This study emphasizes the importance of careful preoperative imaging and select port positions appropriate for the targeted organ in patients with situs inversus undergoing laparoscopic surgery.
Keywords: Laparoscopic surgery, Adrenalectomy, Situs inversus
Abstract
Background:
Situs inversus is a relatively rare congenital disease. A patient with a right adrenal tumor complicated by total situs inversus was treated by laparoscopy.
Case Discussion:
The patient was a 45-y-old male with lower limb weakness. He had been diagnosed with situs inversus during a general health check-up as an infant. His blood pressure was 230/160 mm Hg, and the serum potassium level was 2.0 mEq/L. Abdominal ultrasonography and magnetic resonance imaging showed a mass of about 2cm in diameter in contact with the right adrenal gland. Total situs inversus was simultaneously confirmed. The plasma aldosterone concentration was elevated to 442pg/mL, and renin activity was suppressed, at 0.3ng/mL/hr.
Discussion:
These findings indicated a diagnosis of primary aldosteronism due to an adrenal tumor, and the right adrenal tumor was resected laparoscopically. The right adrenal gland was approached and resected from the lateral side of the spleen, which was located on the right side because of situs inversus. The resected specimen was 4.5cm×1.6cm, and no intraoperative complications occurred. The histopathological examination showed the tumor to be an aldosterone-producing adrenocortical adenoma.
INTRODUCTION
Situs inversus is a congenital condition in which part or all viscera are placed in mirror image to their normal orientations.1–3 It is a relatively rare disease, with an incidence of 1 in 4,000 to 10,000 people. It has no clinical significance per se but may affect surgical procedures.4,5 Situs inversus causes difficulty in surgical maneuvers due to complicating anomalies and anatomical irregularities. This report presents the case of a patient with a right adrenal tumor complicated by total situs inversus that was treated with laparoscopic adrenalectomy.
CASE REPORT
The patient was a 45-y-old male with lower limb weakness. He had been diagnosed with situs inversus on a general health check-up as an infant. He became aware of lower limb weakness, consulted a local physician, and was referred to the hospital for close examination and treatment because hypertension and hypokalemia were noted. The patient's height was 170.0cm, body weight 67.4 kg, blood pressure 230/160 mm Hg, and no abnormality was noted in the abdomen. The serum potassium level was 2.0 mEq/L (3.8 to 5.1 mEq/lL, the plasma aldosterone concentration was 442 pg/mL (39 to 307pg/mL), and the renin activity was 0.3ng/mL/hr (0.3 to 5.4ng/mL/hr), thus indicating hyperaldosteronism.
Plain chest X-ray showed dextrocardia, and no abnormality was observed in the lung field (Figure 1). Abdominal ultrasound findings confirmed situs inversus and detected a mass of about 2cm in diameter in contact with the right adrenal gland (Figure 2A). CT also confirmed situs inversus, and detected a mass of about 2cm in diameter in contact with the right adrenal gland (Figure 2B). Magnetic resonance imaging (MRI) confirmed situs inversus and identified a mass of about 2cm in diameter in contact with the right adrenal gland. MRI findings showed the mass as a low-signal intensity area on T1-weighted imaging and a nearly isosignal intensity area in comparison to fat (Figure 2C) on T2-weighted imaging.
Figure 1.

Plain chest X-ray findings. Dextrocardia was noted. No abnormality was observed in the lung field.
Figure 2.
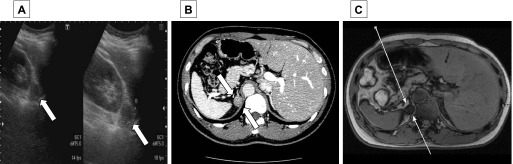
Abdominal ultrasound findings (A), CT findings (B), and MRI findings (C). Situs inversus was confirmed, and a mass of about 2cm in diameter in contact with the right adrenal gland was detected.
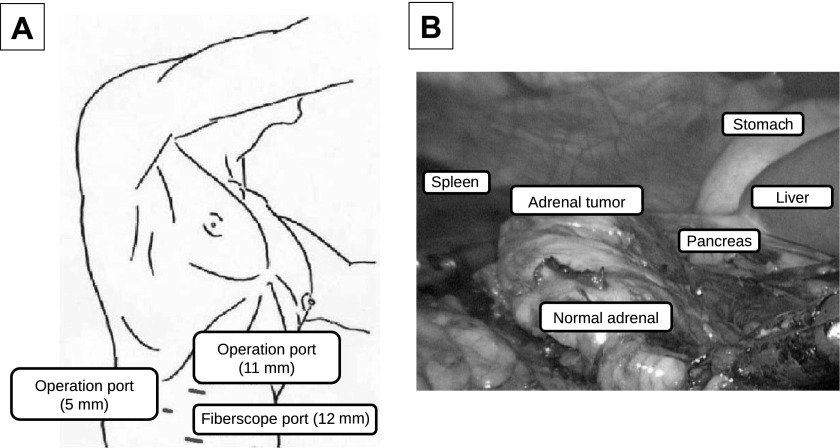
Angiography or scintigraphy could not be performed due to an allergy to iodine. The condition was diagnosed as primary aldosteronism due to adenoma of the right adrenal tumor, and the tumor was resected by laparoscopy. Surgery was started with the patient under general anesthesia by placing the patient in the left lateral recumbent position. A transverse incision about 12 mm in length was made at the umbilical level on the right midclavicular line, a port device for the laparoscope was inserted, and the abdominal cavity was examined. The spleen was in the right subphrenic space because of situs inversus, and the liver was in the left subphrenic space. Ports of 11 mm and 5 mm in diameter were inserted on the right midclavicular line 3 fingerbreadths below the right costal margin, and slightly to the right and above the laparoscopic port, respectively (Figure 3a). The right adrenal gland was approached from the lateral side of the spleen, which was located on the right side due to situs inversus (Figure 3b). Gerota's fascia was incised, and the adrenal gland was detached from the surrounding tissues. The feeding artery was divided after double clipping, and an adrenal tumor about 2cm in diameter was resected by using Multifire Endo GIA30 (Covidien, USA). The operation time was 1 h and 23 min, without any intraoperative complications. The intraoperative blood loss was estimated to be about 10 mL.
Figure 3.
Surgical findings. (A) We made 3 laparoscopic ports on the right lateral abdomen. (B) The right adrenal gland was located on the right side due to situs inversus.
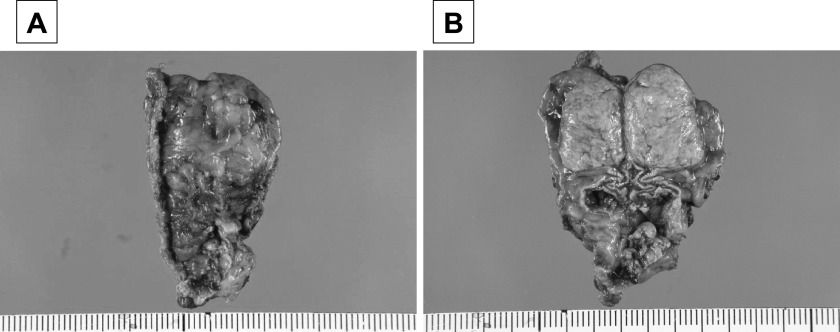
The resected adrenal gland was 4.5cm×1.6cm, the tumor was 2cm in diameter, and no gross extracapsular invasion was found (Figure 4). The histopathological examination revealed an adrenocortical adenoma with an aldosterone-producing tumor. The postoperative course was uneventful, and both hypertension and hypokalemia were completely resolved.
Figure 4.
Resected specimen. The resected specimen measured 4.5cm×1.6cm, the tumor was about 2cm in diameter, and no gross extracapsular invasion was found.
DISCUSSION
Situs inversus is a condition in which the positions of the thoracic and abdominal organs are laterally transposed, in mirror image of their normal positions; it is observed in 1 per 4,000 to10,000 people.1–3 Situs inversus may be total, thereby presenting inversion of all organs, as in this patient, or partial, with inversion of some organs; the incidence of total situs inversus is about 5 times higher than partial situs inversus. While situs inversus itself has no clinical significance, complicating congenital anomalies, particularly cardiovascular anomalies, are observed about 10 times more frequently than among the normal population.6 Situs inversus causes difficulty in surgical maneuvers due to such complicating anomalies and anatomical irregularities. A number of published reports describe surgery in patients with situs inversus, including those with stomach7 and colon cancer,5,8 but none report on surgery for an adrenal tumor or laparoscopic surgery. Other reports present the difficulty in the intraoperative determination of anatomical orientations. Therefore, sufficient comprehension of the anatomy around the surgical field by preoperative imaging studies was particularly important. In addition, laparoscopic surgery could be performed without problem by placing the port positions in a mirror image of their normal locations.
Laparoscopic adrenalectomy has already been established as a standard treatment for benign adrenal tumors due to its safety and minimal invasiveness.9,10 Many report that laparoscopic surgery is advantageous as compared with conventional laparotomy, due to lower invasiveness, shortened hospitalization period, and fewer safety problems.11,12 While laparoscopic surgery allows detailed observation in a magnified visual field, it is difficult to maintain spatial orientations or determine positional relationships between structures, because of the lack of landmarks such as organs in the narrow visible field.12
It is important to pay attention to the presence or absence of complicating anomalies, to carefully interpret preoperative imaging studies, and to select appropriate port positions for the targeted organ positions before laparoscopic surgery for patients with situs inversus. This report presented a successful laparoscopic surgery for a rare instance of right adrenal adenoma in a patient with total situs inversus.
Contributor Information
Shinichiro Kashiwagi, Department of Surgical Oncology, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka, Japan..
Tetsuro Ishikawa, Department of Surgical Oncology, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka, Japan..
Naoyoshi Onoda, Department of Surgical Oncology, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka, Japan..
Hidemi Kawajiri, Department of Surgical Oncology, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka, Japan..
Tsutomu Takashima, Department of Surgical Oncology, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka, Japan..
Kosei Hirakawa, Department of Surgical Oncology, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka, Japan..
References:
- 1. Zelikovsky A, Vidne B, Levy MJ. Mirror-image dextrocardia with situs inversus and coarctation of the aorta. Chest. 1974;66:297–299 [DOI] [PubMed] [Google Scholar]
- 2. Southam JA. Left-sided gallbladder: calculous cholecystitis with situs inversus. Ann Surg. 1975;182:135–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goi T, Kawasaki M, Yamazaki T, et al. Ascending colon cancer with hepatic metastasis and cholecystolithiasis in a patient with situs inversus totalis without any expression of UVRAG mRNA: report of a case. Surg Today. 2003;33:702–706 [DOI] [PubMed] [Google Scholar]
- 4. Romano GG, Grande G, Romano F, Di Luna G, Musto LA, Saldutti L. [Laparoscopic cholecystectomy in situs viscerum inversus totalis: technical note]. G Chir. 2009;30:369–373 [PubMed] [Google Scholar]
- 5. Fujiwara Y, Fukunaga Y, Higashino M, et al. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol. 2007;3:5035–5037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Czeizel A. Familial situs inversus and congenital heart defects. Am J Med Genet. 1987;28:227–228 [DOI] [PubMed] [Google Scholar]
- 7. Yamaguchi S, Orita H, Yamaoka T, Mii S, Sakata H, Hashizume M. Laparoscope-assisted distal gastrectomy for early gastric cancer in a 76-year-old man with situs inversus totalis. Surg Endosc. 2003;17:352–353 [DOI] [PubMed] [Google Scholar]
- 8. Greene QJ, Cheadle WG. Ascending colon cancer in a patient with situs inversus. Am Surg. 2007;73:831–832 [PubMed] [Google Scholar]
- 9. Guazzoni G, Cestari A, Montorsi F, et al. Laparoscopic treatment of adrenal diseases: 10 years on. BJU Int. 2004;93:221–227 [DOI] [PubMed] [Google Scholar]
- 10. Meria P, Kempf BF, Hermieu JF, Plouin PF, Duclos JM. Laparoscopic management of primary hyperaldosteronism: clinical experience with 212 cases. J Urol. 2003;169:32–35 [DOI] [PubMed] [Google Scholar]
- 11. Lin Y, Li L, Zhu J, Qiang W, Makiyama K, Kubota Y. Experience of retroperitoneoscopic adrenalectomy in 195 patients with primary aldosteronism. Int J Urol. 2007;14:910–913 [DOI] [PubMed] [Google Scholar]
- 12. Strebel RT, Muntener M, Sulser T. Intraoperative complications of laparoscopic adrenalectomy. World J Urol. 2008;26:555–560 [DOI] [PubMed] [Google Scholar]