Abstract
Objective
The current study examined racial/ethnic differences in patterns of weight loss and regain in response to an initial behavioral weight loss intervention followed by an extended-care maintenance program.
Methods
We analyzed data from 224 women (African-American n = 43, Caucasian n = 181) from rural communities who participated in an initial 6-month lifestyle intervention for obesity and were then randomized to a face-to-face, telephone, or educational/control extended-care condition.
Results
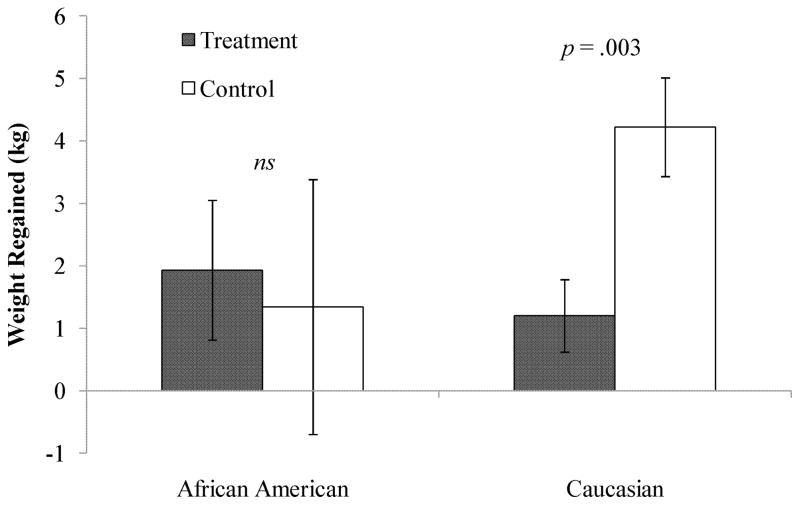
African-American participants lost less weight during the initial phase of treatment than Caucasian participants (mean ± SE = −6.8 ± .80 vs. −10.7 ± .38 kg, respectively, p = .003). Investigating weight change during month 6 to month 18, we found a significant interaction between race/ethnicity and the provision of an extended-care program. Caucasian participants randomized to either of two extended-care programs regained less weight than those assigned to the control condition (1.2 ± .58 and 4.2 ± .79 kg, respectively, p = .003), but the provision of extended care did not influence weight regain among African-American participants (1.9 ± 1.12 and 1.34 ± 2.04 kg, respectively, p = .815).
Conclusion
Collectively, these findings suggest that although African-American participants lost less weight during the initial phase of treatment, they exhibited better long-term weight-loss maintenance than Caucasian participants. Further, while the provision of extended care successfully enhanced weight maintenance among Caucasian participants, African-American participants maintained their initial weight losses regardless of extended care.
Keywords: Weight Loss, Weight Regain, Race, Racial Difference, Lifestyle Intervention
Introduction
Lifestyle interventions for obesity produce both clinically significant weight reductions and improvements in key health indicators (1). Given that U.S. rates of obesity and associated health problems are higher among African-American than Caucasian populations (2), there is a need to investigate the impact of behavioral treatment on short- and long-term weight loss outcomes in these groups. The current literature has yielded mixed outcomes regarding potential differences in initial response to lifestyle intervention. Some studies have yielded similar weight losses in both African-American and Caucasian participants (3), while others have indicated more modest effects among African-American participants as compared to Caucasian participants (4,5).
Preventing weight regain following a period of initial loss has become an important priority in the context of obesity treatment. Extended-care programs following initial lifestyle intervention can be effective in minimizing weight regain (6), but the results of studies examining differential treatment response by race have been inconsistent (5, 7, 8). For example, a study conducted by Smith West and colleagues (5) found that during a 6-month weight loss intervention that included a year-long extended-care program, African-American participants achieved smaller weight losses than Caucasian participants at both short- and long-term follow-up. Results from at least one independent clinical trials suggest, however, that patterns of long-term weight regain following an intensive lifestyle intervention may vary by race. Stevens and colleagues (8) and the Diabetes Prevention Program Research Group (7) found no significant differences between Caucasian and African-American participants in net weight losses at long-term follow-up. In the study by Stevens and colleagues (8), however, patterns of weight change varied by race. African-American participants lost less weight during the initial weight management intervention, but were better able to maintain their losses compared to Caucasian participants; contrastingly, Caucasian participants lost more weight initially, but exhibited a more rapid weight regain. For example, in the study by Stevens and colleagues (8), Caucasian participants experienced a 1.8 kg greater weight loss during initial treatment, but there were no differences by race/ethnicity at follow-up. In the Diabetes Prevention Program (7), Caucasian participants were initially more successful with reaching the weight loss goal (57% achieved a 7% weight loss, while only 30% of African-American participants reached this goal), but there were no differences by race/ethnicity at follow-up.
A recent randomized trial, Treatment of Obesity in Underserved Rural Settings (TOURS), provided an excellent opportunity for further investigation into this question. The TOURS trial was a behavioral weight management intervention that included a 6-month lifestyle intervention phase followed by a 12-month extended-care phase (9). Utilizing data from the TOURS study, the primary aim of the current study was to evaluate racial/ethnic differences in weight change during the initial and extended-care phases of the intervention. Specifically, we were interested in investigating racial/ethnic differences in weight maintenance between the extended-care and control conditions. Secondary aims focused on evaluating racial/ethnic differences in changes in cardiovascular disease risk factors (i.e., blood pressure and cholesterol), dietary intake, physical activity, and functional mobility.
Methods
Design of Parent Study
TOURS was a randomized controlled trial aimed at evaluating the effectiveness of a weight loss intervention among obese women in medically underserved rural areas (9). Eligible participants completed an initial six-month lifestyle intervention for weight management that involved weekly group-based sessions (Phase I), and were then randomized to one of three 12-month extended-care conditions with bi-weekly contact (Phase II). Phase II of the intervention included three extended-care programs that included 26 bi-weekly sessions of either face-to-face counseling, telephone counseling, or an educational control condition with mail-only contact. Participants in the TOURS study were 234 obese women who were aged 50 to 75, with a body mass index (BMI) greater than 30 kg/m2, and who resided in rural counties in north-central Florida. For further details on participant recruitment, screening, attrition, and study design, see the previous paper by Perri and colleagues (9). The current study used data from 224 of these participants who self-identified as “African-American” or “Caucasian” (African-American, N = 43; Caucasian, N = 181).
Measures
Measures were collected at 0, 6, and 18 months. Physiological measures included body weight, manual blood pressure, triglycerides, LDL cholesterol, Hemoglobin A1c, and C-reactive protein. Fasting blood samples were analyzed by Quest Diagnostics (Gainesville, FL). Estimates of macro- and micro-nutrient intake and intake of specific food groups were assessed using the validated Block Food Frequency Questionnaire (10, 11). The 6-Minute Walk Test (6MWT) was used to assess changes in functional mobility (12, 13), and physical activity was measured using the Community Healthy Activities Model Program for Seniors (CHAMPS) Physical Activity Questionnaire (14). Completion of self-monitoring logs of food intake and physical activity (daily steps) was used as a proxy for participant adherence to the intervention. At 18 months, participants completed a 36-item questionnaire that assessed overall satisfaction with the lifestyle intervention (9).
Analysis plan
To address the study’s primary aims, repeated-measures ANOVAs were conducted to examine the interaction between racial/ethnic differences in weight change during Phase I and Phase II. Because the results of the TOURS study demonstrated equivalent weight maintenance benefits for the two extended-care conditions compared to the control condition (9), assignment to these groups was recoded into a dichotomous variable: face-to-face or telephone counseling versus the mail-only educational control. For the secondary aims, repeated measures ANOVAs were conducted to assess changes over Phase I of the intervention. Bonferroni-adjusted estimated marginal means were used to decompose significant interactions. Intent-to-treat analyses were used to account for participant attrition, and multiple imputation was used to control for missing data.
Results
Preliminary analyses
Preliminary analyses demonstrated that African-American participants were significantly younger than Caucasian participants, mean ± SD = 58.0 ± 5.7 vs. 60.1 ± 6.1 years, respectively, p = .046; thus, age was used as a covariate in all analyses entailing racial/ethnic comparisons. Groups were otherwise similar with regard to baseline characteristics (all ps > .05). Demographics of participants by race/ethnicity are available in Table 1, and baseline physiological characteristics of participants by race/ethnicity are available in Table 2.
Table 1.
Demographic characteristics by race/ethnicity
| Variable | African American | Caucasian |
|---|---|---|
| Education level | ||
| High school degree or less | 27.9% | 38.7% |
| Trade, vocational, or associates degree | 39.5% | 42.5% |
| Bachelor’s degree | 14.0% | 10.5% |
| Postbaccalaureate degree | 18.6% | 8.3% |
| Employment status | ||
| Employed | 48.8% | 45.3% |
| Unemployed | 51.2% | 54.7% |
| Income | ||
| <$10,000 – 19,999 | 18.6% | 21.0% |
| $20,000 – 34,999 | 30.2% | 23.8% |
| $35,000 – 49,999 | 20.9% | 21.0% |
| $50,000 – 99,999 | 30.2% | 30.4% |
| >$100,000 | 0% | 3.9% |
| Marital status | ||
| Married/Marriage-like relationship | 62.8% | 81.8% |
| Separated/Divorced | 20.9% | 8.8% |
| Widowed | 14.0% | 8.3% |
| Single | 2.3% | 1.1% |
Table 2.
Baseline characteristics by race/ethnicity
| Variable | African American Mean ± SD (n = 43) |
Caucasian M ± SD (n = 181) |
|---|---|---|
| Body weight, kg | 99.9 ± 16.8 | 95.8 ± 14.5 |
| BMI, kg/m2 | 38.1 ± 6.2 | 36.5 ± 4.5 |
| Age, years | 58.0 ± 5.7 | 60.1 ± 6.1a |
| Cholesterol, mg/dL | ||
| LDL | 114.9 ± 31.5 | 123.5 ± 29.1 |
| HDL | 63.0 ± 16.2 | 54.6 ± 11.8 |
| Blood pressure, mm Hg | ||
| Systolic | 127.1 ± 8.8 | 125.7 ± 9.2 |
| Diastolic | 77.6 ± 7.9 | 74.5 ± 7.5 |
| Tryglycerides, mg/dL | 110.3 ± 9.5 | 152.7 ± 4.5a |
| Hemoglobin A1c, % | 6.5 ± 0.1 | 5.86 ± 0.1a |
| C-Reactive Protein, mg/dL | 6.2 ± 1.0 | 5.9 ± 0.5 |
| Functional Mobility, ft | 1351.5 ± 27.2 | 1420.5 ± 13.2a |
| Weekly expenditure from moderate-intesity physical activity, kcal/week | 619.6 ± 207.9 | 1195.3 ± 102.9a |
| Daily caloric intake, kcal/day | 1694.9 ± 163.5 | 1882.5 ± 79.2 |
| Daily saturated fat intake, g/day | 20.3 ± 2.4 | 25.1 ± 1.7 |
between-group difference significant at p<.05
The number of intervention sessions attended by African-American and Caucasian participants was not significantly different, p = .861. In addition, both groups completed similar percentages of food/caloric intake logs (85.5% and 90.0%, respectively) and exercise logs (83.4% and 85.2%, respectively) between Months 0 and 6. There were no significant differences in the percentage of sessions attended by both groups. According to their responses on a program satisfaction questionnaire, African-American and Caucasian participants expressed similar satisfaction with their group leaders (p = .422), but African-American participants expressed higher levels of overall satisfaction with the intervention, p = .014, when compared to their Caucasian counterparts.
Primary outcome: changes in body weight
During the initial phase of the intervention, weight change over time was significantly moderated by race/ethnicity, p < .001. Caucasian participants lost significantly more weight than African-American women (mean ± SE = −10.7 ± .38 kg vs. −6.8 ± .80, respectively). We explored changes during Phase II of the study and found that although there was no significant difference in weight change by race/ethnicity, p = .520, there was a significant interaction between extended-care provision and race/ethnicity, p < .001. Caucasian participants assigned to an extended-care program regained significantly less weight than those in the control condition, with mean weight changes of 1.5 ± .58 kg for the extended-care group and 4.2 ± .79 for the control group, p = .003. Participation in an extended-care program was unrelated to weight regain for African-American participants, however, with weight changes (mean ± SE) of 1.9 ± 1.12 kg for the extended-care group and 1.34 ± 2.04 kg for the control group, p = .815 (see Figure 1).
Figure 1.
Weight change from month 6 to month 18 in African-American and Caucasian participants assigned to extended-care versus control conditions (Mean ± SE).
Secondary outcomes
During the extended-care treatment phase there were three significant interactions between time and race/ethnicity, for LDL cholesterol, p = .007, total caloric intake, p = .017, and saturated fat intake, p = .014. Specifically, while African American participants experienced additional, albeit non-significant, reductions in LDL cholesterol between Month 6 and Month 18 (mean ± SE = −4.25 ± 4.3 mg/dL, p = .329), Caucasian participants experienced significant increases in LDL cholesterol over this time (8.13 ± 2.1 mg/dL, p < .001). Similarly, while African American participants experienced additional decreases in total caloric intake (−148.6 ± 79.9 kcal/day, p = .064) and no significant change in saturated fat intake (−1.3 ± 1.1 g/day, p = .253) from Month 6 to Month 18, Caucasian participants experienced no additional decreases in total caloric intake (65.5 ± 37.8 kcal/day, p = .085) and significant increases in saturated fat intake (2.1 ± .1 g/day, p < .001). There were no significant interactions between ethnicity and time for systolic blood pressure, diastolic blood pressure, triglycerides, Hemoglobin A1c, C-reactive protein, functional mobility, or weekly energy expenditure from physical activity (all ps > .05).
Discussion
The primary aim of this study was to examine racial/ethnic differences in weight changes achieved during the initial and extended-care phases of a lifestyle intervention for obesity delivered in a community-based setting. Although both African-American and Caucasian participants exhibited significant weight reductions during the initial phase of the intervention, weight losses exhibited by Caucasian participants were greater than those achieved by their African-American counterparts. When examining the impact of extended care on weight changes in Caucasian and African-American women, we found that assignment to an extended-care program was associated with smaller weight regain in Caucasian, but not African-American women. In fact, African-American participants exhibited only small and non-significant weight regain regardless of assignment to an extended-care program or to the control condition.
The unique contributions of this study are twofold. First, to our knowledge this is the only effectiveness trial to date that has examined race/ethnicity as a moderator of response to extended-care programs for obesity. Our results suggest that the provision of additional support during the extended-care period did not provide African-American participants with benefits commensurate with those experienced by Caucasian participants. These findings are in accordance with those of Smith West and colleagues (5), who observed a benefit from a motivational-interviewing program for Caucasian but not for African American participants. The study by Smith West and colleagues (5) was an efficacy trial conducted in an urban academic medical center setting. In contrast, our study was an effectiveness trial conducted in a community setting. Nonetheless, the patterns of results were similar in both contexts. Given that there is a greater need for effectiveness trials delivered in real-world settings as opposed to specialty care clinics, our study represents an important contribution to the obesity treatment literature.
Second, the magnitude of weight losses achieves by African-American participants in this lifestyle intervention also represents a major finding. The weight reductions observed among African-American participants in this lifestyle intervention are significantly larger (and in some cases nearly double) than those observed in previous trials. Prior studies (5, 8, 15, 16) that have examined racial/ethnic differences in response to behavioral interventions, including the Weight Loss Maintenance Trial and the Trial of Nonpharmacologic Interventions in Elderly (TONE), have reported weight changes for African-American participants ranging from −1.0 kg to −4.1 kg at 6 months and 0.2 kg to −2.0 kg at 18 months. Overall, these reductions were considerably smaller than those demonstrated by the participants in the current study (−6.9 kg and −5.2 kg at 6 and 18 months, respectively). Nonetheless, even with the larger magnitude of weight losses observed in the current trial, our results are consistent with the existing literature that suggests African-American participants lose smaller amounts of weight during behavioral weight management interventions relative to Caucasian participants.
Because weight regain may diminish the benefits in cardiovascular disease risk factors observed after weight loss, it is important to examine the changes in these factors over time by race/ethnicity. Thus, additional aims of this study inspected racial/ethnic differences in changes in a variety of outcome measures. Interactions between time and race/ethnicity emerged during the extended-care period for three variables. With regard to LDL-cholesterol and saturated fat intake, Caucasian women demonstrated increases during the extended-care period whereas African-American women did not exhibit significant changes. Additionally, only African-American participants achieved further decreases in caloric intake during extended care.
One limitation to this study was the unequal numbers of African-American and Caucasian participants. As larger sample sizes are generally more representative of the population from which the sample is drawn, it is possible that our results better represent the referent Caucasian population than they do the referent African-American population. Second, we did not conduct follow-up assessments beyond 18 months. Therefore, we do not know whether the racial/ethnic differences in weight would be maintained long-term.
The current investigation has a number of important strengths. As noted above, this study yielded significantly larger weight losses among African-American participants than those observed in previous trials, despite being conducted within a community-based setting as opposed to an academic health science center. Further, a notable limitation of prior studies in this area is the confounding of differential socioeconomic status in the racial/ethnic populations under examination (17, 18). The African-American and Caucasian participants in our sample, however, were comparable on variables related to socioeconomic status. Specifically, similar patterns of employment were observed in each racial/ethnic group (48.8% of African-American and 45.3% of Caucasian participants reported holding a full- or part-time job; see Table 1.) and similar percentages of African-American and Caucasian participants reported annual incomes of $50,000 – $99,000 (30.2% and 30.4%, respectively; see Table 1). Thus, it is unlikely that the racial/ethnic differences in weight change observed for our participants were driven by differential access to resources.
The current study contributes important unique information about differences in weight management treatment response between African American and Caucasian individuals. Specifically, we found that while extended care prevented significant weight regain in Caucasian participants, it did not offer similar benefits to African American participants. There are two possible interpretations to this finding. One interpretation is that African-American participants are able to maintain weight losses without the support of an extended-care program. An alternative interpretation is that smaller initial losses may be easier to maintain long-term (19). We do not know if increasing the initial weight losses of African-American participants would result in a similar weight-regain pattern to Caucasian participants.
Enhancing the efficacy of extended-care programs for obesity among African-American participants is an important priority for future research. As Kumanyika (20) and others have suggested, little attention has been paid to cultural factors that may play an important role in response to weight loss treatment among African-American individuals. Given that traditional extended-care programs for obesity rarely include culturally tailored elements, the field may be at risk of developing extended-care weight-management programs that meet the needs of some groups while neglecting others.
To this end, future directions for research include examining how other modes of extended care delivery might influence weight maintenance among African-Americans. For example, the use of peer support as a maintenance strategy has demonstrated mixed effectiveness in samples comprised of Caucasian and minority individuals (21,22), but benefits specific to African-American participants may have been obscured by the unfavorable responses of other racial/ethnic groups. Future trials might also explore the impact of degree of acculturation on the response of African-American participants to extended-care programs. Although culturally tailored treatment elements are often included in health promotion interventions (23), such components may not always be appropriate or salient for all African-American individuals. Given the dearth of research targeting African-American individuals’ response to lifestyle intervention for obesity and to subsequent extended care, future investigations should focus on ways in which treatment might be made to better suit the needs of this population.
Acknowledgments
This research was supported by grant R01HL73326 and R01HL087800 from the National Heart, Lung and Blood Institute.
References
- 1.Perri M, Fuller P. Success and failure in the treatment of obesity: Where do we go from here? Med Exer Nutr Health. 1995;4:255–272. [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Weinsier RL, Hunter GR, Schultz Y, Zuckerman PA, Darnell BE. Physical activity in free-living, overweight white and black women: Divergent responses by race to diet-induced weight loss. Am J Clin Nutr. 2002;76:736–742. doi: 10.1093/ajcn/76.4.736. [DOI] [PubMed] [Google Scholar]
- 4.Foster GD, Wadden TA, Swain RM, Anderson DA, Vogt RA. Changes in resting energy expenditure after weight loss in obese African-American and white women. Am J Clin Nutr. 1999;69:13–17. doi: 10.1093/ajcn/69.1.13. [DOI] [PubMed] [Google Scholar]
- 5.Smith West D, DiLillo V, Bursac Z, Gore SA, Greene PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care. 2007;30:1081–1087. doi: 10.2337/dc06-1966. [DOI] [PubMed] [Google Scholar]
- 6.Perri MG, Corsica JA. Improving the maintenance of weight lost in behavioral treatment of obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of obesity treatment. Guilford Press; New York: 2002. pp. 357–379. [Google Scholar]
- 7.Diabetes Prevention Program Research Group. Achieving weight and activity goals among Diabetes Prevention Program lifestyle participants. Obesity. 2004;12:1426–1435. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens VJ, Obarzanek E, Cook NR, et al. Long-term weight loss and changes in blood pressure: Results of the trials of hypertension prevention, phase II. Ann Intern Med. 2001;134:1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 9.Perri MG, Limacher MC, Durning PE, et al. Extended-care programs for weight Management in rural communities: The Treatment of Obesity in Underserved Rural Settings (TOURS) Randomized Trial. Arch Intern Med. 2008;168(21):2347–2354. doi: 10.1001/archinte.168.21.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A databased approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 11.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willet, and National Cancer Institute Food Frequency Questionnaires. Am J Epidemiol. 2001;154:1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 12.Kervio G, Ville NS, Leclercq C, Daubert JC, Carre F. Intensity and daily reliability of the six-minute walk test in moderate chronic heart failure patients. Arch Phys Med Rehabil. 2004;85:1513–1518. doi: 10.1016/j.apmr.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 13.Zugck C, Kruger C, Durr S, et al. Is the 6-minute walk test a reliable substitute for peak oxygen uptake in patients with dilated cardiomyopathy? Eur Heart J. 2000;21:540–549. doi: 10.1053/euhj.1999.1861. [DOI] [PubMed] [Google Scholar]
- 14.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Kumanyika SK, Espeland MA, Bahnson JL, et al. Ethnic Comparison of Weight Loss in the Trial of Nonpharmacologic Interventions in the Elderly. Obes Res. 2002;10:96–106. doi: 10.1038/oby.2002.16. [DOI] [PubMed] [Google Scholar]
- 16.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of Strategies for Sustaining Weight Loss: The Weight Loss Maintenance Randomized Controlled Trial. JAMA. 2008;299:1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 17.Wassertheil-Smoller S, Langford HG, Blaufox MD, et al. Effective dietary intervention in hypertensives: sodium restriction and weight reduction. J Am Diet Assoc. 1985;85:423–430. [PubMed] [Google Scholar]
- 18.Juhaeri B, Stevens J, Chambless LE, et al. Associations of weight loss and changes in fat distribution with the remission of hypertension in a bi-ethnic cohort: the Artherosclerosis Risk in Communities Study. Prev Med. 2003;36:330–339. doi: 10.1016/s0091-7435(02)00063-4. [DOI] [PubMed] [Google Scholar]
- 19.Lutes LD, Winett RA, Barger SD, et al. Small changes in nutrition and physical activity promote weight loss and maintenance: 3-month evidence from the ASPIRE randomized trial. Ann Behav Med. 2008;35:351–357. doi: 10.1007/s12160-008-9033-z. [DOI] [PubMed] [Google Scholar]
- 20.Kumanyika SK, Obarzanek E, Stevens VJ, Hebert PR, Whelton PK. Weight-loss experiences of black and white participants in NHLBI-sponsored clinical trials. Am J Clin Nutr. 1991;53:1631S–1638S. doi: 10.1093/ajcn/53.6.1631S. [DOI] [PubMed] [Google Scholar]
- 21.Perri MG, McAdoo WG, McAllister DA, et al. Effects of peer support and therapist contact on long-term weight loss. J Consult Clin Psychol. 1987;55:615–617. doi: 10.1037/0022-006X.55.4.615. [DOI] [PubMed] [Google Scholar]
- 22.Verheijden MW, Bakx JC, van Weel C, Koelen MA, van Staveren WA. Role of social support in lifestyle-focused weight management interventions. Eur J Clin Nutr. 2005;59:S179–S186. doi: 10.1038/sj.ejcn.1602194. [DOI] [PubMed] [Google Scholar]
- 23.Newton RL, Perri MG. A randomized pilot trial of exercise promotion in sedentary African-American adults. Ethn Dis. 2004;14:548–557. [PubMed] [Google Scholar]