Abstract
Background
Cardiac troponin levels help risk-stratify patients presenting with an acute coronary syndrome (ACS). Although they may be elevated in patients presenting with Non-ACS conditions, specific diagnoses and long-term outcomes within that cohort are unclear.
Methods and Results
Using the Veterans Affairs (VA) centralized databases, we identified all hospitalized patients in 2006 who had a troponin assay obtained during their initial reference hospitalization. Based on ICD-9 diagnostic codes, primary diagnoses were categorized as either ACS or Non-ACS conditions. Of a total of 21,668 patients with an elevated troponin level who were discharged from the hospital, 12,400 (57.2%) had a Non-ACS condition. Among that cohort, the most common diagnostic category involved the cardiovascular system and congestive heart failure (N=1661) and chronic coronary artery disease (N=1648) accounted for the major classifications. At one-year following hospital discharge, mortality in patients with a Non-ACS condition was 22.8% and was higher than the ACS cohort (Odds Ratio=1.39; 95%CI: 1.30–1.49). Despite the high prevalence of cardiovascular diseases in patients with a Non-ACS diagnosis, utilization of cardiac imaging within 90 days of hospitalization was low compared with ACS patients (Odds Ratio=0.25; 95%CI: 0.23–0.27).
Conclusions
Hospitalized patients with an elevated troponin level most often have a primary diagnosis that is not an acute coronary syndrome. Their long-term survival is poor and justifies novel diagnostic or therapeutic strategy-based studies to target the highest risk subsets prior to hospital discharge.
Keywords: outcomes, troponins, non-ACS diagnosis, cardiac imaging, coronary artery disease
Cardiac troponins have gained widespread acceptance as an optimal specific cardiac biomarker for timely risk-stratification of patients presenting to the hospital with an acute coronary syndrome (ACS). Among patients with an ACS and an elevated troponin level that exceeds the upper reference limit (URL), an early invasive strategy reduces the long-term risk of death and non-fatal myocardial infarction at one year (1–3). In many conditions that are not diagnosed as an acute coronary syndrome, troponin levels can be elevated above the upper reference limit (4) and may have value as a biomarker for predicting future outcomes in selected conditions (5–11). In the absence of guidelines for specific therapies in this heterogeneous cohort, there is confusion about the need for additional diagnostic or therapeutic interventions (12–14). To address this diagnostic dilemma, a Consensus Statement on the Redefinition of Myocardial Infarction (MI) has categorized patients with an elevated troponin into acute coronary syndrome (Type 1 MI) which is distinctly different from those conditions which are associated with heterogeneous clinical presentations and are not a primary acute coronary syndrome (Non-ACS conditions) (15). The prevalence of Non-ACS conditions with elevated troponin levels relative to an ACS remains unclear, in part, because of limited observational studies within a large healthcare system. Accordingly, by using the Department of Veterans Affairs (VA) centralized database for all hospitalized patients in 2006, we identified the population of hospitalized VA patients with a troponin assay, categorized their primary diagnoses as either an acute coronary syndrome or Non-ACS condition and determined their long-term outcomes.
METHODS
Using VA centralized utilization databases, encompassing patient treatment file, lab results and the Beneficiary Information and Records Locator Subsystem (BIRLS) files, we identified records for all patients who received a troponin assay test during an inpatient stay in FY2006. Because individual patients might have more than one inpatient hospital stay in one year, and because we were interested in determining the outcomes for patients following their first elevated troponin result, we identified the first or reference hospitalization for each patient. These inpatient stays were categorized as acute coronary syndrome (ACS) if any one of the following diagnoses were included in the data of that first hospitalization (ICD-9 codes: 410.×, 411.×, 413.×, 420.×, 425.1, 415.1). Reliability of these codes from patient records has been previously documented (16). All inpatient stays that did not include any of these diagnoses associated with an acute coronary syndrome were categorized as Non-ACS conditions. On the assumption that some patients were so sick that they might not have been deemed eligible for cardiac imaging, we excluded data for those patients who either died during the first hospitalization or who had a low expectation of survival based on either a discharge to hospice or a skilled or community nursing facility, or an initial inpatient hospital stay of more than 30 days. We then identified the highest troponin result in the reference hospital stay for each patient that received the lab test. We were unable to determine the timing of the lab test relative to the time of the admission. In order to classify whether the highest troponin assay results exceeded the 99th percentile upper reference limit (URL), it was necessary to identify the hospital-specific reference limits for each assay method used in FY2006. Because the reference limits are instrument–specific (troponin T or troponin I) and the technology changes rapidly, it was also necessary to use fiscal quarter-specific reference limits to define the results as exceeding the 99th percentile of the upper reference limit. Using criteria defined for VA quality improvement initiatives, we characterized each troponin lab result that exceeded the 99th percentile of the upper reference limit for each reference hospitalization, medical center and each quarter of the fiscal year. In the next step, we gathered the utilization data for each patient for one year following the reference hospitalization. We then identified whether the patients received any cardiac imaging test (coronary angiography or stress nuclear imaging) during the reference hospitalization or within 90 days of the first hospitalization. We also determined whether patients were re-hospitalized or died during the one year following initial hospitalization. We calculated rates and odds ratios (OR) and 95% confidence intervals (CI) comparing results for patients with a Non-ACS diagnosis relative to the ACS cohort stratified to their in-hospital troponin levels.
RESULTS
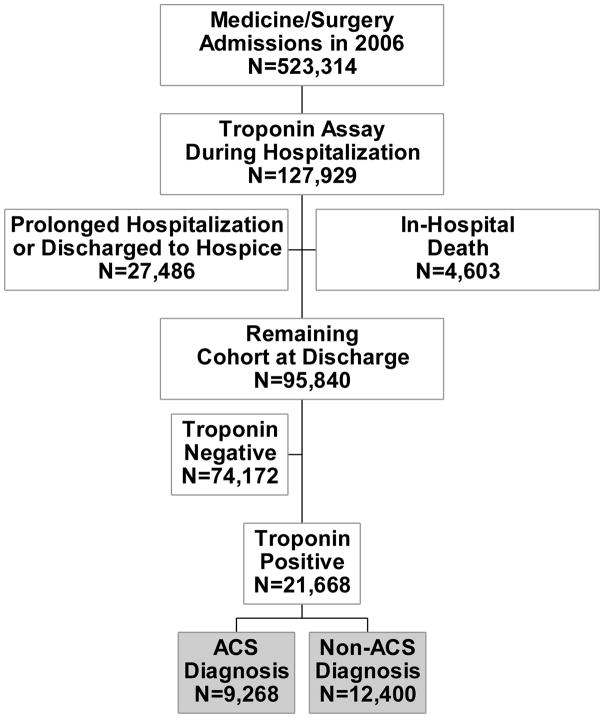
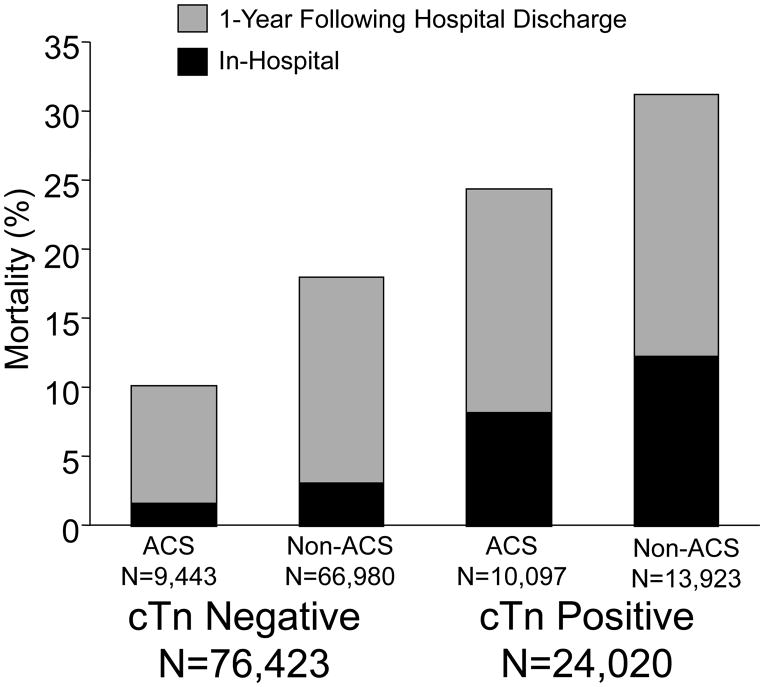
In 2006, 523,314 unique patients were admitted to VA Medical Centers and 127,929 (24.4%) had a troponin measurement reported during their reference hospitalization period. Because the focus of our analysis was on long-term outcomes, data from 27,486 patients were excluded from additional analysis because of a low expectation of survival, based on either a subsequent transfer to hospice or extended care facility or a hospital stay of greater than 30 days. Of the remaining 100,433 patients with a troponin assay obtained during hospitalization, 4,633 patients died within the hospital (Figure 1). Among the cohort with an elevated troponin level, in-hospital mortality was higher in patients with a Non-ACS diagnosis than in those individuals with an ACS (OR=1.373: 95% CI 1.257–1.501). Mortality rates during hospitalization and at one-year mortality following hospital discharge were determined in all hospitalized patients with a troponin assay and as expected, were higher in the cohorts with a positive troponin level (Figure 2).
Figure 1.
The study cohort was obtained from all admissions to VA Medical Centers in 2006 who had a troponin assay obtained during the reference hospitalization. Those patients with a low expectation of long-term survival, based on either a prolonged hospitalization or transfer to hospice care, were censored from additional analyses. A comparative analysis of the long-term outcomes were determined according to the diagnosis of either an acute coronary syndrome (ACS) or Non-ACS condition in those patients with an elevated troponin level who were discharged from the hospital.
Figure 2.
The in-hospital and 1-year post-hospital discharge mortality rates were determined for the 100,433 hospitalized patients who had a troponin level drawn during hospitalization in 2006. Outcomes are displayed according to the ICD-9 diagnosis of an acute coronary syndrome (ACS) or Non-ACS condition and whether the troponin (cTn) level was negative or positive, based on the upper reference limit of the specific assay.
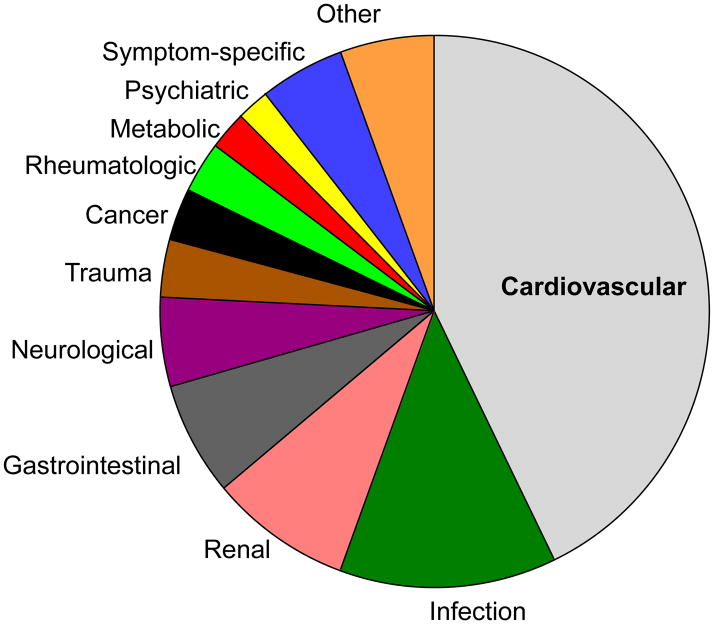
Among all 13,923 hospitalized patients with an elevated troponin level and a Non-ACS condition, ICD-9 coded diagnoses were further grouped according to the specific disease processes and the cardiovascular system accounted for more than 40% of the primary diagnostic categories (Figure 3). In that cohort, 12,400 patients were discharged from the hospital and the most common diagnostic descriptors within the cardiovascular system was congestive heart failure and chronic coronary atherosclerosis and was the principal diagnosis in 3,309 (26.7%) patients (Table 1).
Figure 3.
The primary diagnoses based on the ICD-9 codes are shown for all 13,923 hospitalized patients with an elevated troponin level and a Non-ACS condition. The most common discharge diagnosis involved the cardiovascular system.
Table 1.
The frequency of primary diagnoses for the 12,400 patients who were discharged from the hospital with a Non-ACS condition and an elevated troponin level is shown.
| Diagnostic Description | ICD-9 Code | Number (%) |
|---|---|---|
| Congestive Heart Failure (unspecified) | 428.0 | 1661 (13.4%) |
| Coronary atherosclerosis (native coronary artery) | 414.01 | 1648 (13.3%) |
| Chest pain (other) | 786.59 | 868 (7.0%) |
| Pneumonia | 486 | 526 (4.2%) |
| Atrial fibrillation | 427.31 | 461 (3.7%) |
| COPD with acute exacerbation | 491.21 | 399 (3.2%) |
| Acute renal failure unspecified | 584.9 | 274 (2.2%) |
| Urinary tract infection, site not specified | 599.0 | 221 (1.8%) |
| Syncope and/or collapse | 780.2 | 215 (1.7%) |
Among the 12,400 discharged patients with an elevated troponin, the mortality rate at 1-year following hospital discharge was 22.8% for patients with a Non-ACS condition and 17.5% for patients with an ACS diagnosis (OR=1.389: 95% CI 1.298–1.487). Utilization of cardiac imaging was lower in those patients with a Non-ACS condition, both during the hospital period (OR=0.248: 95% CI 0.232–0.266) as well as within the 90 days following hospital discharge (OR=0.564: 95%CI 0.505–0.629) (Table 2). When considering the influence of cardiac imaging on survival in the patients with an elevated troponin and Non-ACS condition, the risk of death was nearly 2.5-fold higher when no cardiac imaging test was performed during the hospitalization (OR 2.497: 95% CI 2.134–2.921) and remained higher when no cardiac imaging test was performed within 90 days of discharge (OR 2.068: 95% CI 1.675–2.554). The average time from hospitalization to death for the cohort with an elevated troponin and Non-ACS condition was 55.6 days when no cardiac imaging was obtained, 140.2 days with cardiac imaging during hospitalization, and 162.7 days with cardiac imaging within 90 days of discharge from the reference hospitalization.
Table 2.
Long-term outcomes and utilization rates of cardiac imaging tests are shown for patients with an elevated troponin level according to their discharge diagnosis of ACS versus Non-ACS.
| Group | 1-Year Mortality | Cardiac Imaging Test* |
|---|---|---|
| ACS Cohort (N=9,268) | 1,625 (17.5%) | 4,172 (45.0%) |
| Non-ACS Cohort (N=12,400) | 2,827 (22.8%) | 2,371 (19.1%) |
| Odds Ratio (95%Confidence Intervals) | 1.389 (1.298–1.487) | 0.564 (0.505–0.629) |
Coronary angiography or nuclear stress imaging tests performed either during hospitalization or within 90 days following hospital discharge.
DISCUSSION
The principal finding of this study is that troponin measurements are frequently obtained in hospitalized patients within VA Medical Centers and if abnormally elevated, are common among patients presenting with a condition other than an acute coronary syndrome (ACS). In those patients with an elevated troponin level, a Non-ACS diagnosis is associated with an increased risk of long-term mortality when compared with patients presenting with an ACS. Among the troponin positive cohort with a Non-ACS condition, the most frequent ICD diagnostic code involved the Cardiovascular System and within that group, congestive heart failure and chronic coronary artery disease accounted for the most common clinical diagnoses. Despite the high prevalence of advanced chronic cardiac diseases, the utilization rate of cardiac imaging for the presence of myocardial ischemia was low within the first 3 months following admission when compared with those patients who were diagnosed with an ACS.
To address the potential diagnostic dilemma about the interpretation of elevated troponin levels, a Consensus Statement on the Redefinition of MI has categorized patients with an elevated troponin level into acute coronary syndrome (Type 1 MI) which differs from those conditions which are associated with heterogeneous clinical presentations that are not related to an acute coronary syndrome (Non-ACS conditions) (15). Although the pathophysiology of a Type 2 MI remains speculative, this is assumed to be a secondary myocardial ischemic event that is a result of an unstable systemic hemodynamic condition. A Type 4 MI is observed during coronary artery revascularization procedures with either PCI or CABG and they have been censored from this analysis. In the absence of a rise and fall of the troponin level in a patient without a clinical correlate of myocardial ischemia, elevated troponin levels can be nonspecific, particularly with chronic conditions involving congestive heart failure and renal failure.
The reason for the low utilization rate of additional cardiac testing in this cohort is unclear but is likely multi-factorial. It is conceivable that clinicians have the perception that myocardial ischemia is not a major contributor to poor outcomes in patients with Non-ACS conditions and consequently, do not plan for additional testing following hospital discharge. In support of this contention, a report of septic ICU patients with labile hemodynamic conditions showed that a substantial number of patients had elevated troponin concentrations and in the absence of an ACS diagnosis, were subsequently found to have a low probability of significant obstructive coronary artery disease by non-invasive stress imaging (17). More recently however, longitudinal studies involving patients who initially present to the emergency department with an elevated troponin level and a non-cardiac condition as the primary problem had a high prevalence of clinical correlates of myocardial ischemia during hospitalization (18, 19). In addition, consecutive patients who had been admitted to an ICU with an elevated cardiac troponin level and a Non-ACS diagnosis were analyzed subsequent to their hospitalization and mortality was high, with a significant percentage of the individuals demonstrating advanced multi-vessel coronary artery disease (20). These data are more consistent with our cohort of aging veterans, based on the observation that the primary ICD-9 codes in the patients with a Non-ACS diagnosis most commonly involved the Cardiovascular System, with congestive heart failure and chronic coronary artery disease accounting for the primary specific diagnoses. In fact, it is conceivable that clinicians who evaluated these patients after admission did not believe that additional cardiac imaging would be needed, in therapeutic clinical decision-making processes. It is interesting however, that additional cardiac stress imaging within 90 days of hospitalization was associated with improved outcomes, in those patients with a Non-ACS condition.
Clinicians are well aware of the utility of troponin measurements for risk-stratification of patients presenting with an ACS, and if elevated, identifies a subset of individuals who benefit from early aggressive interventions during hospitalization (1–3). Among patients who have been admitted with Non-ACS conditions, the utility of troponin levels as a biomarker is beneficial in selected subsets (4, 11) but the value for additional therapies beyond traditional risk factor modification is unknown. It is a reasonable assumption that earlier cardiac imaging for the presence of coronary artery disease would improve outcomes in a cohort of patients with Non-ACS diagnoses and an elevated cardiac biomarker, though this has not been studied prospectively. The redefinition of myocardial infarction into various types has been an important step in alerting the clinicians to underlying mechanisms of supply-demand ischemia in subsets of patients (15). Despite the causes of the elevated troponin levels however, the poor outcomes among all cohorts need to be recognized, to advance timely therapies. Patients with a low level of troponin release in the blood has been observed in a population with stable coronary artery disease, implying that a significant degree of ischemia may be a causative factor (21). Therefore, an earlier diagnosis of occult coronary artery disease with a more timely consideration of interventions that are known to improve outcomes might be a reasonable strategy. Therapies including high dose statins and strong anti-platelet agents such as ADP inhibitors are now considered important adjunctive therapies, based on proven efficacy in ACS patients, even independent of revascularization procedures (22, 23). Whether these pharmacological interventions should be advanced to patients without an ACS presentation remain speculative and will require additional randomized controlled strategy-based studies in targeted patients. With the advent of newer high sensitivity troponin assays, serial measurements may be a better way of risk-stratifying patients, particularly those individuals with chronic heart failure as the cause (24).
The unique feature of this study is that it summarizes data extracted from a large health care system across the country, involving more than 523,000 hospitalized patients and cross-references discharge diagnoses with results of cardiac biomarkers, outcomes at one year, and utilization rates of cardiac imaging within 3 months of discharge. A limitation of our study is that outcomes were not determined in the patients who did not have troponins drawn during the hospitalization and therefore, we cannot generalize our results to all hospitalized patients. Bias can be created among patients admitted through the emergency department and we can only speculate that those with biomarkers drawn were the highest risk. We assume that the cardiac biomarker was obtained at the time of admission, but the total number of troponins and the time they were drawn in each patient relative to admission and discharge dates is unavailable. We also cannot evaluate therapies that were instituted as a result of the elevated troponin level, nor can we fully understand the clinical rationale for not getting cardiac imaging during follow-up visits. We assume that this group may have had the highest cardiac risks but those data are not available. An additional point worth mentioning is the variability in troponin assays at some medical centers during this time period. Although the manufacturer’s guidelines used a threshold for the upper reference limit (URL), the high coefficient of variation with some assays may have lead to insensitivities of some measurements. In time, higher sensitivity troponin assays may allow for a more standardized analysis in such cohorts.
In conclusion, troponin assays are frequently obtained in hospitalized patients and if elevated, are commonly observed in patients with a diagnosis other than acute coronary syndrome (ACS). These patients have a poor outcome following hospital discharge, in part, because of no proven therapies and a lack of strategy-based studies that can target high-risk subsets prior to hospital discharge.
Acknowledgments
Funding Source: Department of Veterans’ Affairs Cooperative Studies Program
Footnotes
There are no Potential Conflicts of Interest from any authors, related to this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cannon C, Weintraub W, Demopoulos L, Vicari R, Frey M, Lakkis N, Neumann F, Robertson D, DeLucca P, DiBattiste P, Gibson M, Braunwald E. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001;344:1879–87. doi: 10.1056/NEJM200106213442501. [DOI] [PubMed] [Google Scholar]
- 2.Mehta S, Cannon C, Fox K, Wallentin L, Boden W, Spacek R, Widinsky L, McCullough P, Hunt D, Braunwald E, Yusuf S. Routine vs selective invasive strategies in patients with acute coronary syndromes. A collaborative meta-analysis of randomized trials. JAMA. 2005;293:2908–17. doi: 10.1001/jama.293.23.2908. [DOI] [PubMed] [Google Scholar]
- 3.Braunwald E, Antman E, Beasley J, Califf R, Cheitlin M, Hochman J, Jones R, Kereiakes D, Kupersmith J, Levin T, Pepine C, Schaeffer J, Smith E, III, Steward D, Theroux P. ACC/AHA Guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction-2002: Summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the management of patients with unstable angina) Circulation. 2002;106(14):1893–900. doi: 10.1161/01.cir.0000037106.76139.53. [DOI] [PubMed] [Google Scholar]
- 4.Kelley W, Januzzi J, Christenson R. Increases of cardiac troponin in conditions other than acute coronary syndrome and heart failure. Clin Chem. 2009;55:2098–2112. doi: 10.1373/clinchem.2009.130799. [DOI] [PubMed] [Google Scholar]
- 5.Maynard C, Lowy E, Rumsfeld J, Sales A, Sun H, Kopjar B, Fleming B, Jesse R, Rusch R, Fihn S. The Prevalence and Outcomes of In-Hospital Acute Myocardial Infarction in the Department of Veterans Affairs Health System. Arch Intern Med. 2006;166:1410–16. doi: 10.1001/archinte.166.13.1410. [DOI] [PubMed] [Google Scholar]
- 6.Quenot J, Le Teuff G, Quantin C, Doise J, Abrahamowicz M, Masson D, Blettery B. Myocardial Injury in Critically Ill Patients: Relation to Increased Cardiac Troponin I and Hospital Mortality. Chest. 2005;128:2758–2764. doi: 10.1378/chest.128.4.2758. [DOI] [PubMed] [Google Scholar]
- 7.Stein R, Gupta B, Agarwal S, Golub J, Bhutani D, Rosman A, Eng C. Prognostic implications of normal (<0.10 ng/ml) and borderline (0.10 to 1. 49 ng/ml) troponin elevation levels in critically ill patients without acute coronary syndrome. Am J Cardiol. 2008;102:509–512. doi: 10.1016/j.amjcard.2008.04.026. [DOI] [PubMed] [Google Scholar]
- 8.Alcalai R, Planer D, Culhaoglu A, Osman A, Pollak A, Lotan C. Acute coronary syndrome vs nonspecific troponin elevation: clinical predictors and survival analysis. Arch Intern Med. 2007;167:276–281. doi: 10.1001/archinte.167.3.276. [DOI] [PubMed] [Google Scholar]
- 9.Lim W, Cook D, Griffith L, Crowther M, Devereaux P. Elevated cardiac troponin levels in critically ill patients: prevalence, incidence, and outcomes. Am J Crit Care. 2006;15:280–288. [PubMed] [Google Scholar]
- 10.Ammann P, Maggiorini M, Bertel O, Haenseler E, Joller-Jemelka H, Oeschslin E, Minder E, Rickli H, Fehr T. Troponin as a risk factor for mortality in critically ill patients without acute coronary syndromes. J Am Coll Cardiol. 2003;41:2004–9. doi: 10.1016/s0735-1097(03)00421-2. [DOI] [PubMed] [Google Scholar]
- 11.Waxman D, Hecht S, Schappert J, Husk G. A model for troponin I as a quantitative predictor of in-hospital mortality. J Am Coll Cardiol. 2006;48:1755–62. doi: 10.1016/j.jacc.2006.05.075. [DOI] [PubMed] [Google Scholar]
- 12.Pierpont G, McFalls E. Interpreting troponin elevations: do we need multiple diagnoses? European Heart Journal. 2009;30:135–138. doi: 10.1093/eurheartj/ehn517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim W, Holinski P, Devereaux P, Tkaczyk A, McDonald E, Clarke F. Detecting myocardial infarction in critical illness using screening troponin measurements and ECG recordings. Crit Car. 2008;12:R36. doi: 10.1186/cc6815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jesse R. On the relative value of an assay versus that of a test: a history of troponin for the diagnosis of myocardial infarction. J Am Coll Cardiol. 2010;55:2118–24. doi: 10.1016/j.jacc.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 15.Thygesen K, Alpert J, White H, Jaffe A, Apple F, Galvani M, Katus H, Neweby L, Ravkilde J. Universal Definition of Myocardial Infarction. Circulation. 2007;116:2634–2653. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]
- 16.Petersen L, Wright S, Normand S, Daley J. Positive predictive value of the diagnosis of acute myocardial infarction in an administrative database. J Gen Intern Med. 1999;14:555–558. doi: 10.1046/j.1525-1497.1999.10198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maeder M, Fehr T, Rickli H, Ammann P. Sepsis-associated myocardial dysfunction: diagnostic and prognostic impact of cardiac troponins and natriuretic peptides. Chest. 2006;129:1349–1366. doi: 10.1378/chest.129.5.1349. [DOI] [PubMed] [Google Scholar]
- 18.Lim W, Whitlock R, Khera V, Devereaux P, Tkaczyk A, Heels-Ansdell D, Jacka M, Cook D. Etiology of troponin elevation in critically ill patients. J Crit Care. 2010;25:197–205. doi: 10.1016/j.jcrc.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Llva T, Eskola M, Nikus K, Voipio-Pulkki L, Lund J, Pulkki K, Mustonen H, Niemela K, Karhunen P, Porela P. The etiology and prognostic significance of cardiac troponin I elevation in unselected emergency department patients. J of Emergency Medicine. 2010;38:1–5. doi: 10.1016/j.jemermed.2007.09.060. [DOI] [PubMed] [Google Scholar]
- 20.Blich M, Sebbag A, Attias J, Aronson D, Markiewicz W. Cardiac troponin I elevation in hospitalized patients without acute coronary syndromes. Am J Cardiol. 2008;101:1384–1388. doi: 10.1016/j.amjcard.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Wallace T, Abdulah S, Drazner M, Das S, Khera A, McGire D, Wlans F, Sabatine M, Morrow d, de Lemos J. Prevalence and determinants of troponin T elevation in the general population. Circulation. 2006;113:1958–1965. doi: 10.1161/CIRCULATIONAHA.105.609974. [DOI] [PubMed] [Google Scholar]
- 22.Cannon C, Braunwald E, McCabe C, Rader D, Rouleau J, Belder R, Joyal S, Hill K, Pfeffer M, Skene A. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1494–1504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- 23.CURE-Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 24.deFillipi C, de Lemos J, Christenson R, Gotttdiener J, Kop W, Zhan M, Seliger S. Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA. 2010;304:2494–2502. doi: 10.1001/jama.2010.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]