Abstract
Compare with pneumonectomy, sleeve lobectomy has advantage in long-term outcomes and cost-effective measures. As a result, sleeve lobectomy procedure is considered and practiced as the standard therapy for central lung cancers which are anatomically suitable regardless of lung function. In some cases, the lesion invades hilar and mediastinal vessels, the surgeon may faces more technically challenging in vascular reconstruction procedures together with the sleeve lobectomy procedure. The advent of minimally invasive surgery brings numerous advantages, such as shorter hospital stay, alleviated post-operative pain, faster recover and so on, to the patient. In return, it did demands all the surgeons to master the VATS surgery operative skill to meet the patient’s expectation. Although mirror the pathway of open sleeve surgery, the video-assisted bronchial sleeve lobectomy (VABSL) brings numerous obstacles for the surgeon: One needs to accommodate transmission from direct-view to locally 2D screen, from multi-angle multi-direction operation field to one directional operation field, before he can adapt to the VATS operative skill. In addition, VATS surgery did have its’ learning curve for the surgeon and the assistant. Here we present a video of a patient underwent sleeve lobectomy with partial pulmonary artery resection for communicating operative techniques.
KEY WORDS : Video-assisted thoracic surgery (VATS), sleeve lobectomy, pulmonary artery resection, video, case
Introduction
Initially, sleeve lobectomy was considered as an alternative procedure to pneumonectomy for patients with low-grade, centrally located lesions and limited cardiopulmonary reserve. While, as the rapid development of surgical techniques in last decades, sleeve lobectomy has become the first line intervention, rather than a compromise to pneumonectomy, for centrally located lesions of all grades. With the widespread of thoracoscopic instrument, video-assisted bronchial sleeve lobectomy (VABSL), a minimally invasive with more technically challenging procedure, has gradually been an attractive treatment option for qualifying patients. In addition, since the relatively narrow indications and exquisite skill demands double sleeve cases is sparsely reported. Here we present a VATS left upper double sleeve lobectomy case (Video 1) for communicating operative techniques.
Video 1.
VATS left upper sleeve lobectomy with partial pulmonary artery resection.
Indications
Sleeve lobectomy is commonly indicated for lesions involving main or lobar bronchi. So the flexible bronchoscopy is the most important diagnostic step in identifying potential candidates for sleeve procedure. Further, the tissue biopsy can also be done by bronchoscopy to defining the malignancy and to assess the tumor extension. In addition, Computed tomography (CT) as well as Magnetic resonance imaging (MRI), which provides better appreciation of lesion size, extent and location relative to thoracic structures, play a supplement role to bronchoscopy in assessing the potential candidates. In addition to anatomic location, the lymph node metastasis condition, i.e. the N factor, is another important factor for potential candidates screening. The presence of N2 does not contraindicate the sleeve procedure while impairs long term outcomes for the risk of systemic recurrences.
History
Male, 64 years old.
Two weeks before his admission to our institution, the patient suffered from irritable cough, blood-stained sputum without any apparent cause and disclaimed of shortness of Breath, chest tightness. The patient was given anti-inflammatory, hemostasis therapy and the chest computed tomography (CT) in local hospital. The chest computed tomography (CT) shows a mass in the left hilum.
In 2012-11-01, the patient is admitted to Oncology department of our hospital to complete the medical examinations. History, clinical and laboratory data indicate the patient’s cardio-pulmonary function is in good condition and without any sign of metastasis. Chest computed tomography (CT) shows a mass in the left hilum (Figure 1). Bronchoscope examination shows a neoplasm in the orifice of Left Upper Lobe Bronchus (Figure 2). The biopsy result demonstrates squamous-cell carcinoma.
Figure 1.

Computed tomography (CT) shows a mass in the left hilum.
Figure 2.
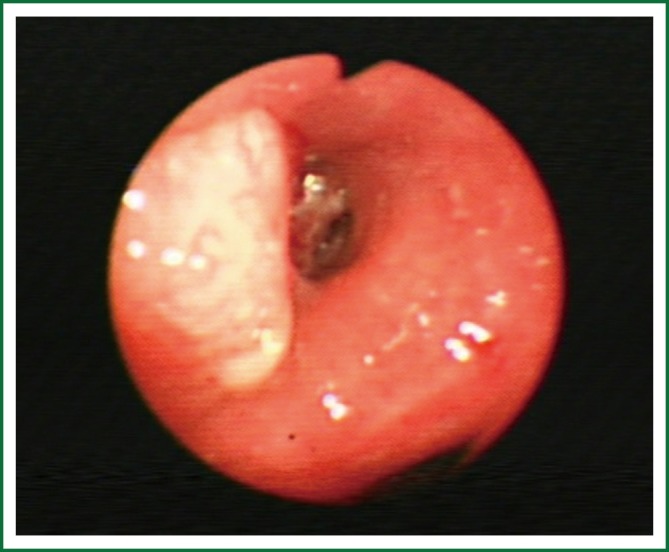
Bronchoscope examination shows a neoplasm in the orifice of Left Upper Lobe Bronchus.
Incision selection
According to our practice, we choose the same incisions as the VATS lobectomy: 2.0-cm-long incision at the 8th intercostal space of the midaxillary line as observing hole; 3-4 cm incision of the 4th (for the low lobe we commonly chose the 5th) intercostal space of the middle axillary line; 1-cm incision in the auscultatory triangle.
Operative technique
Approach
The procedure is generally mirrors that of open surgery: releasing of inferior pulmonary ligament is recommended to bring enough mobility, dissection begins at anterior wall of the hilum, followed by the mobilization and transection of the left superior pulmonary vein, then open the fissure to mobilization and transection of the pulmonary artery and it’s lobar branches. Once the distal and proximal part of pulmonary artery is blocked, the pulmonary artery arterioplasty should be done promptly, finally is the bronchial resection, frozen histological evaluation and anastomosis.
Suture selection
Although both absorbable and prolene suture are applied in this procedure, we prefer to use the 3-0 absorbable sutures to avoidance of foreign body left. And 3-0 prolene suture is applied in the pulmonary artery arterioplasty.
Anastomosis
We perform the anastomosis in a running technique reinforce with three point interrupted suturing. We chose the mind point of offside wall of bronchus as the starting point in interrupted fashion. Once the starting point is located, a U-shape suturing technique is applied to enhance the tensile strength. Absorbable 3-0 sutures, with knots placed outside the bronchial lumen, are used to decrease the possibility of stricture and granuloma formation. Then followed by the continuous suturing clockwise and counter clockwise for one third of the circumference. Another two points of interrupted suturing is followed when the continuous suturing is finished. The final step is to anastomosis the remaining one third of the bronchus circumference in uninterrupted fashion. This anastomosis method can secure the tensile strength as well as saving the operation time. Besides, according to our practice, patient enjoys the comparable post-operation outcomes compared with interrupted suturing.
Operative data and hospital course
Thoracoscopic operation time: 175 min;
The intraoperative bleeding volume: 320 mL;
No intraoperative complications;
ICU stay: 1 day;
Postoperative pathology result shows: 22 lymph nodes removed were all negative for carcinoma.
Comments
In last decades, the minimally invasive surgery prevailed in the thoracic surgery and more patients are willing to take the minimally invasive surgery rather than open surgery if indication qualified. These technically break though greatly propel the development of thoracic surgery and almost every procedure done in open way could be done in VATS fashion either.
When compare to the open surgery, the VATS procedure is generally more technically challenging for the transmission from direct-view to locally 2D screen, from multi-angle multi-direction operation field to one directional operation field. So demands much more clear anatomical view of travel, distribution and variation of pulmonary vessels than open surgery.
Like all other procedures, VATS sleeve lobectomy has its’ nature learning curve for both the surgeon and the assistant. According to my own experience, at least 200 cases VATS lobectomy and 30 cases open sleeve procedures should be done, as to lay the anatomical as well as operative technique foundation, before you can perform the double sleeve procedure.
In this video we perform a unique anastomosis fashion that anastomosis in a running technique reinforce with interrupted suturing: that is every 120 degree of the 360 degree of the bronchus circumference reinforce with the U-shape interrupted suturing technique and finish the anastomosis with continuous between the three points. Such technique is believed to reduce the anastomosis stimulus and sputum retention.
Finally, Blocked view as well as narrow operation space set obstacles for offside of bronchus anastomosis. Under the guidance of “from difficult to easy” principal, we choose the farthest point from surgeon, mid-point of offside of bronchus, as the starting point. Once the first point is settled, the rest anastomosis is easier than the traditional approach. Hence, this method can lower the difficulty and increase the smoothness of anastomosis as a whole.
Acknowledgements
Thanks for the guidance of Dr, Ara A. Vaporciyan, Section Chief of the Division of Cardiothoracic Surgery, I learn the VATS procedures at The University of Texas MD Anderson Cancer Center from April 2006 to October 2006 in which period I accept the systematic training and master key techniques in those procedures. When returning to China, I began to perform VATS procedures to treat early-stage NSCLC and benign disease patients at our department.
Disclosure: The authors declare no conflict of interest.


