Abstract
Objective
To evaluate an e-mental health (EMH) approach to workers' health surveillance (WHS) targeting work functioning (WF) and mental health (MH) of healthcare professionals in a randomised controlled trial.
Methods
Nurses and allied health professionals (N = 1140) were cluster-randomised at ward level to the intervention (IG) or control group (CG). The intervention consisted of two parts: (a) online screening and personalised feedback on impaired WF and MH, followed by (b) a tailored offer of self-help EMH interventions. CG received none of these parts. Primary outcome was impaired WF (Nurses Work Functioning Questionnaire), assessed at baseline and after three and six months. Analyses were performed in the positively screened subgroup (i) and in all participants (ii).
Results
Participation rate at baseline was 32% (NIG = 178; NCG = 188). Eighty-two percent screened positive for at least mild impairments in WF and/or MH (NIG = 139; NCG = 161). All IG-participants (N = 178) received part (a) of the intervention, nine participants (all positively screened, 6%) followed an EMH intervention to at least some extent. Regarding the subgroup of positively screened participants (i), both IG and CG improved over time regarding WF (non-significant between-group difference). After six months, 36% of positively screened IG-participants (18/50) had a relevant WF improvement compared to baseline, versus 28% (32/115) of positively screened CG-participants (non-significant difference). In the complete sample (ii), IG and CG improved over time but IG further improved between three and six months while CG did not (significant interaction effect).
Conclusions
In our study with a full compliance rate of 6% and substantial drop-out leading to a small and underpowered sample, we could not demonstrate that an EMH-approach to WHS is more effective to improve WF and MH than a control group. The effect found in the complete sample of participants is not easily interpreted. Reported results may be useful for future meta-analytic work.
Trial Registration
Dutch Trial Register NTR2786
Introduction
Nurses have a high risk of developing common mental health complaints, such as distress, depression, and anxiety [1]–[3]. Impaired mental health of employees in healthcare occupations can have serious adverse effects, endangering the health and safety of not only themselves but also their patients. A study by Gärtner and colleagues found that impaired mental health in nurses and allied health professionals affects several aspects of their work functioning, including cognitive aspects (e.g. staying alert) and causing incidents at work [4]. Another study by Letvak and colleagues showed that depression in nurses was associated with presenteeism, which is in turn associated with patient falls, medication errors, and lower self-reported quality of care [5]. Adding to this, increased levels of psychological distress, even in a mild form, have been found to be associated with an increased likelihood of obtaining a disability pension in later life [6]. To sustain nurses' and allied health professionals' mental health and to enable them to remain healthy and well-functioning in their profession until retirement age, it is crucial to periodically screen these employees and provide interventions to improve their mental health and work functioning.
A potentially promising method for the early detection of impaired mental health and subsequent treatment in nurses and allied health professionals, is offering a mental module for workers' health surveillance (WHS). Although attention has been paid to the occupational hazards of healthcare employees [7], WHS targeting work functioning and mental health of nurses and allied health professionals has, to our knowledge, not been reported before.
WHS is an important component of occupational healthcare [8]. It is a means to implement preventive action by identifying and treating health complaints relevant to work, and it should be an essential component of programmes aimed at the protection of employees [9]. In the Netherlands, it has three aims: 1) to prevent the onset, recurrence, or worsening of work-related diseases, 2) to monitor and promote work-related health, and 3) to monitor and improve work functioning and employability [10]. It can be used to periodically monitor employees' health and work functioning to detect impairments early and to bring timely interventions into action to prevent further impairment. It is recommended to apply a job-specific assessment, to allow for tailoring of interventions to the specific detected work functioning impairments as fitting as possible [11]. In this study, we detect early signs of impaired mental health and impaired work functioning in nurses and allied health professionals, and offer interventions using an e-mental health approach.
E-mental health (EMH) is the use of information and communication technology, and in particular the many technologies related to the Internet, to support and improve mental health [12]. Applying EMH might be a useful and feasible approach to perform a mental module for WHS. Online screening is a practical and efficient method to screen for self-reported impaired work functioning and impaired mental health. Furthermore, EMH offers possibilities regarding the subsequent interventions. Ritterband and colleagues defined Internet interventions as typically focused on behavioral issues, aiming to institute behavior change and subsequent symptom improvement, usually self-paced, interactive, and tailored to the user, and making use of the multimedia format offered by the Internet [13]. EMH interventions exist which target a wide variety of common mental disorders such as depression, anxiety, panic, phobias, and various addictions. Unguided self-help EMH interventions have been found to have positive outcomes for a variety of mental health aspects (e.g. Warmerdam et al. [14]; Farrer et al. [15]; Riper et al. [16]; Blankers et al. [17]; Billings et al. [18]), although to our knowledge their effects on work functioning have not been studied in a specific working population such as nurses and allied health professionals. Moreover, EMH interventions have thus far only been offered as stand-alone interventions for a specific mental health complaint. In our study, we offer a choice of EMH interventions, tailored to the specific complaints as indicated by the individual's screening results.
In this paper, we study the effect of an EMH-approach to WHS targeting work functioning and mental health of hospital-employed nurses and allied health professionals, on their work functioning, distress, work-related fatigue, posttraumatic stress, and work ability in a cluster-randomized controlled trial. We hypothesized that WHS, consisting of online screening on impaired work functioning and impaired mental health followed by personalised feedback and a tailored offer of self-help EMH interventions, will improve work functioning and mental health.
Methods
The protocol for this trial and supporting CONSORT checklist are available as supporting information; see Checklist S1 and Protocol S1 (http://www.biomedcentral.com/1471-2458/11/290).
Ethics statement
The Medical Ethics Committee of the Academic Medical Center Amsterdam approved this study (for approved protocol see Protocol S2). All participants gave their written informed consent before taking part.
Study design
The study was designed as a cluster-randomised trial with block randomisation carried out at ward level. In order to guarantee allocation concealment, randomisation was performed by one researcher (KN) who was not involved in the practical recruitment of employees, using the computer software program Nquery Advisor with a block size of three. The complete trial included two intervention groups and one control group [19]. The present study compared one of the intervention groups, the e-mental health approach (EMH-approach) group, to the control group. The other intervention group consisted of an invitation for a preventive consultation with an occupational physician. A pre-randomisation procedure with incomplete-double-consent design was applied [20], meaning that individuals were only informed about their own group.
Outcome measures were obtained from all participants at baseline (March 2011) and follow-up measures were obtained three and six months after baseline.
The design, conduct and reporting of this study adhere to the Consolidated Standards of Reporting Trials guidelines [21], [22]. Details of the study design are reported elsewhere [19]. The trial registration number of the study is NTR2786 (Dutch Trial Register: http://www.trialregister.nl).
Participants
The study population of the complete trial was formed by all nurses, including surgical nurses and anaesthetic nurses, and allied health professionals (such as physiotherapists and radiotherapists) employed at one academic hospital in the Netherlands (N = 1731). Nurses and allied health professionals form two large groups of hospital employees, and many of their work demands and work conditions are similar. Since it regarded a preventive study, participants were included if they were not, or were not expecting to be on sick leave for more than two weeks at baseline.
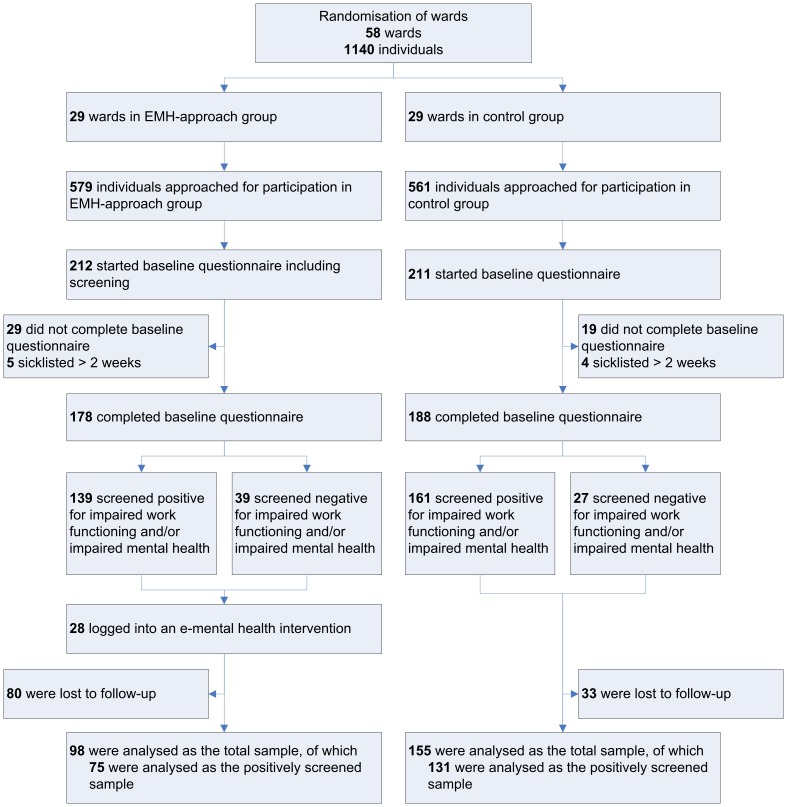
All eligible employees were invited for participation in the study. To detect a clinically significant effect (effect size≥.33), while conducting the tests with alpha = .05 (two-tailed) and power = .80, and allowing for possible cluster effects and loss to-follow-up, the minimum required sample size was 718 participants for the complete trial [19]. After randomization at ward level (N = 86), 29 wards with 579 employees were assigned to the EMH-approach group and 29 wards with 561 employees to the control group (Figure 1).
Figure 1. Flow of participants through the trial.
Procedure
In March 2011, potential participants received an invitation by e-mail to fill out the online baseline questionnaire which could be filled out at any time during six weeks. It was possible to discontinue the questionnaire and complete it after logging in again. Three reminders were sent, as well as an information letter to their home address. Those who had completed the baseline questionnaire were invited to fill out the follow-up questionnaires three and six months after baseline.
Intervention
E-mental health approach group
At baseline, participants in the EMH-approach group were screened on the following aspects (for details see Table 1 and Gärtner and colleagues [19]): impaired work functioning, distress, work-related fatigue, risky drinking behaviour, depression including suicide risk, anxiety, panic disorder, and posttraumatic stress. Participants received personalised feedback on their screening results immediately after filling out the baseline questionnaire, both onscreen and in an e-mail.
Table 1. Screening instruments and cut-off points.
| Aspect | Instrument | Cut-off point |
| Impaired work functioning | Nurses Work Functioning Questionnaire (7 subscales) [4] | Red score on ≥1 subscales and/or orange score on ≥3 subscales [19] |
| Distress | Four-Dimensional Symptoms Questionnaire, distress subscale [32], [33] | Total score≥11 [34] |
| Work-related fatigue | Need for recovery subscale of the Dutch Questionnaire on the Experience and Evaluation of Work [35] | Standardised total score≥54.5 [36] |
| Risky drinking behaviour | AUDIT-C [49] | Total score≥5 for men, ≥4 for women [50] |
| Depression | Brief Symptom Inventory, depression subscale [51] | Mean score≥0.42 [52] |
| (Suicide risk) | (One item from Brief Symptom Inventory, depression subscale [51]) | (Score≥3 on 0–4 scale) |
| Anxiety | Brief Symptom Inventory, anxiety subscale [51] | Mean score≥0.42 [52] |
| Panic disorder | Patient Health Questionnaire [53], only assessed for participants identified as having anxiety complaints | 2 answers affirmative on the first 4 items plus 4 symptoms affirmative on the following 11 items [54] |
| Posttraumatic stress | Dutch translation of the Impact of Event Scale [37], [38] | Total score≥26 [39] |
The personalised feedback was followed by an invitation for a tailored offer of self-help EMH interventions, on the basis of an algorithm based on the specific symptoms and the work-relatedness of the symptoms (available as supporting information, see Algorithm S1). Participants were mostly offered a choice of two or three EMH interventions to leave room for personal preferences. Participants who screened negative on all mental health complaints were invited to follow an EMH intervention aimed at enhancing and retaining their mental fitness.
The EMH interventions used in this study are self-help interventions on the Internet aimed at reducing specific mental health complaints or enhancing wellbeing. The interventions are mainly based on the principles of cognitive behavioural therapy and combine a variety of aspects, e.g. providing information and advice, weekly assignments, the option of keeping a diary and a forum to get in contact with others who have similar complaints. The EMH interventions were developed as stand-alone interventions by the Trimbos Institute (Netherlands Institute of Mental Health and Addiction) at an earlier stage. The following EMH interventions were used in the study:
Psyfit [23] : aimed at enhancing mental fitness. Also applied for healthy participants.
Strong at work [24] : aimed at gaining insight into work stress and learning skills to cope with it.
Colour your Life [25] : aimed at tackling depressive symptoms.
Don't Panic Online [26] : aimed at reducing panic symptoms for subclinical and mild cases of panic disorder.
Drinking Less [16] : aimed at reducing risky drinking behaviour.
Psyfit was found to be effective in decreasing symptoms of depression and anxiety and improving well-being and vitality [27]. Warmerdam and colleagues [14] showed that Colour your Life resulted in significantly lower depression and anxiety scores compared to a waiting-list control group and to significantly higher quality of life scores. The number of participants showing clinically relevant change regarding depression after 12 weeks was significantly higher. Spek and colleagues also found a significantly larger improvement in depressive symptoms compared to a waiting-list control group [28], [29]. Drinking Less resulted in more participants who reduced their drinking successfully to within guideline norms, and a significantly larger decrease in mean weekly alcohol consumption than a control group [16].
In case of positive screening on impaired work functioning (regardless of their mental health status), participants received an onscreen educational leaflet on how to improve their work functioning (available upon request).
Control group
Participants in the control group filled out the same baseline questionnaire as the EMH-approach group, but did not receive an intervention, and thus no screening results either. However, they were informed that they would receive personalised feedback and a tailored offer of self-help EMH interventions after six months, following the six months follow-up questionnaire.
Measures
All outcomes were measured at baseline and at three and six months follow-up.
Primary outcome
The primary outcome of this study was impaired work functioning, measured with the total score of the Nurses Work Functioning Questionnaire (NWFQ) [4]. This questionnaire has been developed to assess impaired work functioning in nurses and allied health professionals. In the screening phase, all seven of the original subscales were used. Participants scored either green, orange or red on each subscale. A red score on one or more subscales and/or three or more orange scores led to case identification of impaired work functioning (i.e. scoring above cut-off point on impaired work functioning) [19].
Only six of the seven original NWFQ subscales were used for the outcome measure, in contrast to what was described in the trial's design study [19], because the reproducibility of the impaired decision-making subscale was found to be poor [30]. The total score on the NWFQ was calculated with the 47 items of the remaining six subscales, with a total score range of 0–100, a higher score indicating more severely impaired work functioning.
The difference between the EMH-approach group and the control group regarding impaired work functioning was investigated using the continuous outcome and the percentage of individuals who had improved relevantly at follow-up [31].
Secondary outcomes
The secondary outcomes included distress, work-related fatigue, posttraumatic stress, and work ability.
Distress was measured with the distress subscale of the Four-Dimensional Symptoms Questionnaire (4DSQ) [32], [33]. The 16-item questionnaire uses a 5-point response scale (0 = no, 4 = very often) and has a total score range of 0–32, a higher score indicating a higher level of distress (cut-off point ≥11 [34]).
Work-related fatigue after working time was measured using the need for recovery subscale of the Dutch Questionnaire on the Experience and Evaluation of Work (QEEW) [35]. The 11-item questionnaire with dichotomous response categories (yes, no) has a total score range of 0–11 and a standardized score range of 0–100, a higher score indicating a higher level of work-related fatigue (cut-off point ≥54.5 [36]).
Posttraumatic stress was measured with the Dutch version of the Impact of Event Scale [37], [38]. The 15 items can be answered on a 4-point response scale (0 = not at all, 3 = often). Total scores range from 0–75, a higher score indicating a higher level of posttraumatic stress (cut-off point ≥26 [39]).
Work ability was assessed with the first item of the Work Ability Index (WAI) [40]. This item concerns the evaluation of current work ability compared to their lifetime best on an 11-point scale (0 = completely unable to work, 10 = work ability at its best), a higher score indicating a higher level of work ability.
Statistical analyses
All participants who completed the baseline questionnaire and who screened positive on impaired work functioning and/or impaired mental health (the targeted sample) were analysed, as the work functioning and mental health of these participants could be expected to change due to the intervention. However, since this was not pre-specified in the trial registration, the analyses were also performed with the total sample of participants (i.e. all participants, regardless of their screening results).
To describe participants, we used the following demographics: sex, age, occupation, specialization (yes/no), years of working experience, working hours per week, and type of contract. Additionally, the number of participants scoring above cut-off point for impaired work functioning and mental health complaints were calculated.
The analyses were performed at the level of the individual employee, according to the intention-to-treat principle. The significance level was set at α = .05. All analyses were carried out using the statistical package IBM SPSS Statistics 19.
Drop-out analysis
A drop-out analysis was performed to detect whether dropping out of the trial was related to the primary outcome impaired work functioning, and to identify potential predictive variables of drop-out. Dropping out of the trial was defined as completing the baseline and three months follow-up questionnaires, but not the six months follow-up questionnaire; or completing the baseline questionnaire, but none of the follow-up questionnaires. Differences between drop-outs and non drop-outs in impaired work functioning over time in both separate groups were explored in graphs. If different patterns of the effect after three months were detected, a Mann-Whitney U test was performed to test the significance of the differences. In the event of statistically significant differences, a multiple logistic regression analysis was performed with drop-out as the dependent variable, to identify potential predictive variables for drop-out. Screening positive on mental health complaints at baseline (yes/no) and age were included as the independent variables, as we expected that these two aspects might be related to dropping out of the trial. If the multiple logistic regression analysis showed one or both of these aspects to have a statistically significant effect on drop-out, they were included as a covariate in the effect analyses [41].
Effect analysis
To analyse the differences over time between the EMH-approach group and the control group on each outcome, Linear Mixed Models (LMM) were applied. If the assumption of a normal distribution of residuals was not met, a log-transformation was used for the LMM and the median and range were used to describe the outcome. Otherwise, the mean and standard deviation were used to describe the outcome.
For each outcome, the scores at three and six months follow-up were included as dependent variables in the LMM, while the baseline score was included as a covariate. The main effects of group and time of measurement, and the interaction of group*time of measurement were included as fixed effects in the model. Ward (the cluster level) and subject (the individual level) were included as random effects; however if the cluster level did not have a statistically significant effect, it was considered negligible and was therefore excluded from the model. The effects of interest were the main effect of group (interpreted as the difference between the groups from baseline to six months follow-up) and the interaction effect of group*time of measurement (interpreted as the difference between the groups from three to six months follow-up).
For all outcomes in the positively screened subgroup, we calculated Cohen's d [42] by determining the mean difference between the baseline score and the score at follow-up, divided by the pooled standard deviation. For Cohen's d, a score of 0.2 to 0.5 can be considered a small effect, 0.5 to 0.8 a medium effect, and greater than 0.8 a large effect [42].
Additionally, the relative change scores of individuals on impaired work functioning after three and after six months of follow-up compared to their baseline score were calculated. Individuals with a relative improvement on their NWFQ total score of 40% or more, which is the minimal important change (MIC) value of the NWFQ total scale [31], were defined as relevantly improved. The percentages of individuals who had improved relevantly in each group were compared using a Fisher's exact test, for both three months and six months follow-up.
Results
Participant flow
Figure 1 presents the flow of participants through the trial. From March 15th until April 26th, 423 employees (37%) started on the baseline questionnaire. Of those, 366 (32% of invited employees) were eligible for participation, 178 (31%) in the EMH-approach group and 188 (34%) in the control group. In the EMH-approach group, 80 participants (45%) were lost to follow-up, compared to 33 participants (18%) in the control group. Reasons for withdrawal were not assessed. Fifty-six participants (31%) in the EMH-approach group and 126 participants (67%) in the control group completed all three questionnaires.
Analyses were performed on the participants who screened positive (primary outcome: EMH N = 75, 54%; control N = 131, 81%), and additionally on all participants (primary outcome: EMH N = 98, 55%; control N = 155, 82%) who had participated in at least one follow-up.
Twenty-two participants (17 positively screened) logged into Psyfit, seven logged into Strong at work, four logged into Colour your Life, and no-one logged into Don't Panic Online or Drinking Less. Nine participants (all positively screened) followed an intervention to at least some extent (Psyfit: 6, Colour your Life: 3).
Study population at baseline
As shown in Table 2, the study groups were quite similar regarding demographic and occupational characteristics. The majority of participants were female and employed as a nurse. Participants in the EMH-approach group had a younger average age of 37, compared to 42 in the control group. The participants worked an average of 31 hours per week and most of them had a permanent position in the hospital. Around 4/5th of participants screened positive on work functioning impairments and/or impaired mental health, more participants in the control group (N = 161, 86%) than in the EMH-approach group (N = 139, 78%).
Table 2. Participant characteristics at baseline for the EMH-approach group and the control group.
| Total sample | Positively screened sample | |||||||
| EMH-approach (N = 178) | Control (N = 188) | EMH-approach (N = 139) | Control (N = 161) | |||||
| Variable | n | (%) | n | (%) | n | (%) | n | (%) |
| Sex | ||||||||
| Female | 147 | (83) | 145 | (77) | 113 | (81) | 126 | (78) |
| Age in years (mean (SD)) | 37 | (12) | 42 | (11) | 38 | (12) | 42 | (12) |
| Occupation | ||||||||
| Nurse | 129 | (73) | 134 | (71) | 99 | (71) | 115 | (71) |
| Nurse practitioner | 11 | (6) | 22 | (12) | 7 | (5) | 18 | (11) |
| Surgical nurse | 0 | (0) | 5 | (3) | 0 | (0) | 5 | (3) |
| Anesthetic nurse | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| Allied health professional | 38 | (21) | 27 | (14) | 33 | (24) | 23 | (14) |
| Nursing specialization | ||||||||
| Yes | 74 | (57) | 86 | (64) | 57 | (58) | 75 | (65) |
| Years of experience (mean (SD)) | 10 | (10) | 11 | (10) | 11 | (10) | 11 | (10) |
| Working hours per week according to contract (mean (SD)) | 31 | (5) | 31 | (6) | 31 | (5) | 31 | (6) |
| Type of contract | ||||||||
| Permanent position | 160 | (91) | 174 | (93) | 125 | (91) | 150 | (94) |
| Fixed-term contract | 13 | (7) | 12 | (6) | 11 | (8) | 9 | (6) |
| Temporary employment | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| Other | 3 | (2) | 1 | (1) | 1 | (1) | 1 | (1) |
| Impaired work functioning * (above cut-off) | ||||||||
| Work functioning impairments | 107 | (60) | 131 | (70) | 107 | (77) | 131 | (81) |
| Impaired mental health (above cut-off) | ||||||||
| Impaired mental health (above cut-off of one or more of the six mental health aspects) | 109 | (61) | 119 | (63) | 109 | (78) | 119 | (74) |
| Distress | 41 | (23) | 48 | (26) | 41 | (30) | 48 | (30) |
| Work related fatigue | 61 | (34) | 65 | (35) | 61 | (44) | 65 | (40) |
| Post traumatic stress | 24 | (14) | 19 | (10) | 24 | (17) | 19 | (12) |
| Screened positive on impaired work functioning and/or impaired mental health | 139 | (78) | 161 | (86) | 139 | (100) | 161 | (100) |
Note: Work functioning is presented here including the subscale impaired decision-making, as it was included in the screening at baseline.
Drop-out analysis
Graphs in which the scores of drop-outs and non drop-outs on the primary outcome were compared, showed that in both groups drop-outs had a worse score on impaired work functioning (EMH baseline median = 13, 3 mn follow-up median = 12; C baseline median = 14, 3 mn follow-up median = 11) than non drop-outs (EMH baseline median = 9, 3 mn follow-up median = 8; C baseline median = 12, 3 mn follow-up median = 8) at baseline and three months follow-up. A Mann-Whitney U test identified that these differences were statistically significant in the EMH-approach group (baseline U = 4.688, p = .01; 3 mn follow-up U = 970, p = .04) and in the entire group of participants (baseline U = 19.202,5, p = .01; 3 mn follow-up U = 5.079,5, p = .01). In a subsequent logistic regression analysis, age was identified as a statistically significant predictor of drop-out in the entire group (p = .02, younger participants had a higher chance of drop-out), but screening positive for mental health complaints at baseline (yes/no) was not (p = .16). Therefore, age was included as a covariate in the effect analyses.
Intervention effects
The results in Table 3 refer to the group of participants who screened positive for impaired work functioning and/or mental health impairments at baseline. The relative frequency of participants who scored above cut-off point on the outcome measures and the mean and median scores (in case of a non-normal distribution) are presented for baseline and both follow-up points, as well as the results of the LMM analyses.
Table 3. Descriptives and analysis results on primary and secondary outcomes of the positively screened sample at baseline, 3 and 6 months follow-up.
| E-mental health approach group | Control group | p-value (LMM analyses)** | |||||||||
| Relative frequency above cut-off (%) | Median (range) | Mean (SD) | Effect size (95% CI) | Relative frequency above cut-off (%) | Median (range) | Mean (SD) | Effect size(95% CI) | group | group*time | ||
| Primary outcome | |||||||||||
| Impaired work functioning | b | 91/139 (66) | 14 (0–56) | 110/161 (68) | 14 (0–54) | .771 | .283 | ||||
| (NWFQ 0–100) * | 3 mn | 33/62 (53) | 10 (0–39) | .19 (−.16–.55) | 61/124 (49) | 10 (0–38) | .26 (.01–.51) | ||||
| 6 mn | 19/52 (37) | 8 (0–41) | .16 (−.22–.55) | 60/116 (52) | 10 (0–44) | .24 (−.01–.50) | |||||
| Secondary outcomes | |||||||||||
| Distress | b | 41/139 (30) | 7 (0–32) | 48/161 (30) | 6 (0–32) | .592 | .828 | ||||
| (4DSQ, 0–32) | 3 mn | 9/61 (15) | 4 (0–29) | .20 (−.16–.56) | 25/123 (20) | 5 (0–29) | .26 (.01–.51) | ||||
| 6 mn | 10/52 (19) | 5 (0–29) | .07 (−.32–.45) | 26/116 (22) | 5 (0–30) | .14 (−.11–.40) | |||||
| Work-related fatigue | b | 61/139 (44) | 44 (28) | 65/161 (40) | 39 (30) | .617 | .732 | ||||
| (QEEW, 0–100) | 3 mn | 22/61 (36) | 36 (31) | .16 (−.20–.52) | 42/123 (34) | 35 (30) | .12 (−.13–.37) | ||||
| 6 mn | 14/52 (27) | 34 (30) | .02 (−.36–.41) | 39/116 (34) | 37 (31) | .02 (−.24–.27) | |||||
| Posttraumatic stress | b | 24/139 (17) | 3 (0–71) | 19/161 (12) | 3 (0–48) | .357 | .124 | ||||
| (IES, 0–75) | 3 mn | 10/61 (16) | 1 (0–48) | .07 (−.29–.42) | 13/122 (11) | 0 (0–62) | .31 (.05–.56) | ||||
| 6 mn | 5/51 (10) | 0 (0–31) | .24 (−.15–.63) | 9/116 (8) | 0 (0–48) | .26 (.00–.51) | |||||
| Work ability | b | 7 (1) | 8 (2) | .483 | .552 | ||||||
| (WAI, 0–10) | 3 mn | 8 (1) | .14 (−.21–.50) | 8 (1) | −.01 (−.26–.25) | ||||||
| 6 mn | 8 (2) | .05 (−.34–.44) | 8 (1) | .01 (−.25–.26) | |||||||
Note: NWFQ total scores were calculated without the subscale impaired decision-making.
Number analysed in EMH-approach group: N = 75 (impaired work functioning), N = 74 (distress and work-related fatigue), N = 73 (posttraumatic stress and work ability); numbers analysed in Control group: N = 131 (all outcomes).
b, baseline; 3 mn, follow-up after 3 months; 6 mn, follow-up after 6 months.
Since the random effect of ward (the cluster level) was not statistically significant in any of the analyses, it was excluded from the model in the LMM analyses.
Impaired work functioning (primary outcome)
The EMH-approach group and the control group improved to a similar degree between baseline and three months follow-up. The EMH-approach group improved further between three and six months, while the control group remained at approximately the same level. As shown in Table 3, in the LMM analysis of impaired work functioning in the positively screened sample of participants, no statistically significant difference between the EMH-approach group and the control group was identified (main effect of group p = .77; interaction effect of group*time p = .28). The effect size estimate after three and six months was comparably low in both groups.
In the LMM analysis of the total sample of participants (data not shown in table), no significant effect of group was found (p = .68), but a significant interaction effect of group*time was found (p = .04), suggesting there to be a different pattern of scores on impaired work functioning from three to six months follow-up between the EMH-approach group and the control group. A closer look at the median scores on impaired work functioning revealed that both groups improved to a similar degree between baseline and three months follow-up, and that the EMH-approach group further improved between three and six months follow-up while the control group slightly deteriorated.
In Table 4, the percentages of individual employees with a relevant improvement on work functioning after three and after six months compared to their baseline score are shown. After three months, in the positively screened sample as well as the total sample, roughly the same percentage of participants in both groups had improved relevantly regarding work functioning compared to their baseline score. After six months, more participants in the EMH-approach group than in the control group had improved relevantly compared to baseline, in both the positively screened sample (EMH 36%; control 28%) and the total sample (EMH 40%; control 30%). However, these differences were not statistically significant (p = .36 and p = .21, respectively).
Table 4. Participants whose work functioning had improved with at least the minimal important change at 3 and 6 months follow-up compared to baseline: descriptives and analysis results.
| EMH-approach | Control group | p-value | ||
| Relative frequency (%) | Relative frequency (%) | (Fisher's exact test) | ||
| Positively screened sample | 3 mn | 18/60 (30%) | 37/123 (30%) | 1.000 |
| 6 mn | 18/50 (36%) | 32/115 (28%) | .357 | |
| Total sample | 3 mn | 24/80 (30%) | 46/142 (32%) | .765 |
| 6 mn | 27/68 (40%) | 40/134 (30%) | .206 |
3 mn, follow-up after 3 months; 6 mn, follow-up after 6 months.
Secondary outcomes
As shown in Table 3, both groups improved over time regarding distress, work-related fatigue, and posttraumatic stress, with the largest improvement between baseline and three months of follow-up. On distress and work-related fatigue, the EMH-approach group had a larger overall improvement than the control group (non-significant). In the LMM analyses on distress, work-related fatigue, posttraumatic stress, and work ability in the positively screened sample, no statistically significant differences were found between the EMH-approach group and the control group (main effect of group .36≤p≤.62; interaction effect of group*time .12≤p≤.83). Effect sizes in both groups were fairly similar, small to non-relevant.
In the LMM analyses on the secondary outcomes in the total sample of participants (data not shown in table), no significant differences were found between the EMH-approach group and the control group either (.31≤p≤.97).
Discussion
The results of our study suggest that an e-mental health (EMH) approach of workers' health surveillance (WHS), consisting of online screening on impaired work functioning and impaired mental health followed by personalised feedback and a tailored offer of self-help EMH interventions, shows no significant improvement in impaired work functioning, distress, work-related fatigue, posttraumatic stress, and work ability to a larger extent than a control group. Compliance to the EMH interventions was low, which impedes drawing a conclusion about the effect of this part of the intervention. Screening and personalised feedback was received by all participants in the intervention group. Although the study had insufficient power, the low effect sizes do not give reason to expect a relevant effect of screening and feedback. The outcomes may be of value for future meta-analytic work.
One third of the employees who were invited, participated in the study. Of these participants, more than 80% screened positive for at least mild impairments in work functioning and/or mental health. Both the intervention group and the control group improved over time on work functioning, distress, work-related fatigue, and posttraumatic stress, with no statistically significant difference between the groups. However, when including all participants in the analyses and not only those who had screened positive on impairments at baseline, the work functioning of the EMH-approach group showed a significantly different pattern compared to the control group, as the EMH-approach group further improved between three and six months after baseline while the control group did not. After six months, a relevant improvement of work functioning was found for 36% of positively screened participants in the intervention group and 28% in the control group, but the difference between the groups was non-significant.
Interpretation of results
First of all, our study had a high percentage of participants who screened positive for at least mild impairments. This included screening positive on impairments in work functioning, on one or more mental health complaints or both. In choosing our cut-off points, we aimed for high sensitivity, since we did not want to miss participants who might need help. The cut-off points that we applied for the mental health complaints were all validated. However, high sensitivity generally comes at the expense of high specificity, which might have led to higher numbers of false positives in our study. We formulated the online feedback mildly, careful not to speak of diagnosis or mental health problems, to prevent incorrect interpretation. Additionally, the relatively high number of screening instruments might have led to a high overall percentage of participants who screened positive for at least one of the screeners.
Our intervention consisted of two parts. First, the participants in the intervention group underwent online screening on impaired work functioning and impaired mental health, followed by personalised feedback on their screening results. Subsequently, they were offered a tailored offer of EMH interventions. In addition, participants with impaired work functioning received an onscreen educational leaflet on how to improve their work functioning. Two scenarios might explain our not finding an effect of the intervention: programme failure and theory failure [43]: the intervention was not carried out as intended (programme failure), or the intervention is not effective (theory failure).
The process evaluation that was carried out alongside this randomised controlled trial [44] offers some information on potential programme failure. The personalised feedback was received by all participants in the intervention group, since it appeared onscreen immediately after filling out the baseline questionnaire and was sent to the participants' e-mail address automatically. The onscreen educational leaflet on how to improve work functioning was also sent automatically to participants with impaired work functioning. However, the compliance to the subsequently offered self-help EMH interventions was low. Only 28 participants logged into an EMH intervention, and 6% (N = 9) of the positively screened participants in the intervention group started an EMH intervention to at least some extent. Regarding the second part of the intervention (the EMH interventions), program failure may therefore have occurred.
Participants offered no explanation why they did not follow an EMH intervention [44]. Three explanations are conceivable. Firstly, there is a reported trend in the literature of a low perception of need for mental health interventions. Lexis and colleagues found that 43% of employees who were identified with mild to severe depressive complaints, did not report to experience health complaints themselves [45]. Codony and colleagues found that merely a third of those who had a mental disorder in the past 12 months, had a perceived need of mental healthcare [46]. Since our study regarded a preventive setting and we chose for high sensitivity in our screening, perhaps the perceived need of our participants was insufficient to motivate them to log into and follow an EMH intervention. Secondly, some of the participants (N = 9) reported problems with logging into the interventions, due to technical problems and/or inadequate computer skills, which might have posed a problem for more participants. A third explanation is that the channelling from the personalised feedback towards the EMH interventions might not have been attractive enough to encourage participants to follow an EMH intervention.
The possibility of theory failure should also be considered. The intervention consisted of screening and personalised feedback on screening results including channelling towards EMH interventions, an onscreen educational leaflet on how to improve work functioning (if applicable), and following the EMH interventions. Most of the EMH interventions that were used in our study have been found effective to reduce symptoms of impaired mental health in previous research [14], [16], [27]–[29], supporting our hypothesis that an EMH-approach to WHS, including EMH interventions (if complied to), might be effective in improving mental health and improving work functioning. However, it should be noted that for these previous studies, most participants had actively responded to advertisements targeting people who wanted to work on their depressive symptoms or their mental fitness. Therefore, these participants actively sought help and improvement through EMH interventions. This differs considerably from our setting, as our participants took part in WHS targeting work functioning and mental health and might not have been as much aware that they would be offered EMH interventions.
However, since the intervention was not carried out as intended, we cannot conclude that the complete EMH-approach to WHS targeting work functioning and mental health of healthcare employees is ineffective. Moreover, we found that when looking at the total sample of participants, both groups improved over time, but the EMH-approach group continued to improve between three and six months after baseline while the control group slightly deteriorated in this time interval. Possibly, we were able to find a significant effect in this total sample, because the number of participants was higher in this group and the analysis was therefore better powered to find existing differences. Since the EMH interventions themselves were hardly followed, this suggests that the other elements of the complete EMH-approach – possibly increasing awareness - might have had some (delayed) effect on work functioning. However, the results in this total sample of participants are not easily interpreted, since only the personalised feedback was received by all participants in the intervention group, and the observed effect did not occur until later in time.
Limitations
Several limitations of our study can be noted. First of all, we did not meet our required sample size for sufficient power, set at 189 participants in each group who completed participation. This increases the chance of finding non-significant p-values despite trends for differences. The data show that, regarding impaired work functioning, a higher percentage of participants in the EMH-approach group than in the control group improved to a relevant degree compared to their own baseline scores, but this difference was not statistically significant, which might have been a result of insufficient power. However, the observed effect sizes were very small, and in most cases were fairly similar between the groups.
A second limitation of our study was the fairly high and selective drop-out rate of participants, especially in the intervention group. Drop-outs had higher scores on impaired work functioning at baseline and three months follow-up than participants who did not drop out of the trial. We do not know why this occurred, since we did not assess reasons for drop-out. We received mixed reactions to the personalised but automatic feedback on screening results and the for some participants unexpected offer to follow an EMH intervention. We suppose this might have led to resistance and the higher drop-out in the intervention group. The high and selective drop-out may have introduced bias, although we have no way of knowing in which direction this possible bias occurred.
Thirdly, as discussed before, the compliance to the offered EMH interventions was low, complicating studying the effect of the complete EMH-approach to WHS.
Lastly, we studied the effects of the EMH-approach in a group of positively screened participants, regardless of what they screened positive for. Since not everyone screened positive for every impairment of complaints and the offered intervention was tailored to each individual, it might not be reasonable to expect an improvement for every impairment or complaint if examining the total group.
Implications for practice and further research
Our study confirms that preventive actions are essential for nurses and allied health professionals, since we identified that more than 80% of participants show at least some level of impaired work functioning and/or symptoms of mental health problems.
We endeavoured to improve work functioning and mental health through online screening, personalised feedback, and a subsequent tailored offer of self-help EMH interventions. We think that targeting work functioning is an important approach, as the ultimate goal of occupational healthcare is to keep employees functioning well and as healthy as possible. However, we were unsuccessful in studying the EMH-approach, because very few participants followed an EMH intervention to at least some degree. Therefore, we recommend further research on two aspects. First, it is essential to identify the specific needs and wishes that nurses and allied health professionals have regarding their work related health and to study how they want to be supported to stay healthy and well-functioning at work. Possibly, a more comprehensive WHS including important other factors of their work, such as physical aspects (e.g. musculoskeletal complaints), would increase their interest and participation. Secondly, it should be investigated whether EMH interventions are suitable and acceptable for a WHS setting for nurses and allied health professionals, and if they would prefer some degree of contact with a healthcare provider. It is recommended to explore the possibility of “blended care”, i.e. combining an offer of an EMH intervention with several coaching sessions. Moreover, it could be useful to apply elements of persuasive design to encourage employees to follow an EMH intervention [47], [48].
Supporting Information
Algorithm for determining the specific choice of e-mental health interventions.
(PDF)
CONSORT Checklist.
(DOC)
Study protocol as published in BMC Public Health ( http://www.biomedcentral.com/1471-2458/11/290 ).
(PDF)
Study protocol as approved by ethics committee.
(PDF)
Acknowledgments
We thank Eva Fischer (Innovation Center of Mental Health & Technology, Trimbos Institute, Netherlands Institute of Mental Health and Addiction, Utrecht, the Netherlands) for her contribution in the design of the study.
Data sharing: data are available on request.
Funding Statement
The Mental Vitality @ Work trial was co-financed by a grant from the Dutch Foundation Institute Gak (URL: http://www.instituutgak.nl, PrevBGZ/project D) and a grant from The Netherlands Organisation for Health Research and Development (ZonMW) (URL: http://www.zonmw.nl/en, grant number 208010001). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Letvak S, Ruhm CJ, McCoy T (2012) Depression in hospital-employed nurses. Clin Nurse Spec 26: 177–182. [DOI] [PubMed] [Google Scholar]
- 2. Hammig O, Brauchli R, Bauer G (2012) Effort-reward and work-life imbalance, general stress and burnout among employees of a large public hospital in Switzerland. Swiss Med Wkly 142. [DOI] [PubMed] [Google Scholar]
- 3. Adriaenssens J, de Gucht V, Maes S (2012) The impact of traumatic events on emergency room nurses: Findings from a questionnaire survey. Int J Nurs Stud 49: 1411–1422. [DOI] [PubMed] [Google Scholar]
- 4. Gärtner FR, Nieuwenhuijsen K, van Dijk FJ, Sluiter JK (2012) Impaired work functioning due to common mental disorders in nurses and allied health professionals: the Nurses Work Functioning Questionnaire. Int Arch Occup Environ Health 85: 125–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Letvak SA, Ruhm CJ, Gupta SN (2012) Nurses' presenteeism and its effects on self-reported quality of care and costs. Am J Nurs 112: 30–38. [DOI] [PubMed] [Google Scholar]
- 6. Rai D, Kosidou K, Lundberg M, Araya R, Lewis G, et al. (2012) Psychological distress and risk of long-term disability: population-based longitudinal study. J Epidemiol Community Health 66: 586–592. [DOI] [PubMed] [Google Scholar]
- 7. Hood J, Larranaga M (2007) Employee health surveillance in the health care industry. AAOHN J 55: 423–431. [PubMed] [Google Scholar]
- 8. Koh D, Aw TC (2003) Surveillance in occupational health. Occup Environ Med 60: 705–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Labour Organization (1998) Technical and ethical guidelines for workers' health surveillance. Geneva: ILO.
- 10.NVAB (2005) Leidraad Preventief Medisch Onderzoek [Guidance Workers' Health Surveillance]. Utrecht, the Netherlands: NVAB [Netherlands Society of Occupational Medicine].
- 11. Sluiter JK (2006) High-demand jobs: age-related diversity in work ability? Appl Ergon 37: 429–440. [DOI] [PubMed] [Google Scholar]
- 12.Riper H, Smit F, van der Zanden R, Conijn B, Kramer J, et al.. (2007) E-mental health. High tech, high touch, high trust. Utrecht: Trimbos-instituut.
- 13. Ritterband LM, Gonder-Frederick LA, Cox DJ, Clifton AD, West RW, et al. (2003) Internet Interventions: In Review, In Use, and Into the Future. Prof Psychol Res Pr 34: 527–534. [Google Scholar]
- 14. Warmerdam L, van Straten A, Twisk J, Riper H, Cuijpers P (2008) Internet-based treatment for adults with depressive symptoms: randomized controlled trial. J Med Internet Res 10: e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Farrer L, Christensen H, Griffiths KM, Mackinnon A (2011) Internet-based CBT for depression with and without telephone tracking in a national helpline: randomised controlled trial. PLoS One 6: e28099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Riper H, Kramer J, Smit F, Conijn B, Schippers G, et al. (2008) Web-based self-help for problem drinkers: a pragmatic randomized trial. Addiction 103: 218–227. [DOI] [PubMed] [Google Scholar]
- 17. Blankers M, Koeter MW, Schippers GM (2011) Internet therapy versus internet self-help versus no treatment for problematic alcohol use: A randomized controlled trial. J Consult Clin Psychol 79: 330–341. [DOI] [PubMed] [Google Scholar]
- 18. Billings DW, Cook RF, Hendrickson A, Dove DC (2008) A web-based approach to managing stress and mood disorders in the workforce. J Occup Environ Med 50: 960–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gärtner FR, Ketelaar SM, Smeets O, Bolier L, Fischer E, et al. (2011) The Mental Vitality @ Work study: design of a randomized controlled trial on the effect of a workers' health surveillance mental module for nurses and allied health professionals. BMC Public Health 11: 290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schellings R, Kessels AG, ter Riet G, Sturmans F, Widdershoven GA, et al. (2009) Indications and requirements for the use of prerandomization. J Clin Epidemiol 62: 393–399. [DOI] [PubMed] [Google Scholar]
- 21. Campbell MK, Elbourne DR, Altman DG (2004) CONSORT statement: extension to cluster randomised trials. BMJ 328: 702–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother 1: 100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bolier L, Haverman M, Kramer J, Boon B, Smit F, et al. (2012) Internet-based intervention to promote mental fitness in mildly depressed adults: design of a randomized controlled trial. JMIR Res Protoc 1: e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cursus ‘Sterk op het werk’ [Course Strong at Work]. Available: http://www.loketgezondleven.nl/i-database/interventies/c/13907. Accessed: December 6, 2012.
- 25. de Graaf LE, Gerhards SA, Arntz A, Riper H, Metsemakers JF, et al. (2009) Clinical effectiveness of online computerised cognitive-behavioural therapy without support for depression in primary care: randomised trial. Br J Psychiatry 195: 73–80. [DOI] [PubMed] [Google Scholar]
- 26. van Ballegooijen W, Riper H, van Straten A, Kramer J, Conijn B, et al. (2011) The effects of an Internet based self-help course for reducing panic symptoms - Don't Panic Online: study protocol for a randomised controlled trial. Trials 12: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bolier L, Haverman M, Bohlmeijer E (2010) Psyfit online - Gerandomiseerde effectstudie naar een e-mental fitness zelfhulpprogramma - Intern rapport [Psyfit online - Randomized effect study on an online mental fitness self-help program - Internal report]. Utrecht: Trimbos-instituut.
- 28. Spek V, Nyklicek I, Smits N, Cuijpers P, Riper H, et al. (2007) Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: a randomized controlled clinical trial. Psychol Med 37: 1797–1806. [DOI] [PubMed] [Google Scholar]
- 29. Spek V, Cuijpers P, Nyklicek I, Smits N, Riper H, et al. (2008) One-year follow-up results of a randomized controlled clinical trial on internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years. Psychol Med 38: 635–639. [DOI] [PubMed] [Google Scholar]
- 30. Gärtner FR, Nieuwenhuijsen K, van Dijk FJ, Sluiter JK (2011) Psychometric properties of the Nurses Work Functioning Questionnaire (NWFQ). PLoS One 6: e26565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gärtner FR, Nieuwenhuijsen K, van Dijk FJ, Sluiter JK (2012) Interpretability of change in the Nurses Work Functioning Questionnaire: minimal important change and smallest detectable change. J Clin Epidemiol 65: 1337–1347. [DOI] [PubMed] [Google Scholar]
- 32. Terluin B (1998) De Vierdimensionele Klachtenlijst (4DKL) in de huisartspraktijk [The Four Dimensional Symptom Questionnaire (4DSQ)]. De Psycholoog 33: 18–24. [Google Scholar]
- 33. Terluin B, van Marwijk HW, Ader HJ, de Vet HC, Penninx BW, et al. (2006) The Four-Dimensional Symptom Questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry 6: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van Rhenen W, van Dijk FJ, Schaufeli WB, Blonk RW (2008) Distress or no distress, that's the question: A cutoff point for distress in a working population. J Occup Med Toxicol 3: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Veldhoven M, Meijman TF (1994) Het meten van een psychosociale arbeidsbelasting met een vragenlijst: de vragenlijst beleving en beoordeling van arbeid (VBBA) [The measurement of psychosocial job demands with a questionnaire: the questionnaire on the experience and evaluation of work (QEEW)]. Amsterdam: Dutch Institute for Working Conditions.
- 36. Broersen JPJ, Fortuin RJ, Dijkstra L, van Veldhoven M, Prins J (2004) Monitor Arboconvenanten: kengetallen en grenswaarden [Monitor occupational health and safety: key indicators and limits]. TBV 12: 100–104. [Google Scholar]
- 37. Brom D, Kleber RJ (1985) De Schok Verwerkings Lijst [The Impact of Event Scale]. Nederlands Tijdschrift voor de Psychologie 40: 164–168. [Google Scholar]
- 38. Horowitz M, Wilner N, Alvarez W (1979) Impact of Event Scale: a measure of subjective stress. Psychosom Med 41: 209–218. [DOI] [PubMed] [Google Scholar]
- 39. van der Ploeg E, Kleber RJ (2003) Acute and chronic job stressors among ambulance personnel: predictors of health symptoms. Occup Environ Med 60 Suppl 1: i40–i46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A (1998) Work Ability Index. Helsinki: Finnish Institute of Occupational Health.
- 41. DeSouza CM, Legedza AT, Sankoh AJ (2009) An overview of practical approaches for handling missing data in clinical trials. J Biopharm Stat 19: 1055–1073. [DOI] [PubMed] [Google Scholar]
- 42.Cohen J (1988) Statistical power analysis for the behavioral sciences. 2nd edn. Hillsdale, N.J.: Lawrence Erlbaum Associates.
- 43. Kristensen TS (2005) Intervention studies in occupational epidemiology. Occup Environ Med 62: 205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ketelaar SM, Gärtner FR, Bolier L, Smeets O, Nieuwenhuijsen K, et al. (2013) Mental Vitality @ Work - A Workers' Health Surveillance mental module for nurses and allied health care professionals. Process evaluation of a randomized controlled trial. J Occup Environ Med 55: 563–571. [DOI] [PubMed] [Google Scholar]
- 45. Lexis MA, Jansen NW, Stevens FC, van Amelsvoort LG, Kant I (2010) Experience of health complaints and help seeking behavior in employees screened for depressive complaints and risk of future sickness absence. J Occup Rehabil 20: 537–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Codony M, Alonso J, Almansa J, Bernert S, de Girolamo G, et al. (2009) Perceived need for mental health care and service use among adults in Western Europe: results of the ESEMeD project. Psychiatr Serv 60: 1051–1058. [DOI] [PubMed] [Google Scholar]
- 47.Fogg BJ (2009) A Behavior Model for Persuasive Design. Available: http://bjfogg.com/fbm_files/page4_1.pdf. Accessed: December 6, 2012.
- 48. Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JE (2012) Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res 14: e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA (1998) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 158: 1789–1795. [DOI] [PubMed] [Google Scholar]
- 50. Gual A, Segura L, Contel M, Heather N, Colom J (2002) Audit-3 and audit-4: effectiveness of two short forms of the alcohol use disorders identification test. Alcohol Alcohol 37: 591–596. [DOI] [PubMed] [Google Scholar]
- 51.de Beurs E (2006) Brief Symptom Inventory (BSI): Handleiding. Leiden, the Netherlands: Pits Publishers.
- 52. de Beurs E, Zitman FG (2006) De Brief Symptom Inventory (BSI): De betrouwbaarheid en validiteit van een handzaam alternatief voor de SCL-90. [The Brief Symptom Inventory (BSI): The reliability and validity of a brief alternative of the SCL-90]. Maandblad Geestelijke Volksgezondheid 61: 120–141. [Google Scholar]
- 53. Spitzer RL, Kroenke K, Williams JB (1999) Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 282: 1737–1744. [DOI] [PubMed] [Google Scholar]
- 54. Lowe B, Grafe K, Zipfel S, Spitzer RL, Herrmann-Lingen C, et al. (2003) Detecting panic disorder in medical and psychosomatic outpatients: comparative validation of the Hospital Anxiety and Depression Scale, the Patient Health Questionnaire, a screening question, and physicians' diagnosis. J Psychosom Res 55: 515–519. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Algorithm for determining the specific choice of e-mental health interventions.
(PDF)
CONSORT Checklist.
(DOC)
Study protocol as published in BMC Public Health ( http://www.biomedcentral.com/1471-2458/11/290 ).
(PDF)
Study protocol as approved by ethics committee.
(PDF)