Abstract
Hydatidosis is a zoonosis of worldwide distribution caused by the parasite Echinococcus granulosus. Clinical manifestations include cyst formation, most commonly in the liver (67–89%) and lungs (10–15%). Renal localizations are rare. We report a case of renal hydatidosis in a five-year-old child treated in a tertiary pediatric hospital in Argentina. After the diagnosis was made, elective surgery was performed, which led to a rapid recovery.
We report a five-year-old previously healthy boy who had an abdominal mass. The patient was born in rural Santiago del Estero in northwestern Argentina and had lived since three years of age in the greater Buenos Aires area. The patient was in close contact with dogs that were not given veterinary care and were regularly fed undercooked animal viscera (cattle, sheep).
The child came to a pediatrician with a history of weight loss and a palpable mass in the abdominal right upper quadrant that was present for two months. After multiple consultations, the child was referred to the Parasitology Service at Ricardo Gutierrez Childrens Hospital in Buenos Aires, where he was in good condition and had a weight in the 10–25 percentile, but had a visible and palpable abdominal mass. Abdominal ultrasonography showed an homogeneous liver with normal bile ducts and gallbladder, and a 112×80 mm cystic image in the hepatic right lobe with moving particulate content (snow flake sign) (Figure 1). The spleen was uniform and both kidneys appeared normal. An abdominal computed tomography scan showed the cystic image to be in close contact with the right kidney. Chest radiography showed no abnormalities. A serologic test result (indirect hemagglutination) was negative for hydatidosis. Blood counts and kidney and liver function test results showed no abnormalities.
Figure 1.
Abdominal ultrasound scan of a five-year-old child with renal hydatidosis, Argentina, showing the snow flake sign caused by mobilization of hydatid sand when the patient is mobilized abruptly through 180 degrees.
Because of the epidemiologic and imaging findings, the mass was assumed to be compatible with an abdominal hydatidosis, and treatment was started with albendazole, 12.5 mg/kg/day orally, twice a day. Four days later, the patient had a fever and abdominal pain. Blood tests showed a leukocyte count of 17,700 cells/mm3 with 78% neutrophils (13,806 cells/mm3) and normal renal and hepatic function. The patient was hospitalized because of the assumption of a bacterial superinfection of the cyst, and antibiotic treatment with clindamycin and cefotaxime was started. Within 48 hours, the patient became afebrile and showed significant clinical improvement.
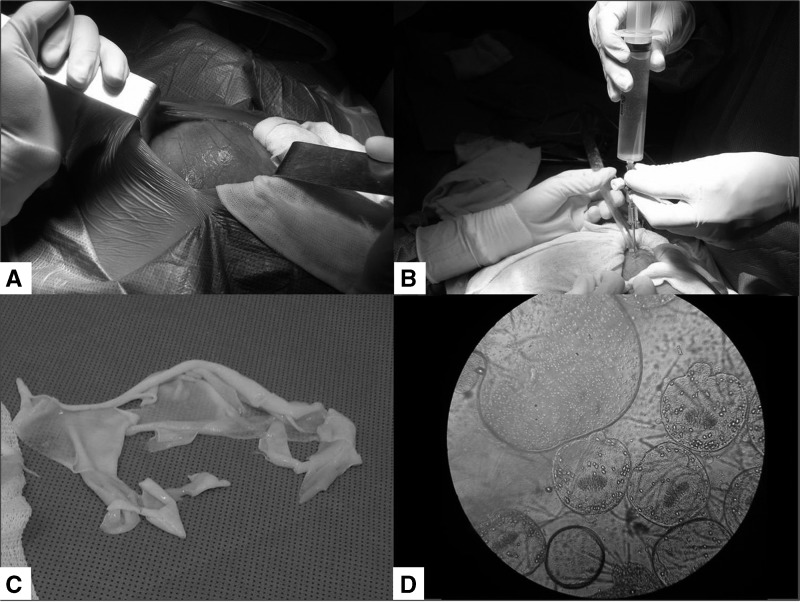
Surgery (laparotomy) was performed through a right subcostal incision to evaluate the cyst, which was found to originate from the right kidney. Cyst content was aspirated and its membranes were removed, followed by resection of the emergent cyst wall. Microscopy showed that the cyst contained a large number of protoscolices (Figure 2), confirming the clinical diagnosis of hydatidosis. Laboratory tests after surgery showed significant eosinophilia (3,000 cells/mm3), which resolved within 30 days, and an indirect hemagglutination test showed a positive result (titer = 1:512).
Figure 2.
Surgical removal of a cyst from a five-year-old child with renal hydatidosis, Argentina. A, hydatid cyst; B, cystic content voiding puncture; C, hydatid membranes; D, evaluation of hydatid fluid in which there are many protoscoleces.
The patient completed 14 days of albendazole therapy in the hospital and continued to receive as an outpatient albendazole for three months to prevent relapse because of the vitality and size of the cyst. The child progressed well and returned to normal activities. Biannual serologic tests showed a marked decrease in specific titers after four years of follow-up. Monthly abdominal ultrasonography showed no abnormalities. The patient is currently being followed-up once a year at our service.
Hydatidosis, or cystic echinococcosis, has a worldwide distribution, and cases have been reported in all continents. In Argentina, 385 cases of hydatid disease were reported in 2010 to the National Health Surveillance System.1
This disease develops mainly in rural areas where parasitized dogs, livestock (sheep, cattle, goats) and humans constitute the triad of the parasitic cycle. The definitive host is the dog, which becomes infected by ingesting protoscoleces within hydatid cysts in livestock organs (liver, lungs, kidney). The parasitized dog eliminates embryonated eggs in its feces, contaminating the water and soil; the eggs can be trapped in the hairs of the muzzle and body of the dog. The eggs ingested by humans or cattle (intermediate hosts) hatch in the gut and released parasites reach the systemic circulation through the small intestine and are distributed to other organs, mostly the liver and the lungs, where the larval stage (hydatid or cyst) develops.2 The pediatric population is at highest risk for infection because contact with the definitive host (dogs) is usually closer. For these reasons, a thorough epidemiologic evaluation is vital for the clinical diagnosis.
The renal localization, albeit rare (2–4%), is the third most common location, after the liver and lungs.3 This finding was reflected in a cohort of 38 children given a diagnosis of hydatidosis and treated in our department over the past 13 years; three patients were found to have renal cysts.4 Symptoms of the disease are related to the size of the cyst, which compresses adjacent structures, may rupture and become infected, or release content into neighboring body cavities. Approximately 18% of renal hydatid cysts release material into the urinary tract, causing hydatiduria and renal colic.3 In our experience, asymptomatic presentation is the most common in children, and the diagnosis is made by ultrasonography or palpation of a lump during a physical examination, as for our patient.5
Early diagnosis of hydatidosis is important for appropriate symptom control and treatment. Diagnosis is based mainly on epidemiology and imaging studies. Epidemiologic evaluation should include questions on area of residency (i.e., if the patient lives or has lived in a rural area), contact with dogs or livestock slaughter products, and diagnosis of hydatidosis in family members.
Ultrasonography is the most sensitive technique for identifying abdominal cysts, and is useful to evaluate evolutionary stage of the cysts, and determine size, location, and relationships with other organs. In addition, ultrasonography is the method of choice for following-up response to treatment, and is currently considered the gold standard for diagnosis and monitoring of the disease. The solid content of the cyst, commonly called hydatid sand, can be observed in abdominal ultrasonography when the patient moves, creating the snow flake sign.1,6
Computed tomography (CT) scans are useful in cases of diagnostic uncertainty in detecting smaller cysts in lungs or the central nervous system and for pre-surgical evaluation. Cysts are seen in CT scans as round or oval masses with well-defined edges and liquid content without intravenous contrast enhancement.7 In our patient, CT images suggested the renal origin of the cyst.
The indirect hemagglutination test and enzyme-linked immunosorbent assay are the currently preferred methods for serologic screening and diagnosis. Sensitivity can vary between 35% and 90% according to the antigen used, cutoff value and stage of the cyst. Serologic techniques may give false-negative results, especially in uncomplicated viable cysts, the most frequent in children.1,6 Therefore, a negative serologic result does not rule out hydatidosis.1,6,8 Because of low sensitivity of serologic tests, definitive diagnosis requires direct visualization of the scolex or pathologic examination of the membranes.4
As noted for our patient, serologic results can become positive after surgery, probably as a consequence of antigen release into circulation during cyst manipulation. Serologic analysis is most useful in tracking post-therapeutic disappearance of a previously positive test result over time, indicating adequate response to treatment, or an increase in titers, suggesting cyst recurrence. After four years of follow-up, serologic results for our patient became negative.
Eosinophilia is uncommon in asymptomatic patients with uncomplicated cysts. This finding may be caused by a lack of circulating parasites. In our experience, eosinophilia is commonly observed after surgery and resolves within a few months. Our patient had severe postoperative eosinophilia, which resolved within 30 days.
Albendazole (10–15 mg/kg/day for 3–5 months) is the treatment of choice for uncomplicated cysts.6,9 Conventional surgery is indicated for large cysts (> 7 cm) that might rupture and for complicated cysts. Treatment with albendazole (15 days before and 30 days after surgery) is also recommended in these cases because of the risks of cyst rupture and dissemination of protoscolices.6
A frequent complication of hydatidosis is bacterial infection of the cyst.1 In our patient, this complication was suspected because of sudden onset of fever, abdominal pain, and leukocytosis with neutrophilia. The patient responded well to empiric antibiotic therapy.
Definitive diagnosis requires direct visualization of the scolex or pathologic examination of the membranes.1,4,6 The protoscoleces can be observed in cyst fluid (Figure 2). The pathogenesis of the material submitted confirmed the diagnosis of renal hydatid disease.
Control of hydatidosis requires preventive measures. The main actions should be deworming of dogs, not feeding dogs offal from slaughtered animals, slaughtering livestock in enclosed places without access to dogs, washing hands before eating or handling food, and preventing close contact of children with non-controlled dogs.
When an abdominal cystic is found, a simple liver cyst is commonly considered the most likely diagnosis, particularly if the cyst is in the liver, kidney, or spleen. However, diagnosis of a simple liver cyst should not be made without a thorough investigation to rule out other etiologies, especially hydatidosis (particularly if epidemiologic results are positive). Early diagnosis of hydatidosis enables successful medical (pharmacologic) treatment in most cases, without complications, thus avoiding more invasive methods such as surgery. For those case-patients who do not response to albendazole or who have complicated cysts, surgery is the option.
Footnotes
Authors' addresses: Guillermo Moscatelli, Samanta Moroni, Héctor Freilij, Facundo García Bournissen, and Jaime Altcheh, Department of Parasitology, Ricardo Gutierrez Childrens Hospital, Gallo 1330, Buenos Aires C1425EFD, Argentina, E-mails: gfmoscatelli@yahoo.com.ar, samantamoroni@yahoo.com.ar, facugb@hotmail.com, and jaltcheh@gmail.com. Fabián Salgueiro, Department of Surgery, Ricardo Gutierrez Childrens Hospital, Buenos Aires, Argentina, E-mail: fabiansalgueiro@yahoo.com.ar.
References
- 1.Dirección de Epidemiología - Ministerio de Salud de la Nación Hidatidosis. Diagnóstico de Hidatidosis. Guía para el Wquipo de Salud no. 11, Marzo 2012. http://www.msal.gov.ar/zoonosis/images/stories/info-equipos-de-salud/pdf/hidatidosis-guia-medica.pdf Available at.
- 2.D'Alessandro A. Descripción, Morfología, Ciclo Biológico y Distribución de las Especies de Echinococcus. In: Denegri G, Elissondo MC, Dopchiz MC, editors. Situación de la Hidatidosis-Echinococcosis en la República Argentina. Editorial Martín; Mar del Plata, Argentina: 2002. pp. 19–30. [Google Scholar]
- 3.Rami M, Khattala K, ElMadi A, Afifi MA, Bouabddallah Y. The renal hydatid cyst: report on 4 cases. Pan Afr Med J. 2011;8:31. doi: 10.4314/pamj.v8i1.71147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altcheh J, Moroni S, Moscatelli G, Ballering G, Biancardi M, Freilij H. Hidatidosis en Pediatría: Eficacia del Tratamiento Médico. XXIII Congreso Mundial de Hidatología; Colonia del Sacramento, Uruguay: Diciembre 9–11, 2009. [Google Scholar]
- 5.Altcheh J, Fernández C, Moscatelli G, Salgueiro F, Moroni S, Biancardi M, Ballering G, Cosani H, Graziano G, Blumenthal L, Freilij H. Hidatidosis: 10 Años de Experiencia del Servicio de Parasitología-Chagas, Hospital de Niños R. Gutiérrez. VI Congreso Argentino de Infectología Pediátrica, Buenos Aires. http://www3.sap.org.ar/congresos/staticfiles/actividades/congresos/congre2008/infecto/Trabajoslibres.pdf Mayo de 2008. Available at. [Google Scholar]
- 6.Moscatelli G, Freilij H, Altcheh J. Hidatidosis o Echinococcosis quística. Buenos Aires: 2011. pp. 770–774. En: Pediatría de Luis Voyer, Raúl Ruvinsky, Carlos Cambiano. 3o edición. [Google Scholar]
- 7.Moscatelli G, Abraham Z, Moroni S, Martínez Iriart E, Rodríguez M, Mirón L, Vásquez Millán S, Casas L, Altcheh J. Pulmonary hydatidosis. Arch Argent Pediatr. 2012;110:265–267. doi: 10.5546/aap.2012.265. [DOI] [PubMed] [Google Scholar]
- 8.Freilij H, Santillán G, Céspedes G, Ballering G, Biancardi M, Andolfi F. Evaluación de dos técnicas serológicas en pacientes con hidatidosis abdominal en Cachi, Salta, Argentina. Parasitología Latinoamericana. 2005;60:236. [Google Scholar]
- 9.Gil Grande LA, Rodriguez Caabeiro F, Prito J. Randomized controlled trial of efficacy of albendazole in intra-abdominal hydatid disease. Lancet. 1993;342:1269–1272. doi: 10.1016/0140-6736(93)92361-v. [DOI] [PubMed] [Google Scholar]