Abstract
Immunoglobulin G4 (IgG4)-related sclerosing disease is rare and is known to involve various organs. We present a case of histologically proven IgG4-related sclerosing disease of the small bowel with imaging findings on computed tomography (CT) and small bowel series. CT showed irregular wall thickening, loss of mural stratification and aneurysmal dilatation of the distal ileum. Small bowel series showed aneurysmal dilatations, interloop adhesion with traction and abrupt angulation.
Keywords: IgG4-related sclerosing disease, Autoimmune pancreatitis, Small bowel, Ileum
INTRODUCTION
Immunoglobulin G4 (IgG4)-related sclerosing disease is a rare disease entity that is known to involve various organs including the pancreas, biliary tree, salivary gland, retroperitoneum, kidneys, and so on (1). Its etiology is still unclear and it is composed of many disorders that have specific clinical, pathological, and serologic features (2). Few studies have been done on IgG4-related sclerosing diseases involving the gastrointestinal tract. So far, there has been only one report of IgG4-related sclerosing diseases arising in the small bowel, and it is mainly described in the histopathologic findings (3). In this paper, we report a case of histologically proven IgG4-related sclerosing disease involving the ileum with imaging findings on CT and small bowel series. This report is, to our knowledge, the first to describe the radiologic findings of IgG4-related sclerosing diseases of the small bowel.
CASE REPORT
A 43-year-old man was admitted to our hospital with a one-year history of intermittent abdominal pains. He had a past medical history of acute myocardial infarction 10 years ago and a six-month history of benign prostatic hyperplasia. The physical examination revealed tenderness in the lower right quadrant of the abdomen.
The laboratory tests at presentation showed mild leukocytosis (10470/uL) with an elevated neutrophil percentage (79.6%) and an elevated C-reactive protein value (50.6 mg/L). The serum eosinophil count was in normal range (1.8%). The serum IgG4 level was not available in this case. A plain abdominal radiograph demonstrated no remarkable findings (not shown).
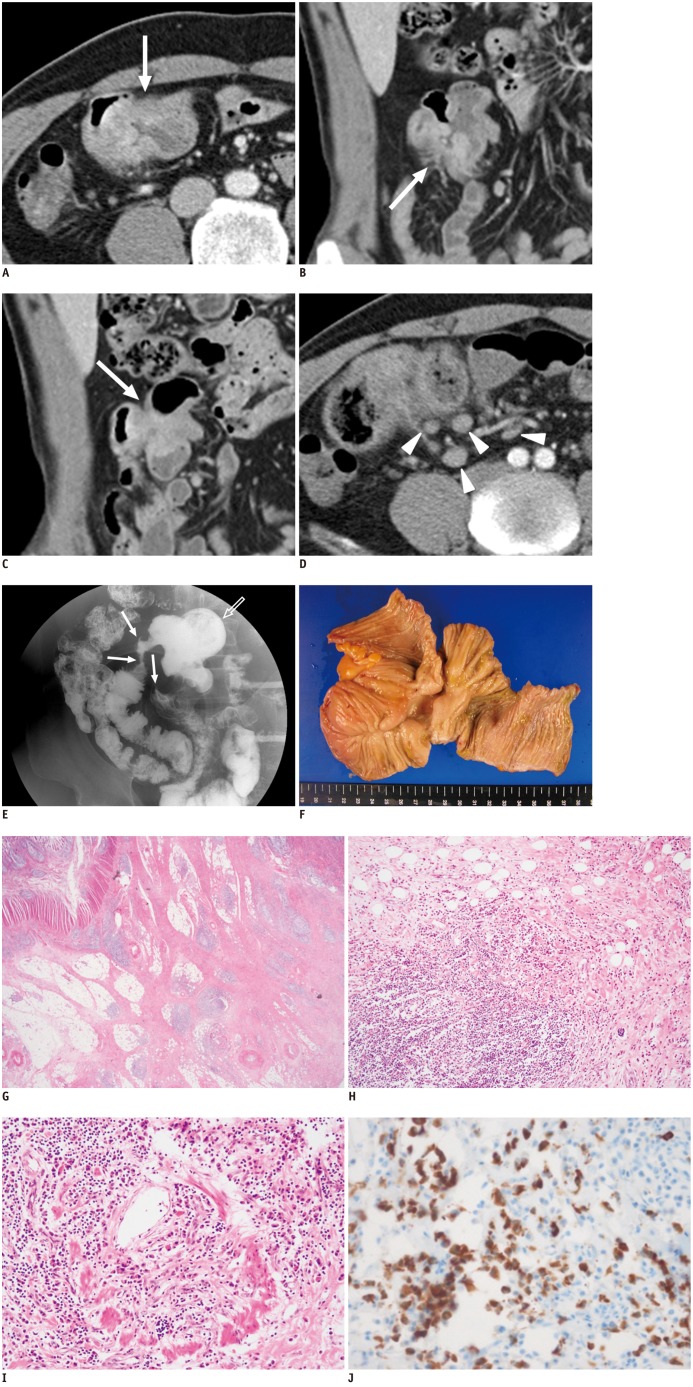
Contrast-enhanced abdominal CT with a 64-row MDCT (Sensation 64, Siemens Medical Solutions, Malvern, PA, USA) showed irregular wall thickening, losses of mural stratification and aneurysmal dilatation of the distal ileum (Fig. 1A, B). Furthermore, adhesion and aggregation of distal ileal loops were also seen (Fig. 1C). There were multiple enlarged lymph nodes (maximal diameter: 1.5 cm) around the distal ileum (Fig. 1D).
Fig. 1.
CT, small bowel series, and histologic findings in 43-year-old man with IgG4-related sclerosing disease of small bowel.
Contrast-enhanced axial (A) and coronal-reformatted (B) CT images show irregular thickening, loss of mural stratification and heterogeneous enhancement of distal ileal wall (arrows). Lesion also reveals aneurysmal dilatation. Another coronal-reformatted CT image (C) shows adhesion and aggregation of few small bowel loops (arrow). Another axial CT image (D) reveals multiple enlarged lymph nodes (arrowheads). Small bowel series (E) shows aggregation of distal ileum with traction, angulation and abrupt narrowing which indicates adhesion of ileal loops (arrows). Aneurysmal dilatation of involved segment is also noted (open arrow). On gross specimen (F) obtained from segmental bowel resection, resected ileum shows depressed lesion (4 × 3 cm) with thickened and edematous wall, forming interloop adhesion. On microscopic examination (G-I), ill-demarcated fibrotic lesion involving submucosa, muscle layer and serosa is seen with prominent lymphoplasmacytic infiltrate (G, Hematoxylin & Eosin, × 10). Lymphoplasmacytic infiltrates occasionally show germinal centers (H) and obliterative phlebitis is present (I). Immunohistochemical stain (J) reveals many IgG4-positive plasma cells (more than 50/high power field).
Small bowel series showed similar findings to those from the CT. Aneurysmal dilatation and multifocal narrowing of the distal ileum were also seen. Adhesion of the bowel loops with traction and abrupt angulation were also revealed (Fig. 1E). There were no significant abnormal findings in the other GI tracts. Clinically and radiologically, there were no significant abnormal findings in other organs.
The clinical and radiologic findings were somewhat confusing and non-specific because their sum can suggest both malignancy and benign inflammatory diseases, and are not specified to one category. The patient underwent exploratory laparoscopy. At surgery, the distal ileum showed segmental wall thickening and edematous wall with interloop adhesions. A segment of the distal ileum was resected. Regional lymph nodes dissection and appendectomy were also performed.
Pathological study confirmed the diagnosis of IgG4-related sclerosing disease, which showed intramural chronic inflammation with prominent IgG4 rich-lymphoplasmacytic infiltrates [IgG4 positive cells > 50/high power field (HPF)], fibrosis, and obliterative phlebitis (Fig. 1F-J).
The patient's post-operative course was uneventful. The patient was discharged on day 9 in good condition with regular follow-ups in the surgical outpatient clinic.
DISCUSSION
Autoimmune pancreatitis was first described in 1995 (4). Since 2003, extra-pancreatic manifestations have been reported and the disease has been recognized as a systemic disease (5). The disease is now commonly referred to as IgG4-related sclerosing disease, with similar histopathologic features in various organs characterized by sclerosing inflammation involving numerous IgG4-positive plasma cells (6). Autoimmune pancreatitis is now considered as part of the IgG4-related sclerosing disease spectrum.
Clinically, patients with autoimmune pancreatitis are usually presented with jaundice or mild abdominal discomforts. Patients with IgG4-related sclerosing disease without pancreatic involvements can manifest various symptoms and signs according to the involved organs. Laboratory findings including elevated IgG and IgG4 serum levels and autoantibodies such as ANA and the rheumatoid factor are helpful in the diagnosis of IgG4-related sclerosing disease. The histolopathological hallmark of the disease is the large number of IgG4-positive plasma cells in the tissue. Cheuk and Chan (7) recently proposed a diagnostic criteria of > 50 IgG4 + plasma cells per HPF and an IgG4 +/IgG + ratio > 40%, which our patient fulfilled. Other important histopathologic findings include lymphoplasmacytic infiltration, sclerosis without cellular myofibroblastic proliferation, and phlebitis (8, 9). Patients usually show dramatic responses to corticosteroid (10, 11).
Various organs can involve IgG4-related sclerosing diseases: the pancreas, salivary glands, hepatobiliary tract, orbit, lymph nodes, aorta, skin, central nervous system, breast, kidney, prostate, lung, thyroid, and urethra (3, 12, 13). Inflammatory bowel disease is occasionally associated with IgG4-related sclerosing disease (14, 15), but there are few reports of IgG4-related sclerosing disease primarily involving the gastrointestinal tract (3). To our knowledge, this report is the first to describe the radiologic findings of IgG4-related sclerosing disease of the small bowel.
In our case, the radiologic findings can suggest both malignant features and benign inflammatory disease features. The imaging findings that are suggestive of malignant tumors showed irregular wall thickening, loss of mural stratification, and aneurysmal dilatation of the distal ileum without small bowel obstruction. With these findings, we can suggest malignant neoplastic diseases such as lymphoma, adenocarcinoma, and metastasis. These mass-like imaging features may be related to the mass-forming characteristics of IgG4-related diseases, which can manifest inflammatory pseudotumor in many organs (16). Other imaging findings that are suggestive of benign inflammations were multifocal narrowing, traction, aggregation, and abrupt angulation of the distal ileum. These findings can suggest benign inflammatory diseases with fibrotic and stenotic features, such as Crohn's disease and tuberculosis. These fibrotic and stenotic imaging features are considered relevant to the sclerosing feature of the recently reported histopathologic findings on IgG4-related sclerosing disease of the small bowel (3). Heterogeneous mural enhancement and multiple enlarged lymph nodes were relatively non-specific findings and can be found in both malignant and benign diseases. We consider that these radiologic findings of combined malignant-looking and inflammatory fibrostenotic features might be clues to the diagnosis of IgG4-related sclerosing diseases of the small bowel.
In summary, IgG4-related sclerosing disease is a rare systemic disease that involves various organs. There are few studies, however, about the IgG4-related sclerosing disease of the gastrointestinal tract. In this report, we present the first case, to our knowledge, of radiologic findings of IgG4-related sclerosing diseases arising in the small bowel. Although a definite diagnosis relies on histopathological confirmation, the radiologic findings may provide a clue to the diagnosis of IgG4-related sclerosing diseases of the small bowel.
References
- 1.Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008;14:3948–3955. doi: 10.3748/wjg.14.3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366:539–551. doi: 10.1056/NEJMra1104650. [DOI] [PubMed] [Google Scholar]
- 3.Wong DD, Pillai SR, Kumarasinghe MP, McGettigan B, Thin LW, Segarajasingam DS, et al. IgG4-related sclerosing disease of the small bowel presenting as necrotizing mesenteric arteritis and a solitary jejunal ulcer. Am J Surg Pathol. 2012;36:929–934. doi: 10.1097/PAS.0b013e3182495c96. [DOI] [PubMed] [Google Scholar]
- 4.Yoshida K, Toki F, Takeuchi T, Watanabe S, Shiratori K, Hayashi N. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40:1561–1568. doi: 10.1007/BF02285209. [DOI] [PubMed] [Google Scholar]
- 5.Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38:982–984. doi: 10.1007/s00535-003-1175-y. [DOI] [PubMed] [Google Scholar]
- 6.Zen Y, Nakanuma Y. IgG4-related disease: a cross-sectional study of 114 cases. Am J Surg Pathol. 2010;34:1812–1819. doi: 10.1097/PAS.0b013e3181f7266b. [DOI] [PubMed] [Google Scholar]
- 7.Cheuk W, Chan JK. IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity. Adv Anat Pathol. 2010;17:303–332. doi: 10.1097/PAP.0b013e3181ee63ce. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto H, Yamaguchi H, Aishima S, Oda Y, Kohashi K, Oshiro Y, et al. Inflammatory myofibroblastic tumor versus IgG4-related sclerosing disease and inflammatory pseudotumor: a comparative clinicopathologic study. Am J Surg Pathol. 2009;33:1330–1340. doi: 10.1097/pas.0b013e3181a5a207. [DOI] [PubMed] [Google Scholar]
- 9.Saab ST, Hornick JL, Fletcher CD, Olson SJ, Coffin CM. IgG4 plasma cells in inflammatory myofibroblastic tumor: inflammatory marker or pathogenic link? Mod Pathol. 2011;24:606–612. doi: 10.1038/modpathol.2010.226. [DOI] [PubMed] [Google Scholar]
- 10.Kuroiwa T, Suda T, Takahashi T, Hirono H, Natsui M, Motoyama H, et al. Bile duct involvement in a case of autoimmune pancreatitis successfully treated with an oral steroid. Dig Dis Sci. 2002;47:1810–1816. doi: 10.1023/a:1016452813815. [DOI] [PubMed] [Google Scholar]
- 11.Kamisawa T, Okamoto A. Autoimmune pancreatitis: proposal of IgG4-related sclerosing disease. J Gastroenterol. 2006;41:613–625. doi: 10.1007/s00535-006-1862-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamano H, Arakura N, Muraki T, Ozaki Y, Kiyosawa K, Kawa S. Prevalence and distribution of extrapancreatic lesions complicating autoimmune pancreatitis. J Gastroenterol. 2006;41:1197–1205. doi: 10.1007/s00535-006-1908-9. [DOI] [PubMed] [Google Scholar]
- 13.Choi JW, Kim SY, Moon KC, Cho JY, Kim SH. Immunoglobulin G4-related sclerosing disease involving the urethra: case report. Korean J Radiol. 2012;13:803–807. doi: 10.3348/kjr.2012.13.6.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fukukura Y, Fujiyoshi F, Nakamura F, Hamada H, Nakajo M. Autoimmune pancreatitis associated with idiopathic retroperitoneal fibrosis. AJR Am J Roentgenol. 2003;181:993–995. doi: 10.2214/ajr.181.4.1810993. [DOI] [PubMed] [Google Scholar]
- 15.Zamboni G, Lüttges J, Capelli P, Frulloni L, Cavallini G, Pederzoli P, et al. Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchows Arch. 2004;445:552–563. doi: 10.1007/s00428-004-1140-z. [DOI] [PubMed] [Google Scholar]
- 16.Moh IH, Kim JB, Shin SR, Jung SW, Park SH, Kim JW, et al. A case of intraperitoneal immunoglobulin G4-related inflammatory pseudotumor. Korean J Gastroenterol. 2012;60:258–261. doi: 10.4166/kjg.2012.60.4.258. [DOI] [PubMed] [Google Scholar]