The learning curve for laparoendoscopic single-site (LESS) surgery was found to be definable, short, and safe.
Keywords: Learning curve, LESS, Nissen fundoplication, Laparoendoscopic single-site surgery, SILS
Abstract
Background and Objectives:
This study of laparoendoscopic single-site (LESS) fundoplication for gastroesophageal reflux disease was undertaken to determine the “learning curve” for implementing LESS fundoplication.
Methods:
One hundred patients, 38% men, with a median age of 61 years and median body mass index of 26 kg/m2, underwent LESS fundoplications. The operative times, placement of additional trocars, conversions to “open” operations, and complications were compared among patient quartiles to establish a learning curve. Median data are reported.
Results:
The median operative times and complications did not differ among 25-patient cohorts. Additional trocars were placed in 27% of patients, 67% of whom were in the first 25-patient cohort. Patients undergoing LESS fundoplication had a dramatic relief in the frequency and severity of all symptoms of reflux across all cohorts equally (P < .05), particularly for heartburn and regurgitation, without causing dysphagia.
Conclusion:
LESS fundoplication ameliorates symptoms of gastroesophageal reflux disease without apparent scarring. Notably, few operations required additional trocars after the first 25-patient cohort. Patient selection became more inclusive (eg, more “redo” fundoplications) with increasing experience, whereas operative times and complications remained relatively unchanged. The learning curve of LESS fundoplication is definable, short, and safe. We believe that patients will seek LESS fundoplication because of the efficacy and superior cosmetic outcomes; surgeons will need to meet this demand.
INTRODUCTION
Gastroesophageal reflux disease (GERD) is the most common gastrointestinal diagnosis given by physicians in the United States, accounting for >9.1 million medical office visits per year.1 A review of the epidemiology of GERD shows that symptoms indicative of GERD are prevalent in the general population and up to 20% of Americans have GERD-related symptoms on a weekly basis.2–4 The medical treatment costs for GERD in the United States are reported to be >$6 billion per year!
The rising prevalence of GERD has been the driving force behind the search for a definitive treatment for reflux.5–11 Patients with GERD typically have two treatment options: lifestyle modifications with medical therapy involving the use of proton pump inhibitors or surgical therapy. Several randomized studies comparing medical treatment versus surgical treatment have shown surgical therapy to be more effective for long-term relief of GERD. Nissen fundoplication is the most commonly undertaken antireflux operation in the United States, and it has evolved significantly from the early days of “open” operations to minimally invasive procedures involving the use of laparoscopy today. Over the past two decades, there has been wide acceptance of laparoscopic fundoplication. Today, the surgical “gold standard” for treating symptoms of GERD is antireflux laparoscopic fundoplication.
Improvements of operative techniques are continuously occurring in the art of surgery. A combination of refinements in laparoscopic tools and increasing surgical experience with laparoscopy has led to the development of laparoendoscopic single-site (LESS) surgery. LESS surgery is undertaken using a single incision at the umbilicus, and it has myriad applications in surgery (cholecystectomy, colectomy, splenectomy, Heller myotomy, fundoplication, gastrectomy, and so on). The main premise behind LESS surgery is no apparent scar. Thus a cosmetically superior approach to antireflux operations can be achieved by the LESS approach when compared with conventional multi-incision laparoscopic antireflux techniques. In addition, other clinical measures that promote LESS fundoplication may include decreased postoperative pain, shorter hospital length of stay, reduction in wound infections, and decreased incisional hernias. We have, thus, undertaken this study to document our learning curve for the LESS approach to fundoplication; the specific purpose of our study was to show that laparoscopic skills are transferable to the LESS approach. Our hypothesis undertaking this study was that the learning curve for LESS fundoplication is short, definable, and safe.
MATERIALS AND METHODS
The study design and patient data collection were conducted with Institutional Review Board approval at the University of South Florida College of Medicine. A prospectively collected database was maintained. Our first consecutive 100 patients undergoing LESS fundoplication for chronic GERD at Tampa General Hospital beginning in May 2008 were reviewed. With informed consent, patients underwent LESS fundoplication as a definitive antireflux therapy. Demographic data were collected preoperatively for all patients, and these patients were followed up prospectively.
Preoperative assessment of patients' GERD included esophagogastroduodenoscopy. In addition, a 48-hour ambulatory esophageal pH monitoring study (eg, Bravo pH study) was conducted to determine the DeMeester score and to confirm the presence of acid reflux. Esophageal motility was studied to determine the presence or absence of esophageal dysmotility. Patients underwent stationary water perfusion esophageal manometry or esophagography, by use of a barium-laden food bolus, while positioned in a 15° head-down position.12
For illustrative purposes, our first 100 patients undergoing LESS fundoplication were divided into consecutive quartiles of 25 patients. We measured the operative times, in minutes, from the time of incision until completion of the application of a dressing. We recorded when operations used additional trocars as well as when operations were converted to open procedures. The operations were undertaken by two laparoscopic surgeons who already had 1 year of experience with single-incision laparoscopic surgery (SILS) (not including fundoplications for GERD). In the first cohort, 14 operations were undertaken by both surgeons together. The remaining 86 operations were undertaken separately by either surgeon with close collaborative learning. We also sought to determine, as proficiency was obtained, whether we extended their patient criteria and undertook more complex cases (ie, “redo” fundoplications, patients with a higher body mass index [BMI]), or patients with concomitant giant hiatal hernias) while maintaining the LESS approach.
Operative Technique
LESS fundoplication was undertaken through a 12-mm vertical skin incision made within the umbilicus while preserving the umbilical ring. Occasionally, a cruciate incision was used if the vertical skin incision would not permit the insertion of the single port. The abdominal wall fascia was divided sharply within the midline, permitting entry into the peritoneal cavity. When possible, the operation was completed through the umbilicus alone and no additional incisions were necessary. A single multitrocar port was used, generally an SILS port (Covidien, Norwalk, CT, USA) or TriPort (Olympus, Center Valley, PA, USA). When the SILS port was used, the insufflation catheter was removed, and instead, a 5-mm trocar was inserted. This maneuver allowed us to have four 5-mm low-profile trocars.
A 5-mm deflectable-tip laparoscope (LTF-VH Deflectable Tip Video Laparoscope; Olympus) was inserted through the 7-o'clock trocar position to visualize the peritoneal cavity. Next, a malleable fan retractor, which was placed at the 5-o'clock trocar position, was used to retract the liver. The upper 5-mm trocars in the 1-o'clock and 11-o'clock positions were interchangeably used for a grasper and for an energy device. During dissection along the right crus, the optimal arrangement of the instruments in the top trocars is the grasper at the 11-o'clock position and the energy device at the 1-o'clock position. During dissection along the left crus and taking down of the short gastric vessels, there is less torque and instrument clashing when the energy device is in the 11-o'clock position and the grasper is in the 1-o'clock trocar position. We began by first taking down the gastrohepatic omentum in a stellate fashion. The dissection was carried up and down the right crus and into the mediastinum. The stomach was then rolled to the patient's right side, and the short gastric vessels were divided. The dissection was carried up and down the left crus. The dissection was carried into the mediastinum to reduce any hiatal hernia present. Our aim was to deliver 8 cm of esophagus into the peritoneal cavity. The hernia sac and the gastroesophageal fat pad were excised. A posterior cruraplasty was undertaken without a bio-prosthesis. A Nissen or Toupet fundoplication was constructed well above the gastroesophageal junction, over a 52F to 60F bougie depending on patient size, with the latter fundoplication used if preoperative study showed esophageal dysmotility. A 5-mm conventional laparoscopic needle holder and O-gauge polyester sutures on a ski needle or a 10-mm Endo Stitch (Covidien) were used for suturing by use of the 1-o'clock trocar position. For the construction of the Nissen fundoplication, the anterior fundus of the stomach was brought to the esophagus and then to the posterior fundus with two interrupted sutures and a third suture brought the anterior fundus to the posterior fundus of the stomach at the level of the gastroesophageal junction. For the construction of the Toupet fundoplication, the posterior fundus was sutured to the right side of the esophagus with 3 interrupted sutures and the anterior fundus was sutured to the left side of the esophagus with 3 additional interrupted sutures to construct a 270° wrap. Intraoperative endoscopy was used to confirm the location of the fundoplication above the gastroesophageal junction. Next, the posterior fundus was sutured to the esophagus and then to the right crus to reduce tension on the wrap and to prevent twisting of the esophagus. The fascia at the umbilicus was closed with a monofilament absorbable suture placed in a figure-of-8 fashion, the skin was approximated with an absorbable suture, and sterile dressing was applied.
Early on, if additional operative exposure was needed, a polypropylene suture on a Keith needle was placed through the body of the stomach and brought through the right side of the anterior abdominal wall to aid in the mobilization of the gastric fundus. This has been abandoned since our very early experience, and instead, an internal retractor (EndoGrab Port-Free Endocavity Retractor; Virtual Ports, Richmond, VA, USA) was used occasionally for exposure when necessary. Most of the dissection was carried out with ultrasonic shears (Auto-Sonix; Covidien), including the division of the short gastric vessels, or a bipolar energy device (LigaSure; Covidien). Lastly, intraoperative endoscopy was used to confirm the appropriate location of the fundoplication above the gastroesophageal junction.
To determine the efficacy and functional outcomes of the LESS fundoplications, patients scored the frequency and severity of their symptoms before and after their fundoplication (at each postoperative follow-up appointment) using a Likert scale (0, indicating never/not bothersome, to 10, indicating always/very bothersome). This scoring system has been used by us since 1991. Symptoms of GERD, including heartburn, dysphagia, regurgitation, coughing, and chest pain, were recorded (Table 1). Patients were queried about their satisfaction with their umbilical/surgical scar, as well as their overall experience, with responses ranging from very unsatisfied to very satisfied.
Table 1.
Some Symptoms Queried Before and After LESS Fundoplication
| How often do you experience the following? |
| Food gets stuck |
| Postprandial chest pain |
| Forceful vomiting |
| Regurgitation |
| Choking |
| Coughing |
| Heartburn |
| Severity of symptoms |
| Heartburn after meals/while sleeping |
| Nausea/vomiting/regurgitation after meals |
| Food stuck in throat/chest |
| Difficulty swallowing |
| Bitter taste in mouth after meals/while sleeping |
| Asthma/coughing |
| Gas/bloating |
| Have you had dietary changes for the following? |
| Spicy foods |
| Bread |
| Meat |
| Coffee |
| Alcohol |
Patients were asked at follow-up whether they would have the operation again, knowing what they know now. Data from last follow-up were analyzed. Data were maintained on a spreadsheet (Excel; Microsoft, Redmond, WA, USA) and analyzed with GraphPad InStat, version 3.06 (GraphPad Software, San Diego, CA, USA). Where appropriate, data are presented for illustrative purposes as median (mean ± standard deviation). Significance is accepted with 95% confidence. Symptom frequency and severity before and after fundoplication were compared by use of the Mann-Whitney U test.
RESULTS
Beginning in May 2008, 100 patients with a median age of 61 years (mean, 56 ± 14.8 years) and a median BMI of 26 kg/m2 (mean, 26 ± 3.2 kg/m2) underwent LESS fundoplication for the treatment of GERD. Sixty-two percent of these patients were women (Table 1). All patients reported chronic suffering from GERD with a preoperative DeMeester score of 34 (mean, 39 ± 30.7).
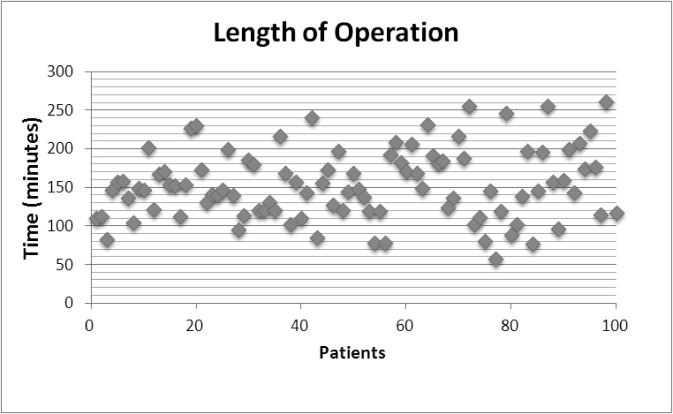
Operative data for patients undergoing LESS fundoplication were divided into 4 consecutive cohorts of 25 patients (Table 2). The median operative time across all quartiles was 147 minutes (mean, 154.9 ± 53.3 minutes). No differences in operative time were found among quartiles (Figure 1). Five patients underwent redo fundoplication by the LESS approach, all after the second quartile. Intraoperative complications or intraoperative adverse events occurred in 5 patients: 2 had inadvertent gastrotomies and 3 had uncomplicated capnothoraces; 1 patient had uncomplicated bilateral capnothoraces. Postoperative complications occurred in 8 patients: 3 had esophageal edema, 2 had cardiac dysrhythmia, 2 had urinary retention, and 1 had excessive abdominal pain. The length of hospital stay for all patients undergoing LESS fundoplication was 1 day (mean, 2 ± 1.4 days). The longer hospital stays were always a consequence of medical comorbidities.
Table 2.
Operative Details for 100 Patients Undergoing LESS Fundoplication
| Cohort 1–25 | Cohort 26–50 | Cohort 51–75 | Cohort 76–100 | All Patients | |
|---|---|---|---|---|---|
| Length of operation (min) | 147 (148 ± 35.6) | 137 (159 ± 72.6) | 169 (163.5 ± 45.4) | 146 (149 ± 54.6) | 147 (154 ± 53.3) |
| Nissen/Toupet | 21/4 | 19/6 | 20/5 | 22/3 | 82 (82%)/18 (18%) |
| Hiatal hernia | 23 | 24 | 23 | 24 | 94 (94%) |
| Giant hiatal hernia | 3 | 6 | 4 | 7 | 20 (20%) |
| Additional trocar (g:n) | 18/25 | 8/25 | 0/25 | 1/25 | 27/73 |
| No. of conversions to open operations | 0 | 0 | 0 | 0 | 0 |
| No. of redo fundoplications | 0 | 0 | 3 | 2 | 5 |
| Intraoperative complications | Gastrotomy (1) | Capnothorax (1) | Capnothorax (1) Gastrotomy (1) |
Bilateral capnothoraces (1) | 5 |
| Postoperative complications | Esophageal edema (1) | Esophageal edema (1) Cardiac dysrhythmia (1) |
Abdominal pain (1) Esophageal edema (1) Urinary retention (1) |
Cardiac dysrhythmia (1) Urinary retention (1) |
8 |
Figure 1.
Operative times, in minutes, beginning at the time of incision until completion of the application of a dressing.
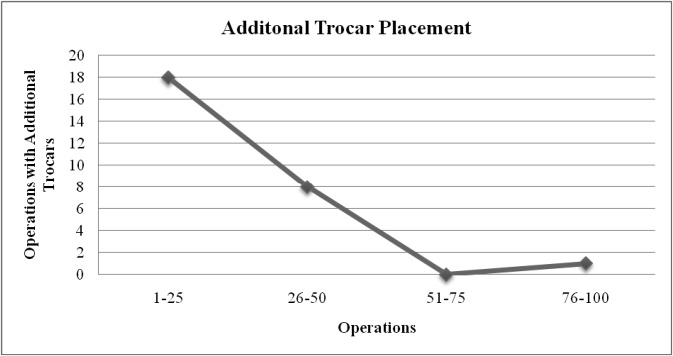
Of the 100 patients in our study, 27 required additional trocars during their operations. However, we identified a significant decrease in the number of operations that used additional trocars after the first quartile (P < .05) (Figure 2). The use of additional trocars was seen in 18 of 25 operations (72%) in the first quartile, 8 of 25 operations (32%) in the second quartile, 0 of 25 operations (0%) in the third quartile, and 1 of 25 operations (4%) in the fourth quartile. Of the operations requiring additional trocars, 66% were in the first quartile. The need for additional trocars was brought about by operative difficulty, which in all cases was related to the difficulty of dealing with a giant hiatal hernia. Ninety-four patients (94%) also had hiatal hernias, of which 20 (21%) were defined as giant hiatal hernias (hernias that include at least 30% of the stomach in the chest and/or other organs [small bowel, colon, and so on]) (Table 2). No operations throughout this study required conversion to open fundoplications. Endoscopy at each operation confirmed the appropriate location of the fundoplication relative to the gastroesophageal junction and a grade I gastroesophageal flap value.
Figure 2.
Placement of additional trocars for LESS fundoplication.
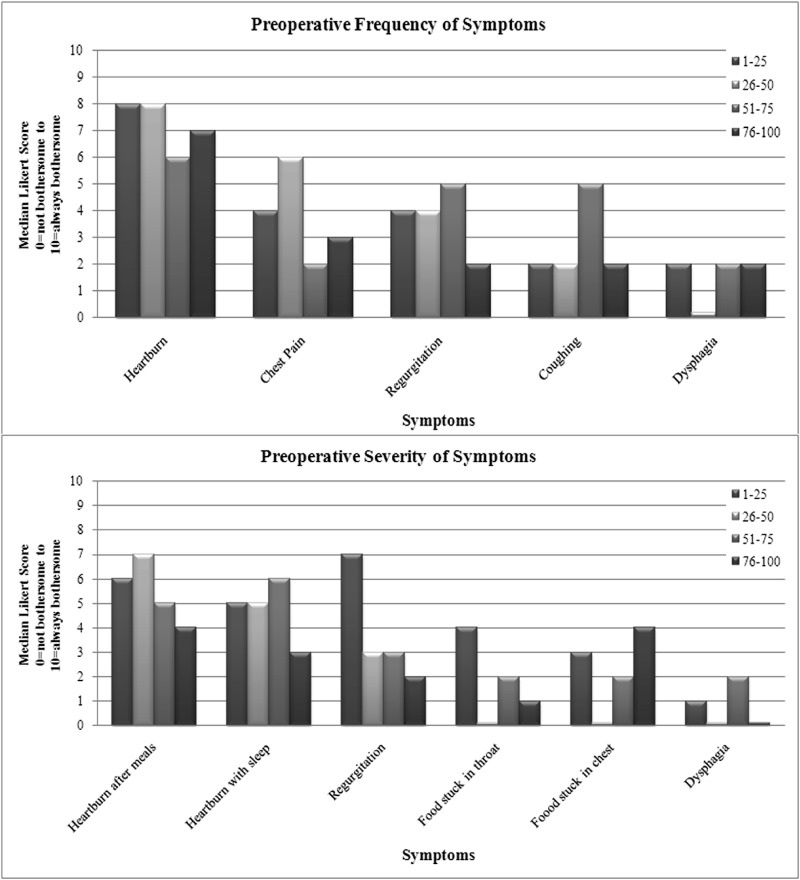
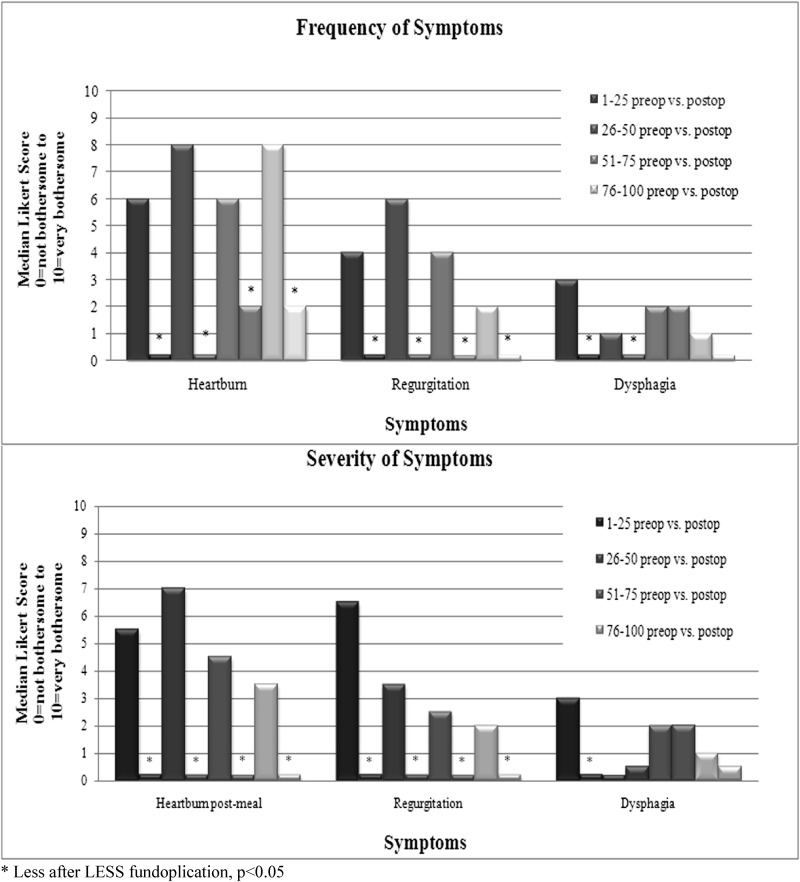
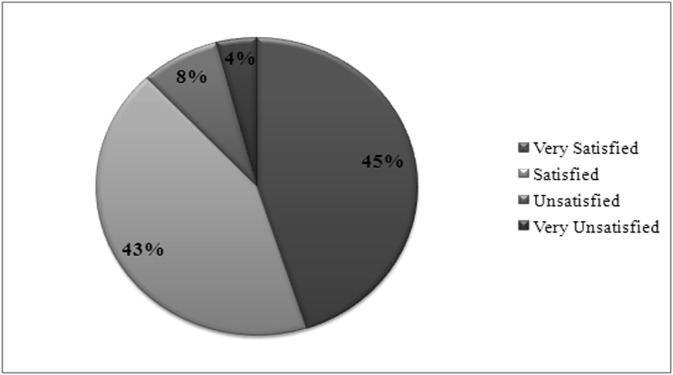
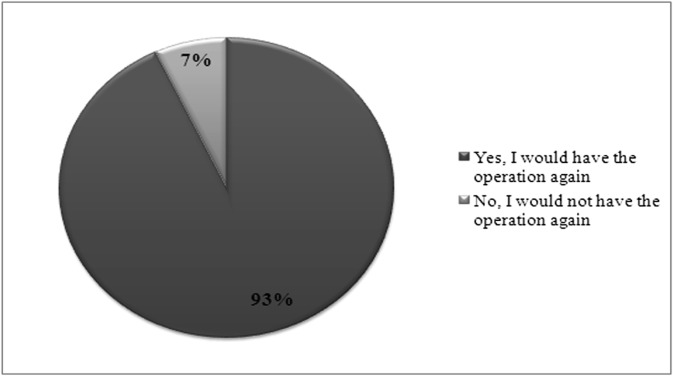
Before LESS fundoplication, patients reported both the frequency and severity of their reflux symptoms (Figure 3). Heartburn was particularly severe among all patients. At last follow-up, patients across all cohorts reported dramatic palliation of symptom severity and frequency (Figure 4). In addition, symptoms after fundoplication were not notable (Figure 4). In our study 88% of patients reported that they were satisfied or very satisfied with their experience (Figure 5) and 93% reported that they would undergo the operation again, knowing what they know now (Figure 6).
Figure 3.
Patients scored the frequency and severity of reflux symptoms before undergoing LESS fundoplication.
Figure 4.
Patients scored the frequency and severity of reflux symptoms preoperatively (preop) and postoperatively (postop). An asterisk indicates that a score was significantly lower after LESS fundoplication (P < .05).
Figure 5.
Patients scored their satisfaction after LESS fundoplication.
Figure 6.
Patients were asked if they would undergo LESS fundoplication again, given what they know now.
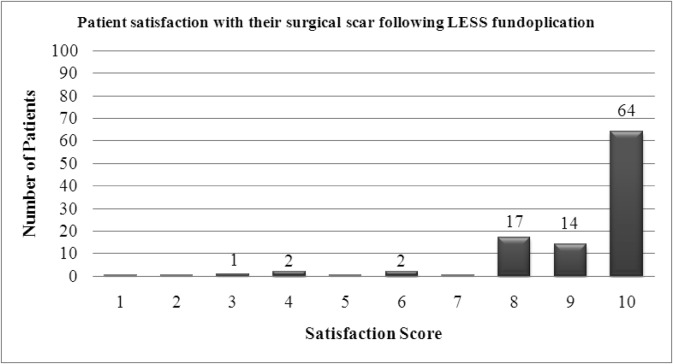
Patients who underwent LESS fundoplication scored the cosmesis of their umbilical incision as 10 (mean, 9 ± 1.3); 78% of patients scored their umbilical incision as 9 or 10, and 95% scored their incision as 8 or better (Figure 7).
Figure 7.
Satisfaction score of cosmetic outcome after LESS fundoplication.
DISCUSSION
Advancements in operative techniques can be described by a learning curve. A typical learning curve involves an initial period of slow acquisition of competence followed by a rapid acquisition of competence that reflects adaptation and standardization, resulting in proficiency with a new technique. LESS fundoplication is a moderately complex laparoscopic operation through a single-port entry. Despite the increased technical difficulties, relative to conventional laparoscopy associated with the LESS approach, our study indicates that advanced laparoscopic skills are transferable to LESS surgery and that proficiency with LESS fundoplication can be safely achieved in a short time with patient safety and satisfaction. In this study we document that the salutary and personal (eg, cosmetic) benefits of LESS surgery are safely and generally expeditiously applicable to fundoplication.
Our study involved the experiences of two surgeons over the course of <2 years in the first 100 consecutive patients undergoing LESS fundoplication for the treatment of GERD. Patients were divided into 4 cohorts of 25 patients each. As a group, they reflect Americans with reflux disease as described by their age, gender, and BMI; the severity of their reflux symptoms; and their abnormal DeMeester scores. We measured operative times, use of additional trocars, intraoperative complications, postoperative complications, and patient satisfaction to reflect parameters of proficiency and define our learning curve for LESS fundoplication.
Given that the operations were undertaken safely and efficaciously, the single most important variable that defined acquiring proficiency—thus our learning curve for LESS fundoplication—was the use of additional trocars through additional incisions. There was a significant decrease in the number of additional trocars used after the first 25-patient quartile. The utilization of additional trocars fell from most operations in the first cohort (ie, 2 of 3) down to some operations in the second cohort of patients (ie, nearly 1 of 3) to essentially no patients in the latter half of the patients. This rapid period of acquisition of competence in the second cohort suggests that the proficiency with LESS fundoplication has occurred by the beginning of the third quartile. Herein, lies our learning curve for LESS fundoplication. These results parallel other previously reported learning curves, for example, our learning curve with LESS cholecystectomy.13,14
In our analysis of the data, the operative times did not differ significantly and remained relatively constant throughout all cohorts of patients undergoing LESS fundoplication. This can be explained by knowing that, as proficiency was obtained during the early cohorts, we took on more challenging operations such as redo operations in the latter cohorts. Operations lasted on average 154 minutes. Although this seems long, generally, the operative times are shorter now as our experience continues. We try to avoid long operations by adding additional trocars when progress is slow or nil. The use of additional trocars proved to be independent of operative times, although the number of additional trocars decreased with each cohort of patients. Presumably, early in our experience, additional trocars saved time. The additional trocar placements should not be considered a “complication” of LESS fundoplication because traditional laparoscopic antireflux operations in comparison typically involve 5 port placements through 5 distant incisions. Placement of additional trocars/incisions when necessary shows “good judgment,” not “failure,” and should be encouraged when exposure is compromised, given that safety is of utmost importance.
What did we learn as we moved along our learning curve? What techniques and instrumentation did we adopt or abandon? We used either bipolar or ultrasonic energy devices and have no preference. With our initial experience, we used adjunctive sutures to facilitate exposure. These were generally abandoned as superfluous. Adjuncts, such as the EndoGrab, are uncommonly used but are helpful in patients with excessive intraperitoneal fat. A roticulating instrument (eg, Roticulator Locking Grasper; Covidien), however, was helpful in accomplishing triangulation, reducing instrument clashing in the operative field, assisting in bringing the posterior fundus behind the esophagus, and holding the posterior fundus while the fundoplication was constructed. We use this instrument as needed and not often. Suturing became easier with experience. We used a 5-mm conventional laparoscopic needle holder and polyester suture on a ski needle or a 10-mm Endo Stitch based on surgeon preference. With time, we used the latter less often. The Endo Stitch is easier to use but requires a 10-mm trocar. In sum, we undertook LESS fundoplication much like we had undertaken conventional multi-incision laparoscopic fundoplication, without superfluous “fancy” or expensive instruments. That said, a 5-mm deflectable-tip laparoscope is a necessity. With LESS fundoplication, our operative goals were always the same as with conventional laparoscopy. Given this, we should expect the outcomes of LESS fundoplication to be similar to, and as excellent as, those of conventional laparoscopic fundoplication.10,15 That is what we achieved.
Going forward, who receives additional trocars? Very few patients do. However, a giant hiatal hernia presents special problems occasionally, and if progress is slow or exposure is suboptimal, then an additional trocar is placed high along the anterior axillary line. This trocar helps with exposure.
LESS fundoplication represents a paradigm shift in minimally invasive surgery for the treatment of GERD. However, currently, there are essentially no published data regarding this innovative approach for antireflux operations. Similar studies were performed to document the learning curve for the LESS approach with different operations, most notably in cholecystectomy, with favorable outcomes and few complications. In this study complications seen with LESS fundoplication were inconsequential, limited, and infrequent, and LESS fundoplication, herein, showed a safety profile similar to the conventional laparoscopic approach. Our outcomes mirror established complication rates with conventional laparoscopic fundoplication, with relatively limited clinical significance. After the operation, patients across all cohorts reported similar and salutary results in amelioration of the frequency and severity of symptoms. Patient satisfaction with the operative scar was also high. More than 9 of 10 patients stated that they would undergo LESS fundoplication again, knowing what they know now. These patients will continue to be followed up by us annually with questionnaires and esophagogastroduodenoscopy/Bravo pH monitoring as necessary. The latter is difficult to obtain because the patients are doing well and decline to be tested.
This study represents the work, and the learning curve, of two surgeons who work closely together. However, their work and the learning curve with LESS fundoplication are inextricably related because of close collaboration, collaborative learning processes, and shared operative experiences. Therefore, this study ultimately translates into one learning curve. It can be argued that for one experienced laparoscopic surgeon, the learning curve might be faster. However, there is much to be gained from close collaboration and collaborative learning. Notably, the learning curve herein is occurring after a very considerable experience with conventional laparoscopic fundoplication. Duplication of this learning curve would require prerequisite basic and advanced “conventional” laparoscopic skills, including suturing and knot tying. Surgeon experience is important, as has been documented in studies for proficiency of many operations including conventional laparoscopic fundoplication. Surgeon experience with antireflux surgery has been linked to better outcomes after fundoplication.8 In our opinion, proficiency with conventional laparoscopic fundoplication is a “must” before one embarks on LESS fundoplication. In addition, further training with LESS courses administered by experienced LESS surgeons, simulation programs, and proctorships may shorten the learning curve and thereby improve proficiency.
Is this approach applicable for patients with pre-existing scars or those without apparent concerns for cosmesis? We have several thoughts. First, all patients care somewhat. Second, conventional laparoscopy is a huge advance over open surgery and is well tolerated and quite cosmetically acceptable. However, the LESS approach is better than a conventional laparoscopic approach, certainly for cosmesis. Third, only by applying this approach will proficiency be attained so that the approach is in each surgeon's armamentarium for safe and expeditious application. Every surgeon will have a learning curve. Only by applying the LESS approach will surgeons move along the learning curve. Without application in patients without specific concerns of cosmesis, application may be too infrequent to be perfected for patients with great concerns about cosmesis. Thereby, we use the LESS approach in all of our foregut surgical procedures, including fundoplication.
Does LESS fundoplication live up to its billing? Patients gave high scores regarding their umbilical scars. However, not all scores were high. We have learned that it is important that discussions about scarring occur preoperatively. Postoperatively, the umbilicus might look fine, just different, and for cosmetically concerned or focused patients, such a difference might be disappointing. However, for those focused patients, the conventional alternative is the same, or essentially the same, umbilical incision plus 4 other incisions, albeit small. For these patients, the LESS approach is strongly preferred.
From our experiences, LESS fundoplication can be completed safely and efficiently with amelioration of symptoms of GERD equivalent to after conventional laparoscopic fundoplication but with superior cosmesis. Surgeons will need to meet the increased demand for advanced minimally invasive surgical techniques used in LESS surgery with associated superior cosmetic results. Our study documents that the learning curve for LESS fundoplication is definable, short, and safe.
Contributor Information
Sharona B. Ross, Florida Hospital Tampa, Tampa, FL, USA..
Edward Choung, Florida Hospital Tampa, Tampa, FL, USA..
Anthony F. Teta, Florida Hospital Tampa, Tampa, FL, USA.
Lotiffa Colibao, Florida Hospital Tampa, Tampa, FL, USA..
Kenneth Luberice, Florida Hospital Tampa, Tampa, FL, USA..
Harold Paul, Florida Hospital Tampa, Tampa, FL, USA..
Alexander S. Rosemurgy, Florida Hospital Tampa, Tampa, FL, USA..
References
- 1. Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500–1511 [DOI] [PubMed] [Google Scholar]
- 2. Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Peters JH. Laparoscopic treatment of gastroesophageal reflux disease and hiatal hernia. In: Scott-Conner CEH, ed. The SAGES Manual: Fundamentals of Laparoscopy, Thoracoscopy, and GI Endoscopy. New York, NY: Springer; 2006:208–224 [Google Scholar]
- 4. Vesper BJ, Altman KW, Elseth KM, et al. Gastroesophageal reflux disease (GERD): is there more to the story? ChemMedChem. 2008;3:552–559 [DOI] [PubMed] [Google Scholar]
- 5. Elakkary E, Duffy A, Roberts K, Bell R. Recent advances in the surgical treatment of achalasia and gastroesophageal reflux disease. J Clin Gastroenterol. 2008;42:603–609 [DOI] [PubMed] [Google Scholar]
- 6. Hinder R, Filipi C, Wetscher G, Neary P, DeMeester T, Perdikis G. Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg. 1994;220:472–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Flum DR, Koepsell T, Heagerty P, Pellegrini CA. The nationwide frequency of major adverse outcomes in antireflux surgery and the role of surgeon experience, 1992 to 1997. J Am Coll Surg. 2002;195:611–618 [DOI] [PubMed] [Google Scholar]
- 8. Watson DI, Baigrie RJ, Jamieson GG. A learning curve for laparoscopic fundoplication: definable, avoidable, or a waste of time? Ann Surg. 1996;224:198–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Voitk A, Joffe J, Alvarez C, Rosenthal G. Factors contributing to laparoscopic failure during the learning curve for laparoscopic Nissen fundoplication in a community hospital. J Laparoendosc Adv Surg Tech A. 1999;9:243–248 [DOI] [PubMed] [Google Scholar]
- 10. Ross SB, Villadolid D, Paul H, et al. Laparoscopic Nissen fundoplication ameliorates symptoms of reflux, especially for patients with very abnormal DeMeester scores. Am Surg. 2008;74:635–642 [PubMed] [Google Scholar]
- 11. Stroup SP, Bazzi W, Derweesh IH. Training for laparoendoscopic single-site surgery and natural orifice transluminal endoscopic surgery. BJU Int. 2010;106:934–940 [DOI] [PubMed] [Google Scholar]
- 12. D'Alessio MJ, Rakita S, Bloomston M, et al. Esophagography predicts favorable outcome after laparoscopic Nissen fundoplication for patients with esophageal dysmotility. J Am Coll Surg. 2005;201:335–342 [DOI] [PubMed] [Google Scholar]
- 13. Hernandez J, Ross S, Morton C, et al. The learning curve of laparoendoscopic single site (LESS) cholecystectomy: definable, short, and safe. J Am Coll of Surg. 2010;211:652–657 [DOI] [PubMed] [Google Scholar]
- 14. Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS. Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg. 2009;75:681–685 [PubMed] [Google Scholar]
- 15. Cowgill S, Gillman R, Kraemer E, Al-Saadi S, Villadolid D, Rosemurgy A. Ten-year follow-up after laparoscopic Nissen fundoplication for GERD. Am Surg. 2007;73:748–752 [PubMed] [Google Scholar]