Abstract
Experimental sleep restriction increases sleepiness and impairs driving performance. However, it is unclear whether short sleep duration in the general population is associated with drowsy driving. The goal of the present study was to evaluate whether individuals in the general population who obtained sleep of 6 hours or less are more likely to report drowsy driving, and evaluate the role of perceived sleep sufficiency. Data exploring whether subgroups of short sleepers (those who report the most or least unmet sleep need) show different risk profiles for drowsy driving are limited. From the 2009 Behavioral Risk Factor Surveillance System (N=31,522), we obtained the following self-reported data: 1) sleep duration (≤5, 6, 7, 8, 9, or ≥10h/night); 2) number of days/week of perceived insufficient sleep; 3) among drivers, yes/no response to: “During the past 30 days, have you ever nodded off or fallen asleep, even just for a brief moment, while driving?” 4) demographics, physical/mental health. Using 7h/night as reference, logistic regression analyses evaluated whether self-reported sleep duration was associated with drowsy driving. Overall, 3.6% reported drowsy driving. Self-identified short-sleepers reported drowsy driving more often, and long sleepers, less often. Among those who perceived sleep as always insufficient, drowsy driving was reported more often when sleep duration was ≤5h, 6h, or ≥10h. Among those who perceived sleep as always sufficient, drowsy driving was reported more often among ≤5h and 6h sleepers. Overall, drowsy driving was common, particularly in self-identified short-sleepers as a whole, as well as subgroups based on sleep insufficiency.
Keywords: Sleep, driving, accidents, sleep duration, insufficient sleep, epidemiology
INTRODUCTION
Crashes related to drowsy driving may be more likely to result in injury or death, since they are not typically preceded by avoidance maneuvers, such as braking or swerving(Strohl et al. 1998, NHTSA 2011). While estimating the number of accidents due to drowsy driving is methodologically difficult, federal data suggest that approximately 15–33% of fatal crashes may be due to drowsy driving. Results from the National Sleep Foundation's “Sleep in America” poll estimated that more than half of drivers admitted to drowsy driving and 17% reported falling asleep at the wheel within the past year(Drobnich 2005, Powell and Chau 2011), and the Centers for Disease Control and Prevention found that >4% of drivers reported driving while drowsy in the previous month(McKnight-Eily et al. 2011).
A number of investigations have linked insufficient sleep with impaired driving ability. In a study of simulated driving performance in shift workers with and without a full night's sleep, prior sleep loss coincided with increased sleepiness levels at the wheel (operationally defined as an increase in eye closure duration and lateral variability)(Anund et al. 2009). Another study, which restricted an experimental group to 5h of sleep, found that, overall, sleep deprivation resulted in driving impairment (through lane shifting events) and, furthermore, younger men were more vulnerable to this effect(Filtness et al. 2012). An increase in break reaction time after a night of insufficient sleep has also been indicated through simulated driving studies(Miyata et al. 2010).
These studies are limited by their ability to effectively measure real-life driving scenarios. Some studies have examined less precise but more ecologically valid measures. For example, night-time driving, which coincided with an increase in sleepiness, was found to be associated with an increase in lateral variability and reduced speed while driving (Sandberg et al. 2011). In a review of California Department of Motor Vehicles driving records and reports, one study found that short sleepers are not at a higher risk for accidents or other violations (Kripke and Rex 2002). This study is strengthened by its use of objective events as outcome and objective sleep measures, but is limited by potential underreporting of single-car accidents, near-misses, and other problems that may be associated with drowsy driving.
One of the key questions that remain to be addressed is whether the association between sleep and driving generalizes to the population level, beyond small studies of restricted cohorts. Also, since many studies examined driving impairment as a result of forced sleep deprivation under experimental conditions, questions remain regarding the effects of habitual short sleep on driving quality. Accordingly, the present study examined the 2009 Behavioral Risk Factor Surveillance System national survey to determine: (1) whether short-sleepers (6h or less) were more likely to report drowsy driving than average-duration sleepers and, (2) if perception of insufficient sleep (as either always sufficient or always insufficient) modified the self-reporting of drowsy driving and/or this association. These analyses were carried out using a large, highly generalizable sample (with weighted data representing ~21 million American adults from 6 states).
METHODS
Data Source
Data from the 2009 Behavioral Risk Factor Surveillance System (BRFSS) were used (Centers for Disease Control 2009b). The BRFSS is an annual, state-based, random-digit-dialed telephone interview survey of United States adults aged ≥18 years. It is conducted by the Centers for Disease Control and Prevention and it is designed to monitor health-related behaviors in the general population. Since not all states are administered all questions, we restricted analyses to states that were asked both sleep and driving survey items. These included 6 states, representing states from the West (Hawaii and Wyoming), South (Georgia and Louisiana), and Midwest (Illinois and Minnesota); no states from the Northeast provided data. Response rates ranged from 45.6% (Hawaii) to 59.7% (Minnesota), and cooperation rates ranged from 68.9% (Hawaii) to 83.9% (Georgia)(Centers for Disease Control 2009a). All analyses are adjusted to remove bias in the sample. To do this, BRFSS assigns a weight to each participant to account for differences in selection probability, lack of coverage or response, number of residential telephone lines in the home of each participant, and number of adults in the household. This increases generalizability of results by accounting for factors of location and accessibility, and characteristics such as age, sex, and ethnicity. A more detailed description can be located within BRFSS documentation (Centers for Disease Control 2009a).
Measures
Drowsy Driving
Drowsy driving was assessed using the item, “During the past 30 days, have you ever nodded off or fallen asleep, even just for a brief moment, while driving?” Responses were coded as Yes or No. Those who did not answer, did not have a license, or do not drive were excluded.
Sleep Duration
Self-reported habitual sleep duration was assessed using the question, “On average, how many hours of sleep do you get in a twenty-four hour period? Think about the time you actually spend sleeping or napping, not just the amount of sleep you think you should get.” Hours of sleep were entered in whole numbers. Responses were categorized as <5, 5– 7 [reference], 8– and ≥10h.
Insufficient Sleep
Perceived sleep insufficiency was assessed using the question, “During the past thirty days, for about how many days have you felt you did not get enough rest or sleep?” Responses were transformed to number of days per week (by dividing by 4.285) for improved clarity in interpretation, with 0 days/week defined as “always sufficient” and 7 days/week defined as “always insufficient”.
Covariates
Covariates included in analyses were age, sex, race/ethnicity (White, Black/African-American, Hispanic/Latino, Asian/Other, Multiracial), education (less than high school, high school graduate, some college, college graduate), and income (<$10,000, $10,000–$15,000, $15,000–$20,000, $20,000–$25,000, $25,000–$35,000, $35,000–$50,000, $50,000–$75,000, and ≥$75,000). Physical health was assessed as days of poor physical health in the past 30 days, and mental health was assessed as days of poor mental health in the past 30 days. These variables were chosen a priori, as previous studies have found that these variables were related to sleep(Buxton and Marcelli 2010, Grandner et al. 2010a).
Statistical Analyses
Complete case analysis was implemented for both sleep duration and sleep insufficiency, such that only participants who provided complete data were included for each analysis. Categorical variables were expressed as percentages while continuous variables were expressed in terms of mean (±SD). To assess unadjusted associations between each dependent variable and all covariates, Rao-Scott Chi-square and binary logistic regression were used. For the dependent outcome (drowsy driving), two separate models were subsequently built as follows; 1) sleep duration alone; 2) sleep duration plus covariates. This was conducted for the entire sample, as well as separately for those reporting 0 and 7 nights/ week of sleep insufficiency.
This large sample of >30,000 individuals represents a population of ~21 million. As a result, we have the power to detect significance for relatively small effect sizes.
We considered a two-tailed P-value of <0.05 as significant. All statistical calculations were performed using STATA/SE version 11.1 (STATA Corp, College Station TX).
RESULTS
Sample Characteristics
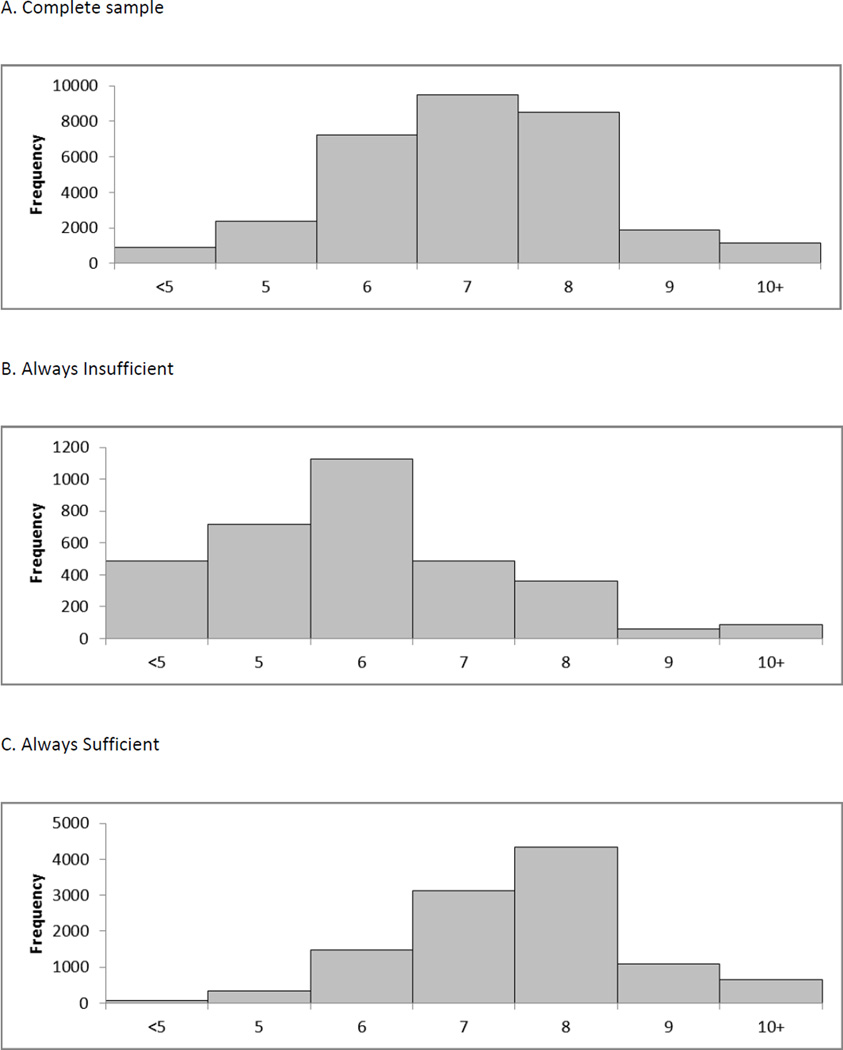
Characteristics of the sample are reported in Table 1. All cases were weighted, resulting in a sample that was nationally-representative. Sleep duration categories were, however, differentially distributed across sociodemographic, socioeconomic, and health variables, justifying their inclusion as covariates. Overall, from a sample N=31,522, 3.6% (N=1,197) reported drowsy driving. Of the total sample, 10.9% reported sleep as always insufficient, and 29.1% as always sufficient. A total of 8.5% that reported sleep duration ≥10h reported that sleep was always insufficient. Frequency distributions of sleep duration in the complete study sample, as well as sub-groups that report always insufficient and always sufficient sleep are displayed in Figure 1.
Table 1.
Characteristics of the Sample, Stratified by Sleep Duration Category
| Variable | Description | Overall Sample | Stratification by Sleep Duration Groups | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤5 Hours | 6 Hours | 7 Hours | 8 Hours | 9 Hours | ≥10 Hours | p | |||
| Age | Mean ± SD | 46.047 ± 17.336 | 46.081 ± 16.223 | 44.016 ± 15.854 | 44.484 ± 15.271 | 48.444 ± 19.148 | 45.385 ± 20.694 | 46.762 ± 23.311 | <0.0001 |
| Sex | Female | 51.478% | 49.332% | 52.048% | 49.472% | 54.609% | 56.468% | 51.182% | 0.0006 |
| Race/Ethnicity | Non-Hispanic White | 68.214% | 74.581% | 55.899% | 66.561% | 70.125% | 66.026% | 53.615% | <0.0001 |
| Black/African-American | 16.080% | 11.216% | 25.458% | 17.803% | 14.781% | 14.922% | 27.761% | ||
| Hispanic/Latino | 7.041% | 5.934% | 7.746% | 6.802% | 7.358% | 9.082% | 10.154% | ||
| Asian/Other | 6.586% | 6.631% | 7.104% | 6.602% | 6.357% | 7.119% | 5.285% | ||
| Multiracial | 2.079% | 1.639% | 3.793% | 2.231% | 1.378% | 2.851% | 3.185% | ||
| Education | Less Than High School | 7.552% | 4.951% | 11.257% | 5.864% | 8.847% | 8.521% | 18.646% | <0.0001 |
| High School | 27.381% | 22.897% | 32.372% | 26.934% | 28.414% | 31.481% | 38.721% | ||
| Some College | 27.924% | 27.256% | 30.198% | 30.372% | 25.674% | 28.899% | 24.368% | ||
| College Graduate | 37.143% | 44.897% | 26.173% | 36.830% | 37.065% | 31.099% | 18.265% | ||
| Income | <$10,000 | 3.831% | 2.084% | 8.714% | 3.199% | 3.403% | 4.045% | 10.894% | <0.0001 |
| $10,000–$15,000 | 4.010% | 2.011% | 6.045% | 4.057% | 4.452% | 5.937% | 8.366% | ||
| $15,000–$20,000 | 6.300% | 4.720% | 8.438% | 6.750% | 6.024% | 4.578% | 15.187% | ||
| $20,000–$25,000 | 8.325% | 6.843% | 9.583% | 7.592% | 9.133% | 10.985% | 12.292% | ||
| $25,000–$35,000 | 10.039% | 7.997% | 12.691% | 9.654% | 10.596% | 14.306% | 11.017% | ||
| $35,000–$50,000 | 14.457% | 14.819% | 13.094% | 14.894% | 14.720% | 14.124% | 11.155% | ||
| $50,000–$75,000 | 17.227% | 18.636% | 15.653% | 17.127% | 17.613% | 15.232% | 11.125% | ||
| >$75,000 | 35.812% | 42.890% | 25.783% | 36.726% | 34.059% | 30.794% | 19.964% | ||
| Physical Health | Mean ± SD | 59.902 ± 38.078 | 62.415 ± 37.309 | 53.083 ± 37.979 | 57.488 ± 37.502 | 62.885 ± 38.605 | 60.576 ± 37.736 | 53.864 ± 39.736 | <0.0001 |
| Mental Health | Mean ± SD | 62.325 ± 37.205 | 65.378 ± 36.048 | 53.708 ± 37.393 | 58.614 ± 36.796 | 66.802 ± 36.974 | 60.479 ± 38.604 | 59.580 ± 39.053 | <0.0001 |
| Fell Asleep Driving | 3.573% | 2.434% | 8.693% | 4.762% | 2.242% | 1.374% | 2.969% | <0.0001 | |
| 7 Days/Week Insufficient Sleep | 10.878% | 5.028% | 36.589% | 15.618% | 4.570% | 2.537% | 8.501% | <0.0001 | |
| 0 Days/Week Insufficient Sleep | 29.072% | 27.465% | 8.960% | 15.399% | 45.543% | 50.550% | 44.298% | <0.0001 | |
Figure 1.
Frequency distributions of sleep duration in the study sample.
Drowsy Driving and Sleep Duration
Table 2 shows the logistic regression results for falling asleep at the wheel as associated with sleep duration for the complete sample. Both before and after adjustment for covariates, short duration sleepers (6h or less) were more likely to report drowsy driving. The unadjusted data shows that very short sleepers (≤ 5h) were 3.8 times as likely to report drowsy driving (OR = 3.816, p<.0001), and that short sleepers (6h) were twice as likely to report drowsy driving (OR = 2.004, p <.0001). After adjustment for covariates, the increase in reported drowsy driving in short sleepers became slightly less pronounced for ≤ 5h: OR = (3.573, p < .001), and for 6h: (OR = 1.894, p < .0001). After adjustment, the 9-hour sleepers showed a decreased likelihood to report drowsy driving (OR = 0.329, p =0.0057).
Table 2.
Unadjusted and Adjusted Logistic Regression Results for Falling Asleep At The Wheel Associated with Sleep Duration for the Complete Sample, Those Reporting 7 Days/Week Insufficient Sleep (“Always Insufficient”), and Those Reporting 0 Days/Week Insufficient Sleep (“Sufficient”)
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Sleep Duration | OR (95% CI) | p | OR (95% CI) | p |
| Complete Sample | ||||
| ≤5 Hours | 3.816 (2.829, 5.146) | <0.0001 | 3.573 (2.593, 4.924) | <0.0001 |
| 6 Hours | 2.004 (1.511, 2.658) | <0.0001 | 1.894 (1.408, 2.548) | <0.0001 |
| 7 Hours | Reference | Reference | ||
| 8 Hours | 0.919 (0.619, 1.364) | 0.6753 | 1.013 (0.669, 1.535) | 0.9508 |
| 9 Hours | 0.558 (0.227, 1.371) | 0.2035 | 0.329 (0.149, 0.724) | 0.0057 |
| ≥10 Hours | 1.226 (0.528, 2.846) | 0.6351 | 1.353 (0.580, 3.153) | 0.4841 |
| 7 Days/Week Insufficient Sleep (Always Insufficient) | ||||
| ≤5 Hours | 4.839 (2.487, 9.415) | <0.0001 | 4.376 (1.967, 9.738) | 0.0003 |
| 6 Hours | 3.347 (1.608, 6.969) | 0.0012 | 3.270 (1.375, 7.776) | 0.0073 |
| 7 Hours | Reference | Reference | ||
| 8 Hours | 1.018 (0.305, 3.395) | 0.9765 | 0.955 (0.248, 3.675) | 0.9467 |
| 9 Hours | 4.693 (0.639, 34.447) | 0.1285 | 5.279 (0.730, 38.193) | 0.0994 |
| ≥10 Hours | 5.670 (1.754, 18.330) | 0.0037 | 5.514 (1.563, 19.450) | 0.0079 |
| 0 Days/Week Insufficient Sleep (Always Sufficient) | ||||
| ≤5 Hours | 2.814 (1.313, 6.029) | 0.0078 | 2.589 (1.121, 5.976) | 0.0259 |
| 6 Hours | 2.597 (1.246, 5.416) | 0.0109 | 2.955 (1.344, 6.495) | 0.0070 |
| 7 Hours | Reference | Reference | ||
| 8 Hours | 1.119 (0.657, 1.906) | 0.6782 | 1.139 (0.633, 2.048) | 0.6643 |
| 9 Hours | 0.396 (0.096, 1.643) | 0.2022 | 0.467 (0.109, 2.000) | 0.3048 |
| ≥10 Hours | 0.393 (0.117, 1.326) | 0.1324 | 0.469 (0.137, 1.609) | 0.2286 |
Drowsy Driving and Perceived Sleep Insufficiency
Table 2 also shows the logistic regression results for drowsy driving and sleep duration for those who reported 7 days/week of insufficient sleep (always insufficient) and 0 days/week of insufficient sleep (always sufficient). Among those who reported sleep that was always insufficient, there was an increased probability of self-reported drowsy-driving in both very short sleepers (≤5h) and short sleepers (6h) when compared to 7 hour sleepers. Long sleepers (≥10h) that also rated their sleep as always insufficient were also more likely to report drowsy driving. After adjustment for covariates, the relationship remained for ≤ 5h, 6h and ≥10h. For those who reported 0 days/week of insufficient sleep (always sufficient), very short and short-sleeper subgroups were again more likely to report drowsy driving both before and after adjustment.
DISCUSSION
We found that “very short” and “short” sleep durations, defined as ≤5 and 6h, respectively, were associated with drowsy driving in main and adjusted analyses. Very short sleepers were 3.6–3.8 times more likely to report drowsy driving than 7-hour sleepers, and short sleepers were 1.9–2.0 times more likely. Members of these sleep duration categories rated themselves as having always sufficient or always insufficient sleep, defined as number of days of perceived insufficient sleep in the past 30 days. The main finding, that short sleep duration is associated with drowsy driving, was independent of perceived sufficiency. Said another way, short sleepers and very short sleepers experienced drowsy driving, regardless of whether or not they rated their sleep as always sufficient – this relationship persisted even in cases where subjects reported no insufficient sleep at all in the past month. The second key finding was that a subgroup of long sleepers (≥10h) who also experienced sleep quality as “always insufficient” also had increased risk of drowsy driving.
Our findings are consistent with previously-reported data(Van Dongen et al. 2004) regarding self-rated sleepiness in response to acute and chronic sleep deprivation. While subjects are able to perceive sleepiness in conditions of acute sleep deprivation, such ability reaches a plateau during sustained periods of chronic sleep insufficiency, and the ability to perceive performance deficits becomes impaired. On the other hand, objective assessments continue to show cumulative deficits in neurocognitive performance under conditions of chronic sleep deprivation. One such measure is the psychomotor vigilance test (PVT)(Rupp et al. 2004, Lim and Dinges 2008, 2010), which measures vigilance and response time, both of which are critical during on-the-road driving performance. These data suggest that short or very short self-reported sleep duration is a robust predictor of drowsy driving, rather than the self-rating of sleep as always sufficient or always insufficient.
In contrast, long sleepers (≥10h) were at increased risk for drowsy driving only if they perceived their sleep as always insufficient. As suggested previously(Grandner and Patel 2009, Grandner et al. 2010b), this group is also at higher risk for all-cause mortality. One prevailing hypothesis is that the combination of long sleep duration and perception of insufficient sleep may mark those with comorbid sleep disorders such as obstructive sleep apnea (OSA). OSA is common in the general population; prevalence estimates from 1993 suggest that OSA afflicts 4% of men and 2% of women (Young et al. 1993). This prevalence has likely risen, given the link between OSA and obesity, though more recent population prevalence data are not currently available. Despite adequate or even long sleep duration, patients with OSA may report daytime sleepiness and suffer increased risk of sleepiness-related vehicular crashes, at a rate of 1.21–4.89 compared to controls without sleep apnea(Tregear et al. 2009). Treatment of sleep apnea in these individuals has been shown to lower crash risk to baseline levels(Tregear et al. 2010). Therefore, our studies may be marking an important subgroup that deserves formal sleep evaluation to assess for sleep disorders.
Limitations
This study incorporated survey data from a large, population-based sample which represented a population of ~21 million. While the large sample size enhanced our ability to detect small effect sizes, and the use of a population-based cohort enhances generalizability of the results, several limitations in study design should be mentioned. The assessment of sleep duration, frequency of perceived insufficient sleep, and drowsy driving were made at a single time point, which limits causal inference. Moreover, our assessments were subjective, raising the possibility of misclassification and possible under-reporting of drowsy driving. Our findings would be strengthened by linking these self-reports with objective data, such as actigraphy, vigilance testing, assessments of driving performance on the road or via simulators, and crash records.
Highlights.
Overall, more drowsy driving in short sleepers and less in long sleepers.
With 7 nights/wk insufficient sleep, more drowsy driving in both short and long sleepers.
With 0 nights/wk insufficient sleep, more drowsy driving in short sleepers.
Short sleepers at greater risk of drowsy driving, irrespective of sufficient sleep.
ACKNOWLEDGEMENTS
This study was supported by the National Heart, Lung and Blood Association (K23HL110216), the National Institute of Environmental Health Sciences (R21ES022931), and the Institute for Translational Medicine and Therapeutics, via the Penn CTSA (UL1RR024134), and the National Institute for Occupational Health and Safety/Centers for Disease Control (R01OH009149). We also wish to thank the Centers for Disease Control and Prevention for collecting these data and making them available, and the BRFSS participants.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Anund A, Kecklund G, Kircher A, Tapani A, Akerstedt T. The effects of driving situation on sleepiness indicators after sleep loss: A driving simulator study. Ind Health. 2009;47(4):393–401. doi: 10.2486/indhealth.47.393. [DOI] [PubMed] [Google Scholar]
- Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the united states. Soc Sci Med. 2010;71(5):1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Brfss 2009 data quality report handbook CDC. Washington DC: 2009a. [Google Scholar]
- Centers for Disease Control. Overview: Brfss 2009 CDC. Washington, DC: 2009b. [Google Scholar]
- Drobnich D. A national sleep foundation's conference summary: The national summit to prevent drowsy driving and a new call to action. Ind Health. 2005;43(1):197–200. doi: 10.2486/indhealth.43.197. [DOI] [PubMed] [Google Scholar]
- Filtness AJ, Reyner LA, Horne JA. Driver sleepiness-comparisons between young and older men during a monotonous afternoon simulated drive. Biol Psychol. 2012 doi: 10.1016/j.biopsycho.2012.01.002. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Patel NP. From sleep duration to mortality: Implications of meta-analysis and future directions. J Sleep Res. 2009;18(2):145–147. doi: 10.1111/j.1365-2869.2009.00753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, Gooneratne N. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep disturbance. Sleep Med. 2010a;11:470–479. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Hale L, Moore M. Mortality associated with sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010b;14:191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripke DF, Rex K. Short sleepers are not at higher risk for driving accidents or other violations. Sleep. 2002;25:A284–A285. (Abstract Supplement) [Google Scholar]
- Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann N Y Acad Sci. 2008;1129:305–322. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- Lim J, Dinges DF. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol Bull. 2010;136(3):375–389. doi: 10.1037/a0018883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcknight-Eily LR, Liu Y, Wheaton AG, Croft JB, Perry GS, Okoro CA, Strine T. Unhealthy sleep-related behaviors --- 12 states, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(8):233–238. [PubMed] [Google Scholar]
- Miyata S, Noda A, Ozaki N, Hara Y, Minoshima M, Iwamoto K, Takahashi M, Iidaka T, Koike Y. Insufficient sleep impairs driving performance and cognitive function. Neurosci Lett. 2010;469(2):229–233. doi: 10.1016/j.neulet.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Nhtsa. Traffic Safety Facts: Crash Stats. Wahinton, DC: US Department of Transportation; 2011. Drowsy driving. [Google Scholar]
- Powell NB, Chau JKM. Sleepy driving. Sleep Med Clin. 2011;6:117–124. [Google Scholar]
- Rupp T, Arnedt JT, Acebo C, Carskadon MA. Performance on a dual driving simulation and subtraction task following sleep restriction. Percept Mot Skills. 2004;99(3 Pt 1):739–753. doi: 10.2466/pms.99.3.739-753. [DOI] [PubMed] [Google Scholar]
- Sandberg D, Anund A, Fors C, Kecklund G, Karlsson JG, Wahde M, Akerstedt T. The characteristics of sleepiness during real driving at night--a study of driving performance, physiology and subjective experience. Sleep. 2011;34(10):1317–1325. doi: 10.5665/SLEEP.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strohl KP, Blatt J, Council F, Georges K, Kiley J, Kurrus R, Mccartt AT, Merritt SL, Pack AI, Rogus S, Roth T, Stutts J, Waller P, Willis D. Drowsy driving and automobile crashes: Ncsdr/nhtsa expert panel on driver fatigue and sleepiness. Washington, DC: National Highway Traffic Safety Administration; 1998. [Google Scholar]
- Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: Systematic review and meta-analysis. J Clin Sleep Med. 2009;5(6):573–581. [PMC free article] [PubMed] [Google Scholar]
- Tregear S, Reston J, Schoelles K, Phillips B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea: Systematic review and meta-analysis. Sleep. 2010;33(10):1373–1380. doi: 10.1093/sleep/33.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanDongen HP, Baynard MD, Maislin G, Dinges DF. Systematic interindividual differences in neurobehavioral impairment from sleep loss: Evidence of trait-like differential vulnerability. Sleep. 2004;27(3):423–433. [PubMed] [Google Scholar]
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]