Abstract
Background
Among golf injuries, low back pain (LBP) is the most common compliant for both professional and amateur golfers. Hip rotational range of motion (ROM) might be related to LBP in those who repeatedly place specific activity rotational demands on the hip in one direction. Coordination of timing of movement (neural control) between the hip and lumbopelvic region during trunk movements is critical for normal mechanics. Altered timing can contribute to areas of high tissue loading and can lead to LBP symptoms seen during active lower limb movement tests. Patient was a 42-year-old male recreational golfer who presented with low back pain and decreased hip internal rotation ROM.
Methods
With the use of manual physical therapy to increase hip ROM and lumbar stabilization therapeutic exercises, the patient was able to return to pain-free golf and to better his handicap by three strokes.
Results
Significant improvement was seen in his Oswestry outcome score, and a (−) prone instability test was noted.
Conclusion
It is recommended to address hip ROM limitations in those experiencing low back pain while golfing. Rapid spinal rotation may produce large spinal loads, but this is likely not the major contributor to low back pain in golfers. Mechanical factors may play a larger role.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-013-9353-9) contains supplementary material, which is available to authorized users.
Keywords: prone instability test, hip ROM, golfer, LBP, stabilization
Introduction
In the sport of golf, the swing requires extreme rotational ranges of motion (ROMs) involving the trunk and lower extremities, especially the hips. Among golf injuries, low back pain (LBP) is the most common complaint for both professional and amateur golfers [21]. Golfers with a history of LBP also experienced their LBP while performing activities of daily living such as walking, standing, or sitting [5]. Activities that require hip rotation such as a golf swing or a racquet sport could result in an increased and out-of-sync lumbopelvic motion [10].
The golf swing produces considerable mechanical forces through compressive, shear, and rotational movements to the lumbar spine due to rapid trunk bending and rotation [13]. Compression forces of up to eight times body weight and 80% more shear forces have been reported in the right lumbar spine of a right-handed professional golfer. Lead leg lateral compression force of 133 N, vertical compression force of 950 N, and 23-N rotatory torques have been measured 0.02 s after a ball impact [1].
Suboptimal function of the hip might result in an alteration of the mechanics of the lumbopelvic region. Hip muscle strength is considered to be an important factor in lumbopelvic-hip stability, and deficits are a risk factor for LBP [23, 24]. Limited hip ROM due to shortened muscles, restricted capsule, or a boney abnormality (musculoskeletal factors) can contribute to altered movements in the lumbopelvic region [4]. Those who play golf are at an increased risk for LBP if there hip rotation is limited [10]. Hip rotational ROM is related to LBP in those who repeatedly place specific rotational demands on the hip in one direction [22, 29, 30]. An asymmetry in hip rotatory ROM would result in an asymmetry in the forces transmitted to the lumbopelvic region, which have been identified as a risk factor for LBP [17, 18]. A potential compensation for limited hip ROM is increased lumbopelvic rotational motion [17, 18]. This increase in the demands placed on the lumbar spine may lead to lumbar segmental instability (LSI). LSI has been defined as a condition in which there is a loss of stiffness between spinal motion segments, such that normally tolerated external loads result in pain or deformity or place neurological structures at risk [7]. LSI has traditionally been diagnosed with the use of lateral flexion and extension radiographs [15, 25, 33], but the prone instability test [11] is also a useful physical examination tool. Two authors have produced a classification scheme which subgroups patients with low back pain into one of four treatment categories [6, 11]. These include manipulation and exercise, activities to promote centralization, stabilization exercises, and traction. This treatment approach cannot be applied in a straightforward fashion when a patient, especially a golfer, fits into the stabilization category for LBP but also would benefit from mobilization of the joints below the spine.
Coordination of timing of movement (neural control) between the hip and lumbopelvic region during trunk movements is critical for normal mechanics. Altered timing can contribute to areas of high tissue loading and can lead to LBP symptoms seen during active lower limb movement tests (hip lateral rotation with knee flexed to 90° and knee flexion) performed in prone [27, 31, 32]. The movements during the golf swing are somewhat unique due to the fact that the spine rotates over the fixed femur. Muscle activation sequencing should be performed in a functional position for the most carry-over to the sport of golf. Previous studies have reported that male professional tennis players and golfers with LBP were more limited in lead hip medial rotation and had a (+) flexion, abduction, external rotation (FABER) test than those without LBP [29]. These previous studies measured hip rotational ROM and when lumbopelvic motion occurred in a non-weight-bearing prone position with the femur moving relative to the pelvis, which may not carry over to as functional as golf. One study by Gulgin et al. measured hip rotation in a weight-bearing position with the use of motion analysis and a custom-built base so that one foot was fixed, while the other was rotating on a disk [8, 9]. The purpose of this case report is to illustrate an example of how LBP can be addressed by focusing on improving hip rotational ROM using hip mobilizations and manual therapy and lumbar functional stabilization exercises which have been adopted specifically for the golfer.
Case Description
The patient is a 42-year-old male accountant who plays golf two to three times a week with clients during the golf season. He was referred for physical therapy by his orthopedist after a brief work-up for low back pain. He had undergone an MRI of his lumbar spine and right hip which documented degenerative disk disease and a cam-type femoroacetabular impingement of his right hip. At the initial physical therapy evaluation, he reported he had a long history of low back pain that has not limited his activity at all and is episodic in nature with no other significant past medical history. Pt reported that this episode of right low back pain began after increasing his activity level and playing more rounds of golf per week. He is a right-handed golfer. He reported that his pain was most significant during rounds of golf as well as during the night and following day after play. The pain was on the right side of his lumbar region with radiation down into his buttock and posterior hip and was interfering with activities of daily living with posterior buttock pain developing with sitting for periods of more than 30 min. He reported occasional groin pain especially after two consecutive days of golfing. He described the pain as sharp, deep, and burning in the right inferior buttock region with associated spasms. The pain was made worse with bending forward and occasionally requiring him to use his hand on his knees (Gower's sign [5]) to bring himself upright. He had mild positional pain at night that decreased with a change of position. He rated his worst pain on a verbal analog pain rating scale to be 5/10.
During the initial physical therapy examination, observation of standing posture indicated a slight right thoracic, left lumbar scoliosis with a swayback posture. Gait observation showed decreased trunk rotation with increased right leg external rotation noted by being able to see the patient's big toe on his right from a posterior view. With ROM testing, he was limited in lumbar spine left side bending by 30% with pain and left rotation by 25% with discomfort in his right lumbar spine and right groin. This 25% deficit in rotational ROM was also observed through his thoracic spine with left rotation. He demonstrated a right lateral aberrant movement going from flexion to extension. His right hip internal rotation (IR) ROM was 10°; external rotation (ER) was 45°; and left hip IR was 18°, and ER was 50° measured prone. Light touch and neurological testing was negative. Manual muscle testing showed right hip flexion, abduction, extension, and IR and ER strength to be 4−/5. Palpation reveled tenderness and trigger points to right quadrates lumborum, piriformis, gluteus medius insertion, and adductors. Lumbar spine segmental spring testing demonstrated hypomobility at L4–L5, hypermobility at L1–L3, and pain with compression of his right SI joint; (+) FADIR, (+) FABER, (+) prone instability test, (+) Thomas test on the right, and a (+) active straight leg raise (ASLR) test were noted [19, 20]. Patients score on the modified Oswestry was 30%.
Based on the patient's examination, he was felt to be most consistent with Hicks stabilization classification for LBP [11]. His plan of care over nine sessions included lumbar stabilization, right hip mobilization and manual therapy, hip strengthening, and proper muscle functional sequencing patterning to return this patient to pain-free golf. Initially, his treatment began with right hip trigger point releases in his adductors, gluteal muscles, and piriformis. Each trigger point was held for 30 s and repeated until the tenderness was no longer palpable, an average of three sets. Soft tissue release with distal movement was used for right hip adductors and gluteus medius to diminish soft tissue restrictions to IR ROM. Each release was done for eight to ten repetitions. Mobilization with movement was used to address capsular restrictions to right hip IR with the use of a lateral distraction belt with applied flexion and IR for ten repetitions (Fig. 1). These manual therapy techniques were followed by hip IR/ER self-ROM stretching in a functional position on a swivel board (towel for home) as a home exercise program (Fig. 2). Decreased rotation noted from the hip to the thoracic spine leads to the use of thoracic muscle energy seated to assist in firing his left serratus anterior in order to gain an increased thoracic left rotation through the muscle pull (Fig. 3.) These soft tissue techniques and mobilizations were done each PT session.
Fig. 1.

Lateral hip distraction with mobilization belt.
Fig. 2.

Hip internal/external rotation on a swivel board. Pelvis is kept level, while lower extremity rotates on a moveable disk.
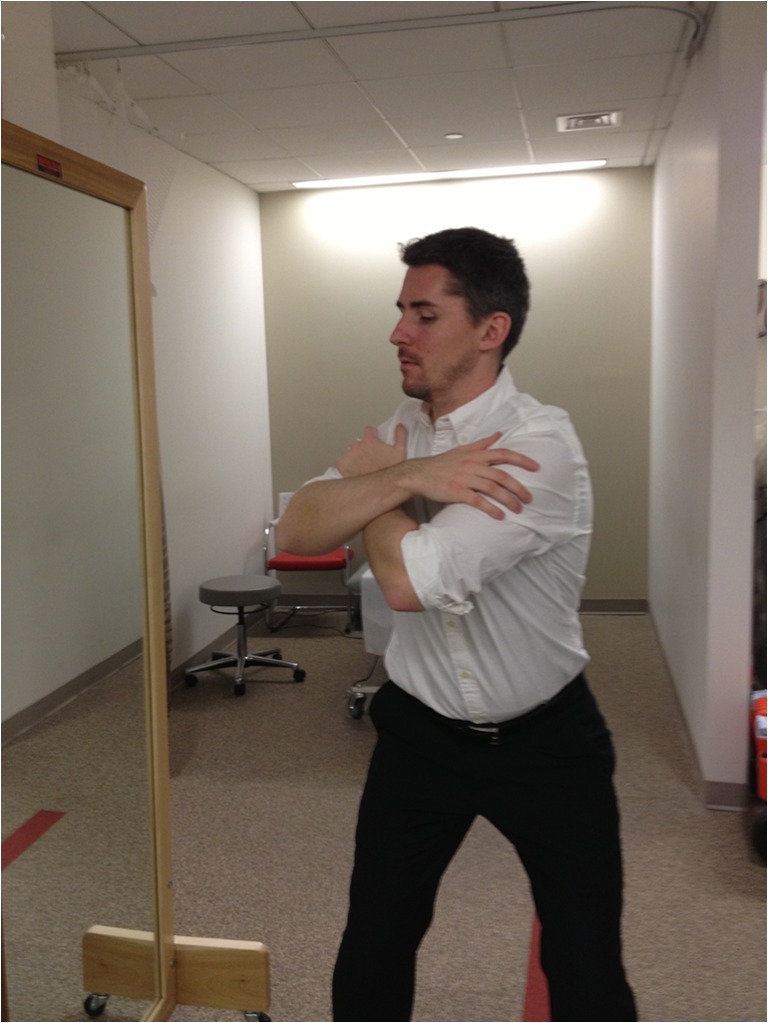
Fig. 3.

Thoracic spine seated rotation. Increased thoracic spine rotation through the use of agonist–antagonist muscle activations.
Lumbar spinal stabilization began supine and progressed to standing over the course of the PT sessions. Supine abdominal bracing was initiated to educate the patient on the proper activation of deep core musculature without spinal movement and as a basis for all future exercises [26]. Bridging, side bridges, and bird dog exercises were then initiated which have all been shown to produce deep lumbar stabilization [3, 14]. Once he demonstrated good control with these exercises, he was progressed to standing and golf-related positions for muscle sequencing.
Standing core progression began in golf stance with his arms crossed to provide a short lever arm for core activation. Dissociation of the trunk and pelvis is critical to the success of the timing of one's golf swing and the decrease for poor mechanics and risk of injury. The patient was instructed on moving his trunk into a backswing position followed by his hips and returning to neutral (forward position) by activating his abdominals first then left hip rotation by gluteal activation to allow his hips to move first as he would in initiating the downswing in golf (Fig. 4). This was progressed with his arms placed straight out in front of him, creating a long lever arm just as in golf. He was then progressed to a windmill exercise, which produces a similar joint movement as seen in the golf swing of the pelvis moving over the relatively fixed femur (Fig. 5). This exercises also educated the patient on proper hip hinging with lumbar stabilization that was then used as a technique in retrieving the ball from the cup or placing his ball on a tee.
Fig. 4.
Trunk on hips on trunk. Ability to rotate the trunk over the stable pelvis and the pelvis under the stable trunk.
Fig. 5.

Windmill. Trunk and pelvis rotating on a relatively fixed lower extremity.
Once he was able to demonstrate a good control with the previous two exercises, he was progressed to two more exercises that built his power and continued to work on trunk/hip sequencing. The first exercise was a half–tall kneeling chop (Fig. 6) that worked in diagonal patterns just as in the downswing and follow-through of a golf swing. He was cued in proper deep abdominal stabilization with movement initiating from his hips and not lumbar spine with decreased lumbar spine extension and side bending. Once he was able to demonstrate a good technique, a 3-lb medicine ball was added to build power into this functional golf swing-based exercise. With two physical therapy sessions left, he was instructed in an exercise using two dowels called double parallel swing to bring all the exercise dimensions together into a functional golf warm-up (Fig. 7). Beginning in golf stance with abdominal bracing, holding a dowel in each hand pointing toward the ground, he was instructed to bring both dowels into his backswing keeping them shoulder width apart and parallel to one another without letting his arms bend and keeping his shoulders level. Once in the backswing, he initiated his left gluteal muscles to begin his downswing and rotate his body keeping his hips and shoulders level with the movement coming from his hips first. His deep core activation created rotational movements throughout his hips and trunk with decreased shear and side-bending motions occurring especially on the right lumbar spine as he swung into his follow-through keeping the dowels parallel to one another and stopping when the dowels were parallel to the ground. Sequencing with stabilization was progressed with this exercise, stopping at points throughout the swing with holds for 10s in the proper posture, building muscular endurance throughout the entire swing. This exercise became a fundamental routine as part of his warm-up on the golf course. On his last session, he demonstrated independence with all exercises with a good form and proper sequencing.
Fig. 6.

Half-kneeling medicine ball chops. Arms are kept in front of the trunk as trunk rotates over the stable pelvis.
Fig. 7.

Double club parallel swing. Trunk and hips remain square as clubs are rotated into backswing and follow-through by way of trunk rotation.
The patient was reevaluated on the ninth session of PT. He reported that he had been able to play pain-free golf in multiple days in a row, and his handicap has improved by two to three strokes. He had no pain with sitting at his desk at work. His lumbar and thoracic spine ROM improved to only a 10% deficit in left side bending and left rotation. Right Hip IR ROM was 15°, and ER, 50°. Manual muscle testing showed right hip flexion, abduction, extension, and IR and ER strength to be 4+/5. He had a (−) prone instability test and a (−) ASLR. His modified Oswestry improved to 10%, which met the minimal clinically important difference of six points on this outcome measure [2]. The patient was discharged on this visit with written instructions for his home exercise program and pre-golf warm-up routine. The patient was contacted 6 months after the treatment. He returned a completed modified Oswestry questionnaire, and his score was 7%, suggesting the ongoing benefit of his home stabilization exercise program.
Discussion
Low back pain is a major hindrance to a golfer. Those who experience pain are unable to perform to their highest level during their game. Historically, those who experience pain, golfer or not, ask the question: Where is causing the pain? This question has an extreme importance in the golfing world, where limited hip rotation has been shown to affect lumbar spine mechanics [23, 24]. The question of lumbar spine pain as a result of first altered hip mechanics and decreased range of motion or a loss of hip range of motion as a protective instinct for lumbar spine pain has yet to be determined. The cause and symptoms of lumbar spine pain is an evolving topic within the realm of physical therapy, in which experts are continuously trying to classify into subgroups for proper interventional care [11, 12].
Physical characteristics such as weak trunk extension and reduced non-lead side hip motion with weakness of lead side hip adductors can fail to adequately stabilize the pelvis in the downswing weight-bearing position [28]. An inability to adequately stabilize and decelerate the torque generated throughout the golf swing can lead to compensations and altered body mechanics, especially seen in the lumbar spine. Physical therapists have an increased responsibility to pay attention to these compensations and teach proper sequencing and alignment to reduce the risk of injury.
No significant differences have been observed in spinal and hip rotation velocities between golfers with and without history of LBP. Hip rotational velocities have been measured up to 498°/s [1]. This may indicate that although rapid spinal rotation may produce large spinal load, rapid rotation is not the sole contributor to LBP injuries of golf [16]. This case provides evidence that the forces generated by the golf swing alone are not likely to cause injury, but underlying factors such as decreased hip rotation and inadequate spinal and core stabilizers increase the risk of injury.
Conclusion
Physical therapists working with golfers must be fully aware of all contributing factors to low back pain. Testing patients in functional positions is critical to the understanding and carry over to the recreational sport, in this case, golf. Decreased hip range of motion can place undue stress on the lumbar spine during a golf swing that will lead to altered body mechanics and potential injury. Golf, like other rotational sports, has multiple moving segments at once, increasing the likelihood for compensations to occur. Minimizing those compensations with sound body mechanics is critical for injury reduction and prevention. Proper exercises that teach sequencing combined with stabilization is vital to the health of a golfer.
Electronic Supplementary Material
(PDF 935 kb)
Disclosures
Conflict of Interest:
Gregory Reinhardt, PT, MSPT, has declared that he has no conflict of interest.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent:
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Barrentine SW, Fleisig GS, Johnson H. Woolley TW. Ground reaction forces and torques of professional and amateur golfers. Science and Golf II: Proceedings of the World Scientific Congress of Golf. London E & FN Spon. 1994; 33–9.
- 2.Bendelba M, Torgerson WS, Ling DM. A validated, practical classification procedure for many persistent low back pain patients. Pain. 2000;87:88–97. doi: 10.1016/S0304-3959(00)00278-5. [DOI] [PubMed] [Google Scholar]
- 3.Callaghan JP, Gunning JL, McGill SM. Relationship between lumbar spine loads and muscle activity during extensor exercises. Phys Ther. 1998;78:8–18. doi: 10.1093/ptj/78.1.8. [DOI] [PubMed] [Google Scholar]
- 4.Cibulka MT, Sinacore D, Cromer GS, et al. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint pain. Spine. 1998;23:1009–1015. doi: 10.1097/00007632-199805010-00009. [DOI] [PubMed] [Google Scholar]
- 5.Delitto A, Erhard RE, Bowling RW. A treatment based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–89. doi: 10.1093/ptj/75.6.470. [DOI] [PubMed] [Google Scholar]
- 6.Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: Evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37:290–302. doi: 10.2519/jospt.2007.2498. [DOI] [PubMed] [Google Scholar]
- 7.Frymoyer JW, Selby D. Segmental Instability. Rationale for treatment. Spine. 1985;10:280–6. doi: 10.1097/00007632-198504000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Gulgin H, Armstrong A, Gribble P. Passive hip rotation range of motion in LPGA golfers. Clinical Kinesiology. 2008;62:9–15. [Google Scholar]
- 9.Gulgin H, Armstrong C, Gribble P. Weight-bearing hip rotation range of motion in female golfers. NAJSPT. 2010;5:55–62. [PMC free article] [PubMed] [Google Scholar]
- 10.Harris-Hayes M, Sahrmann SA, Van Dillen LR. Relationships between the hip and low back pain in athletes who participate in rotation-related sports. J Sports Rehabil. 2009;18:60–75. doi: 10.1123/jsr.18.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hicks G, Fritz J, Delitto A, McGill S. Preliminary development of a clinical prediction rule for determining when patients with low back pain will respond to stabilization exercise program. Arch Phys Med Rehabil. 2005;86:1753–1761. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 12.Hicks G, Fritz J, Delitto A, Mishock J. Inter-rater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84:1858–64. doi: 10.1016/S0003-9993(03)00365-4. [DOI] [PubMed] [Google Scholar]
- 13.Hosea TM, Gatt CJ, Gertner E. Biomechanical analysis of the golfer's back. In: Stover CN, McCarroll JR, Mallon WJ, editors. Feeling up to Par: medicine from tee to green. Philadelphia, PA: F.A. Davis Company; 1994. pp. 97–108. [Google Scholar]
- 14.Juker D, McGill SM, Knopf P, Steiffen T. Quantitative intramuscular myoelectric activity of lumbar portions of psoas and the abdominal wall during a wide variety of tasks. Med Sci Sports Exerc. 1998;30:301–10. doi: 10.1097/00005768-199802000-00020. [DOI] [PubMed] [Google Scholar]
- 15.Knutsson F. The instability associated with disk degeneration in the lumbar spine. Acta Radiol. 1944;25:593–609. doi: 10.3109/00016924409136488. [DOI] [Google Scholar]
- 16.Lindsay D, Horton J. Comparison of spine motion in elite golfers with and without low back pain. J Sports Sci. 2002;20:599–605. doi: 10.1080/026404102320183158. [DOI] [PubMed] [Google Scholar]
- 17.Marras WS, Lavender SA, Leurgans SE, et al. Biomechanical risk-factors for occupationally related low-back disorders. Ergonomics. 1995;38:377–410. doi: 10.1080/00140139508925111. [DOI] [PubMed] [Google Scholar]
- 18.Marras WS, Lavender SA, Leurgans SE, et al. The role of dynamic three-dimensional trunk motion in occupationally-related low back disorders. The effects of workplace factors, trunk position, and trunk motion characteristics on risk of injury. Spine. 1993;18:617–28. doi: 10.1097/00007632-199304000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Martin RL, Irrang JJ, Scheyar JK. The diagnostic accuracy of a clinical examination in determining intraarticular hip pain for potential hip arthroscopy candidates. Arthroscopy. 2008;21:1013–18. doi: 10.1016/j.arthro.2008.04.075. [DOI] [PubMed] [Google Scholar]
- 20.Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy. 2006;22:1304–11. doi: 10.1016/j.arthro.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 21.McCarroll JR. The frequency of golf injuries. Clin Sports Med. 1996;15:1–7. [PubMed] [Google Scholar]
- 22.Mellin G. Correlation of hip mobility with degree of back pain and lumbar spinal mobility in chronic low back pain patients. Spine. 1988;13:668–670. [PubMed] [Google Scholar]
- 23.Nadler SF, Malanga GA, Bartoli LA, Feinberg JH, Prybicien M, DePrince M. Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med Sci Sports Exerc. 2002;34:9–16. doi: 10.1097/00005768-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Nadler SF, Malanga GA, DePrince M, Stitik TP, Fienberg JH. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sports Med. 2000;10:89–97. doi: 10.1097/00042752-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Posner I, White AA, 3rd, Edwards WT, Hayes WC. A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine. 1982;7:374–89. doi: 10.1097/00007632-198207000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Sahrmann S. Diagnosis and treatment of movement impairment syndromes. St. Louis, MO: Mosby; 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scholtes SA, Gombatto SP, Van Dillen LR. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clinical Biomechanics. 2009;24:7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsai YS, Sell TC, Smolgia JM, Myers JB, Learman KE, et al. A comparison of physical characteristics and swing mechanics between golfers with and without history of low back pain. J Orthop Sports Phys Ther. 2010;40:430–8. doi: 10.2519/jospt.2010.3152. [DOI] [PubMed] [Google Scholar]
- 29.Vad VB, Bhat AL, Basrai D, Begeh A, Gebeh A, et al. Low back pain in professional golfers. The role of associated hip and low back range-of-motion deficits. Am J Sports Med. 2004;32:494–7. doi: 10.1177/0363546503261729. [DOI] [PubMed] [Google Scholar]
- 30.Van Dillen LR, Bloom NJ, Gombatto SP, Susco TM. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport. 2008;9:72–81. doi: 10.1016/j.ptsp.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Effect of active limb movements on the symptoms in patients with low back pain. J Orthop Sports Phys Ther. 2001;31:402–13. doi: 10.2519/jospt.2001.31.8.402. [DOI] [PubMed] [Google Scholar]
- 32.Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom NJ. The effect of modifying patient—preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys med Rehabil. 2003;84:313–22. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 33.White AA, Panabi MM. Clinical Biomechanics of the spine. 2. Philadelphia: JB Lippincott; 1990. pp. 23–45. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 935 kb)


