Abstract
The purpose of this study was to compare the effects of lumbar stabilization exercises using balls to the effects of general lumbar stabilization exercises with respect to changes in the cross section of the multifidus (MF), weight bearing, pain, and functional disorders in patients with non-specific chronic low back pain. Twelve patients participated in either a 8 week (3 days per week) stabilization exercise program using balls and control group (n = 12). The computer tomography (CT) was used to analyze MF cross-sectional areas (CSA) and Tetrax balancing scale was used to analyze left and right weight bearing differences. Both groups had significant changes in the CSA of the MF by segment after training (p < 0.05) and the experimental group showed greater increases at the L4 (F = 9.854, p = 0.005) and L5 (F = 39. 266, p = 0.000). Both groups showed significant decreases in weight bearing, from 9.25% to 5.83% in the experimental group and from 9.33% to 4.25% in the control group (p < 0.05), but did not differ significantly between the two groups. These results suggests that stabilization exercises using ball can increases in the CSA of the MF segments, improvement in weight bearing, pain relief, and recovery from functional disorders, and the increases in the CSA of the MF of the L4 and L5 segments for patients with low back pain.
Key Points.
Compared with the stabilization exercise using a ball and general stabilization exercise increased the CSA of the MF, weight bearing, pain, and functional ability in patients with low back pain.
We verified that increases in the CSA of the MF of the L4 and L5 segments and functional ability during the stabilization exercise using a ball.
The stabilization exercise using a ball was shown to be an effective exercise method for patients with low back pain in a rehabilitation program by increasing functional ability and the CSA of the MF.
Key words: Stabilization exercise, ball, multifidus, cross-sectional area, low back pain
Introduction
Low back pain is the most representative musculoskeletal system disorder (Chung et al., 2013; Kwon et al., 2011). Although this disorder can be remedied without any particular treatment, chronic low back pain that persists for three months or longer occurs in approximately 5~10% of the patients and becomes a major cause that restricts productive lifestyle activities (Borenstein, 1996; Watson et al., 2000). Low back pain patients use movement strategies that differ from those of healthy persons (Grabiner et al., 1992) because the onset time of their multifidus (MF) and transverse abdominus (TrA), which are deep muscles, are delayed and their ability to mobilize these muscles is reduced (Hodges and Richardson, 1999). In addition, chronic low back patients frequently show poor balance control (Harding et al., 1994) because they sway backward to maintain their center of force (COF) when they balance themselves (Byl and Sinnott, 1991). Therefore, low back pain patients are instructed to perform exercises that vary in method and intensity in order to improve or maintain their muscle strength and improve balance (Cairns et al., 2006; Goldby et al., 2006; Kofotolis and Kellis, 2006). Recently, stabilization exercises that focus on core strengthening, mobility control, and muscle control have become a very important treatment method for low back pain (MacDonald et al., 2006; Richardson et al., 2002). These exercises can improve the functions of the nervous and the muscular systems and thereby control and protect the spine. In practice, these exercises enhance control over the lumbar spine and the pelvis (Hodges, 2003), and can be performed in diverse body positions using the co-contraction of the abdominal and MF muscles (Andrusaitis et al., 2011). The purpose of stabilization exercises is to improve the activation patterns of trunk muscles, in order to relieve lumbar pain and incapacity through trunk muscle contraction (Goldby et al., 2006; Kavcic et al., 2004).
Unstable training devices, such as balls, can be used to increase the difficulty of exercises employing diverse body weight and free-weight resistance (Anderson and Behm, 2005). Exercises that use balls use all regions of the body so that more extensive activities can occur than with exercises performed on fixed floors. The use of balls therefore can improve the dynamic balance ability, the flexibility and stability of the spine, and the sense of balance as ways to prevent damage (Marshall and Murphy, 2005). Marshall and Murphy, 2006 reported that a 12 week regimen of spinal stabilization exercises using balls by low back pain patients brought about pain relief and decreases in flexion-relaxation disorders as well as improvements in the ability to control balance through the strengthening of the MF muscle, which plays an important role in spinal stability. However, other previous studies reported that spinal motions did not change and revealed no increase in trunk muscle activity during core stability exercises on unstable surfaces (Drake et al., 2006; Freeman et al., 2006; Wahl and Behm, 2008).
Although ball exercises are used for diverse purposes such as balance control and muscle strengthening, the beneficial effects of spinal stabilization exercises using balls on lumbar vertebral segments remain to be verified. The purpose of the present study is the effects of lumbar stabilization exercises using balls with respect to changes in the cross-section area (CSA) of the MF, weight bearing, pain, and functional disorders in patients with non-specific chronic low back pain. The working hypothesis is that stabilization exercise programs will increase trunk muscle activity and improve spinal stability, thereby leading to pain relief, functional disorder reduction, balance improvement, and increases in the CSA of individual segments of the MF; i.e., greater improvement will be seen using stabilization exercise programs using balls than with general stabilization exercise programs.
Methods
Subjects
The calculation of sample size was carried out with α = 0.05 (5% chance of type I error), 1- β = 0.80 (power 80%), and using the results of a previous study comparing between the Swiss ball and a stable surfaces because this most closely resembles devices used in this study (Marshall and Murphy, 2006), and a calculated effect size of δ = 1.21. This provided sample size of n = 20. This study was large enough to consider drop out. The present study was conducted with 28 patients of B Hospital who had no particular anatomical or neurophysiological causes of disease (X-ray and examination by a medical doctor) but had complained of low back pain for at least 12 weeks. Subjects who had low back pain for the last six months, musculoskeletal system disorders, abnormal past histories in the spine (spondylitis, fracture), neurologic diseases, or functional restrictions on the upper or lower limbs were excluded. Data were obtained from 12 patients (6 males, 6 females; excluding two dropouts) in the experimental group and 12 patients (5 males, 7 females; excluding two dropouts) in the control group. The experimental group was divided into two treatment groups by randomly taking out pieces of paper with the treatment groups written in them folded and put into an opaque envelope: group A (Ball) or B (Mat). The CONSORT (consolidated standards of reporting trials) flowchart of the study is shown in Figure 1.
Figure 1.
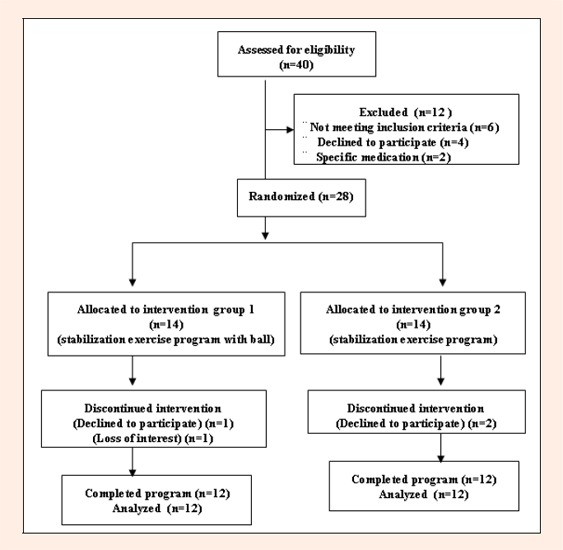
CONSORT flowchart of this study
The experimental group had a mean age of 35.20 ± 10.01 years, height of 1.70 ± 0.01 m, weight of 64.40 ± 7.34 kg, and duration of illness of 12.76 ± 5.28 months while the control group values were 41.32 ± 7.13 years, 1.66 ± 0.05 m, 62.54 ± 2.93 kg, and duration of illness of 13.26 ± 7.13 months respectively. The experimental group performed stabilization exercises using balls and the control group performed general stabilization exercises. All procedures were performed in accordance with the principles outlined in the Declaration of Helsinki, and participants signed the appropriate informed consent form.
Training program
Warm-up and cool-down exercises consisted of walking for 10 minutes each on a treadmill. The main exercises were performed three times per week for eight weeks using four different motions. Three times in the first week, two physical therapists with five years or longer kinesiatrics careers educated the patients one by one by explaining the purpose of the exercise therapy and demonstrating the motions. Three times in the second and subsequent weeks, auditory feedback was provided by verbal instructions and tactile feedback was provided by the therapist's hand to guide the subjects in accurate exercise methods. Each exercise motion and the number of times each was performed were recorded and the subjects were asked if they felt pain.
The stabilization exercise group that used balls performed as the following exercises: 1) In a supine position, the subject placed a ball below the neck, bent the knees, and crossed and bent 90° the arms so that the crossed arms came to the eye level. While breathing out, the subject slowly raised each lower limb in turn. The subject performed the motion of bending the hip joint and the knee joint 90° five times, for 10 seconds each time; 2) In a supine position, the subject placed a ball below the pelvis, bent the knees, and crossed and bent 90° the arms so that the crossed arms came to the eye level. The subject performed the motion of pressing the ball below the pelvis slowly with the pelvis five times, for 10 seconds each time; 3) In a crawling position, the subject placed a ball below one knee and kept the toes away from contact with the floor. The subject balanced first to stabilize the posture and slowly raised the other lower limb. This exercise was performed in turn for the two lower limbs 10 times, for 10 seconds each time; and 4) After assuming a prone position, the subject placed a ball in front of the pelvis and raised both lower limbs. As if kicking, the subjects repeatedly raised and lowered the two lower limbs alternately. The subject performed this exercise 10 times, for five sets, taking a rest of at least 15 seconds between each set, as shown in Figure 2.
Figure 2.
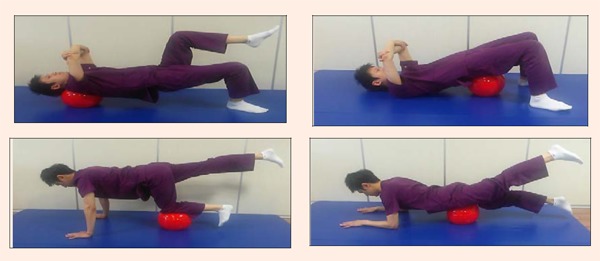
The stabilization exercise using a ball
The general stabilization exercise group performed the same motions on a mat.
Procedures and instrumentation: Visual analog scale (VAS)
In the present study, visual analog scales (VAS) were measured to assess pain. Each subject was instructed to mark the intensity of his/her pain on a 100 mm stick without any gradation (Gould et al., 2001). Subjects marked the intensity as 0 points when they experienced no pain, and severe unendurable pain was given 10 points. The scores were presented as follows: 0-30 = mild pain, 31-69 = moderate pain, 70-100 = severe pain (Kelly, 2001). The inter-rater reliability of this tool is 0.55-0.97, and the reliability within each rater is 0.69-0.91 (Taddio et al., 2009).
Oswestry disability index (ODI)
For the functional assessment of low back pain, the Korean version of the Oswestry disability index (ODI) version 2.0 developed by Fairbank et al. (2000) and translated by Jeon et al., 2006 was used to measure low back pain. This tool was developed based on the 10-item questionnaire of ODI to assess low back pain-related limitations in daily life and requires the subject to select one of six points under each of the 10 items: the intensity of pain, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and travelling (0-5 points).
Functional disability scores were calculated as percentages by adding up the measured scores of individual items, dividing the total score by the full score of the items, and multiplying the resultant value by 100. The scores were presented as follows: 0-20 = mild disability, 20-40 = moderate disability, 40-60 = severe disability, 60-80 = crippled, 80-100 = bed bound. This questionnaire is intended to examine disabilities resulting from pain rather than the pain itself. This questionnaire provides supplementary information for the results of the VAS. Cronbach's alpha coefficient of 0.92, test-retest correlation reliability was 0.93 (Jeon et al., 2006).
Weight bearing
Weight bearing was measured with a Tetrax Portable Multiple System (Tetrax, Sunlight Medical Ltd, Israel), which enables implementation of biofeedback training treatment while measuring balance. The degrees of postural sway for four placements of the feet can be measured to indicate general stability indexes and an individual's control abilities and compensating postural changes can be monitored (Lee et al., 2012). Large changes in body weight percentages at different foot sites and high stability indexes indicate high instability (Kohen-Raz et al., 1994: Kohen-Raz, 1991). This instrument consisted of separate force plates: two 12cm wide x 19cm long rectangular toe side foot force plates (left: B, right: D) and two 12cm wide x 12cm long square heel side foot force plates (left: A, right: C) and indicated weight indexes that showed the proportion of weight distributed among the four force plates. Information about the pressure imposed on the force plates is amplified, filtered, and then delivered to the computer for analysis with the Tetrax software program. The individual force plates measure changes in vertical pressure from the two toe side feet and heel side feet separately.
The subjects stood on the force plates, with arms hanging down straight and their feet at shoulder width, while viewing a mark 3m in front of them. The weight values on the two sides that were fixed after the subject stood on the measuring instrument were selected as values for the right and left sides, respectively. This procedure was repeated three times for 30 seconds and the average values were used as measurements (Kohen-Raz et al., 1994) (Figure 3).
Figure 3.
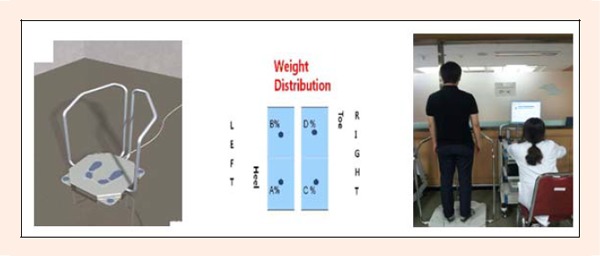
The balance measurement
| |(A % + B %) ? (C % + D %)| = % |
Computed tomography (CT) of the multifidus muscle: Measuring method
The area of the lumbar MF was measured using CT scan (conditions: 120 kV, 160 mA, 0.6 s rotation time, 5 mm slice thickness, 5 mm reconstruction interval) using a Somatom Plus-4C (Siemens General Medical, Germany). The subject assumed a neutral position to avoid compression of the back muscle that occurs in a supine position. A pillow was placed below the abdomen to minimize lumbar lordosis and the subject was instructed to maintain a relaxed posture while being scanned. To confirm the patient's relaxed state, the tester palpated the patient's back muscle (Danneels et al., 2001). The iliac crest on both sides and the spinous process on L5 were identified and their positions were marked on the skin. A longitudinal scan was then performed toward the spine above the spinous process.
Image analysis
The CT images were analyzed after enlargement on the computer screen. On the sagittal plane of each MF, the sizes of the MF at four levels from L2 to L5 were drawn clearly on the computer screen along the boundaries of the muscles using the mouse cursor and the PACS (Picture Archiving and Communication System) program (Piview STAR, Infinitt Inc., Korea). The CSA were then measured and presented in Figure 4. The fat regions on the innermost fascial borders of the MF and the erector spinae and on the MF fascial boundary were included. The fat regions between the MF and the lamina were included in the CSA of the MF.
Figure 4.
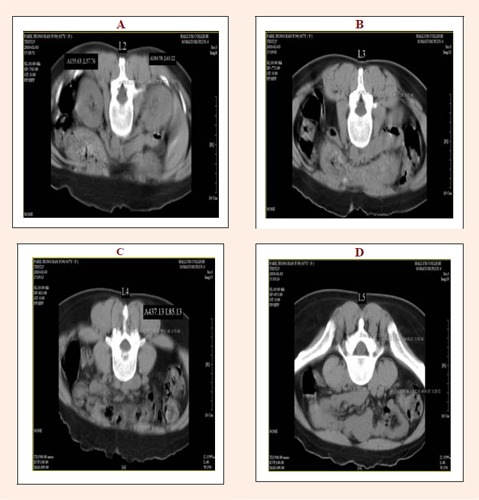
Cross-sectional images of the multifidus muscle. (A) L2 region. (B) L3 region. (C) L4 region. (D) L5 region
In the present study, these four levels were analyzed to identify the most suitable level and to detect any systematic differences between different levels. Because the L5s of many subjects were sharply angled, the lower end plate of L4 was selected instead of the upper end plate of L5 (Danneels et al., 2001; Keller et al., 1999). To reduce selective errors, the data were randomly measured by the same specialist in radiology.
Statistical analysis
Statistical analyses were conducted using SPSS Windows (version 18.0). Data are presented as Mean ± Standard deviations. The normality of the independent variables was tested by Kolmogrov-Smirnov test, indicating that all variables were confirmed normal distributions by the test. Demographic characteristics and dependent variables were analyzed using Levene's test of independent t-tests to verify homogeneity. Data showed that the normality and no violation of homogeneity of variance and thus that parametrical tests. Paired t-tests were conducted to compare differences in the CSA of the MF, weight bearing, pain, and functional disorders in the experimental group and the control group before and after the stabilization exercises. To compared over the training period in the experimental and control groups using two factor (group x time) repeated analysis of variance (ANOVA). The statistical significance level was set at 0.05.
Results
Changes in the CSA of the MF by segment pre and post the experiment are showed significant increases at L2, L3, L4 and L5 of experimental and control groups, respectively (p < 0.05). Between the two groups, in CSA of the MF at L2 (F = 2.236, p = 0.150) and L3 (F = 1.122, p =0.301) no statistically significant and greater increase in the experimental group was statistically significant at L4 (F = 9.854, p = 0.005) and L5 (F = 39.266, p = 0.000) (Table 1). Both groups showed significant decreases in weight bearing (p < 0.05). Comparison between the two groups indicated no statistically significant (F = 2.512, p = 0.128). Decreases in pain were significant in both groups (p < 0.05). Comparison between the two groups indicated no statistically significant (F = 0.316, p = 0.580). Decreases in functional disorders were also significant in both groups (p < 0.05). Comparison between the two groups indicated that the greater decrease in the experimental group was statistically significant (F = 5.256, p = 0.032) (Table 2).
Table 1.
Comparison of CSA within groups and between groups. Values are means (±SD)
| Experimental (n=12) | Control (n=12) | ||
| L2 (mm2) | pre | 351.62 (45.75) | 355.37 (57.19) |
| post | 365.56 (44.39) * | 362.04 (55.61) * | |
| change (95% CI) | 13.94 (14.86) (4.50-23.38) | 6.67 (7.10) (2.16-11.17) | |
| L3 (mm2) | pre | 578.67 (67.58) | 586.03 (88.59) |
| post | 610.25 (59.52) * | 601.60 (86.26) * | |
| change (95% CI) | 31.58 (48.49) (0.77-62.39) | 15.57 (14.44) (6.39-24.74) | |
| L4 (mm2) | pre | 913.92 (61.52) | 919.75 (81.32) |
| post | 1085.57 (73.59) * | 995.84 (117.59) * | |
| change (95% CI) | 171.66 (46.95) † (141.82-201.49) | 76.09 (91.42) (18.00-134.17) | |
| L5 (mm2) | pre | 1175.38 (164.74) | 1187.14 (220.48) |
| post | 1454.82 (125.49) * | 1290.48 (230.95) * | |
| change (95% CI) | 279.43 (69.83) † (235.06-323.80) | 103.34 (70.17) (58.76-147.93) |
CSA: Cross sectional area, CI: Confidence intervals.
* p < 0.05 indicate differences between pre- and post-training exercise groups.
† p < 0.05 indicate differences between experimental and control groups
Table 2.
Comparison of VAS, ODI and WB within groups and between groups. Values are means (±SD)
| Experimental (n=12) | Control (n=12) | ||
| WB (%) | pre | 9.25 (1.66) | 9.33 (2.57) |
| post | 5.83 (2.44) | 4.25 (2.45) | |
| change (95% CI) | -3.42 (2.97) (-1.53 − -5.30) | -5.08 (3.00) (-3.18 − -6.99) | |
| VAS (scores) | pre | 4.58 (.90) | 4.92 (.90) |
| post | 2.75 (.75) * | 3.08 (.79) * | |
| change (95% CI) | -1.83 (.58) (-1.47 − -2.20) | -1.83 (.72) (-1.38 − -2.29) | |
| ODI (scores) | pre | 26.33 (2.81) | 25.25 (3.44) |
| post | 6.42 (2.23) * | 11.00 (6.24) | |
| change (95% CI) | -19.92 (2.91) † (-18.07 − -21.76) | -14.25 (7.49) (-9.49 − -19.01) |
VAS: Visual analog scale, ODI: Oswestry disability index, WB: Weight bearing, CI: Confidence intervals.
* p < 0.05 indicate differences between pre- and post-training exercise groups.
† p < 0.05 indicate differences between experimental and control groups.
Discussion
The most important result of the present study is that significant increases in the CSA of the MF of L4 and L5 and improvement in the functional disorder indexes were observed following stabilization exercises using balls for eight weeks, when compared to general stabilization exercises.
Hides et al., 2001 indicated that the TrA and the MF (which is an erector muscle of the spine) play important roles in the stability of the trunk. The weakening of the lumbar extensor muscles is also dominant over the weakening of the lumbar flexor muscles in chronic low back pain patients, so that strengthening of the extensor muscles is important (Mayer et al., 1985; 1989). Exercises on unstable surfaces provide stability to the spine due to the co-activation of global and local muscles at the beginning of motor control (Carter et al., 2006). Instability training using Swiss balls mainly activates local stabilizing muscles (Cooke, 1980), while the use of resistance to body mass in unstable states without using external resistance increases the integration and recruitment of global and local muscles. The overall effect is an increase in muscle activation and improvement in motor control, which ultimately leads to increased muscle strength (Cug et al., 2012).
Danneels et al., 2001 reported a comparison of the CSA of the MF after subjects had performed stabilization exercises and dynamic-static strengthening exercises and showed that the L3 upper end plate increased in CSA 6.45 %, the L4 upper end plate increased in CSA 6.29 %, and the L4 lower end plate increased in CSA 7.21 %. Hides et al., 2011 reported changes in the thicknesses of the MF after subjects were allowed to take rests on tilting beds for 60 and then made to perform trunk flexor and strength exercises for 14 days thereafter, and showed that L3 increased in CSA 10.50 %, L4 increased in CSA 10.16 %, and L5 increased in its CSA 7.88 %. They explained that L3 showed the largest change because of the position of the vertebral level to which exercise loads were imposed during performance of exercises involving raising the trunk and the lower limbs. On the other hand, Imai et al., 2010 reported that exercises using Swiss balls increased the activity of all trunk muscles compared to exercises on the floor, whereas exercises on unstable surfaces using BOSU Balance Trainers, which have fixed floors, did not change the activity of trunk muscles when compared to exercises on the floor. The authors measured muscle activity in nine healthy subjects in their 20s after the subjects had maintained each motion for three seconds and found no differences in the activity of the MF. Their explanation was that global muscles were more involved in trunk control than were local muscles. However, in the present study, the motions applied to the exercise program using Swiss balls implemented by chronic low back patients with deep muscle atrophy were performed while the trunk was controlled using the upper extremity. The resultant low intensity shaking stimulated deep muscles and led to the re-education and increased activity of the MF, resulting in increased CSA. The large changes at L4 and L5 are considered attributable to the motion load imposed on the lower lumbar spine due to the repetitive movements and resistance exercises applied to the lower extremity.
Beneck and Kulig, 2012 indicated that decreases in the volume of the MF would deteriorate lumbar stability and cause painful structures or new injuries, thereby inducing pain and functional disorders. Hides et al., 1996 said that damage to the MF causing low back pain would not be naturally cured and the resultant lack of stability in local regions was a factor that would increase the recurrence rate of low back pain. The instability of spinal segments in lumbar skeletal structures without any deficit is a major cause of chronic low back pain (Long et al., 1996). This instability induces pain, reduces endurance and flexibility, and restricts the range of motion of the lumbar joints (Gill et al., 1988). Therefore, the prevention of the recurrence of pain due to damage to the musculoskeletal system and the improvement in the functions of decreased activities should be the goals of treatment (Jette, 1995). França et al., 2012 showed that lumbar stabilization exercises applied for six weeks resulted in a decrease in pain by 0.06 points (from 5.94 points) and a decrease in the functional disorder index by 1.80 points (from 17.07 points) and they advised that stabilization exercises were a good therapy. Sung, 2003 reported that four weeks of spinal stabilization exercise training resulted in improvement of functional disability conditions, while Sekendiz et al., 2010 showed that 12 weeks of core strength training exercises using Swiss balls could improve abdominal endurance, lower back muscular endurance, and dynamic balance in female office workers. Marshall and Desai (2010) indicated that recreationally active participants who performed advanced Swiss ball exercises could obtain good levels of physical fitness and strength. The present study also showed that the ball exercise group had a more significant functional improvement (a decrease in pain from 4.58 to 2.75 points compared to 4.92 to 3.08 points for the control group) and decrease in ODI (from 26.33 to 6.42 points compared to 25.25 to 11.0 points in the control group). These low back pain relieving effects are considered to have resulted by obtaining appropriate harmony among deep muscles through lumbar stabilization exercises and decreases in stress imposed on the spine induced by the improvement of the stability of spinal segments.
Nies and Sinnott, 1991 indicated that low back pain patients showed severe back and forth swaying on unstable surfaces and had poor balance when standing on one foot. Stimuli necessary for balance control are delivered to the cerebrum and the cerebellum through central nerves that are linked to sight, vestibular senses, somesthesia, proprioceptive senses, and musculocutaneous and joint receptors. The central nerves integrate these stimuli to control the joints and muscles and maintain balance (Di Fabio and Badke, 1990; Lacour et al., 2008). In low back pain patients, inappropriate proprioceptive senses are delivered to the central nervous system, which may reduce the ability to control postures (Gill and Callaghan, 1998). Mechanical receptors in soft tissues around the lumbar spine or synovial joints are affected by lumbar damage. After the initial damage, changes occur in the quantities or natures of proprioceptive inputs from the muscle spindles, Golgi tendon organs, and joint/skin receptors. Therefore, somesthesia deteriorates due to inappropriate inputs on trunk positions in relation to the ground or gravity (Bennell and Goldie, 1994). Hamaoui et al., 2004 advised that low back pain patients showed increased anterio-posterior (A-P) postural sway, while Mientjes and Frank, 1999 reported that chronic low back pain patients showed increased medio-lateral (M-L) direction balance sway. Rhee et al., 2012 reported that performance of stabilization exercises for four weeks decreased A-P sway but M-L sway was unaffected. In a study comparing low back pain patients and healthy persons, Alexander and LaPier, 1998 reported no significant differences in the states of static balance and the degrees of weight bearing by the two lower limbs when the subjects tilted their bodies forward, backward, and laterally, with the eyes closed or open. In the present study, statistically significant differences in weight bearing were observed between the left and right sides (a decrease from 9.25% to 5.83% in the experimental group and from 9.33% to 4.25% in the control group). Therefore, both exercises are considered effective lumbar stabilization therapies for developing the sense of balance since they improved muscle strength, endurance, and flexibility. However, these authors agree with previous studies (Nies and Sinnott, 1991) indicating that balance impairments in low back pain patients are limited secondary problems that arise due to use of balance strategies that involve hyper-lordotic postures taken to reduce pain in standing positions.
Limitations of the present study include the small number of samples, the relatively short intervention period of eight weeks, and the fact that stability in dynamic conditions was not measured. The present study was also conducted with only some patients who met the study criteria; therefore, the results cannot be generalized to all chronic low back pain patients. In addition, the changes in the sizes of muscles and the quality of muscles in relation to age and muscle strength should be also studied. Since only the CSA of the MF was measured in the present study, measuring and comparing the CSA of other surrounding muscles may generate different results. The effects of the exercises performed by more subjects for longer times should be examined in future studies and the correlation between changes in the size of the MF of low back patients and changes in their functions should be examined through multilateral studies.
Conclusion
This study compared the CSA of the MF segments, weight bearing, pain, and functional disorders in patients with chronic low back pain who performed stabilization exercises using balls vs. general stabilization exercises. The stabilization exercises resulted in increases in the CSA of the MF segments, improvement in weight bearing, pain relief, and recovery from functional disorders, and the increases in the CSA of the MF of the L4 and L5 segments were greater in the experimental group that performed exercises using balls. Future studies should incorporate more subjects and longer intervention periods to compare the effects of exercises on the MF and surrounding muscles that contribute to spinal stabilization and to study the relationship between pain and functional disorders.
Biographies

SinHo Chung
Employment
Department of Rehabilitation Medicine, Hanyang University Hospital, Seoul, Republic of Korea
Degree
PhD
Research interests
Rehabilitation in sport context and Biomechanics of sports movements.
E-mail: wwin72@empal.com

JuSang Lee
Employment
Department of Physical therapy, Hallym College, Gangwon-do, Republic of Korea
Degree
PhD
Research interests
Biomechanics of sports movements and Anatomy.
E-mail: ljspt1004@empal.com

JangSoon Yoon
Employment
Department of Rehabilitation Medicine, Hallym University Chuncheon Sacred Heart Hospital, Gangwon-do, Republic of Korea
Degree
PhD
Research interests
Biomechanics of human locomotor system and Rehabilitation in sport context.
E-mail: ptyjs@hanmail.net
References
- Alexander K.M., LaPier T.L. (1998) Differences in static balance and weight distribution between normal subjects and subjects with chronic unilateral low back pain. Physical Therapy Journal of Orthopedic & Sports Physical Therapy 28(6), 378-383 [DOI] [PubMed] [Google Scholar]
- Anderson K., Behm D.G. (2005) Trunk muscle activity increases with unstable squat movements. Canadian Journal of Applied Physiology 30(1), 33-45 [DOI] [PubMed] [Google Scholar]
- Andrusaitis S.F., Brech G.C., Vitale G.F., Greve J.M.D. (2011) Trunk stabilization among women with chronic lower back pain: a randomized, controlled, and blinded pilot study. Clinics 66(9), 1645-1650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beneck G.J., Kulig K. (2012) Multifidus atrophy is localized and bilateral in active persons with chronic unilateral low back pain. Archives of Physical Medicine & Rehabilitation 93(2), 300-306 [DOI] [PubMed] [Google Scholar]
- Bennell K.L., Goldie P.A. (1994) The differential effects of external ankle support on postural control. Physical Therapy Journal of Orthopedic & Sports Physical Therapy 20(6), 287-295 [DOI] [PubMed] [Google Scholar]
- Borenstein D.G. (1996) Chronic low back pain. Rheumatic Diseases Clinics of North America 22(3), 439-456 [DOI] [PubMed] [Google Scholar]
- Byl N.N., Sinnott P. (1991) Variations in balance and body sway in middle-aged adults: subjects with healthy backs compared with subjects with low-back dysfunction. Spine 16(3), 325-330 [DOI] [PubMed] [Google Scholar]
- Cairns M.C., Foster N.E., Wright C. (2006) Randomized controlled trial of specific spinal stabilization exercises and conventional physiotherapy for recurrent low back pain. Spine 31(19), E670-E681 [DOI] [PubMed] [Google Scholar]
- Carter J.M., Beam W.C., McMahan S.G., Barr M.L., Brown L.E. (2006) The effects of stability ball training on spinal stability in sedentary individuals. The Journal of Strength & Conditioning Research 20(2), 429-435 [DOI] [PubMed] [Google Scholar]
- Chung S.H., Her J.G., Ko T., Ko J., Kim H., Lee J.S., Woo J.H. (2013) Work-related musculoskeletal disorders among Korean physical therapists. Journal of Physical Therapy Science 25(1), 55-59 [Google Scholar]
- Cooke J.D. (1980) The role of stretch reflexes during active movements. Brain Research 181(2), 429-435 [DOI] [PubMed] [Google Scholar]
- Cug M., Ak E., Ozdemir R.A., Korkusuz F., Behm D.G. (2012) The effect of instability training on knee joint proprioception and core strength. Journal of Sports Science & Medicine 11(3), 468-474 [PMC free article] [PubMed] [Google Scholar]
- Danneels L.A., Vanderstraeten G.G., Cambier D.C., Witvrouw E.E., Bourgois J., Dankaerts W., De Cuyper H.J. (2001) Effects of three different training modalities on the cross sectional area of the lumbar multifidus muscle in patients with chronic low back pain. British Journal of Sports Medicine 35(3), 186-191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Fabio R.P., Badke M.B. (1990) Relationship of sensory organization to balance function in patients with hemiplegia. Physical Therapy 70(9), 542-548 [DOI] [PubMed] [Google Scholar]
- Drake J.D.M., Fischer S.L., Brown S.H.M., Callaghan J.P. (2006) Do exercise balls provide a training advantage for trunk extensor exercises? A biomechanical evaluation. Jounal of Manipulative & Physiological Therapeutics 29(5), 354-362 [DOI] [PubMed] [Google Scholar]
- Fairbank J.C.T., Pynsent P.B. (2000) The Oswestry Disability Index. Spine 25(22), 2940-2953 [DOI] [PubMed] [Google Scholar]
- França F.R., Burke T.N., Caffaro R.R., Ramos L.A., Marques A.P. (2012) Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. Journal of Manipulative & Physiological Therapeutics 35(4), 279-285 [DOI] [PubMed] [Google Scholar]
- Freeman S., Karpowicz A., Gray J., McGill S. (2006) Quantifying muscle patterns and spine load during various forms of the push-up. Medicine & Science in Sports & Exercise 38(3), 570-577 [DOI] [PubMed] [Google Scholar]
- Gill K.P., Callaghan M.J. (1998) The measurement of lumbar proprioception in individuals with and without low back pain. Spine 23(3), 371-377 [DOI] [PubMed] [Google Scholar]
- Gill K.P., Krag M.H., Johnson G.B., Haugh L.D., Pope M.H. (1988) Repeatability of four clinical methods for assessment of lumbar spinal motion. Spine 13(1), 50-53 [DOI] [PubMed] [Google Scholar]
- Goldby L.J., Moore A.P., Doust J., Trew M.E. (2006) A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine 31(10), 1083-1093 [DOI] [PubMed] [Google Scholar]
- Gould D., Kelly D., Goldstone L., Gammon J. (2001) Examining the validity of pressure ulcer risk assessment scales: developing and using illustrated patient simulations to collect the data. Journal of Clinical Nursing 10(5), 697-706 [DOI] [PubMed] [Google Scholar]
- Grabiner M.D., Koh T.J., el Ghazawi A. (1992) Decoupling of bilateral paraspinal excitation in subjects with low back pain. Spine 17(10), 1219-1223 [DOI] [PubMed] [Google Scholar]
- Hamaoui A., Do M.C., Bouisset S. (2004) Postural sway increase in low back pain subjects is not related to reduced spine range of motion. Neuroscience Letters 357(2), 135-138 [DOI] [PubMed] [Google Scholar]
- Harding V.R., Williamsa A.C., Richardsonb P.H., Nicholasa M.K., Jacksona J.L., Richardsona I.H., Pithera C.E. (1994) The development of a battery of measures for assessing physical functioning of chronic pain patients. Pain 58(3), 367-375 [DOI] [PubMed] [Google Scholar]
- Hides J.A., Jull G.A., Richardson C.A. (2001) Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine 26(11), E243-248 [DOI] [PubMed] [Google Scholar]
- Hides J.A., Lambrecht G., Richardson C.A., Stanton W.R., Armbrecht G., Pruett C., Damann V., Felsenberg D., Belavý D.L. (2011) The effects of rehabilitation on the muscles of the trunk following prolonged bed rest. European Spine Journal 20(5), 808-818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hides J.A., Richardson C.A., Jull G.A. (1996) Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine 21(23), 2763-2769 [DOI] [PubMed] [Google Scholar]
- Hodges P.W. (2003) Core stability exercise in chronic low back pain. The Orthopedic Clinics of North America 34(2), 245-254 [DOI] [PubMed] [Google Scholar]
- Hodges P.W., Richardson C.A. (1999) Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Archives of Physical Medicine & Rehabilitation 80(9), 1005-1012 [DOI] [PubMed] [Google Scholar]
- Imai A., Kaneoka K., Okubo Y., Shiina I., Tatsumura M., Izumi S., Shiraki H. (2010) Trunk muscle activity during lumbar stabilization exercises on both a stable and unstable surface. Physical Therapy Journal of Orthopedic & Sports Physical Therapy 40(6), 369-375 [DOI] [PubMed] [Google Scholar]
- Jeon C.H, Kim D.J., Kim S.K., Kim D.J., Lee H.M., Park H.J. (2006) Validation in the cross-cultural adaptation of the korean version of the oswestry disability index. Journal of Korean Medical Science 21(6), 1092-1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jette A.M. (1995) Outcomes research: shifting the dominant research paradigm in physical therapy. Physical Therapy 75(11), 965-970 [DOI] [PubMed] [Google Scholar]
- Kavcic N., Grenier S., McGill S.M. (2004) Quantifying tissue loads and spine stability while performing commonly prescribed low back stabilization exercises. Spine 29(20), 2319-2329 [DOI] [PubMed] [Google Scholar]
- Keller A., Johansen J., Hellesnes J., Brox J.I. (1999) Pridictors of isokinetic back muscle strength in patients with low back pain. Spine 24(3), 275-280 [DOI] [PubMed] [Google Scholar]
- Kelly A. M. (2001). The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emergence Medicine Journal 18 (3), 205-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kofotolis N., Kellis E. (2006) Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional performance in women with chronic low back pain. Physical Therapy 86(7), 1001-1012 [PubMed] [Google Scholar]
- Kohen-Raz R. (1991) Application of tetra-ataxiametric posturography in clinical and developmental diagnosis. Perceptual & Motor Skills 73 (2), 635-656 [DOI] [PubMed] [Google Scholar]
- Kohen-Raz R., Kohen-Raz A., Erel J., Davidson B., Caine Y., Froom P. (1994) Postural control in pilots and candidates for flight training. Aviat, Space & Environmental Medicine 65(4), 323-326 [PubMed] [Google Scholar]
- Kwon B.K., Roffey D.M., Bishop P. B., Dagenais S., Wai E.K. (2011) Systematic review: occupational physical activity and low back pain. Occupational Medicine-Oxford 61(8), 541-548 [DOI] [PubMed] [Google Scholar]
- Lacour M., Bernard-Demanze L., Dumitrescu M. (2008) Posture control, aging, and attention resources: models and posture-analysis methods. Neurophysiologie Clinique/Clinical Neurophysiology 38(6), 411-421 [DOI] [PubMed] [Google Scholar]
- Lee J.W., Yoon S.W., Kim J.H., Kim Y.P., Kim Y.N. (2012) The effect of ankle range of motion on balance performance of elderly people. Journal of Physical Therapy Science 24(10), 991-994 [Google Scholar]
- Long D.M., BenDebba M., Torgerson W.S., Boyd R.J., Dawson E.G., Hardy R.W., Robertson J.T., Sypert G.W., Watts C. (1996) Persistent back pain and sciatica in the United States: patient characteristics. Journal of Spinal Disorders 9(1), 40-58 [PubMed] [Google Scholar]
- MacDonald D.A., Moseley G.L., Hodges P.W. (2006) The lumbar multifidus: Does the evidence support clinical beliefs? Manual Therapy 11(4), 254-263 [DOI] [PubMed] [Google Scholar]
- Maeshall P.W., Desai I. (2010) Electromyographic analysis of upper body, lower body, and abdominal muscles during advanced swiss ball exercises. The Journal of Strength & Conditioning Research 24(6), 1537-1545 [DOI] [PubMed] [Google Scholar]
- Marshall P.W., Murphy B.A. (2006) Changes in muscle activity and perceived exertion during exercises performed on a swiss ball. Applied Physiology, Nutrition & Metabolism 31(4), 376-383 [DOI] [PubMed] [Google Scholar]
- Marshall P.W., Murphy B.A. (2006) Evaluation of functional and neuromuscular changes after exercise rehabilitation for low back pain using a Swiss ball: a pilot study. Journal of Manipulative & Physiological Therapeutics 29(7), 550-560 [DOI] [PubMed] [Google Scholar]
- Marshall P.W., Murphy B.A. (2005) Core stability exercises on and off a Swiss ball. Archives of Physical Medicine & Rehabilitation 86(2), 242-249 [DOI] [PubMed] [Google Scholar]
- Mayer T.G., Smith S.S., Keeley J., Mooney V. (1985) Quantification of lumbar function. Part 2: Sagittal plane trunk strength in chronic low-back pain patients. Spine 10(8), 765-772 [PubMed] [Google Scholar]
- Mayer T.G., Vanharanta H., Gatchel R.J., Mooney V., Barnes D., Judge L., Smith S., Terry A. (1989) Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine 14(1), 33-36 [DOI] [PubMed] [Google Scholar]
- Mientjes M.I., Frank J.S. (1999) Balance in chronic low back pain patients compared to healthy people under various conditions in upright standing. Clinical Biomechanics 14(10), 710-716 [DOI] [PubMed] [Google Scholar]
- Nies N., Sinnott P.L. (1991) Variations in balance and body swayin middle-aged adults: subjects with healthy backs compared with subjects with low-back dysfunction. Spine 16(3), 325-330 [DOI] [PubMed] [Google Scholar]
- Rhee H.S., Kim Y.H., Sung P.S. (2012) A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain. Medical Science Monitor 18(3), 174-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson C.A., Snijders C.J., Hides J.A., Damen L., Pas M.S., Storm J. (2002) The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine 27(4), 399-405 [DOI] [PubMed] [Google Scholar]
- Sekendiz B., Cug M., Korkusuz F. (2010) Effects of swiss-ball core strength training on strength, endurance, flexibility, and balance in sedentary women. The Journal of Strength & Conditioning Research 24(11), 3032-3040 [DOI] [PubMed] [Google Scholar]
- Sung P.S. (2003) Multifidi muscles median frequency before and after spinal stabilization exercises. Archives of Physical Medicine & Rehabilitation 84(9), 1313-1318 [DOI] [PubMed] [Google Scholar]
- Taddio A., O'Brien L., Ipp M., Stephens D., Goldbach M., Koren G. (2009) Reliability and validity of observer ratings of pain using the visual analog scale (VAS) in infants undergoing immunization injections.. Pain 147(1-3), 141-146 [DOI] [PubMed] [Google Scholar]
- Wahl M.J., Behm D.G. (2008) Not all instability training devices enhance muscle activation in highly resistance-trained individuals. The Journal of Strength & Conditioning Research 22 (4), 1360-1370 [DOI] [PubMed] [Google Scholar]
- Watson D.J., Harper S.E., Zhao P.L., Quan H., Bolognese J.A., Simon T.J. (2000) Gastrointestinal tolerability of the selective cyclooxygenase-2 (COX-2) inhibitor rofecoxib compared with nonselective COX-1 and COX-2 inhibitors in osteoarthritis. Archives of Internal Medicine 160(19), 2998-3003 [DOI] [PubMed] [Google Scholar]


