Abstract
Background
Iliopsoas tenotomy is a treatment for snapping hip. Does this surgical procedure change the surrounding muscle and tendon anatomy?
Questions/Purposes
This study seeks to evaluate the changes in the MR appearance of the hip muscles and iliopsoas tendon in patients following arthroscopic iliopsoas tenotomy.
Methods
One hundred sixty-nine consecutive adults were evaluated after iliopsoas tenotomy at the lesser trochanter. Each MR exam was evaluated independently by three radiologists for muscle edema, atrophy (grade 0–4), compensatory hypertrophy, signal within the iliopsoas tendon (increased on T1 or T2 sequences), and iliopsoas tendon morphology (distorted or disrupted) above, at, and below the iliopectineal eminence. A finding was considered positive if reported by two or three of the radiologists.
Results
Twenty subjects met the inclusion criteria. Muscle edema was present in 15% (3/20) of subjects within the iliacus, psoas, and quadratus femoris. Atrophy was observed in the following muscles: iliacus 85% (17/20), psoas 75% (15/20), quadratus femoris 10% (2/20), rectus femoris 5% (1/20), vastus lateralis 5% (1/20), and gluteus maximus 25% (5/20). There was no compensatory hypertrophy. Ninety percent (18/20) had increased T1 and 10% (2/20) had increased T2 signal within the iliopsoas tendon. Thirty-five percent (7/20) of the iliopsoas tendons was disrupted and 85% (17/20) was distorted, most commonly below the iliopectineal eminence.
Conclusion
The majority of postoperative symptomatic patients has atrophy of the iliacus and psoas muscles and distortion and disruption of the iliopsoas tendon and should be recognized as a normal imaging appearance following iliopsoas tendon release.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-013-9361-9) contains supplementary material, which is available to authorized users.
Keywords: iliopsoas, tenotomy, muscle atrophy postoperative
Introduction
A painful snapping hip may have an external, internal, or intra-articular cause [1, 2, 8]. In our experience, internal snapping of the iliopsoas tendon is the most clinically significant cause for a painful snapping hip. This snapping is most commonly caused by conflict between the iliopsoas tendon and muscle [4], but can also be due to catching at the iliopectineal eminence or snapping across the femoral head [1]. Spinal radiculopathy and iliopsoas tendinosis should not be confused at MR imaging. With iliopsoas tendinosis, there would be a thickened, hypoechoic, iliopsoas tendon while with spinal nerve root compression the iliopsoas would have normal diameter and morphology.
Treatment for the snapping iliopsoas tendon can include conservative measures such as rest, anti-inflammatory medications, physical therapy, and injection of corticosteroids into the iliopsoas bursa but may require in nonresponders open surgical or endoscopic release and lengthening of the iliopsoas tendon [1, 2, 7, 8, 12].
To date, no study has been performed to evaluate the MR imaging findings of the hip following arthroscopic iliopsoas tenotomy. The goal of this study was to evaluate the changes in the magnetic resonance (MR) appearance of the hip muscles and iliopsoas tendon in patients following arthroscopic iliopsoas tenotomy performed for snapping hip and to determine their relationship to hip function. In particular, we aimed to (a) describe the degree to which the ilioposoas and other muscles develop atrophy, (b) provide a detailed description of the MR signal changes before and after surgery, and (c) correlate MR findings with changes in the modified Harris hip score.
Materials and Methods
The study was performed in compliance with HIPAA regulations, with approval from the Institutional Review Board, and with a waiver of informed consent. Using an operative database of 714 hip arthroscopies performed between June 2004 and June 2011 we identified all patients who had arthroscopic iliopsoas tenotomy at the lesser trochanter by a single orthopedic surgeon.
The iliopsoas tenotomies were performed utilizing two arthroscopic portals that permitted placement of two cannulas on the anterior surface of the lesser trochanter. The iliopsoas tendon was identified and released from the anterior, medial, and superior edges of the lesser trochanter, and the muscle attachments of the iliopsoas muscle-tendon unit (MTU) were left intact. A prior study has shown that a release performed in this manner maintains the iliopsoas muscle attachments to the lesser trochanter and preserves 40% of the iliopsoas muscle-tendon unit [3].
Our initial study population consisted of the 169 consecutive patients (mean age, 34.7 years; 35 men, 134 women) who had an iliopsoas tenotomy performed at the lesser trochanter. We then reviewed the medical records of these 169 patients to identify those who had both a preoperative and postoperative hip MR arthrogram. This review identified 20 patients who met these criteria and formed our final study population. There was no documented interval trauma or intervention. This population consisted of 5 men and 15 women, with a mean age of 36.9 years (range 16 to 57). The male and female demographics were similar, with the mean age of the male patients 36.4 years (range 20 to 54), and the mean age of the female patients 37 years (range 16 to 57).
The mean time after iliopsoas tenotomy to MR exam was 654 days; 7 MR examinations were performed within 1 year (35%), 8 examinations between 1 and 2 years (40%), and 5 examinations between 3 and 6 years (25%).
The protocol for MR arthrogram of the hip for these studies included: coronal T1-weighted with fat-suppression ( TR 700, TE 8, ETL = 2, matrix 288 × 224, FOV = 18 cm, slice thickness 4 mm with 0.4 mm interslice gap), coronal T2-weighted with fat-suppression (TR 4600, TE 80, ETL = 19, matrix 320 × 224, FOV 18 cm, slice thickness 4 mm with 0.4 mm interslice gap), sagittal T1-weighted with fat-suppression (TR 700, TE 8, ETL = 2, matrix 228 × 224, FOV = 18 cm, slice thickness 4 mm with 0.4 mm interslice gap), oblique axial T1-weighted with fat-suppression (TR 700, TE 8, ETL 2, matrix = 288 × 224, FOV 18 cm, slice thickness 4 mm with 0.4 mm interslice gap), axial T1-weighted ( TR 650,TE 18, ETL 2, matrix 228 × 224, FOV = 18 cm, slice thickness 4 mm with 0.4 mm interslice gap, and axial T2-weighted with fat-suppression (TR 4000, TE 80, ETL 19, matrix 18 × 18, FOV 18 cm, slice thickness 4 mm with 0.4 mm interslice gap) performed after the intra-articular administration of approximately 12 mL of a solution consisting of 5 mL non-ionic iodinated contrast, 5 mL sterile saline, 5 mL of 0.5% ropivacaine, 5 mL 1% preservative free lidocaine, and 0.1 mL of gadolinium contrast. Injection of the intra-articular contrast was performed via an anterior lateral approach utilizing fluoroscopic guidance.
Each postoperative MR arthrogram was evaluated independently by two faculty musculoskeletal radiologists with 10 and 20 years experience in interpreting musculoskeletal MR examinations and one musculoskeletal radiology fellow. Each reviewer compared the postoperative study to the preoperative MR arthrogram to determine if the postoperative study revealed muscle edema with new intramuscular high T2 signal intensity, muscle atrophy (grade 0–4), compensatory hypertrophy (enlargement of the muscles on follow-up MR examination), abnormal signal within the iliopsoas tendon (increased on T1 or T2 sequences), and abnormal iliopsoas tendon morphology (irregularity, distortion) above and below the iliopectineal eminence. We used a previously described grading scale for muscle atrophy as follows: 0 = no fat, 1 = muscles containing some fatty streaks, 2 = fatty infiltration with more muscle tissue than fat, 3 = fatty infiltration with equal amounts of fat and muscle, and 4 = fatty infiltration with more fat than muscle [9].
The iliopsoas tendon was considered distorted if it was thickened or irregular in contour. The tendon was considered disrupted if a gap was seen between the tendon and the lesser trochanter. A tendon could be both disrupted and distorted if a gap was seen distally but the tendon was distorted above the gap. A tendon could be distorted both above and below the iliopectineal eminence. For all the MR evaluations, a finding was considered positive if reported by two or three of the radiologists.
Clinical Evaluation
The second hip MR arthrogram was performed in all 20 patients for recurrent hip pain. The diagnoses on the second hip MR arthrogram included new degenerative cartilage loss in 14 patients (70%), recurrent labral tears in 9 patients (45%) and recurrent labral tears versus postoperative change in 3 patients (15%). Additional MR arthrogram diagnoses included new tendinopathy or tearing of the gluteus medius and/or minimus tendons in 3 patients (15%) and peritrochanteric bursitis in 2 patients (10%).
Clinical assessment was performed utilizing the modified Harris hip scoring system described by Byrd [5] by the hip orthopedic surgeon. This scoring system is based on pain (44 points) and function (47 points). The total score is multiplied by 1.1 for a maximum possible score of 100. All hips were evaluated with Byrd’s 100-point modified hip scoring system (MHHS) prior to the release, at 6 and 12 months after surgery, and at the time of their follow-up MRI.
Postoperatively, patients were enrolled in a three-phase rehabilitation protocol. Goals of phase 1 (surgery to week 4) were pain control, hip protection, and initial range of motion and leg control exercises. Phase 2 (postoperative weeks 4 to 10) focused on gait, functional movements, and performing a single leg stance for greater than 15 s. Goals for phase 3 included returning to sport- and work-related activities with good control and no pain and improving hip flexor strength, with a goal of 90% of the contralateral side.
Statistical Analysis
Radiologic findings were then correlated with clinical outcomes, as measured by the modified Harris hip scores. For statistical analysis, Cohen’s kappa (unweighted) was used to assess inter-reader agreement on binary variables. Separate kappas were computed for each possible pairing of the three readers. To assess overall agreement between the three readers, Light’s kappa [11] was computed; this measure equals the arithmetic average of the three pair-wise kappas. Kappa was not computable if at least one reader rated all subjects as lacking a given finding. Standard error (SE) and 95% lower and upper limits were computed for each kappa. All analyses were obtained in R 2.12.1 [13] with the irr 0.83 package [6]. An analysis of variance (ANOVA) was performed on the three atrophy groups (0–1, 2–3, 4) to compare the Harris hip scores at the time of MRI.
Given the large number of attributes examined, descriptive statistics (minimum, maximum, quartiles, mean, and standard deviation [SD]) were obtained for kappas. This was done for each of the three possible reader pairings (Cohen’s kappa) as well as for all readers combined (Light’s kappa). Generalized estimating equation (GEE) models were used to compare the following above or below the iliopectineal eminence (IPE): (1) iliacus atrophy grade, (2) psoas atrophy grade, (3) iliopsoas distortion, and (4) iliopsoas disruption. These models can account for two kinds of dependence, arising from: (a) each reader grading each subject multiple times and (b) each subject potentially contributing data both above and below the IPE. In all cases, a finding was considered positive if two or more readers agreed on its presence for a given patient. For (1) and (2), a normal family with identity link were used for the GEE models, whereas for (3) and (4) a binomial family with logit link was used instead. In all cases the working correlation structure was specified as independent, and the sandwich covariance estimator was used to calculate the robust standard errors used for inference. P < 0.05 (two sided) was the criterion for statistical significance.
Results
The kappa values for all of the pairings indicated fair interobserver variation according to the grading by Landis and Koch [10]. The mean kappa for interobserver variability was 0.245, with a standard deviation of 0.168. Mean values were similar among all reader pairings (0.312, 0.201, and 0.316). The median value was 0.300 for all readers.
Muscle edema was present on the post-tenotomy hip MR arthrogram within the iliacus muscle in 2 patients, within the psoas muscle in 1 patient, and within the quadratus femoris muscle in 1 patient. Compensatory hypertrophy was not observed post-tenotomy in any of the hip musculature including the rectus femoris, tensor fascia lata, vastus lateralis, vastus medialis and gluteus maximus muscles.
Atrophy (Table 1) was most commonly observed in the iliacus and psoas muscles. Eighty-five percent (17/20) of patients had iliacus atrophy and 75% (15/20) of patients had psoas atrophy (Fig. 1). Iliacus atrophy was more commonly observed below than above the iliopectineal eminence (85% versus 75%) and trended toward a higher grade with an average grade of atrophy of 1.915 below the eminence, as opposed to 1.750 above the iliopectineal eminence. However, this difference was not statistically significant, with a p value of 0.37. Atrophy in the psoas muscle also trended toward a higher degree below in comparison to above the iliopectineal eminence, 2.878 versus 2.585, also not statistically significantly different with a p value of 0.11. However, the severity of the atrophy was greater in the psoas than in the iliacus muscle with a p value < 0.001 both above and below the iliopectineal eminence. Atrophy was less frequently observed in other ipsilateral hip muscles and most often present in the gluteus maximus muscles (Table 1) as illustrated in Fig. 1.
Table 1.
Percent of patients with post-tenotomy hip muscle atrophy on MR and average grade of atrophy
| Muscle | Percentage (%) | Average grade |
|---|---|---|
| Iliacus—AIPE | 65 | 1.750 |
| Iliacus—BIPE | 85 | 1.915 |
| Psoas—AIPE | 75 | 2.585 |
| Psoas—BIPE | 75 | 2.878 |
| Quadratus Femoris | 10 | 1.750 |
| Rectus Femoris | 5 | 2.500 |
| Tensor Fascia Lata | 0 | NA |
| Vastus Lateralis | 5 | 1.500 |
| Vastus Medialis | 0 | NA |
| Gluteus Maximus | 25 | 1.300 |
AIPE above the iliopectineal eminence, BIPE below the iliopectineal eminence
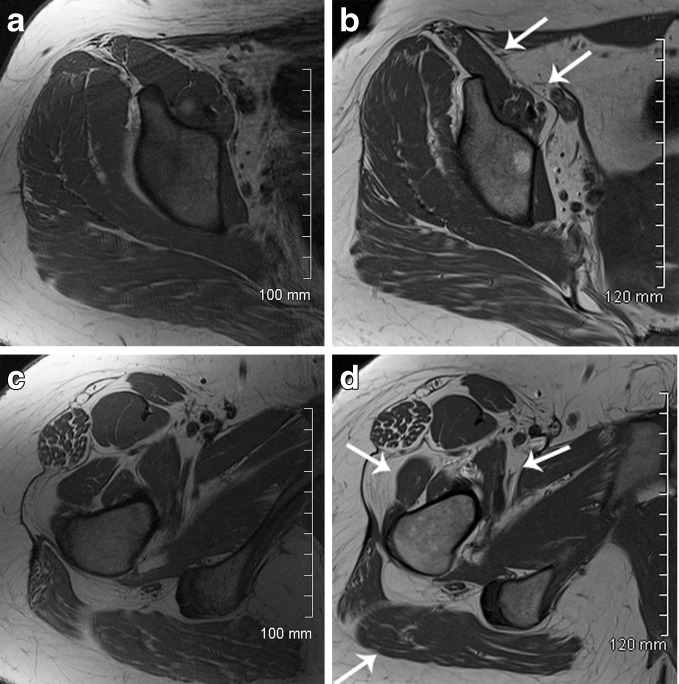
Fig. 1.
40 year old female with right hip pain pre- (a, c) and postoperative (b, d) axial T1 MR arthrogram images demonstrate atrophy of the iliopsoas muscle following arthroscopic iliopsoas tendon release. Atrophy (arrows) was observed both above (B—average grade 1.33) and below (D—average grade 1.67) the iliopectineal eminence. Additionally, postoperative atrophy was observed in the gluteus maximus muscle (average grade 1.5) and vastus lateralis (average grade 1.5) (B). Postoperative imaging was performed approximately 20 months following surgery.
Abnormalities within the iliopsoas tendon were frequently observed, including abnormal intratendinous T1 and T2 signal, distortion, and disruption. Ninety percent (18/20) of patients had increased T1 signal within the residual portion of the iliopsoas tendon (Fig. 2) and 10% (2/20) had increased T2 signal. Thirty-five percent (7/20) of the iliopsoas tendons was disrupted, all below the iliopectineal eminence (Fig. 3). Eighty-five percent (17/20) of the tendons was distorted below the iliopectineal eminence versus 35% (7/20) above the iliopectineal eminence, which was not statistically significant, with a p value of 0.06.
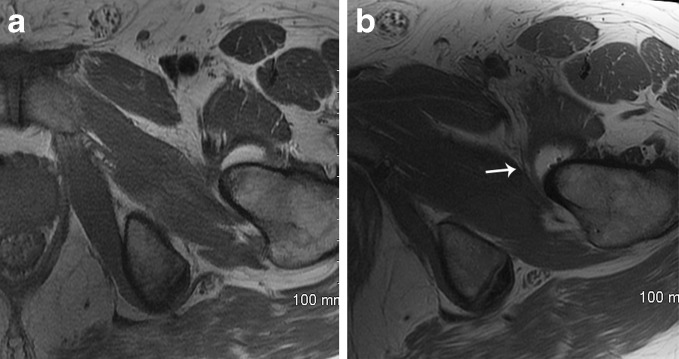
Fig. 2.
Fifty-four-year-old male with left hip pain pre- (a) and postoperative (b) MR arthrogram axial T1 images demonstrate increased T1 and distortion of the iliopsoas tendon (arrow) below the iliopectinal eminence. This patient also had atrophy of the iliacus (average grade 2.33) and psoas (average grade 3.67) below the iliopectineal eminence. Postoperative imaging was performed approximately 3 months following surgery.
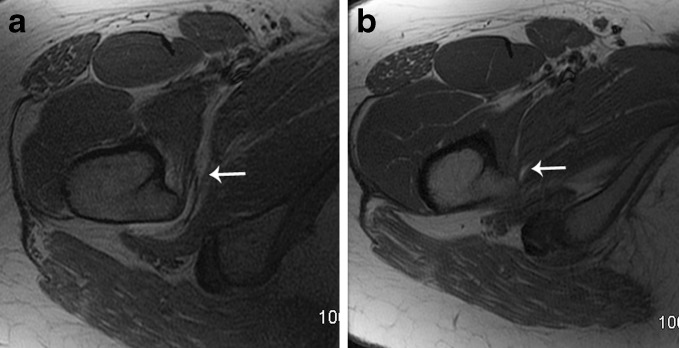
Fig. 3.
Forty-year-old female with right hip pain pre- (a) and postoperative (b) MR arthrogram axial T1 images demonstrate the normal insertion of the iliopsoas tendon preoperatively (a, arrow). Postoperatively, the iliopsoas tendon demonstrated increased T1 signal, distortion, and disruption below the iliopectineal eminence (b, arrow) with no remaining fibers inserting on the lesser trochanter. This patient also had atrophy of the iliacus (average grade 1.67) and psoas (average grade 3.33) below the iliopectineal eminence. Postoperative imaging was performed approximately 8 months following surgery.
Three of the iliopsoas tendons on the post-tenotomy MR arthrogram were graded as without evidence of disruption or distortion when compared to their pre-tenotomy MR arthrogram. None of these 3 tendons had intratendinous T2 signal and only one had intratendinous T1 signal (Fig. 4). A review of the clinical records of these three patients revealed that all were unable to actively flex their hip for 3 to 5 weeks after their tenotomy indicating that a complete release of the iliopsoas tendon had been accomplished. In addition, none of these patients had experienced recurrent snapping of their tendon at the time of their postoperative MRI.
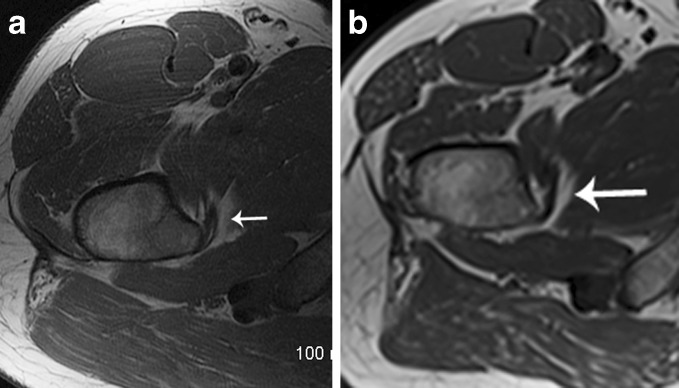
Fig. 4.
Forty-seven-year-old male with right hip pain pre- (a) and postoperative (b) MR axial T1 images demonstrate the normal insertion of the iliopsoas tendon preoperatively (a, arrow). Postoperatively, the iliopsoas tendon remains normal in appearance, with no evidence of abnormal T1 or T2 signal. Additionally, there was no distortion or disruption of the tendon (b, arrow). This patient did have atrophy of the iliacus (average grade 2.00) and psoas (average grade 2.33) below the iliopectineal eminence. Postoperative imaging was performed approximately 22 months following surgery.
Modified Harris hip scores (MMHS) were obtained preoperatively, 3 and 6 months postoperatively, and at the time of the postoperative MRI as a measure of clinical function (Table 2). Patients were grouped based on the highest grade of atrophy observed in either the iliacus or psoas muscle. There was no significant difference in the MMHS relative to the amount of atrophy observed (p = 0.64).
Table 2.
Harris hip scores at the time of the postoperative MRI grouped by severity of iliopsoas muscle atrophy
| Patient | Grade of atrophya | Harris hip score | Post-op months to MRI |
|---|---|---|---|
| 9 | 4 | 100 | 41 |
| 8 | 4 | 95.7 | 36 |
| 10 | 4 | 89.1 | 36 |
| 19 | 4 | 84.7 | 10 |
| 5 | 4 | 81.4 | 3 |
| 6 | 4 | 81.4 | 20 |
| 7 | 4 | 79.2 | 12 |
| 14 | 4 | 78.1 | 22 |
| 18 | 4 | 49.5 | 8 |
| 17 | 4 | 48.4 | 20 |
| 20 | 4 | 38.5 | 9 |
| 3 | 3 | 100 | 5 |
| 11 | 2 | 100 | 42 |
| 2 | 2 | 94.6 | 25 |
| 4 | 2 | 84.7 | 9 |
| 1 | 2 | 81.4 | 63 |
| 15 | 3 | 42.9 | 22 |
| 12 | 1 | 95.7 | 31 |
| 13 | None | 81.4 | 8 |
| 16 | None | 72.6 | 15 |
aHighest grade of atrophy in iliacus or psoas
Discussion
We found that iliacus and psoas muscle atrophy was present in 65% and 85% of our patients, respectively, with the greatest severity of atrophy within the psoas muscles However, there was no significant difference in the modified Harris hip scores of the patients with no atrophy, mild to moderate atrophy, and severe iliacus or psoas muscle atrophy at the time of the post-tenotomy MRI. The majority of the patient’s in the grade 4 atrophy group had good clinical outcomes, with 73% of the patients (8/11) having Harris hip scores that were greater than 75 out of the possible 100 points. These findings suggest that the degree of iliopsoas atrophy is not predictive of clinical function after iliopsoas tenotomy. There was also no edema within the iliacus or psoas muscles even when the post-tenotomy MR arthrogram was performed only 6 months after the tenotomy suggesting that the muscles had reached their baseline status.
Our study has several limitations. The statistical power of the study was limited by the small number of patients who met the inclusion criteria. Statistical differences in the degree of atrophy may have been observed if more patients were included in the study. Our observers had only mild interobserver agreement such that the significant differences in the compared variable might be observer by observer variation. One of the reasons for our low interobserver reliability may be differences in the assessment of subtle changes at MR imaging and the experience of the readers; one reader was a musculoskeletal radiology fellow. A final and important limitation is that all of our patients had repeat MR arthrograms for recurrent hip pain so we do not know if our findings would apply to asymptomatic patients after iliopsoas tenotomy.
We assume that our intensive physical therapy program that focused on regaining hip flexor strength after iliopsoas tenotomy resulted in good hip function despite the reduced hip flexor power that was evident immediately following the iliopsoas tenotomy. We did not find compensatory hypertrophy of other hip muscles in response to this rehabilitation program which we had expected. We hypothesize that the therapy resulted in greater muscle tone and strength but without enlargement when compared to the contralateral hip and pre-tenotomy MR arthrogram.
We had expected that atrophy would occur in the iliacus and psoas muscles after iliopsoas tenotomy as was found in our study. We do not know why atrophy was noted in 25% of the ipsilateral gluteus maximus muscles. Possibly the gluteus maximus atrophy resulted from loss of the normal opposition to hip extension from the iliacus and psoas muscles.
A discrete gap (disruption) was noted on MR in only 35% of the patients after iliopsoas tenotomy. We presume that scar tissue formed at the tenotomy site simulates a distorted tendon. Interestingly, three (15%) of the distal iliopsoas tendons showed no post-tenotomy distortion which suggests that the post-tenotomy scarring closely followed the original course of the tendon. In addition only one of these three tendons had abnormal intratendinous signal. Those interpreting hip MR arthrograms after iliopsoas tenotomy should be aware that the tendon may appear normal on MR imaging.
Another unexpected finding was that 35% of the iliopsoas tendons was distorted above the iliopectineal eminence. Since the tenotomy is performed at the lesser trochanter, we postulate that tendon retraction resulted in the distortion considerably above the location of the tenotomy.
Iliacus and psoas muscle atrophy occur after arthroscopic iliopsoas tenotomy, but in our patient population, this atrophy was not associated with a significant decrease in hip function. In a minority of the patients (15%), the iliopsoas tendon appeared normal on MR imaging despite the presence of iliacus or psoas muscle atrophy.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgments
Disclosures
Conflict of Interest: Alejandro Munoz del Rio, PhD receives payments from Lippincott Williams & Wilkins to perform statistical reviews of articles submitted to “Annals of Surgery”.
Kendra S. Hain, MD, Donna G. Blankenbaker, MD, Arthur A. De Smet, MD, James S. Keene, MD have declared that they have no conflict of interest.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent: Informed consent was waived from all patients for being included in the study.
Required Author Forms: Disclosure forms from provided by authors are available with the online version of this article.
Footnotes
Level of Evidence: Therapeutic Study Level IV. Please see “Levels of Evidence” for a complete description.
References
- 1.Anderson SA, Keene JS. Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med. 2008;36:2363–2371. doi: 10.1177/0363546508322130. [DOI] [PubMed] [Google Scholar]
- 2.Blankenbaker DG, De Smet AA, Keene JS. Sonography of the iliopsoas tendon and injection of the iliopsoas bursa for diagnosis and management of the painful snapping hip. Skeletal Radiol. 2006;35:565–571. doi: 10.1007/s00256-006-0084-6. [DOI] [PubMed] [Google Scholar]
- 3.Blomberg JR, Zellner BS, Keene JS. Cross-sectional analysis of iliopsoas muscle-tendon units at the sites of arthroscopic tenotomies. Am J Sports Med. 2011;39(Suppl):58–63. doi: 10.1177/0363546511412162. [DOI] [PubMed] [Google Scholar]
- 4.Deslandes M, Guillin R, Cardinal E, Hobden R, Bureau NJ. The snapping iliopsoas tendon: new mechanisms using dynamic sonography. AJR Am J Roentgenol. 2008;190:576–581. doi: 10.2214/AJR.07.2375. [DOI] [PubMed] [Google Scholar]
- 5.Flanum ME, Keene JS, Blankenbaker DG, Desmet AA. Arthroscopic treatment of the painful “internal” snapping hip: results of a new endoscopic technique and imaging protocol. Am J Sports Med. 2007;35:770–779. doi: 10.1177/0363546506298580. [DOI] [PubMed] [Google Scholar]
- 6.Gamer M, Lemon J, Fellows I, Singh P. irr: Various Coefficients of Interrater Reliability and Agreement, R package version 0.83. In: http://CRAN.R-projectorg/package=irr; 2010.
- 7.Ilizaliturri VM, Jr, Villalobos FE, Jr, Chaidez PA, Valero FS, Aguilera JM. Internal snapping hip syndrome: treatment by endoscopic release of the iliopsoas tendon. Arthrosc J Arthrosc Relat Surg. 2005;21:1375–1380. doi: 10.1016/j.arthro.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 8.Ilizaliturri VM, Jr, Chaidez C, Villegas P, Briseno A, Camacho-Galindo J. Prospective randomized study of 2 different techniques for endoscopic iliopsoas tendon release in the treatment of internal snapping hip syndrome. Arthroscopy. 2009;25:159–163. doi: 10.1016/j.arthro.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Khoury E, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscule: sonography versus MR. Am J Roentgenol. 2008;190:1105–1111. doi: 10.2214/AJR.07.2835. [DOI] [PubMed] [Google Scholar]
- 10.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 11.Light RJ. Measures of response agreement for qualitative data: some generalizations and alternatives. Psychol Bull. 1971;76:365–377. doi: 10.1037/h0031643. [DOI] [Google Scholar]
- 12.Taylor GR, Clarke NM. Surgical release of the 'snapping iliopsoas tendon'. J Bone Joint Surg Br. 1995;77:881–883. [PubMed] [Google Scholar]
- 13.Team RDC. R: A language and environment for statistical computing. In: R Foundation For Statistical Computing. Vienna, Austria: ISBN 3-900051-07-0; 2009.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)