Abstract
Objective
A new double-lumen balloon catheter was being developed for the treatment of cerebral aneurysms. The purpose of this study is to report our initial experience of a double-lumen balloon catheter for the treatment of wide-necked aneurysms.
Materials and Methods
Seventeen patients (mean age, 63 years; range, 45-80 years) with wide-necked, with or without a branch-incorporated aneurysms, (10 ruptured and 9 unruptured) were treated with balloon-assisted coil embolization using a double-lumen balloon catheter (Scepter C™ or Scepter XC™) for 7 months after being introduced to our country. Locations of the aneurysms were posterior communicating artery (n = 7), anterior communicating artery or A2 (n = 7), middle cerebral artery (MCA) bifurcation (n = 3), basilar artery tip (n = 1) and anterior choroidal artery (n = 1). The initial clinical and angiographic outcomes were retrospectively evaluated.
Results
Coil embolization was successfully completed in all 19 aneurysms, resulting in complete occlusions (n = 18) or residual neck (n = 1). In one procedure, a thrombus formation was detected at the neck portion of the ruptured MCA bifurcation aneurysm near to the end of the procedure. It was completely resolved with an intra-arterial infusion of Glycoprotein IIb/IIIa inhibitor (Tirofiban, 1.0 mg) without any clinical sequela. There were no treatment-related events in the remaining 18 aneurysms. At discharge, functional neurological state improved in 11 patients (10 patients with ruptured aneurysm and 1 with unruptured aneurysm presenting with mass symptoms) and 6 patients with unruptured aneurysms had no newly developed symptoms.
Conclusion
In this preliminary case series, the newly developed double-lumen Scepter balloon appears to be a safe and convenient device for coil embolization of wide-necked aneurysms.
Keywords: Intracranial aneurysm, Coil embolization, Balloon
INTRODUCTION
Several assistance techniques have increased to keep in pace with the rapid growth of coil embolization of cerebral aneurysms. Stents and balloons are two major devices used for assisting coil embolization. Each device has several implicit strengths and weaknesses. Because stents require dual antiplatelet medication, balloons appear to be favorable for the treatment of ruptured aneurysms. Additionally, a balloon catheter is often useful when saving a branch incorporated into the aneurysm sac during coiling (1). Until recently, only a single lumen balloon occlusion catheter (HyperForm™ or HyperGlide™, Covidien/ev3, Irvine, CA, USA) has been available for coil embolization at another institution. This balloon catheter requires a balloon-specifically 0.010-inch microgidewire (X-pedion, Covidien/ev3, Irvine, CA, USA), which often makes it difficult to navigate across the aneurysm neck and occasionally creates an unstable balloon position. The Scepter balloon is a newer double lumen balloon for the remodeling technique in aneurysm coil embolization. The purpose of this study is to evaluate the initial results of this device for the treatment of wide-necked cerebral aneurysms.
MATERIALS AND METHODS
Seventeen patients with 19 wide-necked aneurysms (Dome to neck ratio < 1.5 or neck diameter ≥ 4 mm) were treated with balloon-assisted coil embolizations using a newly available double lumen balloon catheter at an outside institution. All patients were registered in the recorded neuro-interventional database prospectively. Inclusion criterion was a wide neck aneurysm (dome to neck ratio < 1.5). Patients included 11 women and 6 men with a mean age of 63 years (range, 45-80 years). Ten aneurysms were ruptured and 9 were incidentally or coincidentally found. Three aneurysms recurred after the initial coil embolization (n = 2) or clipping (n = 1), of which 2 were presented with subarachnoid hemorrhage (SAH) and the other with mass symptom. Locations of aneurysms were posterior communicating artery (n = 7), anterior communicating artery (Acom) or A2 (n = 7), middle cerebral artery (MCA) bifurcation (n = 3), basilar artery (BA) tip (n = 1) and anterior choroidal artery (n = 1). Initial clinical and angiographic outcomes were retrospectively evaluated. The institutional review board approved this retrospective study with a waiver of patient informed consents.
Scepter Balloon Catheter
The Scepter balloon catheter (Scepter C™ or Scepter XC™, Microvention, Inc., Tustin, CA, USA) is a newly developed balloon catheter with a coaxial double lumen which is compatible with any type of 0.014-inch microguidewire and the other serves for balloon inflation. This balloon catheter has 3 markers: a distal catheter tip marker and 2 proximal and distal balloon markers. The distance between the distal end of the balloon and the distal catheter tip marker is 5 mm in length. Another important characteristic of the Scepter balloon catheter is that the 5 mm-length distal tip allows for steam shaping, which makes it easier to track the microguidewire in a tortuous artery that has acute angulations and prevents blood reflux into the balloon. The currently available balloon catheters' features are summarized and compared in the Table 1.
Table 1.
Competitive Analysis of Balloon Catheters
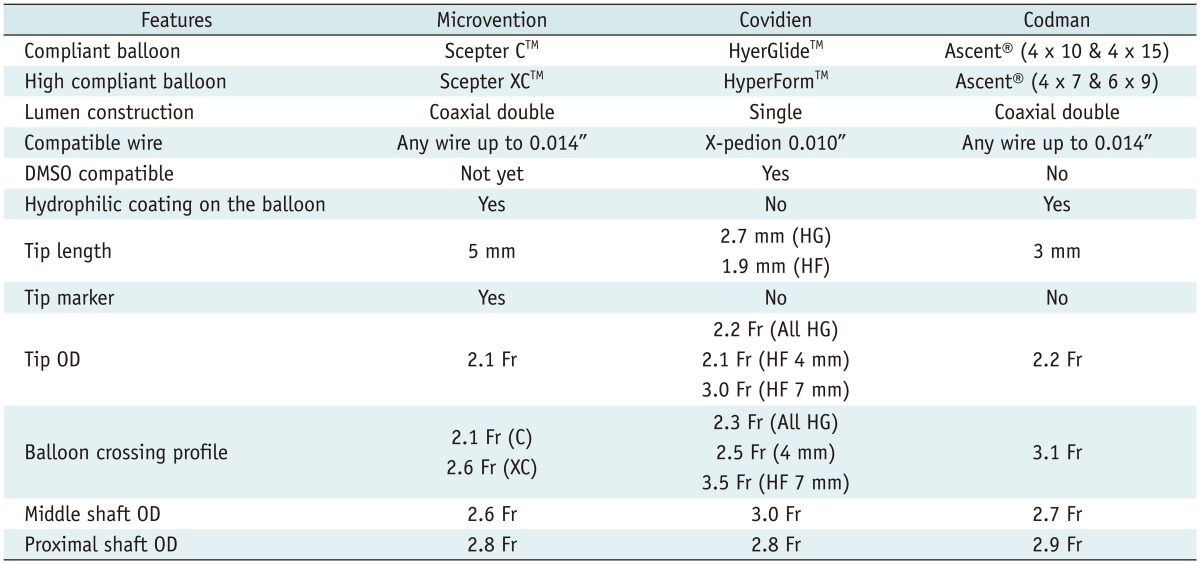
Note.- HG = HyperGlide, HF = HyperForm, C = Scepter C, XC = Scepter XC, DMSO = dimethylsulfoxide, OD = outer diameter
Procedure
All procedures, but one, were performed under general anesthesia. After placing a guiding catheter (Shuttle 6 Fr, Cook or Envoy 6 Fr, Coddman Neurovascular) in the cervical portion of the internal carotid or vertebral artery, the Scepter balloon catheter, with or without steam shaping of its distal tip, was navigated across the aneurysm neck at the distal portion using a 0.014-inch microguidewire (Traxus-14, Microvention, Inc., Tustin, CA, USA). After confirming that the balloon position spanned the entire aneurysm neck, the microguidewire was removed and the balloon catheter lumen for microguidewire insertion was continuously flushed with a pressurized heparinized solution during the procedure. In the case of removing the guidewire to unfix the balloon position, the guidewire was reinserted and maintained in position. The aneurysm sac was selected with another microcatheter (Excelsior-10, Stryker, Fremont, CA, USA) and the balloon-assisted coil embolization was performed. If needed for bifurcation aneurysms (Acom, MCA, or BA), the balloon was repositioned to the other branch that was not initially selected with the Scepter balloon catheter, using a 0.014-inch microguidewire (Fig. 1). Procedural success was defined as complete occlusion or residual neck of the aneurysm sac on final control angiogram as classified according to Raymond classification (2). The aneurysm sac volume was calculated using the following formula: aneurysm sac volume = (4 / 3) × π × (length / 2) × (width / 2) × (height / 2). The volume of the inserted coil was calculated as follows: coil volume = π × (diameter of coil / 2)2 × (length of coil). Packing density (%) was calculated by dividing the volume of inserted coils by the volume of aneurysm × 100.
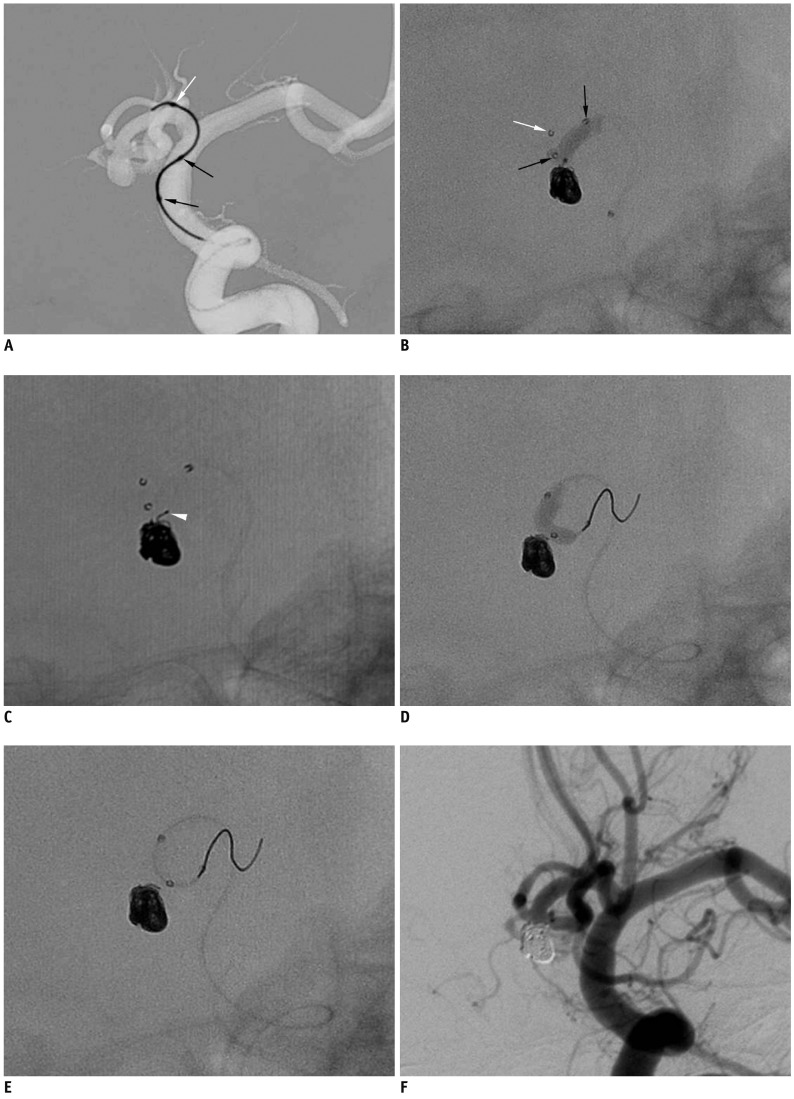
Fig. 1.
Case 1. 72-year-old man with ruptured anterior communicating artery aneurysm.
A. Advancement of Scepter balloon catheter over 0.014-inch microguidewire that was prepositioned at anterior cerebral artery A1 portion. B. Scepter balloon-assisted coil embolization performed after removal of microguidewire. C. Coil tail (white arrowhead) protruded after balloon deflation. D, E. Scepter balloon catheter is repositioned from right A2 to left A2 using microguidewire and is used to push coil tail in sac. F. Final control angiogram shows complete occlusion of aneurysm sac without any coil loop protrusion. Note that white arrow indicates distal tip marker of Scepter balloon catheter and black arrows indicate proximal and distal markers of balloon itself.
RESULTS
Characteristics of patients, aneurysms, and immediate post-treatment angiographic outcomes are summarized in Table 2. Coil embolization was successfully completed in all 19 aneurysms, resulting in complete occlusions (n = 18) or residual neck (n = 1). For one patient, a thrombus formation was detected at the neck portion of the ruptured MCA bifurcation aneurysm towards the end of the procedure. It was completely resolved with an intra-arterial infusion of Glycoprotein IIb/IIIa inhibitor (Tirofiban, 1.0 mg) without any clinical consequences (Fig. 2). There were no treatment-related events in the remaining 18 aneurysms. At discharge, functional neurological state improved in 11 patients (10 patients with a ruptured aneurysm and 1 with mass symptoms) and the remaining 6 patients with unruptured aneurysm showed no newly developed symptoms (Table 2).
Table 2.
Characteristics of Patients, Aneurysms, and Immediate Post-Treatment of Angiographic Outcomes
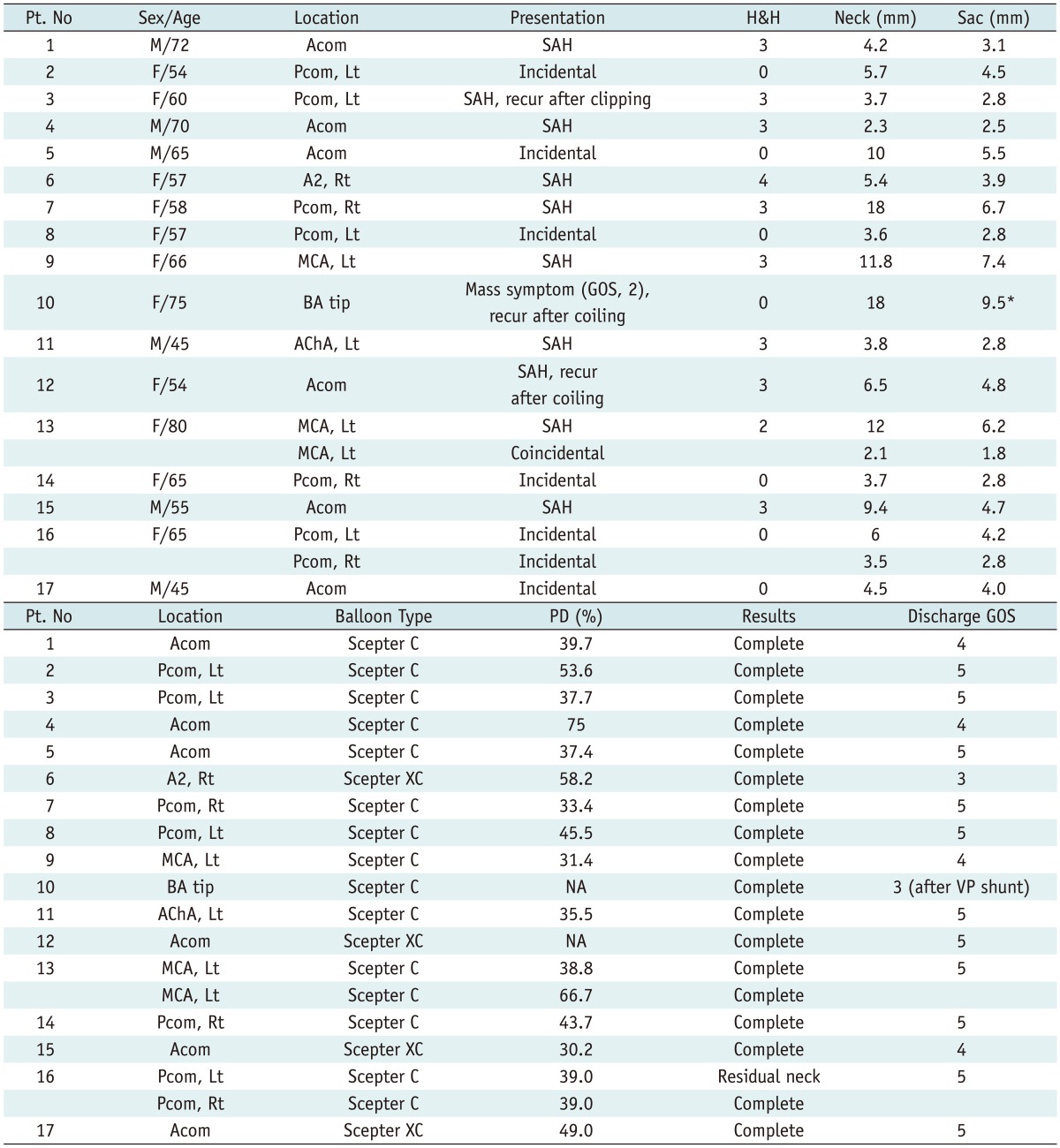
Note.- *Contrast medium filling portion, large portion of aneurysm was thrombosed. H&H = Hunt & Hess grade, Discharge GOS = glasgow outcome scale at discharge, PD = packing density, SAH = subarachnoid hemorrhage, Acom = anterior communicating artery, Pcom = posterior communicating artery, MCA = middle cerebral artery, BA = basilar artery, AChA = anterior choroidal artery, Lt = left, Rt = right, VP shunt = ventriculoperitoneal shunt
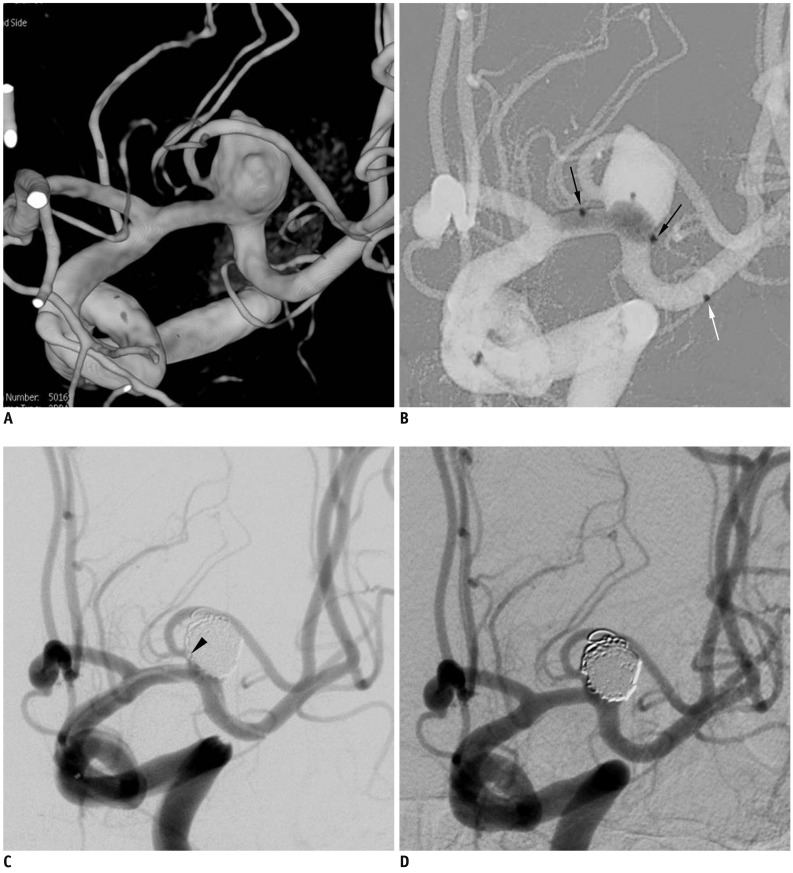
Fig. 2.
Case 2. 66-year-old woman with ruptured aneurysm at middle left cerebral artery.
A. Three-dimension reconstruction angiogram reveals large aneurysm at middle left cerebral artery bifurcation. Note that superior branch is incorporated into sac. B. After placement of balloon across aneurysm neck, gradual over-inflation causes substantial portion of balloon to herniate into aneurysm sac. C. At end of procedure, small thrombus (black arrowhead) is detected at aneurysm neck, close to origin of superior branch. D. After intraarterial infusion of Glycoprotein inhibitor, 30-minutes follow-up angiogram shows resolution of thrombus and complete occlusion of aneurysm sac. Note that white arrow indicates distal tip marker of Scepter balloon catheter and black arrows indicate proximal and distal markers of balloon itself.
Representative Cases
Case 1 (of Patient No. 1)
A 72-year-old man was being admitted with a Hunt & Hess grade 3 SAH. An angiography revealed a small, wide-necked aneurysm at the Acom. Under general anesthesia, a shuttle 6 Fr-guiding catheter was placed in the cervical ICA. First, a 0.014-inch microguidewire was positioned on the left anterior cerebral artery (ACA) A1 portion and the Scepter-C balloon 4/10 catheter was advanced over the microguidewire to the ACA A1 portion (Fig. 1A). The microguidewire was positioned further to the right A2 portion and the balloon catheter was placed, thus, spanning the entire aneurysm neck, and then, the balloon-assisted coil embolization was performed (Fig. 1B). Near the end of the coil embolization, a coil tail protruded the Acom after balloon deflation (Fig. 1C). The balloon catheter was re-positioned to the left A2 using a reintroduced microguidewire. Inflation of the balloon pushed the protruded coil tail into the aneurysm sac (Fig. 1D, E). A final control angiogram showed complete occlusions of the aneurysm sac (Fig. 1F).
Case 2 (of Patient No. 9)
A 66-year-old woman was being admitted with a Hunt & Hess grade 3 SAH. An angiography showed a large aneurysm at the left MCA bifurcation. A three-dimensional reconstruction of the angiogram revealed that a superior branch was incorporated into the sac (Fig. 2A). After placement of the Scepter-C balloon catheter from the M1 to MCA inferior division, a gradual over-inflation of the balloon indicated that a substantial portion of the balloon was herniated into the sac (Fig. 2B), which made it possible to save the incorporated superior branch and, in turn, to perform the coil embolization of the aneurysm. At the end of the procedure, an angiography revealed a thrombus formation at the aneurysm neck close to the origin of the superior branch (Fig. 2C). After administering an intra-arterial Glycoprotein IIb/IIIa inhibitor (Tirofiban, 1 mg) infusion, a follow-up angiography 30 minutes later showed a resolution of the thrombus and a complete occlusion of the aneurysm sac (Fig. 2D). The patient showed no neurological deficit post-treatment.
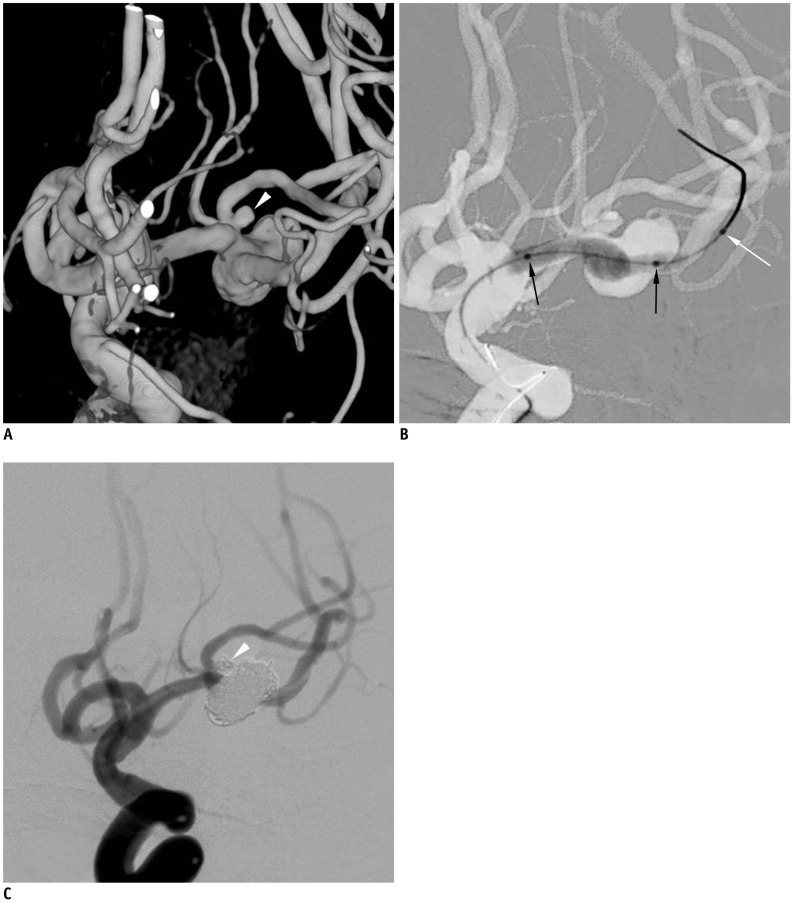
Case 3 (of Patient No. 13)
An 80-year-old woman was being admitted with a Hunt & Hess grade 2 SAH. A three-dimensional reconstruction of the angiogram showed a large aneurysm on the left MCA bifurcation and another very small aneurysm close to the bifurcation aneurysm neck at the superior branch (Fig. 3A). After placement of the Scepter C balloon catheter from M1 to the inferior M2 division (Fig. 3B), a balloon-assisted coil embolization of the large aneurysm was successfully completed. After repositioning the balloon catheter, a very small aneurysm at the superior division was also embolized. The final control angiogram revealed a complete occlusion of both aneurysms and well-preserved MCA superior and inferior divisions (Fig. 3C).
Fig. 3.
Case 3. 80-year-old woman with ruptured middle left cerebral artery aneurysms.
A. Three-dimensional reconstruction angiogram reveals large aneurysm at middle left cerebral artery bifurcation and another very small aneurysm (white arrowhead) close to aneurysm neck at superior branch. B. After positioning Scepter balloon catheter across aneurysm neck, gradual over-inflation leads to herniation of central portion of balloon into large aneurysm sac. C. After balloon-assisted coil embolization of both aneurysms, final control angiogram shows complete occlusion of both aneurysms and well-preserved superior and inferior divisions. Black arrows indicate proximal and distal balloon markers of Scepter balloon catheter. White arrow indicated distal tip marker of Scepter balloon catheter (black arrows, proximal and distal balloon markers; white arrow, tip marker of balloon catheter).
DISCUSSION
Although self-expandable neurovascular stents have been increasingly used for the treatment of wide-necked and/or complex aneurysms with various deployment techniques (3-5); compliant or hypercompliant balloons still remained as very useful tools, especially for endovascular treatment of acutely ruptured aneurysms. Stents have an inherent limitation in that they may induce in-stent thrombosis and may potentially increase thromboembolic complications. To prevent such thrombosis, stents require dual antiplatelet medications, which in turn may cause a hemorrhagic complication in 20% of patients, especially in those with a ruptured aneurysm (6). Such drawbacks lead to increased procedure-related morbidity and mortality rates in stent-assisted coiling relative to simple coiling (7, 8). On the other hand, according to a few reports, procedure-related complications are significantly higher when using a balloon-assisted technique as compared to the conventional single-catheter technique (9). However, in a meta-analysis and recent prospective trials, the balloon-assisted technique did not significantly increase peri-procedural morbidity and mortality rates (10, 11). Until recently, at our institution, only the single-lumen balloon catheter has been available for coil embolization, which requires a balloon-specific 0.010-inch microguidewire. In contrast, the new double-lumen Scepter balloon catheter allows for any type of 0.014-inch microguidewire, which makes it easy to navigate across the aneurysm neck at any location to a distal portion of a tortuous parent artery without requiring an exchange technique. Furthermore, because of the 0.014-inch microguidewire compatibility, it is easier to reposition the balloon catheter from one distal branch to the other in a bifurcation type aneurysm. In representative case 1, a coil tail protruded towards the A2, which was not covered by prepositioned Scepter balloon, after the balloon deflated towards the end of embolization. It has been an occasionally experienced limitation inherented to balloon-assisted coiling. In order to push the protruded coil, the repositioning of the balloon to the other branch in which the balloon was not initially positioned is necessary. Owing to its superior controllability, a 0.014-inch microguidewire seemed to make it easier to reposition the balloon than a 0.010-inch microguidewire as in the representative case 1. First case report on the Scepter C balloon catheter usage documented that all types of 0.014-inch guidewire compatibility was very helpful (12). A recent case series mentioned that the Scepter C balloon catheter was only navigated in one of the 52 aneurysms at various locations, and only one adverse event (1.9%) was documented with attributions to balloon use (aneurysm perforation); thus, suggesting the safety and convenience of Scepter balloon catheter (13). An additional advantage is that the Scepter balloon catheter has a 5 mm-length soft distal catheter tip that permits steam shaping. Steam shaping of the distal tip makes it much easier for the balloon catheter to track a tortuous artery with acute angulation and precludes blood reflux into the balloon. As shown in Figure 1, although a short portion of the 0.014-inch microguidewire was placed in the A1 portion with an acute angulation from the ICA, the balloon catheter was easily tracked to the A1 portion over the prepositioned microguidewire. The excellent compliance of the Scepter balloon revealed the tendency of a balloon herniation into the aneurysm sac, which saved the incorporated branch in the aneurysm sac (Fig. 2) and made the coil embolization of a wide-necked aneurysm at arterial bifurcation possible. Finally, with a double-lumen Scepter balloon catheter, the continuous flushing of the occluded distal branch with heparinized solution during the balloon inflation may theoretically decrease clot formations and possible distal embolization during the coiling. Two types of Scepter balloon catheters are currently available, Scepter C and Scepter-XC. Scepter C balloon catheter is a compliant balloon similar to HyperGlide balloon catheter and Scepter-XC is a super-compliant balloon catheter similar to HyperForm balloon catheter. Therefore, their uses are similar to HyperGlide or HyperForm, respectively. Generally, Scepter XC is useful to treat bifurcation aneurysms such as basilar tip or MCA bifurcation aneurysm with regards to its super-compliance, while the Scepter-C is for side-wall aneurysms such as ICA paraclinoid aneurysms. Scepter XC may be more useful in partial herniation of balloon into the aneurysm sac to save a branch incorporated into the sac or neck such as the HyperForm balloon catheter (1).
This study does not include follow-up angiographic results. However, the purpose of this study is to report an initial experience in the safety and convenience of the double-lumen Scepter balloon catheter for assisting coil embolization, and not to evaluate the durability of balloon-assisted coil embolization. Long-term durability of balloon-assisted coil embolization should be elucidated in larger case series.
In conclusion, a new double-lumen Scepter balloon catheter appears to be a convenient and safe tool for assisting coil embolization. This balloon catheter may be useful for the treatment of wide-necked aneurysms, especially for ruptured aneurysms.
Footnotes
This study was supported by a new faculty research seed money grant of Yonsei University College of Medicine for 2013 (8-2013-0026).
References
- 1.Kim BM, Park SI, Kim DJ, Kim DI, Suh SH, Kwon TH, et al. Endovascular coil embolization of aneurysms with a branch incorporated into the sac. AJNR Am J Neuroradiol. 2010;31:145–151. doi: 10.3174/ajnr.A1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–1403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]
- 3.Jeon P, Kim BM, Kim DI, Park SI, Kim KH, Kim DJ, et al. Reconstructive endovascular treatment of fusiform or ultrawide-neck circumferential aneurysms with multiple overlapping enterprise stents and coiling. AJNR Am J Neuroradiol. 2012;33:965–971. doi: 10.3174/ajnr.A2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim BM, Kim DJ, Kim DI. Stent application for the treatment of cerebral aneurysms. Neurointervention. 2011;6:53–70. doi: 10.5469/neuroint.2011.6.2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roh HG, Chun YI, Choi JW, Cho J, Moon WJ, Solander S. Retrograde stent placement for coil embolization of a wide-necked posterior inferior cerebellar artery aneurysm. Korean J Radiol. 2012;13:510–514. doi: 10.3348/kjr.2012.13.4.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim DJ, Suh SH, Kim BM, Kim DI, Huh SK, Lee JW. Hemorrhagic complications related to the stent-remodeled coil embolization of intracranial aneurysms. Neurosurgery. 2010;67:73–78. doi: 10.1227/01.NEU.0000370937.70207.95. discussion 78-79. [DOI] [PubMed] [Google Scholar]
- 7.Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010;41:110–115. doi: 10.1161/STROKEAHA.109.558114. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro M, Becske T, Sahlein D, Babb J, Nelson PK. Stent-supported aneurysm coiling: a literature survey of treatment and follow-up. AJNR Am J Neuroradiol. 2012;33:159–163. doi: 10.3174/ajnr.A2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sluzewski M, van Rooij WJ, Beute GN, Nijssen PC. Balloon-assisted coil embolization of intracranial aneurysms: incidence, complications, and angiography results. J Neurosurg. 2006;105:396–399. doi: 10.3171/jns.2006.105.3.396. [DOI] [PubMed] [Google Scholar]
- 10.Pierot L, Cognard C, Anxionnat R, Ricolfi F CLARITY Investigators. Remodeling technique for endovascular treatment of ruptured intracranial aneurysms had a higher rate of adequate postoperative occlusion than did conventional coil embolization with comparable safety. Radiology. 2011;258:546–553. doi: 10.1148/radiol.10100894. [DOI] [PubMed] [Google Scholar]
- 11.Pierot L, Cognard C, Spelle L, Moret J. Safety and efficacy of balloon remodeling technique during endovascular treatment of intracranial aneurysms: critical review of the literature. AJNR Am J Neuroradiol. 2012;33:12–15. doi: 10.3174/ajnr.A2403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gory B, Kessler I, Seizem Nakiri G, Riva R, Al-Khawaldeh M, Mounayer C. Initial experience of intracranial aneurysm embolization using the balloon remodeling technique with Scepter C, a new double-lumen balloon. Interv Neuroradiol. 2012;18:284–287. doi: 10.1177/159101991201800306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spiotta AM, Miranpuri A, Hawk H, Chaudry MI, Turk AS, Turner RD. Balloon remodeling for aneurysm coil embolization with the coaxial lumen Scepter C balloon catheter: initial experience at a high volume center. J Neurointerv Surg. 2012 doi: 10.1136/neurintsurg-2012-010552. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]