Abstract
Background
Measures for pain management after total knee arthroplasty (TKA) are important for early improvement in the quality of life after operation and early postoperative rehabilitation. We investigated the benefits and safety analgesic effect of locally injected drugs around the total knee prosthesis.
Methods
60 patients undergoing TKA for osteoarthritis were divided randomly into three groups.Group A (20 knees; control group), this group did not receive multimodal drug cocktailtherapy; group B (21 knees), received intra-articular injection of a multimodal drug cocktail; and group C (19 knees), received localperiarticular injection of a multimodal drug cocktail. All analgesics administered in the first 24 h after surgery were recorded. The evaluation items included assessment of pain using a 100-point visual analogue scale (VAS) after the patients awoke on the day of the operation and on postoperative day 1, the dose of diclofenac sodium suppository, the number of days for acquiring assisted ambulation with a walking cane, and side effects. Assessment of flexion angles was conducted at postoperativeweek 1 and at theconclusion of the study.
Results
The VAS scores on the day of surgery and the amounts of diclofenac sodium used indicated good pain relief in groups B and C; the level of pain control was higher in group C than in group B. No cardiac or central nervous system toxicity was observed.
Conclusions
Periarticular injection with multimodal drugs can significantly reduce the requirements for analgesia, with no apparent risks, following TKA.
Keywords: Pain control, Total knee arthroplasty, Periarticular injection
Total knee arthroplasty (TKA) is performed for pain relief, normal joint motion, and a deformity correction of the knee. Postoperative analgesia can be achieved by a variety of techniques such as intravenous analgesia, epidural analgesia, and peripheral nerve block techniques. Local injection of a multimodal drug cocktail consisting of an analgesic drug and an opioid is both safe and easy to administer for pain management following TKA. In this study, we prospectively compared the efficacy and side effects of treatments for pain control between a group in which no multimodal drug cocktail therapy was used following TKA and 2 groups in which different drugs and methods of administration were employed.
1. Materials and methods
The study participants included 60 patients (11 men and 49 women) who had undergone unilateral TKA between June 2010 and February 2012 for previously diagnosed osteoarthritis of the knee (Table 1). All they had written informed consent. Exclusion criteria were major psychological problems, previous drug dependency, allergies to any of the ingredients of the injection, renal insufficiency, abnormal liver enzymes, a history of stroke or a major neurological deficit, or uncontrolled angina and bifascicular blocks with prolonged QT intervals. The mean age of the participants was 75.6 years. Two different knee devices were used in this study: Zimmer NexGen LPS Flex was used in 51 patients and Zimmer NexGen CR-Flex in 9. The patients were divided randomly into 3 groups: group A (20 knees; control group), this group did not receive multimodal drug cocktail therapy; group B (21 knees), received intra-articular injection of a mixture (30 ml) containing 0.5% bupivacaine (20 ml), 10 mg of morphine hydrochloride (1 ml), 0.3 mg of epinephrine (0.3 ml), and sterile normal saline (8.7 ml); and group C (19 knees), received local periarticular injection of 50 ml of a mixture containing 0.75% ropivacaine (30 ml), 10 mg of morphine hydrochloride (1 ml), 4 mg of betamethasone (1 ml), 0.25 mg of epinephrine (0.25 ml), and saline (17.75 ml) before and after implant placement. Operative anesthesia was all genera, and anesthesia regimen was standardized. TKA was performed through a mini medial para-patellar approach. Pain assessment was conducted using 5 examination parameters. A visual analog scale (VAS) was used to assess pain 4 h after the patients returned to their recovery rooms and 24 h after surgery. Assessment of flexion angles was conducted at postoperative week 1 and at the conclusion of the study. The amounts of diclofenac sodium suppository used during 24 h after the surgery were quantitated. The number of days required to achieve assisted ambulation with a walking cane was recorded. The nature and frequency of side effects were also recorded. Chi-square test and analysis of variance were used for statistical testing, and the level of significance was set at P < 0.05.
Table 1.
Subjects.
| Group A | Group B | Group C | ||
|---|---|---|---|---|
| Number of knees | 20 | 21 | 19 | |
| Age (years) | 75.0 | 75.0 | 77.0 | NS |
| Male-to-female ratio | 3/17 | 5/16 | 3/16 | NS |
| OA grade (Kellgren Lawrence Classification) | 17 grade IV knees 3 grade III knees |
16 grade IV knees 5 grade III knees |
16 grade IV knees 3 grade III knees |
NS |
| Preoperative extension angles | −7.0 | −6.9 | −4.7 | NS |
| Preoperative flexion angles | 115.5 | 118.1 | 118.4 | NS |
| (LPS/CR) | 17/3 | 18/3 | 16/3 | NS |
NS; not significant.
2. Results
The mean VAS scores on the day of surgery were 65.0 for group A, 51.7 for group B, and 29.2 for group C, with significant differences observed between the scores of groups A and C and groups B and C. The mean VAS scores 24 h after surgery were 45.0 for group A, 55.3 for group B, and 41.3 for group C, with no significant intergroup differences (Fig. 1). The amounts of diclofenac sodium suppository used during the 24 h period after the surgery were 61.3 mg for group A, 25.0 mg for group B, and 13.2 mg for group C, with significant differences noted between groups A and B and groups A and C (Fig. 2). The mean flexion angles at postoperative week 1 were 117.0° for group A, 114.8° for group B, and 113.7° for group C. Flexion angles at the conclusion of the study were 124.5° for group A, 126.0° for group B, and 122.1° for group C, with no significant intergroup differences. The mean number of days required to achieve assisted ambulation with a walking cane was 6.3 for group A, 7.0 for group B, and 6.4 for group C, with no significant intergroup differences.
Fig. 1.

Mean VAS scores.
*P < 0.05, NS; not significant.
Fig. 2.
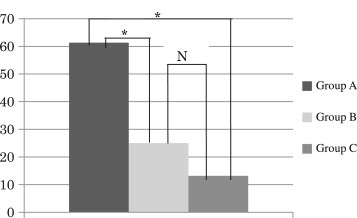
Amount of diclofenac sodium suppository used (mg).
*P < 0.05, NS; not significant.
The primary side effects reported were postoperative nausea and vomiting (PONV). The incidence rates of PONV were 10.0% for group A, 38.1% for group B, and 10.5% for group C, with the incidence observed in group B being significantly higher than those in the other 2 groups. No other side effects were reported.
3. Discussion
According to reports by TKA specialists, local anesthetic drugs, opioids, and epinephrine are the primary agents used to control postoperative pain, along with steroids and non-steroidal anti-inflammatory drugs. The typical method of administration is periarticular injection.1–4 In our previous report, we suggested the possibility of achieving different degrees of pain control depending on the drugs used in the multimodal drug cocktail therapy and the method of dosing.5 On the basis of these results, in this study, we compared drug mixtures and administration methods for groups B and C against the control group A. The VAS scores on the day of surgery and the amount of diclofenac sodium suppository administered indicated good pain control in the groups that were administered cocktail therapy (B and C), but the level of pain control was greater in group C than in group B. Because several components of the drug therapy differed between groups B and C, the most effective agent or combination of agents remains unknown; nevertheless, we considered that the agents produced synergistic effects. Regarding PONV due to morphine, measures against PONV were initially not taken in group B, and thus PONV frequently occurred in group B. Therefore, intramuscular administration of 5 mg prochlorperazine was initiated after the patients of group B returned to the recovery room. The drug was effective to varying extents in some patients, which was not a sufficient measure. Therefore, we referred to the consensus guidelines for managing PONV published in the USA6 and started intramuscular administration of 5 mg prochlorperazine during the operation followed by intravenous injection of droperidol 1.25 mg intraoperatively, which significantly improved PONV.
4. Conclusions
The VAS scores on the day of surgery and the amounts of diclofenac sodium used indicated good pain control in groups B and C; the level of pain control was higher in group C than in group B. Regarding the measures taken to prevent PONV, intramuscular administration of prochlorperazine 5 mg and intravenous injection of droperidol 1.25 mg were initiated intraoperatively, which significantly improved PONV.
Conflicts of interest
All authors have none to declare.
References
- 1.Parvataneni H.K., Shah V.P., Howard H., Cole N., Ranawat A., Ranawat C.S. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty. 2007;22:33–38. [Google Scholar]
- 2.Busch C.A., Shore B.J., Bhandari R. Efficacy of periarticular multimodal drug injection in total knee arthroplasty: a randomized trial. J Bone Joint Surg. 2006;88-A:959–963. doi: 10.2106/JBJS.E.00344. [DOI] [PubMed] [Google Scholar]
- 3.Essving P., Axelsson K., Aberg E., Spannar H., Gupta A., Lundin A. Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. Anesth Analg. 2011;113:926–933. doi: 10.1213/ANE.0b013e3182288deb. [DOI] [PubMed] [Google Scholar]
- 4.Mullaji A., Kanna R., Shetty G.M., Chavda V., Singh D.P. Efficacy of periarticular injection of bupivacaine, fentanyl, and methylprednisolone in total knee arthroplasty: a prospective, randomized trial. J Arthroplasty. 2010;25:851–857. doi: 10.1016/j.arth.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Nakamura T., Tamaki M., Ueda Y., Nakai T. Pain management by periarticular cocktail injection after total knee arthroplasty. Cent Jpn J Orthopaedic Surg Traumatol. 2011;54:665–666. [Google Scholar]
- 6.Gan T.J., Meyer T., Apfel C.C. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62–71. doi: 10.1213/01.ane.0000068580.00245.95. [DOI] [PubMed] [Google Scholar]


