Abstract
Child neglect has been hypothesized to be a risk factor for both obesity and underweight in early childhood, although little research has examined the relation between neglect and body mass index (BMI). The current study examined the relation between neglect and BMI among 185 children (91 with a Child Protective Services [CPS] history of neglect) who were initially seen at ages 4–6 years and who were followed through ages 7–9 years. Neglected and comparison children were found to have similar BMIs, although both groups had BMIs that were significantly greater than Centers for Disease Control and Prevention (CDC) norms for age, gender, and ethnicity. Neglect chronicity did predict lower BMIs but only at ages 8 and 9 years. The current findings suggest that greater examination of moderators is needed to identify the specific contexts in which neglect is related to children’s weight.
Keywords: child neglect, obesity, BMI, weight
Neglect has long been considered a risk factor for being underweight or failure to thrive, as emotional deprivation may affect children’s eating behavior or appetite, whereas physical neglect may lead to caregivers offering inadequate calories (Skuse, 1985). More recently, neglect also has been considered a risk factor for the opposite end of the weight spectrum, as excessive eating may occur amid poor parental supervision or may serve as a way to cope with stress (Whitaker, Phillips, Orzol, & Burdette, 2007). Both weight extremes pose significant risk for children’s development. Being underweight in early childhood may place children at risk for poor cognitive development (Corbett & Drewett, 2004), whereas obesity places children at risk for many problems including high blood pressure, elevated lipid levels, chronic inflammation, type 2 diabetes, and poor self-concept (Ebbeling et al., 2002; Young-Hyman, Schlundt, Herman-Wenderoth, & Bozylinski, 2003). A better understanding of the role of neglect in children’s weight status would be important for directing early intervention efforts among neglected children who may be at risk for weight extremes.
Maternal report of neglectful parenting has been linked to increased obesity among 3-year-olds (Whitaker et al., 2007). Examining older children, Lissau and Sorensen (1994) found those rated by school staff as “dirty and neglected” in their hygiene or as having poor parental support at 9–10 years to have increased obesity in early adulthood. Similarly, a retrospective study found adults who reported experiencing mild neglect in childhood to have elevated body mass indices (BMIs) at age 45 (Thomas, Hypponen, & Power, 2008). In contrast, Olivan (2003) found 2- to 3-year-old boys with histories of physical neglect and emotional abuse to be underweight. Thus, research has found neglected children to be at risk for both weight extremes.
Several limitations exist in our current knowledge of the relation between neglect and weight. First, prior studies indicate that neglected children may be at risk for both underweight and overweight, yet no study has examined both extremes. Second, prior studies have been cross sectional or used only a single follow-up assessment. Longitudinal designs with multiple time points can help identify when differences in weight emerge among neglected children. Early childhood is an important time to examine risk factors for weight extremes as children learn and show individual differences in food preferences and eating styles that may affect eating and weight patterns throughout life (Birch & Fisher, 1998). The time between ages 5 and 7 years may be particularly important in the development of obesity as this is a period of adiposity rebound (Dietz, 1994). Third, prior studies have used only a single source to assess neglect (e.g., parent report) although parent reports of child maltreatment may be biased (Bennett, Sullivan, & Lewis, 2006). Fourth, the chronicity of neglect has not been examined in relation to weight. Given that chronicity of maltreatment is related to worse psychosocial adjustment (Bolger, Patterson, & Kupersmidt, 1998; English, Graham, Litrownik, Everson, & Bangdiwala, 2005), chronicity may also predict weight problems. Finally, child age and gender need to be considered as potential moderators of a relation between neglect and weight. Neglect has been found to affect the hypothalamic–pituitary–adrenal system, which is integral to stress-related eating (Adam & Epel, 2007; Sullivan, Bennett, & Lewis, 2010). Girls and older children have been shown to exhibit more stress-related eating (Ashcroft, Semmler, Carnell, van Jaarsveld, & Wardle, 2008; Greeno & Wing, 1994), raising the possibility that they will show greater weight gain or variability in weight extremes when stressed (Braet & Van Strien, 1997; Roemmich, Wright, & Epstein, 2002). The current study sought to examine whether neglected children are at increased risk for being either underweight or overweight.
Method
Participants
Participants were 185 children (91 neglected), predominately African American (75%), from two age groups in an overlapping panel design. Children from the younger cohort (n = 86; 41 males, 41 neglected; mean age = 4.3 years [SD = 0.4] at enrollment) were assessed annually from 4 to 7 years while those from the older cohort (n = 99; 41 males, 50 neglected; mean age = 6.1 years [SD = 0.4] at enrollment) were assessed annually from 6 to 9 years. Participants were recruited via flyers posted in publicly funded preschool or therapeutic programs and other community agencies (e.g., Women, Infants and Children [WIC] offices) in Philadelphia and central New Jersey. The flyers stated that the study was of development in young children and requested parents to call the research program if they were interested in obtaining more information. Upon calling, parents were told that the study involved comparing the development of neglected and nonneglected children and that they would be asked to sign a consent form permitting the research team to review Child Protective Services (CPS) records for classification of maltreatment status. At the initial study visit, parents signed the Institutional Review Board (IRB) approved study consent form before initiating any study activities. Children with CPS allegations of sexual abuse and children with known histories of mental retardation were excluded from the study.
The number of children in the younger cohort, who had BMIs collected at follow-up visits were 73 at 5 years, 58 at 6 years, and 40 at 7 years. For the older cohort, 87 were seen at 7 years, 72 at 8 years, and 48 at 9 years. The BMIs of children who participated throughout the study and of those who missed visits were not significantly different at any age. Likewise, the BMIs of neglected and comparison children did not significantly differ between cohorts at the common ages of 6–7 years. Thus, BMIs were pooled across cohorts at these two ages to optimize statistical power for subsequent analyses.
Procedure
Mothers completed a brief demographic interview and the Parent–Child Conflict Tactics Scale (CTSPC; Straus et al., 1998) at the research program’s office or the child’s school. Families were paid $40 in gift cards for their participation at the conclusion of each visit.
BMI, weight, and height
BMI scores, percentiles, and z scores for age, gender, and ethnicity were computed for each child using HealthWatch Pro 3.0 software (BV Tech, Inc., Martinez, Georgia) from weight and height data based on CDC age, gender, and ethnicity-specific growth charts (Kuczmarski et al., 2002). Children’s weight was assessed using a Taylor Lithium electronic digital scale (Las Cruces, New Mexico; #205s). Height was assessed using a stadiometer (Seca, Inc., Hamburg, Germany).
CPS neglect status
Given that unsubstantiated CPS allegations have been related to increased risk of child problems (Gracia, 1995), children were included in the neglect group if they had either a substantiated or unsubstantiated allegation of neglect. There were 65 children with substantiated allegations of neglect and 26 with unsubstantiated allegations of neglect. Twelve neglected children also had CPS allegations of physical abuse (four substantiated and eight unsubstantiated).
Chronicity of neglect
The number of months between children’s first and last CPS neglect allegation was computed to assess neglect chronicity (for subjects with only one allegation, the chronicity score was set at 1; comparison children were assigned a score of 0). Among neglected children, chronicity ranged from 1 to 79 months (M = 28.1, SD = 28.3).
CTSPC (Straus et al., 1998)
The CTSPC contains a 5-item Neglect subscale. The CTSPC was administered in Year 1 and Year 2 of the study; mother’s scores, which were correlated across the two time points (r = .48, p < .001), were averaged to provide a composite measure of neglectful parenting. Neglect subscale scores were significantly correlated with children’s CPS neglect status (rpb = .29, p < .001).
Results
Chi-square analyses are presented to examine the differences between groups on demographic variables. Mixed models analyses are then presented to examine the effect of neglect status, age, and gender on anthropometric measures. However, given that any relation between neglect status and BMI might only be observed when examining extreme scores, Chi-square analyses comparing the relation between neglect and both very low (i.e., ≤ 5th percentile) and high (i.e., ≥ 95th percentile) BMIs are reported. The final analysis presents correlations between neglect chronicity and BMI.
Demographic Similarity of Groups
Neglected and comparison children did not vary on age, gender, or maternal employment but did on ethnicity (Neglect Group: 88% African American, 6% Hispanic, and 6% Other; Comparison Group: 65% African American, 22% Hispanic, and 13% Other; χ2(3) = 17.03, p < .001) and whether mothers received public assistance (80% of Neglected vs. 65% of Comparisons; χ2(1) = 4.99, p < .05).
BMI as a Function of Neglect
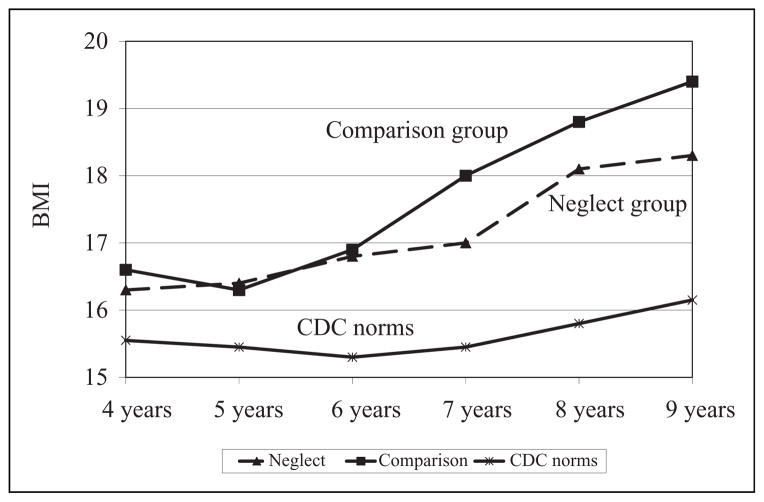
Figure 1 presents the BMI data for the Neglect and Comparison groups over time. Mixed models analyses with random effects specified for the intercept and for the age coefficient were conducted, with neglect status (Neglect vs. Comparison group), gender (male/female), and public assistance status (received/did not receive) entered as predictors (see Table 1). Interactions between neglect and both gender and age also were included. Although the Neglect group had lower BMI scores than the Comparison group, these differences were not significant. As expected, BMI increased with age (coefficient = .35, SE = 0.09; CI = 0.17–0.53, p < .001), consistent with age trends observed in the CDC norms during this period (see Figure 1). Neglect did not interact with gender or with age to predict BMI. Although our focus was on BMI, parallel mix models analyses were conducted for weight and for height; neglect status did not predict either weight or height. Maternal ratings of neglect on the CTSPC also were consistent with the mixed models analyses for BMI, as correlations (and partial correlations controlling for public assistance status) showed no significant relation between neglect and BMI.
Figure 1.
Body mass index (BMI) as a function of neglect status and age.
Table 1.
Coefficients (and Standard Errors; Followed by 95% Confidence Intervals) From Mixed Model Analysis Predicting Body Mass Index (BMI)
| BMI | |
|---|---|
| Intercept | 15.95 (0.40; 15.17 to 16.73) |
| Neglect (0 = control, 1 = neglected) | 0.22 (0.40; −0.58 to 1.02) |
| Age | 0.35 (0.09; 0.17 to 0.53)* |
| Gender | 0.25 (0.42; −0.58 to 1.09) |
| Public assistance (0 = none; 1 = received) | −0.04 (0.35; −0.74 to 0.66) |
| Neglect × age | 0.14 (0.13; −0.13 to 0.40) |
| Neglect × gender | −0.38 (0.60; −1.56 to 0.80) |
p < .001.
As shown in Figure 1, Neglected children did have greater BMIs relative to CDC norms (i.e., from a standardized z score of 0.00) for age, gender, and ethnicity at each age (t scores ranged from t(24) = 2.76, p ≤ .01, at 9 years to t(67) = 4.91, p ≤ .001, at 6 years). The Comparison group, however, also had greater BMIs relative to CDC norms at each age (t scores ranged from t(22) = 3.10, p ≤ .01, to t(73) = 6.31, p ≤ .001). Thus, children in both the Neglect and Comparison groups had higher BMIs than would be expected based on gender, ethnicity, and age norms.
Neglect and Extreme BMIs
Examining low BMIs, no significant differences were found as low BMIs occurred at similar prevalence rates across the two groups. The percentage of children with a low BMI during at least one assessment was 4.4% for the Neglect group and 2.1% for the Comparison group. Examining high BMIs, neglected children were at lower risk of a high BMI only at 8 years (χ2(1) = 4.20, p ≤.05). The percentage of children with a high BMI during at least one assessment was 24.2% for the Neglect group and 25.5% for the Comparison group.
Chronicity of Neglect and BMI
Chronicity predicted lower BMIs at 8 (r(73) = −.24, p ≤.05) and 9 years (r(50) = −.24, p ≤ .10) but was unrelated to BMI at earlier ages.
Discussion
The current findings indicate that neglected children in a predominantly urban, African American sample are not at increased risk of being underweight or overweight relative to comparison children. Children in both groups, however, had high BMIs relative to CDC norms, consistent with research indicating that urban American youth are at elevated risk for obesity (Braunschweig et al., 2005). The lack of evidence for neglect to be associated with underweight is consistent with recent research showing at best a weak relation between neglect and being underweight (Black et al., 2006; Wright & Birks, 2000), although it is possible that the relation between neglect and being underweight occurs primarily in the most severe cases of neglect and among younger children who depend on caregivers for their feeding. Comorbid conditions also need to be considered, as the underweight boys in Olivan’s (2003) sample were not only physically neglected but also emotionally abused for more than 6 months. Such chronicity of maltreatment may also be important to consider as the chronicity of neglect was related to lower BMIs, although only at older ages, in the current study. Neglect chronicity has been associated with lower peer popularity, which in turn has been related to both thin and heavy body types among adolescents, suggesting that peer relations may be a potential mediator of a relation between neglect chronicity and weight as children enter late childhood (Bolger et al., 1998; Wang, Houshyar, & Prinstein, 2006).
The current findings contrast those of two prior studies that found neglect to be a risk factor of obesity. Lissau and Sorensen (1994) found Danish children who were not neglected to have low rates of obesity both in childhood and in early adulthood. It is likely, however, that their Danish subjects were not exposed to the extensive risk factors of obesity experienced by children currently living in American urban environments, especially since their subjects were first seen in 1974. The low obesity rate of their nonneglected subjects suggests that neglect may contribute to obesity risk only when children are not already living in an obesogenic environment. Whitaker and colleagues (Whitaker et al., 2007), however, did study children residing in contemporary urban America and found neglect, as rated by mothers, to be concurrently associated with increased obesity at age 3 years. It would be interesting to examine whether the obesity rates of the nonneglected children in their sample caught up to those of the neglected children at older ages, as it is possible that neglectful parents may be more likely to allow their children free reign of the refrigerator in toddler-hood, leading to the higher rates of obesity among neglected children in their sample.
Several limitations deserve mention. First, although we followed children between the ages of 4 and 9 years, it will be important to assess neglected children’s BMI later in childhood and adolescence. Lissau and Sorensen (1994), for example, failed to find an association between neglect and obesity at ages 9–10 years but did find neglect to predict increased obesity in early adulthood. Second, the current study did not examine specific neglect subtypes. It is possible, for example, that physical neglect is more strongly related to undernourishment, whereas supervisory or emotional neglect may be more strongly related to obesity. Third, larger samples are needed to examine whether a history of physical abuse alters risk for weight problems among neglected children. Fourth, neglect and the chronicity of neglect pose assessment challenges. We assessed chronicity as the length of time between the initial and most recent CPS neglect allegation, similar to other studies (e.g., Bolger et al., 1998), but chronicity is a complex construct and alternative measures of chronicity should be considered (English et al., 2005). Finally, the current results may not generalize beyond a predominantly African American sample residing in urban American settings.
In summary, the current study is the first to examine neglect as a possible antecedent of both under- and over-weight prospectively from early to middle childhood. The current findings call for greater examination of moderators to identify the specific contexts in which neglect is related to children’s weight. Further study is needed to examine whether neglected children residing in other environments, with particular types of neglect and of other ethnicities are at greater risk of obesity than their peers. In addition to examining such potential moderators of the possible relation between neglect and obesity, research is needed to better understand the processes by which some neglected children become at risk for obesity and whether these processes are distinct from those that place nonneglected children at risk for obesity.
Acknowledgments
The authors gratefully acknowledge the assistance of the Philadelphia Department of Human Services and the New Jersey Division of Youth and Family Services.
Funding
The authors disclosed receipt of the following financial support for the research and/or authorship of this article: This study was supported by Grant DA11153/MH56751 to Michael Lewis from the National Institute of Mental Health and the National Institute on Drug Abuse, and by Grant MH64473 to Michael Lewis from the National Institute of Mental Health.
Footnotes
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Reprints and permission: sagepub.com/journalsPermissions.nav
References
- Adam TC, Epel ES. Stress, eating and the reward system. Physiology & Behavior. 2007;91:449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Ashcroft J, Semmler C, Carnell S, van Jaarsveld CHM, Wardle J. Continuity and stability of eating behavior traits in children. European Journal of Clinical Nutrition. 2008;62:985–990. doi: 10.1038/sj.ejcn.1602855. [DOI] [PubMed] [Google Scholar]
- Bennett DS, Sullivan MW, Lewis M. Relations of parental report and observation of parenting to maltreatment history. Child Maltreatment. 2006;11:63–75. doi: 10.1177/1077559505283589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- Black MM, Dubowitz H, Casey PH, Cutts D, Drewett RF, Drotar D, et al. Failure to thrive as distinct from child neglect. Pediatrics. 2006;117:1456–1458. doi: 10.1542/peds.2005-3043. [DOI] [PubMed] [Google Scholar]
- Bolger KE, Patterson CJ, Kupersmidt JB. Peer relationships and self-esteem among children who have been maltreated. Child Development. 1998;69:1171–1197. [PubMed] [Google Scholar]
- Braet C, Van Strien T. Assessment of emotional, externally induced and restrained eating behavior in nine to twelve-year-old obese and non-obese children. Behaviour Research and Therapy. 1997;35:863–873. doi: 10.1016/s0005-7967(97)00045-4. [DOI] [PubMed] [Google Scholar]
- Braunschweig CL, Gomez S, Liang H, Tomey K, Doerfler B, Wang Y, et al. Obesity and risk factors for the metabolic syndrome among low-income, urban, African American schoolchildren: The rule rather than the exception? American Journal of Clinical Nutrition. 2005;81:970–975. doi: 10.1093/ajcn/81.5.970. [DOI] [PubMed] [Google Scholar]
- Corbett SS, Drewett RF. To what extent is failure to thrive in infancy associated with poorer cognitive development? A review and meta-analysis. Journal of Child Psychology and Psychiatry. 2004;45:641–654. doi: 10.1111/j.1469-7610.2004.00253.x. [DOI] [PubMed] [Google Scholar]
- Dietz WH. Critical periods in childhood for the development of obesity. American Journal of Clinical Nutrition. 1994;59:955–999. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. The Lancet. 2002;360:473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- English DJ, Graham JC, Litrownik AJ, Everson M, Bangdiwala SI. Defining maltreatment chronicity: Are there differences in child outcomes? Child Abuse & Neglect. 2005;29:575–595. doi: 10.1016/j.chiabu.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Gracia E. Visible but unreported: A case for the “not serious enough” cases of child maltreatment. Child Abuse & Neglect. 1995;19:1083–1093. doi: 10.1016/0145-2134(95)00070-o. [DOI] [PubMed] [Google Scholar]
- Greeno CG, Wing RR. Stress-induced eating. Psychological Bulletin. 1994;115:444–464. doi: 10.1037/0033-2909.115.3.444. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. CDC growth charts for the United States: Methods and development. Vital and Health Statistics. 2002;11:1–190. [PubMed] [Google Scholar]
- Lissau I, Sorensen TIA. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet. 1994;343:324–327. doi: 10.1016/S0140-6736(94)91163-0. [DOI] [PubMed] [Google Scholar]
- Olivan G. Catch-up growth assessment in long-term physically neglected and emotionally abused pre-school age male children. Child Abuse & Neglect. 2003;27:103–108. doi: 10.1016/s0145-2134(02)00513-6. [DOI] [PubMed] [Google Scholar]
- Roemmich JN, Wright SM, Epstein LH. Dietary restraint and stress-induced snacking in youth. Obesity Research. 2002;10:1120–1126. doi: 10.1038/oby.2002.152. [DOI] [PubMed] [Google Scholar]
- Skuse DH. Non-organic failure to thrive: A reappraisal. Archives of Disease in Childhood. 1985;60:173–178. doi: 10.1136/adc.60.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect. 1998;22:249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Sullivan MW, Bennett DS, Lewis M. Individual differences in the stress hormone responses of neglected children. 2010 doi: 10.1177/1077559512449378. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas C, Hypponen E, Power C. Obesity and Type 2 diabetes risk in midadult life: The role of childhood adversity. Pediatrics. 2008;121:e1240–e1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- Wang SS, Houshyar S, Prinstein MJ. Adolescent girls’ and boys’ weight-related health behaviors and cognitions: Associations with reputation- and preference-based peer status. Health Psychology. 2006;25:658–663. doi: 10.1037/0278-6133.25.5.658. [DOI] [PubMed] [Google Scholar]
- Whitaker RC, Phillips SM, Orzol SM, Burdette HL. The association between maltreatment and obesity among preschool children. Child Abuse & Neglect. 2007;31:1187–1199. doi: 10.1016/j.chiabu.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright C, Birks E. Risk factors for failure to thrive: A population-based survey. Child: Care, Health, and Development. 2000;26:5–16. doi: 10.1046/j.1365-2214.2000.00135.x. [DOI] [PubMed] [Google Scholar]
- Young-Hyman D, Schlundt DG, Herman-Wenderoth L, Bozylinski K. Obesity, appearance, and psychosocial adaptation in young African American children. Journal of Pediatric Psychology. 2003;28:463–472. doi: 10.1093/jpepsy/jsg037. [DOI] [PubMed] [Google Scholar]