Abstract
The DNA-damage response (DDR) plays a crucial role in tumor development in different tissues. Here we show that p53-binding protein 1 (53BP1), a key element of the DDR, is heterozygously lost in approximately 20% of human glioblastoma multiforme (GBM) specimens, primarily of the Proneural subtype, and low 53BP1 expression levels are associated with worse prognosis. We present evidence that 53BP1 behaves as haploinsufficient tumor suppressor in a mouse model of PDGF-induced gliomagenesis. We also show that very low level of 53BP1 as found in 53BP1 null gliomas or robust 53BP1 gene silencing in glioma cell lines (but not 53BP1 heterozygous tumors or partial gene knock-down) sensitizes glioma cells to ionizing radiation (IR), both in vitro and in vivo. We further demonstrate the 53BP1 gene silencing induces defects in the nonhomologous end-joining (NHEJ) DNA repair pathway. These deficiencies lead to a failure to fully repair the damaged DNA upon exposure of glioma cells to IR with a consequent prolonged cell-cycle arrest and increased apoptosis. Our data suggest that either 53BP1 or other NHEJ components may be critical molecules to be pharmacologically-targeted in GBM in combination with standard therapies.
Keywords: 53BP1, DDR, GBM, Ionizing radiation, NHEJ
Introduction
The p53-binding protein 1 (53BP1) was initially identified as a protein that interacts with the DNA-binding domain of wild-type but not mutant p53, having the ability to modulate p53-mediated transcription activation (1, 2). 53BP1 has subsequently been shown to also have p53-independent functions as a key mediator of the DNA damage response (DDR) and a direct modulator of DNA double-strand break (DSB) repair (3). 53BP1-deficient cells exhibit increased genomic instability and consequently 53BP1 null mice are highly radiation sensitive, display growth retardation and are tumor-prone (4, 5).
Even though a critical role of the DDR pathway in tumor formation and modulation of therapeutic response has been established recently, it is unclear whether 53BP1 takes an active part in these processes, and if so in which tumor type. Here we show that 53BP1 is frequently heterozigously lost in glioblastoma multiforme (GBM) and behaves as a haploinsufficient tumor suppressor in a mouse model of glioma. Gliomas are the most frequent primary malignancies in the central nervous system (CNS), with GBM being the most malignant form of gliomas. We have previously demonstrated that some essential components of the DDR, such as ATM, Chk2 and p53, are frequently inactivated in GBM and exert a crucial activity during in glioma development and radiation response (6). Contrasting with its role as a tumor suppressor when partly lost, complete loss of 53BP1 in glioma cells increases radiosensitivity both in vitro and in vivo. We present evidence that the radiation sensitivity might be related to 53BP1’s role in modulating nonhomologous end-joining (NHEJ) DNA repair.
Material and Methods
TCGA analysis
The analysis of the TCGA dataset for GBM was performed through the cBio Cancer Genomics Portal (7), ;based on the 24 January 2012 Broad Firehose run of TCGA data. Copy number alterations, expression and patients survival data are also presented on Table S1 and Table S2.
Mice and generation of murine gliomas
53bp1−/− mice (4) were obtained from Titia de Lange. Athymic Nude-Foxn1nu mice were purchased from Harlan Laboratories. Ntv-a mice, and procedures for RCAS-mediated gliomagenesis have been described previously (8). All animal experiments were done in accordance with protocols approved by the Institutional Animal Care and Use Committee of MSKCC and followed NIH guidelines for animal welfare.
Histology, Immunohistochemistry and TUNEL assay
Tissues were fixed in 10% neutral buffered formalin and subsequently embedded in paraffin, following standard procedures. Immunohistochemical and TUNEL staining was performed using a Discovery XT automated staining processor (Ventana Medical Systems, Inc.). The antibodies were diluted in PBS 2%BSA as follow: anti-53bp1 (Novus, #NB100–304) 1:800 anti-phospho-Histone H3 (Ser10) (Millipore, #06–750) 1:800. The TUNEL assay was performed with a terminal transferase recombinant kit (Roche, #333–574-001). The quantification of TUNEL staining was performed has previously described (6). 53BP1 staining was quantified using the ImageJ software.
Cell culture, transfection and gene silencing
DF1 cells (ATCC) were grown at 39°C in DMEM (ATCC) containing 10% FBS (PAA, The cell culture company, USA). U87, U251 and T98G were grown at 37°C in DMEM containing 10% FBS. The cell lines used in the manuscript have not been tested or authenticated. DF1 cells were transfected with the RCAS-PDGF viral plasmid, using Fugene 6 Transfection reagent (Roche), accordingly to manufacture protocol. pGIPZ lentiviral 53bp1 shRNAmirs were purchased from Openbiosystem (clone ID and sequences are provided in Supplemental Material and Methods). pRetroSuper retroviral vectors encoding 53bp1 shRNAs (53bp1_A, 5’-GATACTGCCTCATCACAGT-3’; 53bp1_B 5’-GAACGAGGAGACGGTAATA-3’) (9) were kindly provided by Roderik Beijesbergen. Either empty pRetroSuper or pRetroSuper encoding GFP shRNA were used as control. Retroviral and lentiviral vectors were introduced into glioma cell lines using standard infection procedures.
More detailed Materials and Methods can be found in Supplemental Materials and Methods.
Results
53BP1 is heterozigously loss in human GBMs, primarily of the Proneural subtype
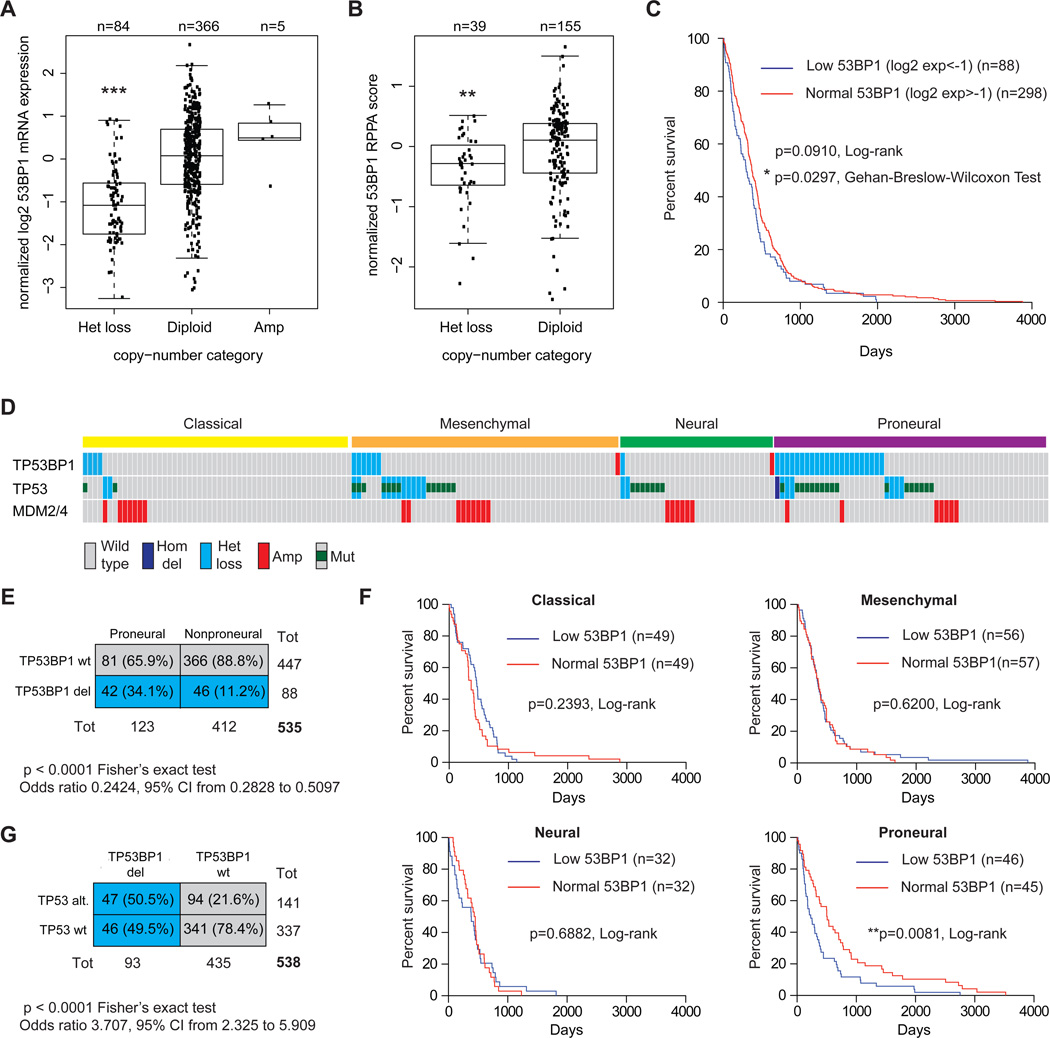
We performed an analysis of The Cancer Genome Atlas (TCGA) dataset for GBM (10) looking at 53BP1 copy number alterations (CNAs), mRNA expression levels and protein expression levels. Genomic loss of a single copy of 53BP1 was found in 17.5% (88/501) of GBM samples (Table S1). In a subset of this TCGA dataset for which mRNA or protein expression data were available, copy number loss was associated with significantly lower gene expression (p<0.0001, t-test) (Figure 1A and Table S1) and also lower 53BP1 protein levels (p=0.006, t-test), as measured by reverse phase protein array (RPPA) (Figure 1B and Table S1). Patients with lower level of 53BP1 (normalized log2 mRNA expression <-1) have a poorer survival than patients with higher level of 53BP1 (normalized log2 mRNA expression >-1) (p=0.0910, Long-rank Mantel-Cox test and p=0.0297, Gehan-Breslow-Wilcoxon test) (Figure 1C). Analogously, patients with lower 53BP1 RPPA score have a poorer survival than patients with higher 53BP1 RPPA score (p=0.0540, Long-rank Mantel-Cox test and p=0.0413, Gehan-Breslow-Wilcoxon test) (Figure S1A). We then determined whether 53BP1 gene copy was more common in a specific GBM subtype (11, 12) and we found that loss of 53BP1 is significantly associated with the Proneural subclass (p<0.0001, Fisher’s exact test). Approximately 35% of the Proneural GBMs (42/123) present single copy loss, as compared to the 11% (46/412) of non-Proneural tumors (Figure 1D, 1E and Table S1). Moreover, when the patients were stratified accordingly to the different GBM subtypes, low level of 53BP1 were associated with significant worse prognosis (p=0.0081, Long-rank Mantel-Cox test) exclusively in the Proneural subclass (Figure 1F).
Figure 1. 53BP1 is heterezygously lost in human GBM, primarily of the Proneural subtype, and co-occurs with TP53 alterations.
(A) Copy number alterations (CNAs) and mRNA expression of TP53BP1 in the TCGA dataset of human GBMs (***p<0.0001, t-test). Expression data are normalized on the average expression of diploid samples. (B) 53BP1 protein expression measured by reverse phase protein array (RPPA) (**p=0.006, t-test). (C) Kaplan-Meier survival curve of GBM patients with low (normalized log2<-1) and normal/high (normalized log2>-1) 53BP1 mRNA expression. (D) Gene-dosage profiles for TP53BP1, TP53 and MDM2/4 across 191 GBMs in TCGA dataset, separated accordingly to the four molecular subtypes of glioblastoma (Classical, Mesenchymal, Neural, and Proneural). (E) Two way contingency table showing that TP53BP1 copy loss is significantly associated with the Proneural subtype. (F) Kaplan-Meier survival curve of GBM patients of the indicated subtypes; “low 53BP1”=bottom 50% and “normal 53BP1”=top 50%). (G) Two way contingency table indicating co-occurrence of TP53BP1 copy loss with TP53 alterations.
53BP1 cooperates with TP53 in tumor suppression, and the loss of one or both copies of 53BP1 greatly accelerates lymphomagenesis in a p53-null mouse model (4, 5). Consequently we analyzed the TCGA GBM dataset for the co-occurrence of 53BP1 gene copy loss and TP53 alterations (either gene copy loss or somatic mutations). There is a significant co-occurrence of 53BP1 and p53 alterations (p<0.0001, Fisher’s exact test), but not with MDM2 or MDM4 amplifications, both well-described p53 inhibitors. Approximately 50% (47/93) of the patients with one 53BP1 gene copy also present alterations in p53 (Figure 1D, 1G, S1B, S1C and Table S2), suggesting that 53BP1 might work in p53-indipendent manner in the gliomagenesis process.
53bp1 is a haploinsufficient tumor suppressor in a glioma mouse model
The frequent loss of 53BP1 in human GBMs suggested a putative tumor suppressor activity of this molecule in gliomas. Hence, to directly demonstrate a role of 53BP1 loss in glioma formation, we took advantage of the RCAS/tv-a system, which uses a specific avian leukosis virus (RCAS) to mediate gene transfer into somatic cells transgenic for its receptor (tv-a). In this study we used the Nestin-tv-a (Ntv-a) mice that express the tv-a receptor under the control of the Nestin promoter, a marker of neural/glial stem and progenitor cells (13). Newborn mice were injected with cells producing the RCAS retroviruses carrying the Platelet-Derived Growth Factor-B (PDGFB) (14).
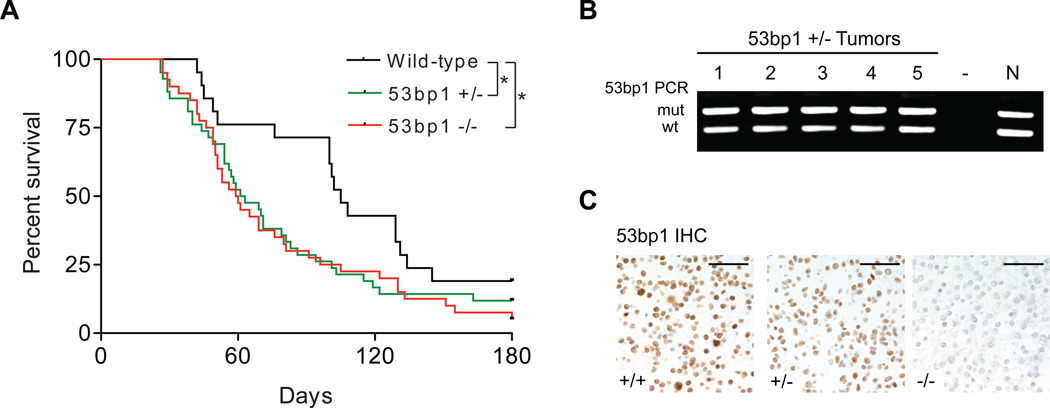
In Ntv-a mice, loss of either one or both copies of 53bp1 similarly accelerates PDGF-induced glioma formation, with the wild-type mice having an average survival of 105 days, 53bp1−/− mice of 59.5 days (p=0.0255, Log-rank test) and 53bp1+/− of 62 days (p=0.0470, Log-rank test) (Figure 2A). Loss of heterozigosity (LOH) was not detected in 53bp1+/− gliomas (Figure 2B). Expression of 53BP1 protein, as measured by immunohistochemistry (IHC), appears to be lower in 53bp1+/− gliomas compared to wild-type tumors, but was still detectable as shown in Figure 2C, suggesting that 53bp1 might behave as a classical haploinsufficient tumor suppressor gene.
Figure 2. 53bp1 is a haploinsufficient tumor suppressor in a glioma mouse model.
(A) Kaplan-Meier survival curves of PDGF-induced gliomas in Nestin-tva mice of the indicated genotypes. (B) Genotyping PCR was performed on genomic DNA extracted from 53bp1+/− tumors. N, normal tissue; wt and mut, wild-type and mutant allele respectively. (C) Immunohistochemistry (IHC) staining with anti-53bp1 antibody, performed on gliomas of the indicated genotypes. Scale bars, 100 εm.
Robust 53bp1 knockdown improves the response to DNA damaging therapy in GBM cells
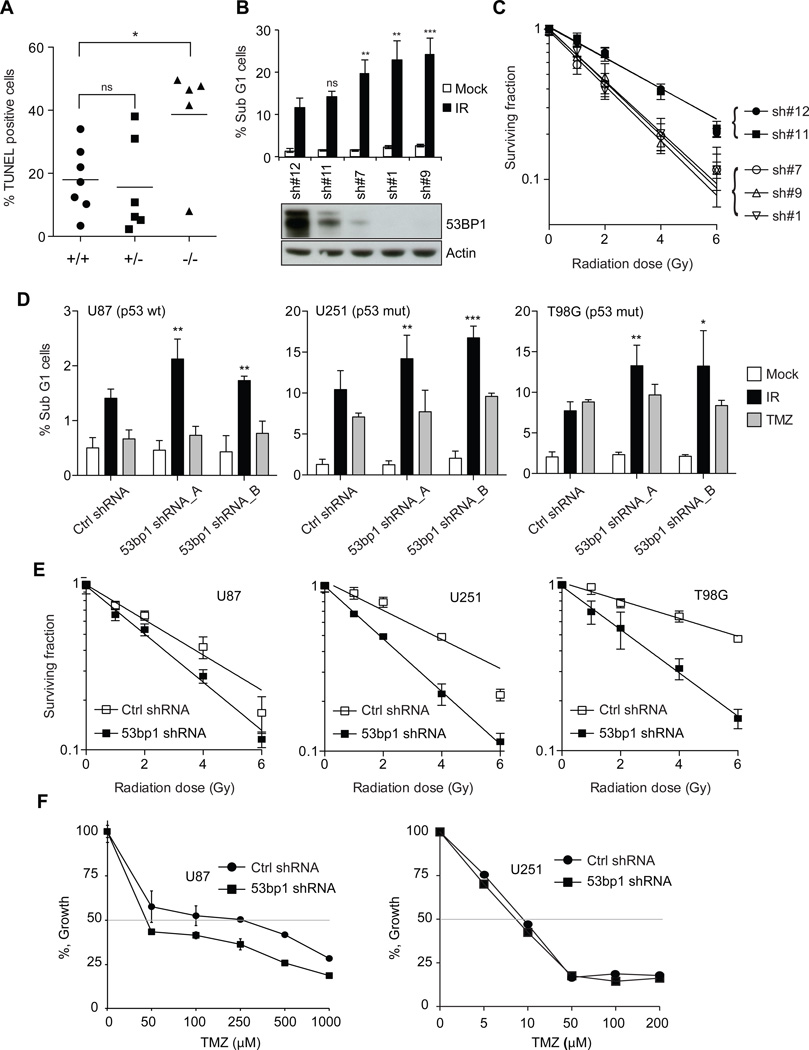
53BP1 plays a well-established role in the DNA damage response. Therefore we determined whether gliomas of different 53bp1 genotype presented alterations in radiation sensitivity in vivo. Glioma-bearing mice were exposed to 10 Gy IR and apoptosis was measured after 24h. Upon treatment with IR 53bp1−/− but not 53bp1+/− gliomas exhibited a significant increase of TUNEL positive cells as compared to that seen for wild-type tumors (p<0.05, Student t-test) (Figure 3A). Analogously, when we exposed to IR normal primary brain cultures derived from pups from the different genotypes, only 53bp1−/− and not 53bp1+/− cells presented an increased frequency of apoptotic cells, relatively wild-type cells (Figure S2A).
Figure 3. Efficient 53BP1 gene silencing sensitize GBM cell lines to DNA damaging therapy.
(A) Percentage of TUNEL positive glioma cells in tumor-bearing mice of the indicated genotypes; t-test *p=0.0272. (B) Top panel: Percentage of sub-G1 cells in U251 cells transduced with the pGIPZ shRNAs. Bottom panel: Western blot analysis showing 53BP1 knockdown efficiency. (C) Colony formation assay of U251 cells transduced with the indicated pGIPZ shRNAs. Data are presented as mean±SD of a representative of 2 independent experiments, each performed in triplicate. (D) Percentage of sub-G1 cells in U87MG, U251 and T98G glioma cell lines transduced with a pSuper control (ctrl) shRNA or two different shRNAs targeting 53bp1, upon IR or TMZ treatment. Data are presented as mean±SD of a representative of either 2 or 3 independent experiments, each performed in triplicate; t-test: ***p<0.001, **p<0.01, *p<0.05. (E) Colony formation assay of the indicated cell lines transduced with ctrl shRNA or 53bp1 shRNA _A. (F) Cell counts of U87MG (left panel) and U251 (right panel) cell lines transduced with ctrl shRNA or 53bp1 shRNA _A, at 3 days after TMZ exposure. Data are presented as mean±SD of a representative of 2 independent experiments, each performed in triplicate.
To further characterize the role of 53BP1 in glioma therapeutic response, we silenced its expression with a panel of 11 different 53BP1 shRNAs (cloned into the pGIPZ lentiviral vector) in two different glioma cell lines, U251 and T98G (Figure S2B). We next selected four shRNAs with various knockdown efficiency (sh#11 ≈50%, sh#7 ≈80%, sh#9 and sh#1 ≈100%), when compared to the non-targeting shRNA (sh#12). The cells were then exposed to 10Gy IR and the frequency of apoptotic cells was measured as sub-G1 population by propidium iodide staining, 72 hr after treatment. As shown in figure 3B, in U251 cells we observed an increase in the percentage of apoptotic cells that is proportional to the increase in 53BP1 silencing. Similarly to what we noticed in the RCAS glioma model and in the primary brain cell cultures, we observe no difference between control cells and the cells were 53BP1 expression was reduced by 50% (sh#11). Equivalent results were obtained in T98G cells (Figure S2C). Colony forming ability is considered the gold standard of radiosensitivity, therefore we then plated the cells at clonal density and exposed them to increasing doses of IR (0, 1, 2, 4 and 6 Gy). U251 cells with low 53BP1 levels (sh#7, sh#1 and sh#9) showed the lowest colony forming ability, as compared to either non-targeting shRNA (sh#12) or sh#11 (Figure 3C).
To confirm these data and to broaden our studies on 53BP1 in glioma therapy response, U87MG (p53 wild type), U251 (p53 mutant) and T98G (p53 mutant) cells were transduced with other two shRNAs that target 53BP1 mRNA, which both efficiently silenced 53BP1 protein level (Figure S2D). The cells were then exposed either to 10Gy IR or treated with temozolomide (TMZ), of which various doses were used due to the variable sensitivity of the cell lines in the study (100 εM for U87, 10 εM for U251 and 250 εM for T98G). As shown in Figure 3D, 53BP1 gene silencing significantly increases IR sensitivity across all of these cell lines, while only slightly affects the percentage of apoptotic cells upon TMZ exposure. Moreover, 53BP1 gene silencing reduced the colony formation ability of the different cell lines, with the least sensitization in U87MG cells as compared to the U251 and T98G cells (Figure 3E). We then measured the growth ability of the different glioma cells lines treated with different doses of TMZ. 53BP1 gene silencing increased the sensitivity to TMZ in U87MG cells (Figure 3F, left panel) but not in U251 cells (Figure 3F, right panel) and T98G cells (Figure S3).
These data show that although 53BP1 appears to be haploinsufficient in tumor suppression, this is not the case in therapy response. Moreover, 53BP1 function broadly protects all GBM cells from cell death in response to radiation, however, its role in TMZ response appears to be variable.
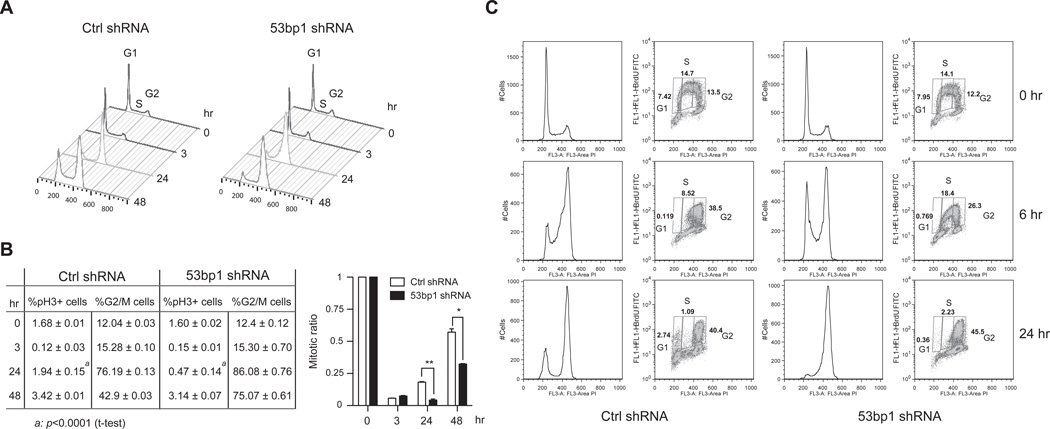
53bp1 silencing slows cell-cycle and leads to accumulation of GBM cells in G2 after IR exposure
IR and other DNA damaging agents create double-strand DNA breaks (DSBs) that are responsible for the initiation of the DDR and consequently the activation of cell-cycle checkpoints. Upon DNA damage exposure, GBM cells don’t accumulate at the G1/S checkpoint, while predominantly arrest in the G2 phase (15, 16). 53bp1−/− mouse embryonic fibroblasts (MEFs) have a minor S-phase checkpoint defect and prolonged G2/M arrest after treatment with IR (17). To better understand the role of 53BP1 in glioma radiation response we analyzed the cell-cycle checkpoints activation in GBM cells where 53BP1 expression was silenced. As determined by propidium iodide staining, U251 cells accumulated in the G2 phase at 24 hr after 10Gy IR exposure. However, while the cells transduced with a control shRNA subsequently re-enter the cell-cycle the cells in which 53BP1 was knocked-down failed to do so (Figure 4A). To confirm that it is a true cell-cycle arrest (and not simply an increase in G2 phase), we performed a phospho-Histone H3 (pH3) staining, commonly used to identify mitotic cells. The G2/M checkpoint is rapidly activated in both control and 53BP1 knocked-down cells, as shown by the significant reduction of pH3 positive cells 3h post-IR (Figure 4B). On the other hand, control cells progress into mitosis 24 hr after IR exposure (pH3+ cells = 1.94±0.15) whereas the cells in which 53BP1 expression has been silenced were still arrested in G2 (pH3+ cells = 0.47±0.14) (p<0.0001, t-test). It’s worth noting that although at 48 hr the percentage of pH3+ cells in 53BP1 silenced cells is only slightly lower than control cells, because the number of cells in G2 phase much higher in 53BP1 silenced cells, the mitotic ratio (%pH3+ cells/% G2/M cells) is still significantly lower than control cells (p=0.011, t-test). A similar prolonged arrest in G2 phase, though with somewhat different kinetics (probably due to differences in cell-cycle length) was also observed in T98G and U87MG cells (Figure S4A and S4B)
Figure 4. 53BP1 knockdown in GBM cells leads to a prolonged cell-cycle arrest after exposure to IR.
(A) Cell cycle analysis of U251 cells transduced with ctrl shRNA or 53bp1 shRNA _A at 0 hr (red line), 3 hr (blue line), 24 hr (green line), 48 hr (orange line), after IR exposure. (B) Left panel: table of the percentage of pH3 positive cells and percentage of cells in G2/M phases of the cell-cycle, at the indicated time point after 10Gy of IR. Data are presented as mean±SD of a representative of 2 independent experiments, each performed in triplicate. Right panel: graph showing the mitotic ratio (%pH3+ cells/% G2/M cells) of the data presented in left panel; t-test: **p=0.0046, *p=0.011. (C) Cell cycle analysis and BrdU staining in U251 cells exposed to a 30’ pulse of BrdU followed by 10Gy of IR, and harvested at the indicated time-point after treatment.
In order to determine whether defects in the G1/S and S phase checkpoints contribute to the differences in cell-cycle progression observed with 53BP1 knock-down, U251 cells were exposed to IR (10Gy) and the percentage of cells in S phase 16 hr post-treatment was measured by BrdU incorporation. Control cells showed only a moderate reduction (approximately 20%) in the percentage of BrdU positive cells relative to mock-irradiated cells. By contrast, in cells where 53bp1 expression had been silenced we detected an increase of BrdU positive cells (from 40% to 100%, depending on the experiment) (Figure S4C). This unexpected increase in the number of cells incorporating BrdU upon IR exposure might be due either to lengthened S phase or a compromised S phase arrest in 53BP1 defective cells. To explore these two hypotheses we gave the cells a short pulse of BrdU (30’) and followed their progression through the cell-cycle after exposure to IR. As shown in figure 4C, at 6hr post-IR in the control cells the BrdU positive cells are mainly in late S and G2 phases, having only 8.5% of BrdU positive cells with a S phase DNA content. By contrast, the 53bp1 shRNA cells lagged behind with 18.4% of BrdU positive cells having an S phase DNA content, suggesting that 53BP1 loss compromises the progression through S phase after exposure to IR. Analogous to what we describe above, by 24 hr post-IR the control shRNA cells are re-entering the cell-cycle while the 53bp1 shRNA cells were still arrested in G2.
53BP1 is required for efficient nonhomologous end-joining in GBM cells
In eukaryotic cells two major pathways are responsible for the repair of DSBs: the error-free homologous recombination (HR), that uses the intact sister chromatid as a template, and the error-prone nonhomologous end-joining (NHEJ), with direct joining at the break site. Considering that many of the different effects in IR response observed in GBM cells could be related to defects in DSBs repair ability, we tested which of the two major DNA repair pathways (HR or NHEJ) was affected in GBM cells depleted for 53BP1.
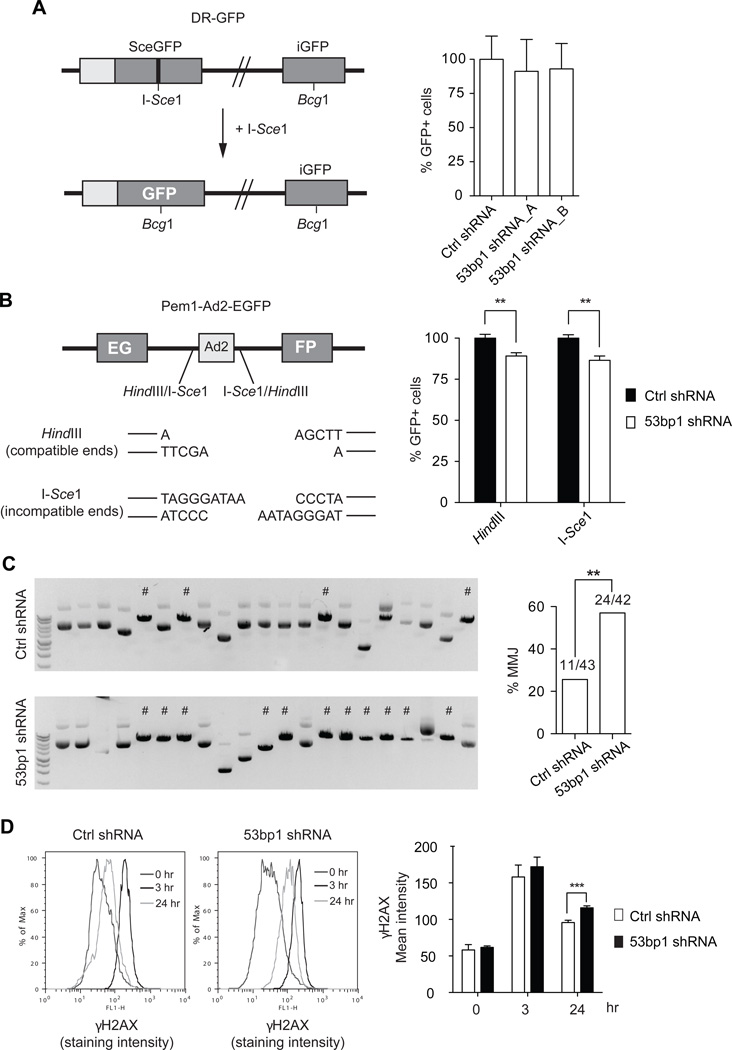
To study HR we took advantage of the DR-GFP reporter system (18), an assay that has been widely used to identify HR components of DNA repair. The DR-GFP reporter is made of two differentially mutated green fluorescent protein (GFP) gene repeats, with the upstream copy (SceGFP) containing a recognition site for the I-SceI endonuclease and the downstream copy being a truncated inactive GFP fragment (iGFP) (Figure 5A). Expression of the I-SceI enzyme leads to the creation of DSB in the upstream GFP gene copy; homologous recombination of the DSB will result in GFP+ cells that can be quantified by flow cytometry. U251 cells that were stably transduced with control shRNA and with two different shRNAs that target 53BP1, transiently transfected with the DR-GFP reporter and an expression plasmid encoding the I-SceI endonuclease were analyzed by FACS 24 hr later. As shown in the graph in Figure 5A, no differences in HR efficiency between the two cell lines were detected.
Figure 5. 53BP1 is required for an efficient NHEJ, while represses alternative-NHEJ.
(A) Left panel: schematic representation of the DR-GFP construct and assay used to measure HR efficiency (see text for details). Right panel: graph showing HR analysis performed in U251 cells transduced with the indicated shRNAs. Data are presented as mean±SD of 3 independent experiments. (B) Left panel: schematic representation of the Pem1-Ad2-EGFP construct and assay used to measure NHEJ efficiency (see text for details). Right panel: graph showing NHEJ analysis results, performed in U251 cells transduced with ctrl shRNA or 53bp1 shRNA_A and with the Pem1-Ad2-EGFP previously linearized in vitro with either HindIII or I-SceI enzymes. Data are presented as mean±SD of 3 independent experiments, each done in either duplicate or triplicate; t-test: **p<0.005. (C) Left panels: Representative ethidium bromide stained agarose gels showing HindIII digestion products on the recovered plasmids from the NHEJ assay in (B). # indicate microhomology-mediated junctions (MMJ) events. Right panel: graph showing the percentage of MMJ in ctrl shRNA and 53bp1 shRNA U251 cells; Fisher’s exact test: **p=0.0042. (D) DNA damage measured by γH2AX staining and analysis by flowcytometry, of U251 cells after exposure to IR. Left panel: Representative γH2AX staining intensity distribution. Right panel: graph of γH2AX mean intensity. Data are presented as mean±SD of 3 independent experiments, each performed in either duplicate or triplicate; t-test: ***p=0.0005.
We then analyzed NHEJ efficiency using the Pem1-Ad2-EGFP reporter assay (19, 20). This reporter construct consists of a EGFP coding sequence interrupted by the 2.4 kb Pem1 gene intron in which it has been inserted the adenoviral exon Ad2, flanked at both sides by two HindIII restriction sites and two recognition sites for the I-SceI endonuclease (in opposite directions). Digestion in vitro with the HindIII enzyme leads to the creation of cohesive ends, while digestion with I-SceI leads to the formation of incompatible ends (Figure 5B). Once the linearized plasmid is transduced into cells, it can be re-circularized by NHEJ, the Pem1 intron is spliced out restoring EGFP expression and the GFP+ cells can be detected by FACS. Control shRNA and 53bp1 shRNA U251 cells were transduced with the linearized Pem1-Ad2-EGFP plasmid and analyzed by flow cytometry after 48 hr. An approximate 10–15% reduction of NHEJ efficiency was consistently detected in 53bp1 shRNA U251 cells using either HindIII or I-SceI linearized plasmids (t-test, p=0.0034 and p=0.0018, respectively) (Figure 5B). The Pem1-Ad2-GFP reporter can also be transduced into the cells prior to the linearization and a DSB can be induced by co-transduction of the I-SceI endonuclease, parallel to the HR assay. Similar to that observed for the in vitro linearized plasmid, 53bp1 shRNA U251 cells showed significantly lower NHEJ efficiency (p=0.0069, t-test) (Figure S5A).
At least two molecularly distinct sub-pathways of NHEJ have been documented: a prominent “classic” pathway (C-NHEJ) and a less-understood “alternative” pathway (A-NHEJ), known also as microhomology-mediated end joining (MMEJ) (21). While the C-NHEJ, normally may lead to small insertions or deletion at the junction site, the A-NHEJ always results in deletions (often with microhomology at the repair junction) and is frequently associated with chromosome translocation. One advantage of the Pem1-Ad2-EGFP reporter assay is that the repaired plasmids can be recovered from the cells and molecularly analyzed (20, 22). The HindIII -linearized substrate contains 4bp compatible overhangs that represent microhomologous sequences. When these overhangs are used to mediate the repair event, the product now contains a single HindIII restriction site. As a consequence, the recovered Pem1-Ad2-EGFP plasmids can be analyzed by cleavage with the HindIII enzyme and by gel electrophoresis to measure the frequency of event that reconstitutes a single HindIII site (“microhomology-mediated junctions” or MMJ). Using this system we found that 53BP1 gene silencing led to a significant increase of MMJ in U251 cells (Figure 5C), with a frequency of 25.6% (11/43) in control shRNA cells and of 57.1% (24/42) in 53bp1 shRNA cells (p=0.0042, Fisher Exact test). Similar results were obtained when the analysis of MMJ was performed in T98G cells (Figure S5B).
We then asked whether the observed differences in NHEJ were sufficient to lead to a prolonged accumulation of DNA damage. The phosphorylated form of histone H2AX, commonly known as γH2AX, is routinely used as a marker of damaged DNA and of an activated DDR and can be measured by florescence activated cell sorting (FACS). At 3 hr after IR exposure control and 53bp1 shRNA cells have similar level of γH2AX, whereas at 24 hr post treatment 53bp1 knockdown cells have significantly higher level of γH2AX (p=0.0005, t-test) (Figure 5D). All together these data would suggest that 53BP1 is required for the repair of the DNA breaks induced by IR in glioma cells, and that the increase level of DNA damage might be responsible for the prolonged cell-cycle arrest and increased apoptosis observed in the 53bp1 shRNA cells.
53bp1 silencing potentiates radiosensitivity and extends survival in a GBM orthotopic model
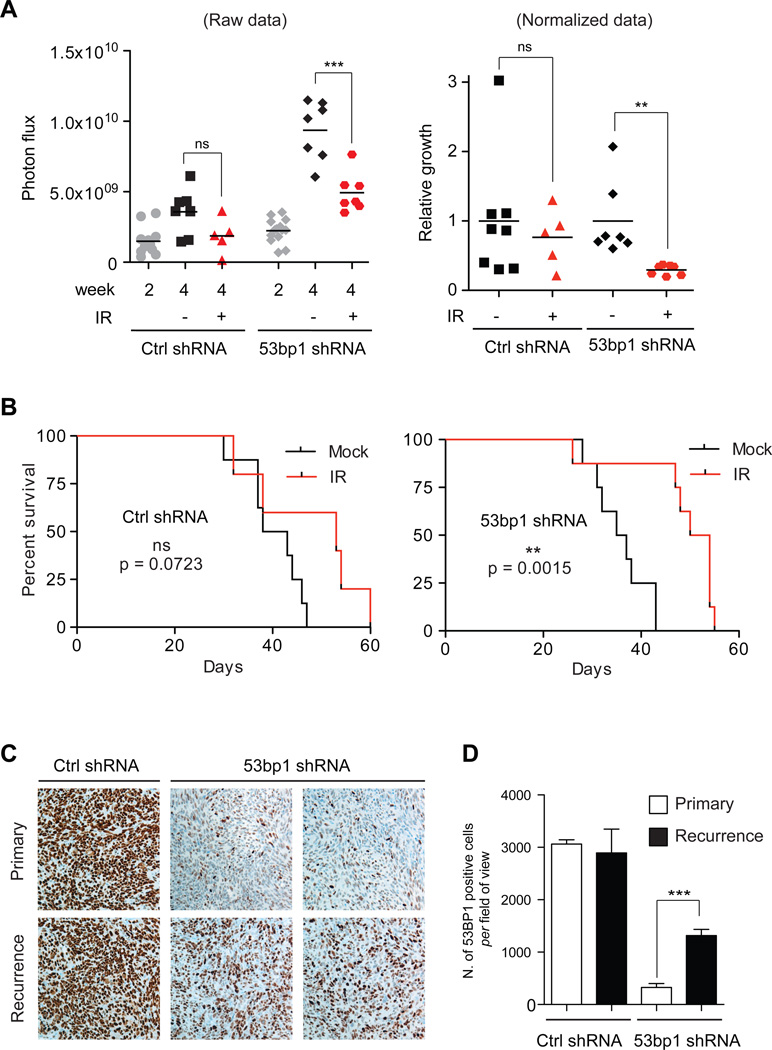
Despite having a generally poor clinical outcome, ionizing radiation and TMZ treatments are still the most effective therapies for GBMs patients. Different strategies to increase radiation efficacy are currently under investigation in numerous laboratories and particular interest has been focused on the modulation of the DNA repair pathways (23). Although 53BP1 is a tumor suppressor, because of its role in radiation response we decided to investigate whether 53BP1 inhibition might be an effective addition to radiotherapy for GBM. 53bp1−/− mice are extremely sensitive to IR and die of radiation poisoning even with local irradiation to the head (data not shown), we therefore used an orthotopic GBM model for long-term survival analysis. U251 cells were transduced with a TK-GFP-Luciferase reporter plasmid (TGL) (24) to monitor tumor growth by bioluminescence measurements, and infected with either control shRNA or 53bp1 shRNA. These cells were then injected intracranially into athymic nude mice. Two weeks after injection half of the mice of each group (ctrl shRNA or 53bp1 shRNA), received local irradiation to the brain with a single dose of 6Gy, analogous to what was used in a similar orthotopic model (16). In mice injected with control shRNA U251-TGL cells, bioluminescence analysis at two weeks post-irradiation showed a non-significant difference (t-test raw data p=0.158 and normalized data p=0.3853) in tumor progression between irradiated and non-irradiated group (Figure 6A). By contrast, the mice injected with 53bp1 shRNA U251-TGL cells showed a highly significant reduction in tumor growth (raw data, p=0.0006, t-test; normalized data, p=0.005). Consequently, survival analysis demonstrated a significant extension of survival in the irradiated group of 53bp1 shRNA injected mice (p=0.0015, Long rank test) (Figure 6B, right panel) but not in the control shRNA injected mice (p=0.0723, Long rank test) (Figure 6B, left panel). Interestingly, when we compared 53BP1 expression by IHC in the “primary” tumors (that arise in the non-irradiated groups) with that of the “recurrent” tumors (that arise in the irradiated groups) we observed that, in the mice injected with the 53bp1 shRNA U251-TGL cells, the frequency of 53BP1 positive cells was significantly higher in the “recurrent” tumors (p = 0.0002, t-test) (Figure 6C and 6D). No differences in 53BP1 staining were observed in the tumor derived from the control shRNA U251-TGL cells. A possible explanation of these data is that 53bp1 might have not been efficiently targeted in all cells by the shRNA expression, and considering that these cells survive better following IR, compared to the ones with no or low 53BP1 expression, they also might proficiently re-populate the tumor after IR exposure. As a consequence, a more efficient and homogenous silencing of 53BP1 would possibly lead to an even stronger radiosensitization of the tumors as a whole.
Figure 6. 53BP1 silencing increases radiosensitization in vivo in an orthotopic GBM mouse model.
(A) U251-TGL cells transduced with ctrl shRNA or 53bp1 shRNA_A were intracranial injected into nude mice. Two weeks after the injection the mice were divided in two groups, one of which was locally irradiated to the head with 6Gy. The graph on the left shows the bioluminescence raw data at 2 and 4 weeks after injection; the graph on the right shows the normalized data for each tumor (photon flux at 4 weeks/ photon flux at 2 weeks) presented as fold change over the average of the non-irradiated group; t-test: ns = non significative, ***p=0.0006 and **p=0.005. (B) Kaplan-Meier survival curves of mice in (A). (C) Representative IHC analysis of 53BP1, performed on primary and recurrent gliomas generated in (B). (D) Quantification of 53BP1 positive cells in gliomas as in (C). Data are presented as mean±SD of at least 3 independent tumors; t-test: ***p=0.0002.
Discussion
In recent years the DDR has emerged as an inducible barrier to tumorigenesis, and defects in elements of the DDR have been associated with different human cancers. Various studies had lately looked at 53BP1 protein expression and localization in different tumor types in human. As an example, in breast and lung tumors a subset of cases show aberrant 53BP1 activation, such as nuclear foci formation, however others presented a reduction or a complete lack of its expression, that correlated with tumor stage (25, 26). A recent report shows that 53BP1 expression is reduced in a subset of basal-like/triple-negative breast cancers and in BRCA1/2-associated breast cancers, and among the triple-negative tumors, those that lack 53BP1 staining showed decreased metastasis-free survival (27).
Here we present evidence that 53BP1 behaves as a haploinsufficient tumor suppressor in glioma. The TP53BP1 gene, which encodes for the 53BP1 protein, is localized on 15q15-q21 and an analysis of the TCGA dataset for GBM showed single copy loss spanning this chromosomal region in approximately 20% of the patients, with a significant reduction of 53BP1 mRNA and protein expression. No homozygous loss was detected. These data are consistent with a previous array-CGH (aCGH) study performed on a collection of 54 gliomas (including 31 GBMs), in which a subset of tumors showed two noncontiguous minimally deleted regions within chromosome 15q, mapping to 15q15.1 and 15q15.3 involving deletions of the RAD51 gene and the TP53BP1 gene (28). Most importantly, this study detected loss of a single gene copy of TP53BP1, both by aCGH and by real-time quantitative PCR analysis. Moreover, single-nucleotide polymorphisms (SNPs) arrays showed loss of heterozigousity (LOH) of the chromosomal region containing TP53BP1 in 55% (10/18) pediatric glioblastomas samples (29), indicating the relevance of our finding not only in the adult but also in pediatric glial tumors.
Our in vivo studies using the RCAS/PDGF glioma model ultimately confirmed the evidence of 53BP1’s haploinsufficient role in glioma formation. Indeed, loss of a single copy of TP53BP1 was sufficient to accelerate PDGF-induced glioma in mice. Similarly GBM patients with lower 53BP1 levels show a somewhat poorer prognosis (Figure 1C and S1A). It is important to note that, as further discussed below, 53BP1 appears to have haploinsufficient activity in tumor formation but not in therapy response. Nevertheless, we speculate that both of these aspects are connected to 53BP1 role in DNA repair. While loss of a single 53BP1 gene copy would be sufficient to sensitize the cells to oncogene induced DNA damage, a low persistent level of damage, this would not be the case for the acute DNA damage created by IR. In fact, it was previously shown that 53BP1 haploinsufficiency compromises genomic stability, though at lower extent than nullizigosity (4). However, we cannot exclude that this tumor suppressor activity might be linked to other not yet characterized role of 53BP1 in cellular transformation.
At present, a number of laboratories are exploring the possibility of manipulating the DDR to cause selective tumor cell death through mitotic catastrophe and as a possible therapeutic approach to improve the response to radiotherapy and chemotherapy in GBM patients (6, 23). Here we have demonstrated that 53BP1 null mouse glioma cells, but not the heterozygous tumors, and human glioma cell lines in which 53BP1 was robustly silenced by shRNA, show higher level of sensitivity to IR, both in vitro and in vivo. 53BP1 levels seem to be critical for this radiosensitization, and a 50% reduction appears not to be sufficient to increase radiation sensitivity. This hypothesis would predict that only those patients in which 53BP1 expression falls under a threshold level, or in which 53BP1 activity would be acutely inhibited, might have an improved therapy response.
Here we propose that 53BP1 might represent one DDR component that would be worth targeting in GBM patients in combination with radiotherapy. The fact that 20% of GBM patients have lower levels of 53BP1, might give an enhanced therapeutic window, with limited normal tissue toxicity. The question is how effectively can 53BP1 function be inhibited. So far, it does not appear to have any enzymatic activity that eventually can be targeted. However interfering with the proteins modifications necessary for 53BP1 recruitment to DNA damage foci would possibly lead to 53BP1 loss of function. Lastly, delivery of siRNA targeting 53BP1, by polyethylenimine (PEI)/siRNA or liposome/siRNA complexes, could be utilized as an alternative strategy, and it has been successfully used for other genes in GBM xenograft models (30–32).
Supplementary Material
Acknowledgements
We thank Robert Finney, Quancho Zhang and Eletha Carbajal for technical support and Diane Domingo for part of the flowcytometric analysis. We thank members of Dr Holland’s laboratory and Ranjit Bindra for discussion. We thank Lisa Sevenich for the help in the TUNEL quantification. We gratefully acknowledge Junjie Chen, Titia de Lange, Roderick Beijesbergen and Scott H. Kaufmann for providing reagents.
Grant support
The work of M. Squatrito was supported by a Fondazione Italiana Ricerca Cancro (FIRC) Fellowship, an American Brain Tumor Association (ABTA) Fellowship in memory of Justin Porter, and a Memorial Sloan-Kettering Brain Tumor Center Grant Award. F. Vanoli was supported by an American-Italian Cancer Foundation (AICF) Post-Doctoral Research Fellowship.
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Iwabuchi K, Bartel PL, Li B, Marraccino R, Fields S. Two cellular proteins that bind to wild-type but not mutant p53. Proc Natl Acad Sci U S A. 1994;91:6098–6102. doi: 10.1073/pnas.91.13.6098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iwabuchi K, Li B, Massa HF, Trask BJ, Date T, Fields S. Stimulation of p53-mediated transcriptional activation by the p53-binding proteins, 53BP1 and 53BP2. J Biol Chem. 1998;273:26061–26068. doi: 10.1074/jbc.273.40.26061. [DOI] [PubMed] [Google Scholar]
- 3.Noon AT, Goodarzi AA. 53BP1-mediated DNA double strand break repair: Insert bad pun here. DNA Repair (Amst) 2011 doi: 10.1016/j.dnarep.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Ward IM, Difilippantonio S, Minn K, Mueller MD, Molina JR, Yu X, et al. 53BP1 cooperates with p53 and functions as a haploinsufficient tumor suppressor in mice. Mol Cell Biol. 2005;25:10079–10086. doi: 10.1128/MCB.25.22.10079-10086.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morales JC, Franco S, Murphy MM, Bassing CH, Mills KD, Adams MM, et al. 53BP1 and p53 synergize to suppress genomic instability and lymphomagenesis. Proc Natl Acad Sci U S A. 2006;103:3310–3315. doi: 10.1073/pnas.0511259103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Squatrito M, Brennan CW, Helmy K, Huse JT, Petrini JH, Holland EC. Loss of ATM/Chk2/p53 pathway components accelerates tumor development and contributes to radiation resistance in gliomas. Cancer Cell. 2010;18:619–629. doi: 10.1016/j.ccr.2010.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, et al. The cBio Cancer Genomics Portal: An Open Platform for Exploring Multidimensional Cancer Genomics Data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holland EC, Hively WP, DePinho RA, Varmus HE. A constitutively active epidermal growth factor receptor cooperates with disruption of G1 cell-cycle arrest pathways to induce glioma-like lesions in mice. Genes Dev. 1998;12:3675–3685. doi: 10.1101/gad.12.23.3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brummelkamp TR, Fabius AW, Mullenders J, Madiredjo M, Velds A, Kerkhoven RM, et al. An shRNA barcode screen provides insight into cancer cell vulnerability to MDM2 inhibitors. Nat Chem Biol. 2006;2:202–206. doi: 10.1038/nchembio774. [DOI] [PubMed] [Google Scholar]
- 10.The Cancer Geneome Atlas Network Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature. 2008;455:1061–1068. doi: 10.1038/nature07385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brennan C, Momota H, Hambardzumyan D, Ozawa T, Tandon A, Pedraza A, et al. Glioblastoma subclasses can be defined by activity among signal transduction pathways and associated genomic alterations. PLoS One. 2009;4:7752. doi: 10.1371/journal.pone.0007752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verhaak RG, Hoadley KA, Purdom E, Wang V, Qi Y, Wilkerson MD, et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell. 2010;17:98–110. doi: 10.1016/j.ccr.2009.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holland EC, Hively WP, Gallo V, Varmus HE. Modeling mutations in the G1 arrest pathway in human gliomas: overexpression of CDK4 but not loss of INK4a–ARF induces hyperploidy in cultured mouse astrocytes. Genes Dev. 1998;12:3644–3649. doi: 10.1101/gad.12.23.3644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shih AH, Dai C, Hu X, Rosenblum MK, Koutcher JA, Holland EC. Dose-dependent effects of platelet-derived growth factor-B on glial tumorigenesis. Cancer Res. 2004;64:4783–4789. doi: 10.1158/0008-5472.CAN-03-3831. [DOI] [PubMed] [Google Scholar]
- 15.Hirose Y, Berger MS, Pieper RO. p53 effects both the duration of G2/M arrest and the fate of temozolomide-treated human glioblastoma cells. Cancer Res. 2001;61:1957–1963. [PubMed] [Google Scholar]
- 16.Mir SE, De Witt Hamer PC, Krawczyk PM, Balaj L, Claes A, Niers JM, et al. In silico analysis of kinase expression identifies WEE1 as a gatekeeper against mitotic catastrophe in glioblastoma. Cancer Cell. 2010;18:244–257. doi: 10.1016/j.ccr.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ward IM, Minn K, van Deursen J, Chen J. p53 Binding protein 53BP1 is required for DNA damage responses and tumor suppression in mice. Mol Cell Biol. 2003;23:2556–2563. doi: 10.1128/MCB.23.7.2556-2563.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pierce AJ, Johnson RD, Thompson LH, Jasin M. XRCC3 promotes homology-directed repair of DNA damage in mammalian cells. Genes Dev. 1999;13:2633–2638. doi: 10.1101/gad.13.20.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel AG, Sarkaria JN, Kaufmann SH. Nonhomologous end joining drives poly(ADP-ribose) polymerase (PARP) inhibitor lethality in homologous recombination-deficient cells. Proc Natl Acad Sci U S A. 2011;108:3406–3411. doi: 10.1073/pnas.1013715108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seluanov A, Mittelman D, Pereira-Smith OM, Wilson JH, Gorbunova V. DNA end joining becomes less efficient and more error-prone during cellular senescence. Proc Natl Acad Sci U S A. 2004;101:7624–7629. doi: 10.1073/pnas.0400726101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McVey M, Lee SE. MMEJ repair of double-strand breaks (director’s cut): deleted sequences and alternative endings. Trends Genet. 2008;24:529–538. doi: 10.1016/j.tig.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fattah F, Lee EH, Weisensel N, Wang Y, Lichter N, Hendrickson EA. Ku regulates the non-homologous end joining pathway choice of DNA double-strand break repair in human somatic cells. PLoS Genet. 2010;6:e1000855. doi: 10.1371/journal.pgen.1000855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Squatrito M, Holland EC. DNA damage response and growth factor signaling pathways in gliomagenesis and therapeutic resistance. Cancer Res. 2011;71:5945–5949. doi: 10.1158/0008-5472.CAN-11-1245. [DOI] [PubMed] [Google Scholar]
- 24.Ponomarev V, Doubrovin M, Serganova I, Vider J, Shavrin A, Beresten T, et al. A novel triple-modality reporter gene for whole-body fluorescent, bioluminescent, and nuclear noninvasive imaging. Eur J Nucl Med Mol Imaging. 2004;31:740–751. doi: 10.1007/s00259-003-1441-5. [DOI] [PubMed] [Google Scholar]
- 25.Bartkova J, Horejsi Z, Sehested M, Nesland JM, Rajpert-De Meyts E, Skakkebaek NE, et al. DNA damage response mediators MDC1 and 53BP1: constitutive activation and aberrant loss in breast and lung cancer, but not in testicular germ cell tumours. Oncogene. 2007;26:7414–7422. doi: 10.1038/sj.onc.1210553. [DOI] [PubMed] [Google Scholar]
- 26.Nuciforo PG, Luise C, Capra M, Pelosi G, d’Adda di Fagagna F. Complex engagement of DNA damage response pathways in human cancer and in lung tumor progression. Carcinogenesis. 2007;28:2082–2088. doi: 10.1093/carcin/bgm108. [DOI] [PubMed] [Google Scholar]
- 27.Bouwman P, Aly A, Escandell JM, Pieterse M, Bartkova J, van der Gulden H, et al. 53BP1 loss rescues BRCA1 deficiency and is associated with triple-negative and BRCA-mutated breast cancers. Nat Struct Mol Biol. 2010;17:688–695. doi: 10.1038/nsmb.1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bredel M, Bredel C, Juric D, Harsh GR, Vogel H, Recht LD, et al. High-resolution genome-wide mapping of genetic alterations in human glial brain tumors. Cancer Res. 2005;65:4088–4096. doi: 10.1158/0008-5472.CAN-04-4229. [DOI] [PubMed] [Google Scholar]
- 29.Qu HQ, Jacob K, Fatet S, Ge B, Barnett D, Delattre O, et al. Genome-wide profiling using single-nucleotide polymorphism arrays identifies novel chromosomal imbalances in pediatric glioblastomas. Neuro Oncol. 2010;12:153–163. doi: 10.1093/neuonc/nop001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grzelinski M, Urban-Klein B, Martens T, Lamszus K, Bakowsky U, Hobel S, et al. RNA interference-mediated gene silencing of pleiotrophin through polyethylenimine-complexed small interfering RNAs in vivo exerts antitumoral effects in glioblastoma xenografts. Hum Gene Ther. 2006;17:751–766. doi: 10.1089/hum.2006.17.751. [DOI] [PubMed] [Google Scholar]
- 31.Kato T, Natsume A, Toda H, Iwamizu H, Sugita T, Hachisu R, et al. Efficient delivery of liposome-mediated MGMT-siRNA reinforces the cytotoxity of temozolomide in GBM-initiating cells. Gene Ther. 2010;17:1363–1371. doi: 10.1038/gt.2010.88. [DOI] [PubMed] [Google Scholar]
- 32.Hendruschk S, Wiedemuth R, Aigner A, Topfer K, Cartellieri M, Martin D, et al. RNA interference targeting survivin exerts antitumoral effects in vitro and in established glioma xenografts in vivo. Neuro Oncol. 2011;13:1074–1089. doi: 10.1093/neuonc/nor098. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.