Abstract
Among patients with cardiovascular disease (CVD), depression is highly prevalent and is associated with worse cardiovascular prognosis and lower quality of life. Treatments for depression in CVD patients produce modest, but clinically significant reductions in depressive symptoms and show promise for improving cardiovascular prognosis. While tricyclics should generally be avoided, antidepressants from multiple other classes appear to be safe in cardiac patients. A strategy of engaging patients in choosing medications or psychotherapy and then intensifying treatment to therapeutic goal appears to be more effective at reducing depression than single mode interventions. Recommendations for screening all CVD patients for depression may be premature given increased costs associated with screening and gaps in knowledge about the risk-benefit ratio of depression treatment in mild and moderately depressed patients.
Introduction
Patients with cardiovascular disease (CVD) have a two-fold increased risk of depression compared to patients without heart disease.1 Moreover, the presence of depression in CVD patients is associated with increased mortality, cardiac events, and health care costs, as well as lower quality of life and adherence to recommended treatments.2 Given the high impact of comorbid depression on medical, quality of life, and societal outcomes in patients with CVD, a growing body of research has assessed the effectiveness of depression interventions in these patients. While a tantalizing goal of depression treatment is the possibility that it might improve cardiovascular prognosis, the remission of depression, alone, is a worthy goal of depression treatment as depression is a major contributor to lower quality of life and increased health care costs in CVD patients.
Before evaluating the effectiveness of depression treatments in CVD patients, it is important to consider why treatment of depression in such patients may differ from treatment of depression in the general population. First, there is heightened concern regarding the possibility for cardiotoxic effects of some depression treatments. Second, if the depressive symptoms are in reaction to the stressful medical event (e.g. an adjustment disorder in reaction to the CVD event), then the symptoms are likely to spontaneously remit without screening and treatment. Third, the acceptability of a psychiatric treatment may differ in patients for whom CVD is the primary disease. Fourth, although mild sub-syndromal symptoms of depression have been associated with worse prognosis in CVD patients, it is not clear whether standard depression treatments will benefit CVD patients with milder depressive symptom burden. With these considerations in mind, below we review the evidence behind single modality and combined interventions involving pharmacotherapy, psychotherapy, or other approaches to treating depression in CVD patients.(Table 1)
Table 1.
Summary of key trials of depression treatment in patients with cardiovascular disease
| Study name | Participants | Intervention | Depression outcomes at end of treatment |
Cardiovascular outcomes at follow-up |
Notes |
|---|---|---|---|---|---|
| SADHART (Glassman et al. 2002) 4 |
369 Participants with depression after myocardial infarction or unstable angina |
Sertraline (n = 186) Control: Placebo (n = 183) Duration: 24 weeks |
Response rate: 67% sertraline, 53% placebo (P = 0.01) |
No significant difference in major adverse cardiac events; 17& intervention, 22% control Follow-up: 24 weeks |
Sertraline no different from placebo on measures of left ventricular ejection fraction, QTc prolongation and other measures of cardiovascular function or mortality |
| ENRICHD (Berkman et al. 2003) 9 |
1,834 Participants with depression after myocardial infarction |
Cognitive behavioral therapy (CBT) + sertraline if insufficient response to CBT (n = 925) Control: Usual care (n = 909) Duration: 26 weeks |
Change in HAM-D depression score: intervention -10, control - 8, p<.001 |
No significant difference in recurrent MI or death, 25 % intervention, 25% control Follow-up: 18 to 48 months |
Only study powered to find a difference in cardiovascular outcomes as a result of treatment |
| CREATE A (Lesperance et al 2007) 5 |
284 Participants with depression and coronary artery disease |
Intervention A: Interpersonal Psychotherapy + clinical management (n=142) Control A: Clinical management (n=142) |
No benefit of interpersonal psychotherapy over clinical management |
No significant difference in serious cardiovascular events, but only 12 total events Follow-up: 12 weeks |
2X2 factorial design |
| CREATE B (Lesperance et al 2007) 5 |
284 Participants with depression and coronary artery disease |
Intervention B: Citalopram (n=142) Control B: Placebo (n=142) Duration: 12 weeks |
Response rate: 53% intervention, 40% control, P=0.03 |
No significant difference in serious cardiovascular events but only 12 total events Follow-up: 12 weeks |
2X2 factorial design |
| Freedland et al. 2009 10 |
123 Participants with depression within 1 year of coronary artery bypass graft |
Intervention A: Cognitive behavioral therapy (n=41) Intervention B: Supportive stress management (n=42) Control A+B: Usual care (n=40) Duration: 12 weeks |
Response rate: 71% CBT, 57% stress management; 33% usual care; p=0.002 |
Not assessed | Cognitive behavior therapy was superior to usual care at most later time points on secondary measures of depression, anxiety, hopelessness, stress, and quality of life |
| Bypassing the Blues (Rollman et al 2009) 11 |
302 Participants with depression after coronary artery bypass graft |
Intervention: Telephonebased collaborative depression care (n=150) Control: Usual care (n=152) Duration: 32 weeks |
Response rate: 50% intervention, 30% control; p<.001 |
No significant difference in cardiac re- hospitalizations Follow-up: 32 weeks |
Intervention patients also had significant improvements in mental health-related quality of life and physical functioning |
| COPES (Davidson et al 2010) 12 |
157 Participants with persistent depression after myocardial infarction or unstable angina |
Intervention: Patient- preference, stepped care with problem solving therapy +/− antidepressants (n=80) Control: Usual care (n=77) Duration: 24 weeks |
Change in BDI symptom score intervention −5.7, control −1.9, p<.001; effect size 0.59 (0.18-1.00) |
Major adverse cardiac events/all-cause mortality 4% (n=3) intervention, 13% (n=10)control, p=0.046 Follow-up: 6 months |
Satisfaction with depression care was higher in the intervention compared to usual care group (p<.001) |
Anti-depressant medications
Concern about the safety of antidepressant medications in cardiac patients emerged from the experience gained from the Cardiac Arrhythmia Suppression Trial (CAST) in which post-myocardial infarction (MI) patients treated with Class 1 antiarrhythmics had increased mortality. Because tricyclic antidepressants belong to the group of Class 1a antiarryhthmics, tricyclic antidepressants are presumed to be unsafe for use in depressed patients with ischemic heart disease.3 Subsequent to CAST, investigators have carefully explored the safety and benefits of newer generation antidepressants in CVD patients.
The first large-scale trial carefully assessing the safety of serotonin-specific reuptake inhibitors (SSRIs) in CVD patients was the Sertraline Treatment of Major Depression in Patients with Acute Myocardial Infarction or Unstable Angina (SADHART).4 In this study, 369 participants with major depressive disorder after MI were randomized to sertraline or placebo. The primary outcome was change in left ventricular ejection fraction (LVEF) at four months. SADHART also assessed the effectiveness of sertraline at reducing depressive symptoms. Sertraline was found to have short-term safety with respect to LVEF as well as safety for secondary outcomes including blood pressure and ECG characteristics.
Although sertraline demonstrated short-term safety, sertraline did not significantly reduce depression symptoms in the overall sample according to the primary depression rating scale. This study, however, was not powered to detect differences in depression symptoms. Subsequent trials have assessed the effectiveness of other antidepressants in CVD patients. Antidepressants tested include citalopram (CREATE)5 and mirtazepine (MIND-IT)6, and of these two, only citalopram resulted in a clear reduction in depression symptoms and increase in depression remission. A Cochrane meta-analysis of antidepressant trials showed that, overall, antidepressants produce a small, but clinically significant reduction in depression symptoms and result in reduced re-hospitalizations for combined cardiac and non-cardiac diagnoses.7
The Cochrane meta-analysis also examined the effect of antidepressants in depressed CVD patients on cardiac outcomes and all-cause mortality. The meta-analysis showed that although antidepressants were associated with lower odds of mortality and recurrent cardiac events, the confidence intervals for these comparisons crossed 1 such that they did not reach the predefined significance level.7 A separate meta-analysis that only included trials of SSRI antidepressants concluded that SSRI use was associated with a significant decrease in CVD readmission (risk ratio 0.63, 95% CI 0.46 to 0.86) and mortality rates (risk ratio 0.56, 95% CI 0.35 to 0.88).8 This meta-analysis, however, included data from non-randomized samples.
Psychotherapy
The largest study of depression treatment in CVD patients is the Enhanced Recovery in Coronary Heart Disease Patients (ENRICHD) trial.9 This study randomized 2500 post-myocardial infarction (MI) patients and tested whether enhanced treatment of depression with cognitive behavioral therapy (augmented by sertraline for treatment non-responders) could improve both depression and event-free survival. While the intervention significantly decreased depressive symptoms, there were no significant differences in all-cause mortality or MI recurrence between the intervention and usual care arms. Subgroup analysis showed that while there was a trend toward benefit in men, there was a nearly significant p-value for harm in women (p < 0.03 for the interaction between arms and gender for MI recurrence/death). Post-hoc adjustment for age and Charlson comorbidity index attenuated the interaction considerably (p<0.20), but there is no other sufficiently-powered trial to determine if this was a chance finding, or if some harm might accrue to female MI patients provided with psychological depression treatment. While the results of ENRICHD were a disappointment to experts in the field of behavioral cardiology, commentators noted that 1) the cognitive behavioral therapy treatment yielded only modest improvements in depression with an effect size of 0.31 (typically considered a ‘small’ effect size) and 2) usual depression care resulted in greater improvements than expected, possibly because some of the depressed cases had adjustment disorder that spontaneously remitted, and possibly because participation in the trial led to greater awareness of depression and this improved usual depression care.
Researchers have subsequently tested other psychological treatments for depression including interpersonal psychotherapy 5 and supportive stress management.10 These approaches overall resulted in small benefits in improving depression on the same order of magnitude as pharmacologic based interventions. No trial of psychological intervention, alone, has yet been associated with a reduction in cardiovascular outcomes or mortality, but as mentioned above, only one has had a sufficient number of patients to actually test this properly.
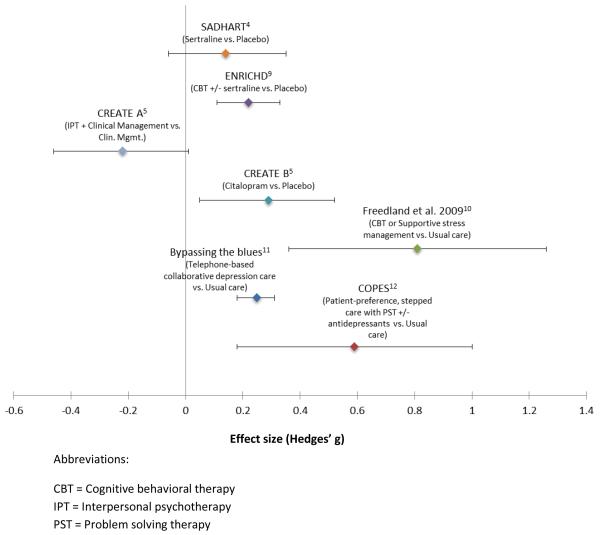
There are a few examples of head-to-head comparisons between different types of psychological interventions or between psychological and pharmacologic interventions for depression treatment in CVD patients.(Figure 1) The Canadian Cardiac Randomized Evaluation of Antidepressant and Pyschotherapy Efficacy Trial (CREATE) involved a full factorial design with four arms: citalopram + interpersonal psychotherapy , citalopram + clinical management, placebo + interpersonal psychotherapy , and placebo + clinical management. In this trial, citalopram outperformed interpersonal psychotherapy in reducing depression in patients with stable coronary artery disease. Freedland et al. compared cognitive behavioral therapy with stress management in post-coronary artery bypass graft (CABG) patients and found cognitive behavioral therapy more effective.10
Figure 1.
Comparison of effect sizes of depression treatments on depression outcomes in patients with cardiovascular disease.
Combined approaches
In mental health and primary care settings, evidence suggests that combinations of psychotherapy and antidepressants are better than either treatment modality alone. Furthermore, many patients hold preferences for one mode of mental health treatment over another. For example, while some patients have heightened concerns about side-effects of antidepressant medications, others are skeptical of the potential for benefitting from psychotherapy or may lack the time and financial resources to attend multiple psychotherapy appointments. Accordingly, in an effort to develop more potent depression interventions, cardiovascular researchers have tested enhanced depression care interventions in which patients choose their initial treatment modality and then are followed by mental health specialists who intensify or “step-up” treatment when depression symptoms are not remitting.11,12 This patient-preference, stepped-care approach resulted in a larger depression treatment effect size in one trial of post-ACS patients (Coronary Psychosocial Evaluation Study; COPES, effect size 0.59).12 Participants in the intervention group of this study were all given access to problem solving psychotherapy at no cost. Notably, the COPES intervention also resulted in a borderline significant short-term reduction in recurrent cardiovascular events (p=0.05).
Other treatments
Exercise is effective at treating depression in the general population. Accordingly, trials are underway to determine whether exercise can compare favorably with antidepressant medications for treating depression in cardiac patients13 and there is speculation that such an approach may also be more effective at improving CVD outcomes. Investigators have also explored whether alternative depression treatments such as omega-3 fatty acids can help increase the effectiveness of antidepressant medications in CVD patients, but found no benefit of omega-3 fatty acids in one recent placebo-controlled clinical trial.14
Other considerations during depression treatment
Adherence to secondary prevention
One of the mechanisms by which depression is believed to influence CVD prognosis is through its adverse impact on adherence to secondary prevention behaviors and risk-factor control. Depressed patients have lower rates of adherence to medications, exercise, smoking cessation, and cardiac rehabilitation attendance among others.15,16 Enhanced treatment of depression, alone, may be insufficient for improving adherence behaviors. One study of CVD patients with depression and comorbid cardiovascular risk factors (systolic blood pressure, LDL cholesterol) found that simultaneous treatment of both depression and risk factors to goal with the assistance of collaborative care managers led to improvements in risk factor control.17 Interestingly, despite improving risk factors and depression, this approach did not improve adherence to medications and improvements in risk factor control were attributed to more intensive titration of medications by clinicians.
The role of beta-blockers
Historically, there have been concerns that beta-blockers, a mainstay of secondary prevention in post-MI patients, cause or exacerbate depression symptoms. Beta-blockers can be associated with adverse side-effects including fatigue and, in some cases, sexual dysfunction. However, rigorously conducted, placebo-controlled, studies have since disproven the conventional wisdom that beta-blockers worsen overall depressive symptoms.18 While this does not preclude the possibility that certain individuals are susceptible to rare depressogenic side-effects of beta-blockers, this class of drug should not be denied to depressed patients for this reason. Instead, careful attention should be paid to ensuring that depressed patients are using all available evidence-based risk-reducing pharmacologic treatments since these patients are at elevated risk for cardiac events.
Unanswered Questions
Who are the optimal patients to target for enhanced depression treatment?
Existent trials of depression treatments have used a heterogeneous set of eligibility criteria, both in terms of the nature of CVD (acute versus stable) and with respect to the severity and timing of depression symptoms. Elevated depressive symptoms frequently remit without treatment after hospitalization for ACS. Hence, targeting depression treatments at persistent, rather than remittent, depressed patients may lead to greater relative benefits. Further, in non-cardiac populations, there is evidence that antidepressant medications are only effective in patients with severe depressive symptoms. Hence, while even mild depressive symptoms confer increased risk in CVD patients, novel interventions may be needed to reduce this type of milder depression in CVD patients. Depression is a heterogeneous condition comprised of both somatic and psychological symptoms. There is data demonstrating that patients with anhedonic (lack interest or pleasure in doing things), but not depressive symptoms have increased risk for poor cardiac outcomes.19 Hence, targeting anhedonic depression may be more effective at improving cardiovascular prognosis. Finally, some studies have shown that patients with first-onset of depression after acute coronary events are at especially high risk for poor subsequent prognosis.20 This may represent an important group of depressed CVD patients to target in future studies.
Should all CVD patients be screened for depression?
Despite the extensive epidemiology connecting depression and poor prognosis in CVD patients, recent surveys have shown that many cardiologists are unaware of the epidemiology associating depression and CVD and even fewer screen or treat depression.21 Accordingly, several professional societies including the American Association of Family Physicians and multiple European societies of cardiovascular disease prevention have published guidelines for the management of depression in CVD patients and, in 2008, the American Heart Association (AHA) published a science advisory recommending routine screening for depression in CVD patients.22 This AHA publication led to considerable controversy by leaders in the field. On the one hand, proponents argued that depression screening when tied to depression care management programs is already evidence-based for primary care and can be assessed with as few as two questions. Proponents further argued that depression treatments appear to be safe and similarly effective at reducing depression in CVD patients as compared to the general population, and may potentially improve prognosis. Others, however, are concerned that there is insufficient information to recommend depression screening.23 Many patients identified through screening will have mild symptoms that are unlikely to benefit from current treatments and which may spontaneously remit. Further, while depression treatments appear to be safe, there was a trend toward harm from psychological treatment among women in ENRICHD and the long-term consequences of newer generation antidepressants in CVD patients remain poorly understood. Those opposed to universal screening point out that while screening may be brief, the consequences of screening may consume significant health care resources with unclear benefits.24
Summary and recommendations for treating depression in CVD patients
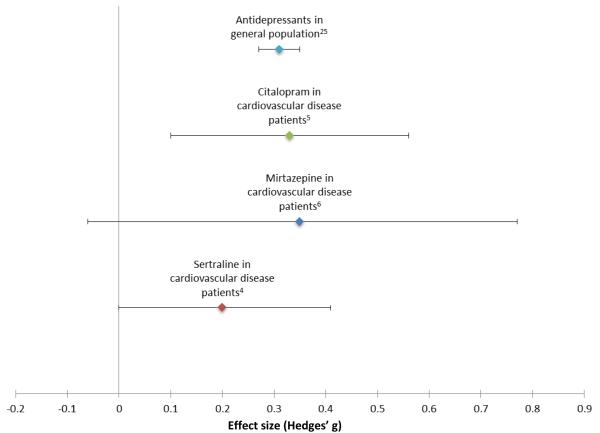
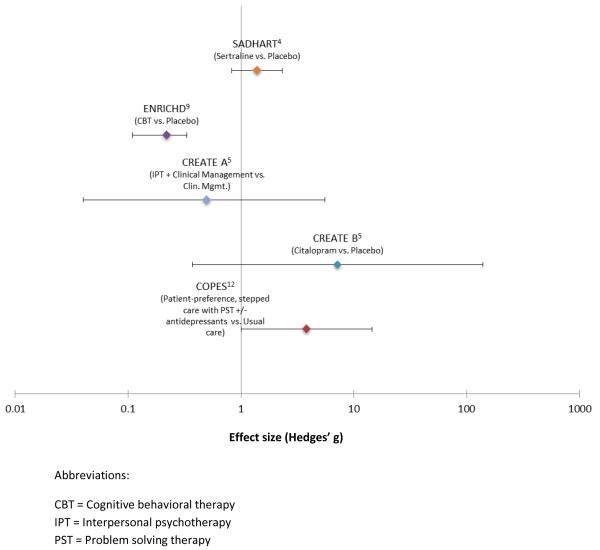
A variety of depression treatments are effective in depressed CVD patients. Although there is a need to develop more potent depression interventions for CVD patients, the effect size of such treatments with respect to reducing depression is similar in CVD patients as compared to the general population. (Figure 2) Other than one trial for which the effect of the intervention on prognosis was a secondary outcome12, depression treatment has not thus far been proven to offset the risk of depression on cardiovascular prognosis. However, only one trial of depression treatment has been adequately powered to assess this outcome, and when analyzed together, depression interventions show promise for being able to not only reduce depression, but reduce major adverse cardiac events and mortality as well.(Figure 3) Accordingly, there is a need for additional trials of our most potent depression interventions in CVD patients.
Figure 2.
The effect sizes of pharmacotherapy for depression are similar in trials of patients with cardiovascular disease as compared to the general population. The estimate for the effect size of antidepressants in the general population is based on a systematic review of 125 published and unpublished trials.25
Figure 3.
Comparison of effects sizes of depression treatments on cardiovascular outcomes and/or all-cause mortality in patients with cardiovascular disease
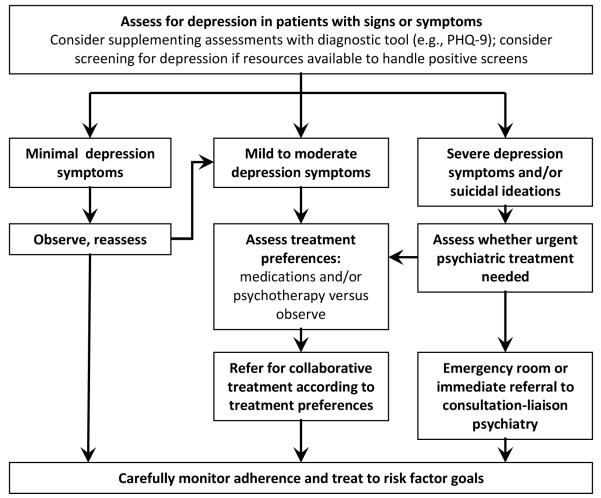
Until these definitive trials have been performed, patients who present with symptoms or signs of depression should be carefully interviewed to assess for the severity of symptoms and the risk of suicide.(Figure 4) Clinicians can also consider screening all CVD patients for depression, however current evidence has not verified that this is a cost-effective approach. Structured depression assessment tools like the Patient Health Questionnaire-9, comprised of 9 items that ask about the frequency of symptoms used to diagnose depression according to the Diagnostic and Statistical Manual (DSM-IV) classification system, can be useful supplements to clinical interviews. In addition, serial measurements of depression severity using such tools can be helpful for tracking the effectiveness of depression treatments. Patients with minimal symptoms can be observed with a plan to re-assess symptoms at a later date. In contrast, patients with severe symptoms or at risk for suicide should be urgently assessed by a mental health specialist. Patients with mild to moderate symptoms should be educated about treatment options and should then be asked for their preferred approach. Unless patients have severe symptoms or are at risk for suicide, observation with scheduled follow-up remains a reasonable option as depression symptoms may spontaneously remit especially if they developed after acute coronary events. Clinicians will benefit by being informed as to the availability and affordability of treatment options in their health care system, especially non-pharmacologic ones. Ideally, clinicians will have identified mental health specialists or collaborative care managers with expertise in managing patients with comorbid depression and CVD. With patient preferences in mind, patients can then be referred to appropriate specialists and/or antidepressants can be initiated by the treating provider. Close collaboration with mental health specialists or other members of the treatment team will be important to ensure that depression treatment is optimized. Clinicians should be cautioned that these recommendations are opinion-based, and not evidence-based, as neither a depression screening or CVD outcome randomized trial has been performed yet to directly inform clinical practice.
Figure 4.
Algorithm for managing depression in patients with cardiovascular disease
Other than ensuring that depressed patients are receiving appropriate depression treatment, clinicians should pay special attention to risk factor control and to adherence problems. The use of non-judgmental language during adherence assessments and possibly, validated adherence assessment tools such as the Morisky Medication Adherence Questionnaire, may facilitate more accurate adherence assessments.
Acknowledgments
Dr. Kronish is funded by grant K23HL098359 from the National Heart, Lung, and Blood Institute
References
- 1.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–13. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 2.van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66:814–22. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 3.Glassman AH, Roose SP, Bigger JT., Jr The safety of tricyclic antidepressants in cardiac patients. Risk-benefit reconsidered. JAMA. 1993;269:2673–5. [PubMed] [Google Scholar]
- 4.Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–9. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 5.Lesperance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–79. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 6.Honig A, Kuyper AM, Schene AH, et al. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med. 2007;69:606–13. doi: 10.1097/PSY.0b013e31814b260d. [DOI] [PubMed] [Google Scholar]
- 7.Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions for depression in patients with coronary artery disease. Cochrane Database Syst Rev. 2011;9:CD008012. doi: 10.1002/14651858.CD008012.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pizzi C, Rutjes AW, Costa GM, Fontana F, Mezzetti A, Manzoli L. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am J Cardiol. 2011;107:972–9. doi: 10.1016/j.amjcard.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106–16. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 10.Freedland KE, Skala JA, Carney RM, et al. Treatment of depression after coronary artery bypass surgery: a randomized controlled trial. Arch Gen Psychiatry. 2009;66:387–96. doi: 10.1001/archgenpsychiatry.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rollman BL, Belnap BH, LeMenager MS, et al. Telephone-delivered collaborative care for treating post-CABG depression: a randomized controlled trial. JAMA. 2009;302:2095–103. doi: 10.1001/jama.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davidson KW, Rieckmann N, Clemow L, et al. Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms: coronary psychosocial evaluation studies randomized controlled trial. Arch Intern Med. 2010;170:600–8. doi: 10.1001/archinternmed.2010.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blumenthal JA, Sherwood A, Rogers SD, et al. Understanding prognostic benefits of exercise and antidepressant therapy for persons with depression and heart disease: the UPBEAT study--rationale, design, and methodological issues. Clin Trials. 2007;4:548–59. doi: 10.1177/1740774507083388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carney RM, Freedland KE, Rubin EH, Rich MW, Steinmeyer BC, Harris WS. Omega-3 augmentation of sertraline in treatment of depression in patients with coronary heart disease: a randomized controlled trial. JAMA. 2009;302:1651–7. doi: 10.1001/jama.2009.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med. 2005;165:2508–13. doi: 10.1001/archinte.165.21.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kronish IM, Rieckmann N, Halm EA, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med. 2006;21:1178–83. doi: 10.1111/j.1525-1497.2006.00586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Melle JP, Verbeek DE, van den Berg MP, Ormel J, van der Linde MR, de Jonge P. Beta-blockers and depression after myocardial infarction: a multicenter prospective study. J Am Coll Cardiol. 2006;48:2209–14. doi: 10.1016/j.jacc.2006.07.056. [DOI] [PubMed] [Google Scholar]
- 19.Davidson KW, Burg MM, Kronish IM, et al. Association of anhedonia with recurrent major adverse cardiac events and mortality 1 year after acute coronary syndrome. Arch Gen Psychiatry. 2010;67:480–8. doi: 10.1001/archgenpsychiatry.2010.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parker GB, Hilton TM, Walsh WF, et al. Timing is everything: the onset of depression and acute coronary syndrome outcome. Biol Psychiatry. 2008;64:660–6. doi: 10.1016/j.biopsych.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 21.Feinstein RE, Blumenfield M, Orlowski B, Frishman WH, Ovanessian S. A national survey of cardiovascular physicians’ beliefs and clinical care practices when diagnosing and treating depression in patients with cardiovascular disease. Cardiol Rev. 2006;14:164–9. doi: 10.1097/01.crd.0000200977.41695.43. [DOI] [PubMed] [Google Scholar]
- 22.Lichtman JH, Bigger JT, Jr., Blumenthal JA, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–75. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 23.Thombs BD, de Jonge P, Coyne JC, et al. Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA. 2008;300:2161–71. doi: 10.1001/jama.2008.667. [DOI] [PubMed] [Google Scholar]
- 24.Ziegelstein RC, Thombs BD, Coyne JC, de Jonge P. Routine screening for depression in patients with coronary heart disease never mind. J Am Coll Cardiol. 2009;54:886–90. doi: 10.1016/j.jacc.2009.01.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358:252–60. doi: 10.1056/NEJMsa065779. [DOI] [PubMed] [Google Scholar]