection rates are lacking.
We determined the overall prevalence of TST positivity to be 52%, showing that TB infection is still at high levels, similar to previous studies up to 20 years ago.11–13 Our results indicate that overall infection rates in this region were similar in 2012 to 2005 and 1990. This observation may be confounded by our observations that TB infection rates increased with age, as reported previously,2,30–34 and the population age has increased significantly. These similarities in overall TST positivity prevalence contrasted with a significant decrease in TST positivity (and corresponding increase in borderline results) in the youngest age groups, most likely because BCG revaccinations cause false-positive TST results and were policy until 1996 in Peru2 but had become rare by 2005 and 2012. Thus, the effect of multiple BCG administrations is a bias to the estimate of true TB infection rates. In the oldest age group there was no statistically significant change in the very high prevalence of TST positivity. Recent studies corroborate these findings revealing that TB infection in older populations has been stable or increasing in developing countries around the world,30–34 making TB infection one of the most prevalent infections affecting older populations.34
There were few differences in TST and tetanus results from 200511 to 2012. One distinction is that there were more borderline TST results in 2012 than 2005 in the 15–24 age groups and the ≥ 25 age group for reasons that were not determined. These similarities, between 2005 and 2012, contrast with marked changes in TST and tetanus positivity rates between 1990 and 2005.
In Peru, BCG vaccinations at birth are ubiquitous and have been for several decades. The 99.5% prevalence of BCG scars in our study are similar to other recent Peruvian studies11,14 and to a 98% rate in Peru in 199512 but are higher than in 1990 when the BCG vaccination rate was 87%.13 Current policy in Peru is to administer only one BCG vaccination at birth.35,36 Children 5–14 years of age almost universally have only one BCG scar, indicating that in this population current policy is being implemented effectively. Although most participants had more than one BCG scar this was because of the high proportion of older individuals with more than one scar. A single BCG vaccine administered at birth has little effect on the sensitivity and specificity of the TST when tested more than 6 months later.12,14,37,38 However, BCG revaccination caused multiple BCG scars and can cause false positive TST results but has no known protective effect against developing disease.2,39 Indeed, we estimated that after adjusting for confounding factors, 40% of the TST positivity observed in this study was attributable to BCG revaccination. Potentially, use of interferon-gamma release assays in place of the TST would be expected to reduce the effect of BCG revaccination on estimating latent TB infection prevalence because these assays are not affected by most BCG vaccine strains.40,41
Analysis of BMI revealed that in the oldest age category (25 years of age and older), 45% of participants were pre-obese, and almost 30% were overtly obese, rates that are among the highest in the world. For comparison, the prevalence of pre-obesity and obesity in the United States are 27% and 36% among adults.42 However, it should be noted that BMI is an imperfect marker of build for Peruvians caused by their short leg: body length ratio that affects the BMI disproportionately compared with Caucasians.43 Although this high prevalence of overweight is notable, we found no association between nutritional status and TST positivity.
There were substantial changes in tetanus skin test positivity from 199013 to 2012. Free tetanus vaccinations are provided by the Peruvian government and three vaccinations are required before children are permitted to begin school.44 In 1990 only a minority had a positive (weak or strong) skin test reaction tetanus toxoid in contrast to almost universal positivity in 200511 and 2012. The high tetanus positivity rate shows that anergy was not prevalent in 2012 and did not appear to influence our skin test results, probably because of the high current levels of tetanus immunization and low prevalence of malnutrition.
There were several limitations to this study including the low sample size within the 15–24 age group compared with the other two age categories and the lack of data concerning the actual number of BCG scars for participants in the 1992 study that only recorded whether any BCG scar was present. As described in Saito and others,2 Peru policy in 1990 of administering two BCG vaccinations was discontinued in 1996, although this policy change was implemented gradually and inconsistently.1 In addition, in some studies TST reactivity has varied between tuberculin supplied by different manufacturers and Pelly and others (2005) used Tubersol, whereas Getchell and others (1992) and our current study both used Aplisol.45–48
In conclusion, despite recent reductions in reported rates of TB disease, TST positivity rates are still high in these shantytowns, especially among those 25 years of age and older. The TST positivity in the 15–24 age group decreased since 1990 probably at least partially because multiple BCG vaccinations (that cause false positive TST) were common, and have now become rare. A decrease in TB infection also may have contributed to this fall in TST positivity in younger age groups, but TST positivity rates have not fallen overall or in older adults. Thus, in these shantytowns latent TB infection occurs in most adults and overall prevalence has remained similar from 1990 to 2012. These changes in population age and BCG vaccination policies confound attempts to monitor TB infection rates, which could be important to Peru and other countries embarking upon large sample TST surveys in the future.
ACKNOWLEDGMENTS
In memoriam Luz Caviedes Rojas, 1968–2012. We thank the Pampas de San Juan de Miraflores residents who donated their time for health research. We thank the Pampas PRISMA office that worked meticulously on this project. Special thanks to Ruth Limasca, Luz Caviedes and her laboratory, Marco Varela, Erika Falcon, Brigida Rosario Jimenez Hualpa, Antonio Bernabe-Ortiz, and JB Phu and D. Sara.
Footnotes
Financial support: LM and GC were supported through the Tulane-Xavier Minority Health International Research Training (MHIRT) Program, funded by a training grant from the National Institutes of Health (T37 MD001424). CAE, TFP, and the 2005 study were supported by IFHAD: Innovation For Health And Development and The Wellcome Trust. This study was funded in part by the anonymous RG–ER fund and NIH RO1 HD059005.
Authors' addresses: Leonardo Martinez and Richard Oberhelman, Global Community Health and Behavioral Sciences, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, E-mails: lmartin7@tulane.edu and oberhel@tulane.edu. Alyssa Arman and Nathan Haveman, California State University, Fullerton, San Diego, CA, E-mails: lyssiejoy@gmail.com and n.eight.h@gmail.com. Ashley Lundgren, Weill Cornell Medical College, New York, NY, E-mail: ashley.diana@gmail.com. Lilia Cabrera, Asociación Benefica PRISMA, Lima, Peru, E-mail: lilia_deviaje@yahoo.com. Carlton A. Evans, Wellcome Trust Centre for Clinical Tropical Medicine, Department of Infectious Diseases and Immunity, Imperial College London Hammersmith Hospital Campus, London, UK, E-mail: carlton.evans@ifhad.org. Tom F. Pelly, IFHAD - Innovation For Health And Development, Universidad Peruana Cayetano Heredia LID#218, Lima, Peru, E-mail: tompelly@doctors.org.uk. Mayuko Saito, University of California, San Diego, San Diego, CA, E-mail: msaitop@gmail.com. David Callacondo, Molecular and Clinical Hematology Branch, National Heart Lung and Blood Institute, National Institutes of Health, Bethesda, MD, E-mail: david.callacondo@upch.pe. Gisela Collazo, Tulane University, New Orleans, LA, E-mail: gcollazo@tulane.edu. Andrés M. Carnero, Postgraduate School, Universidad Peruana Cayetano Heredia, Lima, Peru, E-mail: andrescarnero@gmail.com. Robert H. Gilman, Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, E-mail: rgilman@jhsph.edu.
References
- 1.World Health Organization Global Tuberculosis Report 2012. 2012. http://apps.who.int/iris/bitstream/10665/75938/1/9789241564502_eng.pdf Available at. Accessed November 1, 2012.
- 2.Saito M, Bautista CT, Gilman RH, Bowering A, Levy MZ, Evans CA. The value of counting BCG scars for interpretation of tuberculin skin tests in a tuberculosis hyperendemic shantytown, Peru. Int J Tuberc Lung Dis. 2004;8:842–847. [PMC free article] [PubMed] [Google Scholar]
- 3.Millet JP, Moreno A, Fina L, Del Baño L, Orcau A, de Olalla PG, Caylà JA. Factors that influence current tuberculosis epidemiology [published online ahead of print 8 May 2012] Eur Spine J. 2012 doi: 10.1007/s00586-012-2334-8. http://link.springer.com/article/10.1007%2Fs00586-012-2334-8 Available at. Accessed May 21, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Tuberculosis. 2012. http://www.who.int/mediacentre/factsheets/fs104/en/index.html Available at. Accessed July 1, 2012.
- 5.Suárez PG, Watt CJ, Alarcón E, Portocarrero J, Zavala D, Canales R, Luelmo F, Espinal MA, Dye C. The dynamics of tuberculosis in response to 10 years of intensive control effort in Peru. J Infect Dis. 2001;184:473–478. doi: 10.1086/322777. [DOI] [PubMed] [Google Scholar]
- 6.Sobero RA, Peabody JW. Tuberculosis control in Bolivia, Chile, Colombia and Peru: why does incidence vary so much between neighbors? Int J Tuberc Lung Dis. 2006;10:1292–1295. [PubMed] [Google Scholar]
- 7.Santiago EM, Lawson E, Gillenwater K, Kalangi S, Lescano AG, Du Quella G, Cummings K, Cabrera L, Torres C, Gilman RH. A prospective study of Bacillus Calmette-Guérin scar formation and tuberculin skin test reactivity in infants in Lima, Peru. Pediatrics. 2003;112:e298. doi: 10.1542/peds.112.4.e298. [DOI] [PubMed] [Google Scholar]
- 8.Raharimanga V, Ratovoson R, Ratsitorahina M, Ramarokoto H, Rasolofo V, Talarmin A, Richard V. Tuberculin reactivity in first-year schoolchildren in Madagascar. Trop Med Int Health. 2012;17:871–876. doi: 10.1111/j.1365-3156.2012.03013.x. [DOI] [PubMed] [Google Scholar]
- 9.Donald PR. Childhood tuberculosis. Curr Opin Pulm Med. 2000;6:187–192. doi: 10.1097/00063198-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Lockman S, Tappero JW, Kenyon TA, Rumisha D, Huebner RE, Binkin NJ. Tuberculin reactivity in a pediatric population with high BCG vaccination coverage. Int J Tuberc Lung Dis. 1999;3:23–30. [PubMed] [Google Scholar]
- 11.Pelly TF, Santillan CF, Gilman RH, Cabrera LZ, Garcia E, Vidal C, Zimic MJ, Moore DA, Evans CA. Tuberculosis skin testing, anergy and protein malnutrition in Peru. Int J Tuberc Lung Dis. 2005;9:977–984. [PMC free article] [PubMed] [Google Scholar]
- 12.Madico G, Gilman RH, Checkley W, Cabrera L, Kohlstadt I, Kacena K. Community infection ratio as an indicator for tuberculosis control. Lancet. 1995;345:416–419. doi: 10.1016/s0140-6736(95)90401-8. [DOI] [PubMed] [Google Scholar]
- 13.Getchell WS, Davis CE, Gilman J, Urueta G, Ruiz-Huidobro E, Gilman RH. Basic epidemiology of tuberculosis in Peru: a prevalence study of tuberculin sensitivity in a pueblo joven. Am J Trop Med Hyg. 1992;47:721–729. doi: 10.4269/ajtmh.1992.47.721. [DOI] [PubMed] [Google Scholar]
- 14.Sandhu G, Battaglia F, Ely BK, Athanasakis D, Montoya R, Valencia T, Gilman RH, Evans CA, Friedland JS, Fernandez-Reyes D, Agranoff DD. Discriminating active from latent tuberculosis in patients presenting to community clinics. PLoS ONE. 2012;7:e38080. doi: 10.1371/journal.pone.0038080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loret de Mola C, Stanojevic S, Ruiz P, Gilman RH, Smeeth L, Miranda JJ. The effect of rural-to-urban migration on social capital and common mental disorders: PERU MIGRANT study. Soc Psychiatry Psychiatr Epidemiol. 2011;47:967–973. doi: 10.1007/s00127-011-0404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.INEI . Las Migraciones Internas en el Peru: 1993–2007. Lima. Peru: Instituto Nacional de Estadística e Informática; 2009. pp. 1–185. [Google Scholar]
- 17.World Health Organization Global Database on Body Mass Index: An Interactive Surveillance Tool for Monitoring Nutrition Transition. 2012. http://apps.who.int/bmi/index.jsp Available at. Accessed April 1, 2012.
- 18.Vidmar S, Carlin J, Hesketh K, Cole T. Standardizing anthropometric measures in children and adolescents with new functions for egen. Stata J. 2004;4:50–55. [Google Scholar]
- 19.Bouros D, Maltezakis G, Tzanakis N, Tzortzaki E, Siafakas N. The role of inexperience in measuring tuberculin skin reaction (Mantoux test) by the pen or palpation technique. Respir Med. 1992;86:219–223. doi: 10.1016/s0954-6111(06)80059-4. [DOI] [PubMed] [Google Scholar]
- 20.Caviedes L, Moore DA. Introducing MODS: a low-cost, low-tech tool for high-performance detection of tuberculosis and multidrug resistant tuberculosis. Indian J Med Microbiol. 2007;25:87–88. doi: 10.4103/0255-0857.32711. [DOI] [PubMed] [Google Scholar]
- 21.Oberhelman RA, Soto-Castellares G, Gilman RH, Caviedes L, Castillo ME, Kolevic L, Del Pino T, Saito M, Salazar-Lindo E, Negron E, Montenegro S, Laguna-Torres VA, Moore DA, Evans CA. Diagnostic approaches for pediatric tuberculosis by use of different specimen types, culture methods, and PCR: a prospective case-control study. Lancet Infect Dis. 2010;10:612–620. doi: 10.1016/S1473-3099(10)70141-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore DA, Evans CA, Gilman RH, Caviedes L, Coronel J, Vivar A, Sanchez E, Piñedo Y, Saravia JC, Salazar C, Oberhelman R, Hollm-Delgado MG, LaChira D, Escombe AR, Friedland JS. Microscopic-observation drug-susceptibility assay for the diagnosis of TB. N Engl J Med. 2006;355:1539–1550. doi: 10.1056/NEJMoa055524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caviedes L, Lee TS, Gilman RH, Sheen P, Spellman E, Lee EH, Berg DE, Montengro-James S. Rapid, efficient detection and drug susceptibility testing of Mycobacterium tuberculosis in sputum by microscopic observation of broth cultures. The Tuberculosis Working Group in Peru. J Clin Microbiol. 2000;38:1203–1208. doi: 10.1128/jcm.38.3.1203-1208.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control Tuberculosis. 2012. http://www.cdc.gov/tb/topic/basics/risk.htm Available at. Accessed April 1, 2012.
- 25.Hosmer DW, Lemeshow S. Applied Logistic Regression. Second edition. New York: John Wiley & Sons; 2000. pp. 143–200. [Google Scholar]
- 26.Arnadottir T, Rieder HL, Trebucq A, Waaler HT. Guidelines for conducting tuberculin skin test surveys in high prevalence countries. Tuber Lung Dis. 1996;77((Suppl)):1–20. doi: 10.1016/s0962-8479(96)90127-6. [DOI] [PubMed] [Google Scholar]
- 27.Rieder HL. Methodological issues in the estimation of the tuberculosis problem from tuberculin surveys. Tuber Lung Dis. 1995;76:114–121. doi: 10.1016/0962-8479(95)90552-9. [DOI] [PubMed] [Google Scholar]
- 28.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 30.Mori T, Leung CC. Tuberculosis in the global aging population. Infect Dis Clin North Am. 2010;24:751–768. doi: 10.1016/j.idc.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 31.Schaaf HS, Collins A, Bekker A, Davies PD. Tuberculosis at extremes of age. Respirology. 2010;15:747–763. doi: 10.1111/j.1440-1843.2010.01784.x. [DOI] [PubMed] [Google Scholar]
- 32.Chan-Yeung M, Dai DL, Cheung AH, Chan FH, Kam KM, Tam CM, Leung CC. Tuberculin skin test reaction and body mass index in old age home residents in Hong Kong. J Am Geriatr Soc. 2007;55:1592–1597. doi: 10.1111/j.1532-5415.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 33.Dolin PJ, Raviglione MC, Kochi A. Global tuberculosis incidence and mortality during 1990–2000. Bull World Health Organ. 1994;72:213–220. [PMC free article] [PubMed] [Google Scholar]
- 34.Cruz-Hervert LP, García-García L, Ferreyra-Reyes L, Bobadilla-Del-Valle M, Cano-Arellano B, Canizales-Quintero S, Ferreira-Guerrero E, Báez-Saldaña R, Téllez-Vazquez N, Nava-Mercado A, Juárez-Sandino L, Delgado-Sánchez G, Fuentes-Leyra CA, Montero-Campos R, Martínez-Gamboa RA, Small PM, Sifuentes-Osornio J, Ponce-de-León A. Tuberculosis in ageing: high rates, complex diagnosis and poor clinical outcomes. Age Ageing. 2012;41:488–495. doi: 10.1093/ageing/afs028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peruvian Ministry of Health . Estrategia Sanitaria Nacional de Inmunizaciones. Norma tecnica de Inmunizaciones. Lima, Peru: Direccion General de Salud de las Personas; 2006. pp. 1–17. [Google Scholar]
- 36.World Health Organization Global Health Observatory. 2009. http://www.who.int/gho/en/ Available at. Accessed June 18, 2012.
- 37.Menzies R, Vissandjee B. Effect of Bacille Calmette-Guérin vaccination on tuberculin reactivity. Am Rev Respir Dis. 1992;145:621–625. doi: 10.1164/ajrccm/145.3.621. [DOI] [PubMed] [Google Scholar]
- 38.Burl S, Adetifa UJ, Cox M, Touray E, Whittle H, McShane H, Rowland-Jones SL, Flanagan KL. The tuberculin skin test (TST) is affected by recent BCG vaccination but not by exposure to non-tuberculosis mycobacteria (NTM) during early life. PLoS ONE. 2010;5:e12287. doi: 10.1371/journal.pone.0012287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colditz GA, Brewer TF, Berkey CS, Wilson ME, Buradick E, Fineberg HV, Mosteller F. Efficacy of BCG vaccine in the prevention of tuberculosis. Meta-analysis of the published literature. JAMA. 1994;271:698–702. [PubMed] [Google Scholar]
- 40.Menzies D, Pai M, Comstock G. Meta-analysis: new tests for the diagnosis of latent tuberculosis infection: areas of uncertainty and recommendations for research. Ann Intern Med. 2007;146:340–354. doi: 10.7326/0003-4819-146-5-200703060-00006. [DOI] [PubMed] [Google Scholar]
- 41.Pai M, Zwerling A, Menzies D. Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Ann Intern Med. 2008;149:177–184. doi: 10.7326/0003-4819-149-3-200808050-00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control Vital signs: state-specific obesity prevalence among adults—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:951–955. [PubMed] [Google Scholar]
- 43.Trowbridge FL, Marks JS, Lopez de Romana G, Madrid S, Bouton TW, Klein PD. Body composition of Peruvian children with short stature and high weight-for-height. II. implications for the interpretation for weight-for-height as an indicator of nutritional status. Am J Clin Nutr. 1987;46:411–418. doi: 10.1093/ajcn/46.3.411. [DOI] [PubMed] [Google Scholar]
- 44.Madico G, Salazar G, McDonald J, Checkley W, Calderon M, Verastegui M, Gilman RH. Rates of tetanus protection and transplacental tetanus antibody transfer in pregnant women from different socioeconomic groups in Peru. Clin Diagn Lab Immunol. 1996;3:753–755. doi: 10.1128/cdli.3.6.753-755.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Villarino ME, Brennan MJ, Nolan CM, Catanzaro A, Lundergan LL, Bock NN, Jones CL, Wang YC, Burman WJ. Comparison testing of current (PPD-S1) and proposed (PPD-S2) reference tuberculin standards. Am J Respir Crit Care Med. 2000;161:1167–1171. doi: 10.1164/ajrccm.161.4.9906050. [DOI] [PubMed] [Google Scholar]
- 46.Tat D, Polenakovik H, Herchline T. Comparing interferon-gamma release assay with tuberculin skin test readings at 48–72 hours and 144–168 hours with use of 2 commercial reagents. Clin Infect Dis. 2005;40:246–250. doi: 10.1086/426816. [DOI] [PubMed] [Google Scholar]
- 47.Mehta SR, MacGruder C, Looney D, Johns S, Smith DM. Differences in tuberculin reactivity as determined in a veterans administration employee health screening program. Clin Vaccine Immunol. 2009;16:541–543. doi: 10.1128/CVI.00375-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gillenwater KA, Sapp SC, Pearce K, Siberry GK. Increase in tuberculin skin test converters among health care workers after a change from Tubersol to Aplisol. Am J Infect Control. 2006;34:651–654. doi: 10.1016/j.ajic.2006.05.288. [DOI] [PubMed] [Google Scholar]