Abstract
Exenatide has been widely used for the treatment of type 2 diabetes mellitus. However, its short plasma half-life of 2.4 hours has limited its clinical application. The exenatide products on the market, twice-daily Byetta™ and once-weekly Bydureon™ (both Amylin Pharmaceuticals, San Diego, CA, USA), are still not perfect. Many researchers have attempted to prolong the acting time of exenatide by preparing sustained-release dosage forms, modifying its structure, gene therapies, and other means. This review summarizes recent advances in long-acting exenatide preparations.
Keywords: exendin-4, diabetes mellitus type 2, sustained release, long acting, extended release, microsphere
Introduction
Diabetes is a common chronic disease in modern society, thus the development of antidiabetic drugs and relevant formulations are of prime importance.1–3 It is widely accepted that type 2 diabetes mellitus is caused by a genetic defect in leptin signaling, which leads to low sympathetic activity. A reduced level of sympathetic activity can result in decreased fatty acid oxidation, leading to excess insulin secretion. Thus, related cells become insulin resistant as a protective mechanism. Insulin resistance can be overcome by increasing insulin levels via direct or indirect methods.4,5
“Exenatide” is an incretin mimetic, a synthetic form of the naturally occurring exendin-4 isolated from the saliva of the Gila monster (Heloderma suspectum). It is a 39-amino acid peptide, which shares 53% of its amino acid sequence identity with human glucagon-like peptide-1 (GLP-1), and both have common glucoregulatory actions. As a potent agonist of the GLP-1 receptor, exenatide has been widely used as an adjunctive therapy to improve glycemic control in type 2 diabetes mellitus patients who are unable to achieve adequate glucose control using metformin and/or sulfonylurea.6–9 Exenatide was approved by the US Food and Drug Administration (FDA) on April 28, 2005, marketed as Byetta™ (Amylin Pharmaceuticals, San Diego, CA, USA).10
The pharmacology of exenatide is related to a combination of mechanisms that may include glucose-dependent stimulation of insulin secretion, suppression of glucagon secretion, enhancement of beta-cell mass, slowing of gastric emptying, inhibition of food intake, and modulation of glucose trafficking in peripheral tissues.11,12 However, its detailed mechanism of action remains under study.
Exenatide only has a short plasma half-life of 2.4 hours and an action time of about 8 hours.13 The clinical use of exenatide in its Byetta form is subcutaneous injection twice daily. As is known, daily injection causes pain and inconvenience in patients with a chronic disease such as diabetes. Further, the fluctuation of drug plasma concentration may also aggravate side effects such as sour stomach, diarrhea, heartburn, indigestion, belching, nausea, and vomiting.
Much effort has been put into obtaining a longer action time by structure modification, sustained-release dosage forms, or gene therapies. The resultant long-acting dosage forms of exenatide show priorities such as better patient compliance and a stable blood concentration which minimizes side effects. Long-acting release is also called “sustained release” (SR) or “extended release.”13
This review summarizes the recent advances in the area of long-acting dosage forms of exenatide.
Microspheres
Microspheres are a stable and seasoned way of achieving SR for peptides such as exenatide (Table 1).14–16 The safety, reliability, and efficiency of microspheres have been well established over the years. Currently, the only long-acting exenatide product on the market in microsphere form is Bydureon™ (Amylin Pharmaceuticals).
Table 1.
Summary of long-acting exenatide preparations
| Preparation method | SR period/Half-life | Advantage(s) | Disadvantage(s) |
|---|---|---|---|
| Microsphere | • Technology is mature • Easy to adjust SR period |
• Usually requires subcutaneous injection | |
| PLGA microsphere | 5–30 d; mostly 30 d | • PLGA is biocompatible and biodegradable • Approved by FDA |
|
| Polysaccharide microsphere | 21 d | • Better encapsulation rate than PLGA microspheres | • Relatively elevated inflammation compared with PLGA microspheres |
| Phase-transition gel in situ | Several days to 360 d | • Use of organic solvent avoided • Easy to prepare |
• Severe initial burst in the phase-transition process |
| Implantable device | 21 d | • Avoidance of severe initial burst that is found with phase-transition gel | • Usually surgery is required to implant the device |
| Structure modification | • Well established and versatile strategy to attain desired properties | • Relatively short SR time • High cost • Safety and efficiency of new molecules need to be evaluated |
|
| PEGylation | 43 h | • Reduces the immunogenicity | • Yields complex product mixtures • Harmful to kidneys |
| Introduction of a lysine residue | 40 h | • Decreases the degradation by metabolic enzymes | • Lack of detailed data in vivo |
| Recombinant polypeptide exenatide-XTEN | 139 h | • XTEN technology can be universal to peptides and proteins | • Sophisticated |
| Conjugation with hyaluronate | 96 h | • High bio-conjugation efficiency to hyaluronate of 90% | • Slight reduction of insulinotropic activity |
| Conjugation with acid (lauric, palmitic, lithocholic) | 4–20 h | • Slight reduction of cell viability | |
| PLGA microparticles | 7 d | • Pulmonary delivery |
Notes: For sustained-release (SR) preparations, the SR time is given; for structurally modified molecules, the plasma half-life is given. Data presented are based on the literature cited in this review; the same technologies may result in different data in other research.
Abbreviations: d, days; FDA, US Food and Drug Administration; h, hours; PEG, polyethylene glycol; PLGA, poly(lactic-co-glycolic acid); XTEN, half-life extension technology.
The drug is loaded onto the surface of or into the microsphere, which then releases it as the matrix materials degrade. Peptides and proteins can be protected before release. The main application drawback of microspheres is that most microsphere products must be injected subcutaneously, which causes pain and can result in patient noncompliance.
Poly (lactic-co-glycolic acid) microspheres
Poly (lactic-co-glycolic acid) (PLGA) is the most common material from which microspheres are prepared and is approved by the FDA. The release profile of PLGA can be easily adjusted. A once-weekly PLGA microsphere injection – Bydureon, developed by Amylin Pharmaceuticals (Indianapolis, IN, USA) – was approved by the FDA on January 27, 2012. This once-weekly form and the twice-daily form of injection are currently the only two exenatide forms on the market.
The Bydureon microsphere is prepared based on Medisorb® microsphere technology (Alkermes plc). The water-in-oil (W/O) solvent evaporation method is employed. Exenatide is dissolved in a water phase then mixed with a dichloromethane solution containing PLGA. Following this, the W/O emulsion is sonicated for several minutes. After a coacervate formation process undertaken to form embryonic microspheres with silicone oil, the embryonic microspheres are transferred into a heptane/ethanol solvent mixture to harden them.17–19
The diameter of the microspheres is 0.06 mm and they have a typical pinched-raisin shape and dense surface layer. In comparative trials, compared with twice-daily exenatide, Bydureon microspheres improved hemoglobin A1c (HbA1c) and reduced fasting plasma glucose, with fewer gastrointestinal side effects, no increased risk of hypoglycemia and with similar reductions in bodyweight.8,20,21 Norwood et al carried out a 2-year trial to estimate the safety of exenatide once weekly in patients with type 2 diabetes mellitus treated with a thiazolidinedione alone or in combination with metformin. Their results showed coherent improvements in HbA1c and weight.21 Many other researchers have also proved the better efficiency and the reduction of side effects of this formulation over the twice-daily injection dosage form of exenatide.22–25
However, the release profiles of Bydureon microspheres show a “lag phase,” which is also seen in other microspheres of small peptides.26,27 Taking the Bydureon microsphere’s patent, for example, after a common initial burst in the first 2 days due to the loosely bound exenatide on the surface, the drug is not released until 2 weeks later, and it takes up to 7 weeks for complete release.16 The presence of this lag phase leads to poor pharmacokinetics and efficacy.
Other researchers have also investigated exenatide PLGA microspheres, aiming to develop a better formulation than the Bydureon microsphere. For instance, Shi et al investigated how the molecular weight of PLGA affects the properties of exenatide microspheres.28 Three different molecular weights were studied (10, 20, and 30 kDa,). Results showed that as molecular weight increased, encapsulation efficiency increased. PLGA with a molecular weight of 30 kDa could achieve a 78.1% ± 8.8% (mean ± standard deviation) encapsulation rate. 10kDa PLGA microsphere showed a severe initial burst, while the other two microspheres’ release lasted for 30 days, and their release profiles were similar to the Bydureon microsphere.
Kwak et al prepared a biweekly dosage formulation of exenatide microspheres by single-emulsion solvent evaporation using PLGA.29 Plasma exenatide, as well as plasma insulin, non-fasting blood glucose and HbA1c concentrations, and changes in food intake and bodyweight were evaluated in both Zucker diabetic fatty and Zucker diabetic fatty lean control rats. Compared with twice-daily administration of exenatide, this biweekly microsphere lowered non-fasting blood glucose and HbA1c concentrations more effectively.
Liu et al prepared a 1-monthly PLGA microsphere of exenatide by double-emulsion solvent evaporation method. The size of the prepared microspheres ranged from 5.8 to 13.6 μm. Its hypoglycemic efficiency was similar to that of twice-daily exenatide injection.30
Kim et al fabricated a porous PLGA microsphere loaded with palmityl-acylated exenatide for pulmonary delivery.31 The palmityl-acylation was to aid exenatide absorption onto the hydrophobic surface of PLGA microsphere. In vitro, the release results of exenatide indicated a more severe initial burst than palmityl-acylated exenatide because of the poor absorption of the microsphere. The palmityl-acylated exenatide showed SR over 5 days both in vitro and in vivo.
Polysaccharide microspheres
Yang et al prepared polysaccharide microspheres of exenatide by a water-in-oil-in-water (W1/O/W2) emulsion method with three different degrees of acetylation (0.8, 1.5, 2.3) of polysaccharide.32 The mean particle size of the microspheres was 35 to 110 μm. A higher degree of acetylation (2.3) showed higher encapsulation efficiency (90.3%). The SR lasted for 21 days, and the fact that there was no loss of the molecular weight of exenatide showed that the exenatide was well protected in the polysaccharide microspheres. However, the foreign body reaction and immune cell configurations indicated higher inflammation than that produced by traditional PLGA microspheres. Thus, the safety of polysaccharide microspheres still needs further investigation.
Phase-transition gel in situ
In recent years, the phase-transition hydrogel in situ system has been used as an alternative SR delivery system for peptides and proteins. It is easy to prepare, can avoid the use of organic solvents, and achieves better patient compliance due to the longer dosing intervals than traditional dosage forms. These preparations are usually in solution form and, once injected into the body, change into hydrogels due to the change of temperature, pH, or electric field. However, the concurrence of the phase-transition process and release process may lead to a severe initial burst, which can be perilous to patients. Phase-transition gels are less durable compared with microspheres and the biocompatibility of the materials still needs to be determined.33–35
Li et al prepared a 1-week-release exenatide hydrogen with a triblock copolymer, PLGA-poly (ethylene glycol)-PLGA (PLGA-PEG-PLGA).36 The triblock copolymer was dissolved in deionized water then exenatide, zinc acetate, PEG 200 and/or sucrose were mixed with the copolymer solution. This mixed, drug-containing solution would turn into a hydrogel in situ at body temperature after being injected. SR over 1 week was realized with an acceptable initial burst and almost complete release. The hydrogel matrix also enhanced the stability of the drug significantly. In a mouse experiment in vivo, steady blood glucose level was achieved for 1 week, proving its efficiency. This strategy of using synergistic excipients (zinc acetate, PEG 200, and sucrose) to reduce the early stage burst effect and enhance the late-stage release might also be of interest to developers of other SR preparations.
Joabsson et al invented a pre-formulation for the in situ generation compositions for the controlled release of glucagon-like-peptide-1 (GLP-1) and its analogs (including exenatide).37 This pre-formulation comprised a low viscosity mixture of: at least one neutral diacyl lipid and/or a tocopherol; at least one phospholipid; at least one biocompatible organic solvent; and 0.02 to 12 wt% of at least one GLP-1 analog. The pre-formulation is for parenteral delivery (such as subcutaneous injection). When the mixture is exposed to body fluid, a phase transition occurs and an SR hydrogel matrix is formed. The SR time can be adjusted within the range of several to 360 days.
Implantable device
The implantable device is an SR device that can achieve relatively stable release compared with phase-transition gel in situ due to the avoidance of the phase-transition process. However, usually surgery is needed for the subcutaneous implantation of the device, which leads to pain and patient reluctance to proceed with the implantation. The implantable device should act much longer than other preparations, showing its superiority.38,39
Kuzma et al invented an SR implantable device for exenatide.40 This device comprises a homogeneous copolymer matrix – which forms a hydrogel with an equilibrium moisture content value ranging from 20% to 85% – and a solid formulation of polypeptide. In an embodiment, the homogeneous copolymer matrix can be prepared with 2-hydroxyethyl methacrylate, ethylene glycol dimethacrylate, vitamin E, β-mercaptoethanol, and so on, while a typical solid formulation consists of 98% exenatide and 2% steric acid. The SR can be achieved for 21 days, which did not prevail much than other no surgical preparations.
Structure modification
Structure modification has been a successful strategy to attain desired properties that the original molecules do not possess. Longer half-life, higher stability, lower immunogenicity, fewer side effects, and greater water solubility can be achieved by the introduction of new groups, exchange of existing groups, interaction with biomolecules, cross-linking, and so on.41–44 The major obstacles are the cost of modification and the safety of the new molecules for drug use. Moreover, sometimes the process yields complex product mixtures.45
PEGylation
PEGylation is one of the most common methods used to increase the half-life of peptides or proteins, and it can reduce the immunogenicity by sterically shielding the conjugated protein and decrease the degradation by metabolic enzymes.46–48 However, PEGylation increases the cost, and may be harmful to the kidneys.49
Gong et al used maleimide-PEG to induce site-specific PEGylation.50 An analog, PB-105, was produced by replacing cysteine at position 39 of exenatide to provide a free thiol group. Then, at this site, PEGs of different molecular weights were grafted on. The effects of these on intracellular cyclic adenosine monophosphate (cAMP), acute glucoregulatory activity, and pharmacokinetic profile were compared in mice and rats. The results showed that PB-105 did not change the efficiency and half-life of exenatide. An analog of PB-105, PEGylated by 20 kDa PEG, had a plasma half-life of 43 hours, approximately tenfold that of PB-105, and exhibited glucoregulatory activity superior to that of PB-105 in normal and diabetic mice.50
Introduction of a lysine residue
Hansen and Lau prepared an exenatide compound to prolong its half-life.51 At the sequence position 20 or 38 of exenatide (Figure 1), an amino acid was replaced with a lysine residue, which then acylated with a diacid, such as a dicarboxylic acid. This new exenatide analog can increase the acting time to more than 40 hours.
Figure 1.
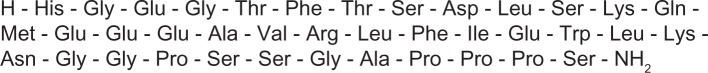
Sequence of exenatide.
Recombinant polypeptide exenatide-XTEN
Schellenberger et al extended the half-life of exenatide by fusing exenatide and XTEN.52 To create a genetically stable, highly expressed, unstructured polypeptide in Escherichia coli, they generated a library of non-repetitive 36-amino-acid segments comprising more than 1,500 kinds. The first expression level was screened, and highly expressed segments were iteratively ligated to obtain maximum expression, resulting in 864 amino acids. Following this, genetic stability, solubility, heat stability, aggregation resistance, and contaminant profile, including host-cell proteins, were taken into consideration, and the optimum sequence, named “XTEN,” was picked out.
They fused the 864-amino-acid XTEN sequence to the 3′ end of a synthetic gene encoding exenatide, which was in turn fused at its 5′ end to a gene encoding a Clostridium thermocellum cellulose-binding domain. The process of removing the cellulose-binding domain yielded the histidine of exenatide at the first amino acid position of the final protein, which is required for exenatide function. The fusion of exenatide and XTEN extended the half-life exenatide in humans from 2.4 hours to a predicted 139 hours.
Conjugation with hyaluronate
Kong et al also modified the structure of exenatide to address the problem of short plasma half-life.53 Vinyl sulfone-modified hyaluronate and thiolated exenatide were conjugated. In a db/db mouse experiment, the conjugation of hyaluronate-exenatide resulted in an ~20-fold improvement in half-life (achieving 96 hours) while maintaining the glucoregulatory efficiency of exenatide.
Conjugation with acid
Chae et al modified exenatide with acids to obtain a long-acting exenatide.54,55 As there are two lysine residues on exenatide, fatty acids (FA) (lauric acid [C12] and palmitic acid [PAA; C16]) and a bile acid (lithocholic acid [LCA]) can be conjugated with exenatide. Thus, a series of exenatide analogs was produced, including Lys12-FA-exenatide (FA-M2), Lys29-FA-exenatide (FA-M1), Lys12,29-diFA-exenatide (FA-Di), Lys12-LCA-exenatide (LCA-M2), Lys29-LCA-exenatide (LCA-M1), and Lys12,29-LCA-exenatide (LCA-Di). Their pharmacokinetic and pharmacologic properties were investigated. Results showed that affinity between the GLP-1 receptor and exenatide analogs was reduced slightly, so there was a corresponding reduction insulinotropic activity. The plasma half-life of these exenatide analogs was prolonged, ranging from ~4 to ~10 hours.
Lee et al evaluated pharmacokinetics and pharmacodynamics of PAA-conjugated exenatide (pal-exenatide).56 Molecular imaging showed that the subcutaneous absorption of pal-exenatide was delayed until 24 hours post-injection, whereas exenatide was rapidly absorbed and distributed systemically. The hypoglycemic degree of pal-exenatide was 4.2-fold greater than exenatide. In addition, the plasma half-life of pal-exenatide was about 20 hours, almost tenfold longer than that of exenatide.
Other preparations
Binding of exenatide to the surface of PLGA microparticles for pulmonary delivery
Pulmonary delivery is an eminent non-parenteral delivery method. It has better compliance, as it is a noninvasive method, and the huge absorption area of the lung (approximate 100 m2) can ensure high bioavailability for peptides and proteins.57,58
Kim et al combined the strategies of PLGA microparticles (MPs) and exenatide structure modification to prolong the release period.59 Porous PLGA MPs were prepared by W1/O/W2 double emulsification using hydroxypropyl-β-cyclodextrin and poly(ethylene-alt-maleic anhydride). Then albumin was covalently attached to the MPs by 1-(3-dimethylaminopropyl)-3-ethylcarbodiimide (EDC). Finally, palmityl-acylated exenatide was bound to the albumin surface. The porous PLGA MPs offered a low density for pulmonary delivery. Results showed that the MPs bound with palmityl-acylated exenatide demonstrated 5-day glucoregulatory efficiency, while those bound with unmodified exenatide only exhibited 2-day efficiency. The acute cytotoxicity of PLGA MPs on Calu-3 and A549 cells was evaluated after 48 hours, and it was found that cell viability was affected slightly.
Chewing gum tablet
Andersen et al invented a compressed chewing gum tablet which may prolong exenatide release slightly.60 This gum tablet contains elastomer, natural resin softener, polyvinyl acetate, and active components (such as exenatide in example 6 of the patent).60 Compared with the fast plasma half-life after injection (~2.4 hours), the chewing and release process with this preparation may prolong the acting time. However, as detailed release profiles and evaluations in vitro/in vivo are not given in the patent, the glucoregulatory efficiency remains doubtful.
Gene therapy
Kim et al developed an exenatide plasmid system as an alternative therapy.61 This gene therapy was constructed using the two-step transcription amplification system, which comprised pβ-Gal4-p65 and plasmid DNA system up-stream activating sequence (pUAS)-signal peptide (SP)-exenatide, combining the advantages of SP to facilitate its secretion in ectopic cells or tissue. Arginine-grafted cyctaminebisacrylamide-diaminohexane polymer (ABP) was employed as the gene carrier. Compared with 25K polyetherimide (PEI), the exenatide expression in the cells treated with 25K PEI/TSTA-SP-exenatide was 1.4-fold lower than that of cells treated with ABP/TSTA-SP-exenatide. The glucoregulatory effect of ABP/TSTA-SP-exenatide showed a long-acting mode, lasting from the third day post-injection to ~12 days post-injection.
Improvements to GLP-1
GLP-1 only has a short half-life of several minutes, thus some improvements to it are required before it can be applied as a drug. As GLP-1 shares with exenatide the same receptor and 50% of the amino acid sequences, strategies employed with GLP-1 are also helpful in improving exenatide.
Léger et al used their PC-DAC™ technology to develop a novel GLP-1 analog called “CJC-1131.”62 When conjugated with human serum albumin, this analog has a half-life 30-fold longer than that of exenatide. Amiram et al fabricated a protease-operated depots (PODs) gene to produce a delicately designed molecule comprising protease cleavable oligomers of GLP-1, and a thermally responsive, depot-forming elastin-like-polypeptide that undergoes a thermally triggered inverse phase transition in situ below body temperature.63 On injection into the body, it forms an SR matrix and the protease cleaves the linkages among the peptides, liberating GLP-1 into circulation. High-yield expression of the GLP-1 PODs gene was demonstrated in E. coli. Results showed a 5-day glucoregulatory effect in mice injected with the PODs.
“Liraglutide” is a fatty acid derivative of GLP-1 for type 2 diabetes treatment with one amino acid substitution (Arg34 Lys) and attached with a C16 PAA side chain via a glutamyl. These modifications result in longer acting time, allowing for a slower absorption from subcutaneous tissue, reversible albumin binding, and resistance to GLP-1 inactivation by dipeptidyl peptidase-4. Liraglutide has been developed as a once-daily treatment for type 2 diabetes (marketed as Victoza® [Novo Nordisk, Bagsværd, Denmark]) as an adjunctive therapy.64
Agersø et al investigated the safety, tolerability, pharmacokinetics, and pharmacodynamics in healthy male subjects following 7 days’ treatment with NN2211 (liraglutide).65 Results showed that liraglutide had a half-life of 12.6 ± 1.1 (mean ± standard deviation) hours and a higher incidence of adverse events relating to the gastrointestinal system.
Conclusion
Considering the important role exenatide plays in the treatment of type 2 diabetes mellitus, patients suffering from this chronic disease stand to benefit significantly from improvements to the acting period of exenatide. Both twice-daily Byetta and once-weekly Bydureon have some drawbacks, which is why researchers are continuing to work on improving exenatide preparations.
It is not so difficult to prolong the acting time of exenatide preparations with existing pharmaceutical technologies, through which the release period can be adjusted from several hours to nearly 1 year. For an ideal long SR preparation, a longer and stable release profile is desired, which means better compliance, safety, and fewer side effects. PLGA microspheres with an appropriate release time (such as 1 month) and smooth release profile (ie, release at a constant speed) are best for clinical application. Any new analog of exenatide with a longer plasma half-life stands to have a momentous impact once its safety and efficiency are confirmed, as these analogs can be applied independently or in combination with other SR strategies.
The trend in the area of long-acting preparations is universal technologies that can be applied to a series of proteins or peptides (such as XTEN technology) and in combination with gene therapies, we can achieve a once and for all therapeutic effect. Although many pertinent studies have been carried out in recent years, there is still a long way to go until we accomplish a new successful product for the market.
Acknowledgments
This study was supported by the Projects of National Science Foundation of China (81373366, 81071025 and 81171203) and Projects of the Shanghai Committee of Science and Technology, People’s Republic of China (11nm0503300, 11410708900, and 12XD1403800).
Footnotes
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.Khafagy el-S, Morishita M, Onuki Y, Takayama K. Current challenges in non-invasive insulin delivery systems: a comparative review. Adv Drug Deliv Rev. 2007;59(15):1521–1546. doi: 10.1016/j.addr.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 2.Jin Y, Song YP, Zhu X, et al. Goblet cell-targeting nanoparticles for oral insulin delivery and the influence of mucus on insulin transport. Biomaterials. 2012;33(5):1573–1582. doi: 10.1016/j.biomaterials.2011.10.075. [DOI] [PubMed] [Google Scholar]
- 3.Kendall DM, Riddle MC, Rosenstock J, et al. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylurea. Diabetes Care. 2005;28(9):1083–1091. doi: 10.2337/diacare.28.5.1083. [DOI] [PubMed] [Google Scholar]
- 4.McGarry JD. Banting lecture 2001: dysregulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes. 2002;51(1):7–18. doi: 10.2337/diabetes.51.1.7. [DOI] [PubMed] [Google Scholar]
- 5.Pories WJ, Albrecht RJ. Etiology of type II diabetes mellitus: role of the foregut. World J Surg. 2001;25(4):527–531. doi: 10.1007/s002680020348. [DOI] [PubMed] [Google Scholar]
- 6.Cvetkovic′ RS, Plosker GL. Exenatide: a review of its use in patients with type 2 diabetes mellitus (as an adjunct to metformin and/or a sulfonylurea) Drugs. 2007;67(6):935–954. doi: 10.2165/00003495-200767060-00008. [DOI] [PubMed] [Google Scholar]
- 7.Triplitt C, Chiquette E. Exenatide: from the Gila monster to the pharmacy. J Am Pharm Assoc (2003) 2006;46(1):44–55. doi: 10.1331/154434506775268698. [DOI] [PubMed] [Google Scholar]
- 8.Gentilella R, Bianchi C, Rossi A, Rotella CM. Exenatide: a review from pharmacology to clinical practice. Diabetes Obes Metab. 2009;11(6):544–556. doi: 10.1111/j.1463-1326.2008.01018.x. [DOI] [PubMed] [Google Scholar]
- 9.Eng J, Kleinman WA, Singh L, Singh G, Raufman JP. Isolation and characterization of exendin-4, an exendin-3 analogue, from Heloderma suspectum venom. Further evidence for an exendin receptor on dispersed acini from guinea pig pancreas. J Biol Chem. 1992;267(11):7402–7405. [PubMed] [Google Scholar]
- 10.Cure P, Pileggi A, Alejandro R. Exenatide and rare adverse events. N Engl J Med. 2008;358(18):1969–1972. doi: 10.1056/NEJMc0707137. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen LL, Young AA, Parkes DG. Pharmacology of exenatide (synthetic exendin-4): a potential therapeutic for improved glycemic control of type 2 diabetes. Regul Pept. 2004;117(2):77–88. doi: 10.1016/j.regpep.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 12.Kolterman OG, Buse JB, Fineman MS, et al. Synthetic exendin-4 (exenatide) significantly reduces postprandial and fasting plasma glucose in subjects with type 2 diabetes. J Clin Endocrinol Metab. 2003;88(7):3082–3089. doi: 10.1210/jc.2002-021545. [DOI] [PubMed] [Google Scholar]
- 13.Painter NA, Morello CM, Singh RF, McBane SE. An evidence-based and practical approach to using Bydureon™ in patients with type 2 diabetes. J Am Board Fam Med. 2013;26(2):203–210. doi: 10.3122/jabfm.2013.02.120174. [DOI] [PubMed] [Google Scholar]
- 14.Xiao L, Chen Q, Bao Y, Pan F. Release pattern improvement of nomegestrol from biodegradable microspheres by using polymer-alloys as matrix. Asian J Pharm Sci. 2010;5(6):231–238. [Google Scholar]
- 15.Jeyanthi R, Mehta RC, Thanoo BC, DeLuca PP. Effect of processing parameters on the properties of peptide-containing PLGA microspheres. J Microencapsul. 1997;14(2):163–174. doi: 10.3109/02652049709015330. [DOI] [PubMed] [Google Scholar]
- 16.Nikou KN, Stivaktakis N, Avgoustakis K, et al. A HER-2/neu peptide admixed with PLA microspheres induces a Th1-biased immune response in mice. Biochim Biophys Acta. 2005;1725(2):182–189. doi: 10.1016/j.bbagen.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Wright SG, Christenson T, Yeah TY, inventors, et al. Alkermes Inc, assignee Polymer-based sustained release device. Nov 1, 2008. United States patent US7456254 B2.
- 18.Li X, Li L, Wang X, Ren Y, Zhou T, Lu W. Application of model-based methods to characterize exenatide-loaded double-walled microspheres: in vivo release, pharmacokinetic/pharmacodynamic model, and in vitro and in vivo correlation. J Pharm Sci. 2012;101(10):3946–3961. doi: 10.1002/jps.23236. [DOI] [PubMed] [Google Scholar]
- 19.DeYoung MB, MacConell L, Sarin V, Trautmann M, Herbert P. Encapsulation of exenatide in poly-(D,L-lactide-co-glycolide) microspheres produced an investigational long-acting once-weekly formulation for type 2 diabetes. Diabetes Technol Ther. 2011;13(11):1145–1154. doi: 10.1089/dia.2011.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drucker DJ, Buse JB, Taylor K, et al. Exenatide once weekly versus twice daily for the treatment of type 2 diabetes: a randomised, open-label, non-inferiority study. Lancet. 2008;372(9645):1240–1250. doi: 10.1016/S0140-6736(08)61206-4. [DOI] [PubMed] [Google Scholar]
- 21.Norwood P, Liutkus JF, Haber H, et al. Safety of exenatide once weekly in patients with type 2 diabetes mellitus treated with a thiazolidinedione alone or in combination with metformin for 2 years. Clin Ther. 2012;34(10):2082–2090. doi: 10.1016/j.clinthera.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 22.Wysham C, Grimm M, Chen S. Once weekly exenatide: efficacy, tolerability and place in therapy. Diabetes Obes Metab. 2013 Feb 20; doi: 10.1111/dom.12084. [DOI] [PubMed] [Google Scholar]
- 23.Malone J, Trautmann M, Wilhelm K, et al. Exenatide once weekly for the treatment of type 2 diabetes. Expert Opin Investig Drugs. 2009;18(3):359–367. doi: 10.1517/13543780902766802. [DOI] [PubMed] [Google Scholar]
- 24.Murphy CE. Review of the safety and efficacy of exenatide once weekly for the treatment of type 2 diabetes mellitus. Ann Pharmacother. 2012;46(6):812–821. doi: 10.1345/aph.1Q722. [DOI] [PubMed] [Google Scholar]
- 25.Ridge T, Moretto T, Macconell L, et al. Comparison of safety and tolerability with continuous (exenatide once weekly) or intermittent (exenatide twice daily) GLP-1 receptor agonism in patients with type 2 diabetes. Diabetes Obes Metab. 2012;14(12):1097–1103. doi: 10.1111/j.1463-1326.2012.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang J, Wang BM, Schwendeman SP. Characterization of the initial burst release of a model peptide from poly (D, L-lactide-co-glycolide) microspheres. J Control Release. 2002;82(2):289–307. doi: 10.1016/s0168-3659(02)00137-2. [DOI] [PubMed] [Google Scholar]
- 27.Cleland JL. Solvent evaporation processes for the production of controlled release biodegradable microsphere formulations for therapeutics and vaccines. Biotechnol Progr. 1998;14(1):102–107. doi: 10.1021/bp970128t. [DOI] [PubMed] [Google Scholar]
- 28.Shi L, Liu B, Wang M, et al. Effect of molecular weight of poly(Lactic-co-Glycolide) on properties of exenatide-loaded microspheres. China Modern Medicine. 2009;7:117–118. [Google Scholar]
- 29.Kwak HH, Shim WS, Hwang S, et al. Pharmacokinetics and efficacy of a biweekly dosage formulation of exenatide in Zucker diabetic fatty (ZDF) rats. Pharm Res. 2009;26(11):2504–2512. doi: 10.1007/s11095-009-9966-3. [DOI] [PubMed] [Google Scholar]
- 30.Liu B, Dong Q, Wang M, et al. Preparation, characterization, and pharmacodynamics of exenatide-loaded poly(DL-lactic-co-glycolic acid) microspheres. Chem Pharm Bull (Tokyo) 2010;58(11):1474–1479. doi: 10.1248/cpb.58.1474. [DOI] [PubMed] [Google Scholar]
- 31.Kim H, Park H, Lee J, et al. Highly porous large poly(lactic-co-glycolic acid) microspheres adsorbed with palmityl-acylated exendin-4 as a long-acting inhalation system for treating diabetes. Biomaterials. 2011;32(6):1685–1693. doi: 10.1016/j.biomaterials.2010.10.045. [DOI] [PubMed] [Google Scholar]
- 32.Yang HJ, Park IS, Na K. Biocompatible microspheres based on acetylated polysaccharide prepared from water-in-oil-in-water (W1/O/W2) double-emulsion method for delivery of type II diabetic drug (exenatide) Colloids Surf A. 2009;340(1–3):115–120. [Google Scholar]
- 33.Hiemstra C, Zhou W, Zhong Z, Wouters M, Feijen J. Rapidly in situ forming biodegradable robust hydrogels by combining stereocomplexation and photopolymerization. J Am Chem Soc. 2007;129(32):9918–9926. doi: 10.1021/ja072113p. [DOI] [PubMed] [Google Scholar]
- 34.Vermonden T, Censi R, Hennink WE. Hydrogels for protein delivery. Chem Rev. 2012;112(5):2853–2888. doi: 10.1021/cr200157d. [DOI] [PubMed] [Google Scholar]
- 35.Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20(2):86–100. doi: 10.1016/j.smim.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li K, Yu L, Liu X, Chen C, Chen Q, Ding J. A long-acting formulation of a polypeptide drug exenatide in treatment of diabetes using an injectable block copolymer hydrogel. Biomaterials. 2013;34(11):2834–2842. doi: 10.1016/j.biomaterials.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 37.Joabsson FC, Johnsson MC, Tiberg FC, inventors, Camurus AB, Goddard C., applicants GLP-1 analogue formulations. Feb 20, 2008. European patent EP1888031 A1.
- 38.Leitch JW, Gillis AM, Wyse DG, et al. Reduction in defibrillator shocks with an implantable device combining antitachycardia pacing and shock therapy. J Am Coll Cardiol. 1991;18(1):145–151. doi: 10.1016/s0735-1097(10)80232-3. [DOI] [PubMed] [Google Scholar]
- 39.Wilkins E, Atanasov P, Muggenburg BA. Integrated implantable device for long-term glucose monitoring. Biosensors and Bioelectronics. 1995;10(5):485–494. doi: 10.1016/0956-5663(95)96894-5. [DOI] [PubMed] [Google Scholar]
- 40.Kuzma P, Decker S, Quandt H, inventors, Endo Pharmaceuticals Solutions Inc, assignee Sustained delivery of exenatide and other peptides. Nov 18, 2010. United State patent US 20100292144 A1.
- 41.Khandare J, Minko T. Polymer–drug conjugates: progress in polymeric prodrugs. Prog Polym Sci. 2006;31(4):359–397. [Google Scholar]
- 42.Laman AG, Shepelyakovskaya AO, Boziev KhM, et al. Structural modification effects on bioactivities of the novel 15-mer peptide adjuvant. Vaccine. 2011;29(44):7779–7784. doi: 10.1016/j.vaccine.2011.07.113. [DOI] [PubMed] [Google Scholar]
- 43.Rolin B, Larsen MO, Gotfredsen CF, et al. The long-acting GLP-1 derivative NN2211 ameliorates glycemia and increases beta-cell mass in diabetic mice. Am J Physiol Endocrinol Metab. 2002;283(4):E745–E752. doi: 10.1152/ajpendo.00030.2002. [DOI] [PubMed] [Google Scholar]
- 44.Pan CQ, Buxton JM, Yung SL, et al. Design of a long acting peptide functioning as both a glucagon-like peptide-1 receptor agonist and a glucagon receptor antagonist. J Biol Chem. 2006;281(18):12506–12515. doi: 10.1074/jbc.M600127200. [DOI] [PubMed] [Google Scholar]
- 45.Dhalluin C, Ross A, Leuthold LA, et al. Structural and biophysical characterization of the 40 kDa PEG-interferon-alpha2a and its individual positional isomers. Bioconjug Chem. 2005;16(3):504–517. doi: 10.1021/bc049781+. [DOI] [PubMed] [Google Scholar]
- 46.Kochendoerfer G. Chemical and biological properties of polymer-modified proteins. Expert Opin Biol Ther. 2003;3(8):1253–1261. doi: 10.1517/14712598.3.8.1253. [DOI] [PubMed] [Google Scholar]
- 47.Park EJ, Tak TH, Na DH, Lee KC. Effect of PEGylation on stability of peptide in poly(lactide-co-glycolide) microspheres. Arch Pharm Res. 2010;33(7):1111–1116. doi: 10.1007/s12272-010-0718-z. [DOI] [PubMed] [Google Scholar]
- 48.Veronese FM, Pasut G. PEGylation, successful approach to drug delivery. Drug Discov Today. 2005;10(21):1451–1458. doi: 10.1016/S1359-6446(05)03575-0. [DOI] [PubMed] [Google Scholar]
- 49.Bendele A, Seely J, Richey C, Sennello G, Shopp G. Short communication: renal tubular vacuolation in animals treated with polyethylene-glycol-conjugated proteins. Toxicol Sci. 1998;42(2):152–157. doi: 10.1006/toxs.1997.2396. [DOI] [PubMed] [Google Scholar]
- 50.Gong N, Ma AN, Zhang LJ, et al. Site-specific PEGylation of exenatide analogues markedly improved their glucoregulatory activity. Brit J Pharmacol. 2011;163(2):399–412. doi: 10.1111/j.1476-5381.2011.01227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hansen TK, Lau J, inventors, Novo Nordisk A/S., assignee Protracted exendin-4 compounds. Dec 8, 2011. United States patent US20110301084 A1.
- 52.Schellenberger V, Wang CW, Geething NC, et al. A recombinant polypeptide extends the in vivo half-life of peptides and proteins in a tunable manner. Nat Biotechnol. 2009;27(12):1186–1190. doi: 10.1038/nbt.1588. [DOI] [PubMed] [Google Scholar]
- 53.Kong JH, Oh EJ, Chae SY, Lee KC, Hahn SK. Long acting hyaluronate – exendin 4 conjugate for the treatment of type 2 diabetes. Biomaterials. 2010;31(14):4121–4128. doi: 10.1016/j.biomaterials.2010.01.091. [DOI] [PubMed] [Google Scholar]
- 54.Chae SY, Jin CH, Shin JH, et al. Biochemical, pharmaceutical and therapeutic properties of long-acting lithocholic acid derivatized exendin-4 analogs. J Control Release. 2010;142(2):206–213. doi: 10.1016/j.jconrel.2009.10.025. [DOI] [PubMed] [Google Scholar]
- 55.Chae SY, Choi YG, Son S, Jung SY, Lee DS, Lee KC. The fatty acid conjugated exendin-4 analogs for type 2 antidiabetic therapeutics. J Control Release. 2010;144(1):10–16. doi: 10.1016/j.jconrel.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 56.Lee J, Lee C, Kim I, et al. Preparation and evaluation of palmitic acid-conjugated exendin-4 with delayed absorption and prolonged circulation for longer hypoglycemia. Int J Pharm. 2012;424(1–2):50–57. doi: 10.1016/j.ijpharm.2011.12.050. [DOI] [PubMed] [Google Scholar]
- 57.Agu RU, Ugwoke MI, Armand M, Kinget R, Verbeke N. The lung as a route for systemic delivery of therapeutic proteins and peptides. Respir Res. 2001;2(4):198–209. doi: 10.1186/rr58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patton JS, Fishburn CS, Weers JG. The lungs as a portal of entry for systemic drug delivery. Proc Am Thorac Soc. 2004;1(4):338–344. doi: 10.1513/pats.200409-049TA. [DOI] [PubMed] [Google Scholar]
- 59.Kim H, Lee J, Kim TH, et al. Albumin-coated porous hollow poly(lactic-co-glycolic acid) microparticles bound with palmityl-acylated exendin-4 as a long-acting inhalation delivery system for the treatment of diabetes. Pharm Res. 2011;28(8):2008–2019. doi: 10.1007/s11095-011-0427-4. [DOI] [PubMed] [Google Scholar]
- 60.Andersen C, Lorenzen G, Arent N, Thorengaard B, Wittorff H., inventors and assignees Compressed chewing gum tablet. Oct 7, 2010. United States patent US20100255063 A1.
- 61.Kim PH, Lee M, Kim SW. Delivery of two-step transcription amplification exendin-4 plasmid system with arginine-grafted bioreducible polymer in type 2 diabetes animal model. J Control Release. 2012;162(1):9–18. doi: 10.1016/j.jconrel.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Léger R, Thibaudeau K, Robitaille M, et al. Identification of CJC-1131-albumin bioconjugate as a stable and bioactive GLP-1(7–36) analog. Bioorg Med Chem Lett. 2004;14(17):4395–4398. doi: 10.1016/j.bmcl.2004.06.066. [DOI] [PubMed] [Google Scholar]
- 63.Amiram M, Luginbuhl KM, Li X, Feinglos MN, Chilkoti A. Injectable protease-operated depots of glucagon-like peptide-1 provide extended and tunable glucose control. Proc Natl Acad Sci U S A. 2013;110(8):2792–2797. doi: 10.1073/pnas.1214518110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Buse JB, Rosenstock J, Sesti G, et al. LEAD-6 Study Group Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6) Lancet. 2009;374(9683):39–47. doi: 10.1016/S0140-6736(09)60659-0. [DOI] [PubMed] [Google Scholar]
- 65.Agersø H, Jensen LB, Elbrønd B, Rolan P, Zdravkovic M. The pharmacokinetics, pharmacodynamics, safety and tolerability of NN2211, a new long-acting GLP-1 derivative, in healthy men. Diabetologia. 2002;45(2):195–202. doi: 10.1007/s00125-001-0719-z. [DOI] [PubMed] [Google Scholar]


