Abstract
Importance
This study provides further evidence from a national sample to generalize the relationship between depression and vision loss to adults across the age spectrum. Better recognition of depression among people reporting reduced ability to perform routine activities of daily living due to vision loss is warranted.
Objectives
To estimate, in a national survey of US adults 20 years of age or older, the prevalence of depression among adults reporting visual function loss and among those with visual acuity impairment. The relationship between depression and vision loss has not been reported in a nationally representative sample of US adults. Previous studies have been limited to specific cohorts and predominantly focused on the older population.
Design
The National Health and Nutrition Examination Survey (NHANES) 2005–2008.
Setting
A cross-sectional, nationally representative sample of adults, with prevalence estimates weighted to represent the civilian, noninstitutionalized US population.
Participants
A total of 10 480 US adults 20 years of age or older.
Main Outcome Measures
Depression, as measured by the 9-item Patient Health Questionnaire depression scale, and vision loss, as measured by visual function using a questionnaire and by visual acuity at examination.
Results
In 2005–2008, the estimated crude prevalence of depression (9-item Patient Health Questionnaire score of ≥10) was 11.3% (95% CI, 9.7%–13.2%) among adults with self-reported visual function loss and 4.8% (95% CI, 4.0%–5.7%) among adults without. The estimated prevalence of depression was 10.7% (95% CI, 8.0%–14.3%) among adults with presenting visual acuity impairment (visual acuity worse than 20/40 in the better-seeing eye) compared with 6.8% (95% CI, 5.8%–7.8%) among adults with normal visual acuity. After controlling for age, sex, race/ethnicity, marital status, living alone or not, education, income, employment status, health insurance, body mass index, smoking, binge drinking, general health status, eyesight worry, and major chronic conditions, self-reported visual function loss remained significantly associated with depression (overall odds ratio, 1.9 [95% CI, 1.6–2.3]), whereas the association between presenting visual acuity impairment and depression was no longer statistically significant.
Conclusions and Relevance
Self-reported visual function loss, rather than loss of visual acuity, is significantly associated with depression. Health professionals should be aware of the risk of depression among persons reporting visual function loss.
Vision loss and depression have been reported in older adult cohorts around the world.1–8 A meta-analysis9 has shown that vision loss is among the most common chronic conditions associated with depression in old age. However, for younger adults, the relationship between vision loss and depression has not been well studied. Furthermore, in the United States, the national-level associations of visual function and visual acuity with depression remain unknown. Many conditions resulting in vision loss can be delayed or prevented,10,11 and depression is a treatable condition12,13 that can be identified by screening.14 Estimates of the prevalence of depression among people with and without vision loss, on a national level, could inform the need for medical care and referral services. Alleviating the joint burden of depression and vision loss would improve the quality of life for those affected.
Herein, we examine the prevalence of depression among community-dwelling adults in the United States 20 years of age or older with normal vision and those with vision loss, and we describe the associations between depression and vision loss as measured by reported loss of visual function and by measured visual acuity.
METHODS
STUDY POPULATION
The National Health and Nutrition Examination Survey (NHANES) is a nationally representative survey conducted by the Centers for Disease Control and Prevention (CDC).15 In NHANES 2005–2008, a total of 10 480 persons 20 years of age or older were interviewed to collect sociodemographic, medical, and family information, and subsequently they underwent a detailed medical examination at the Medical Examination Center. The response rates were 74% for those participating in the home interview and 71% for those reporting to the Medical Examination Center.16 The NHANES protocol was approved by a human subjects review board at the CDC. Informed consent was obtained from all participants.
VISUAL FUNCTION
In their home, participants were asked about eyesight and activity limitations due to their vision. The questions used were selected from the National Eye Institute 25-item Visual Functioning Questionnaire, for which reliability and validity have been reported previously.17 Limitations in activities of daily living due to vision were assessed in 6 survey questions asking about the degree of difficulty (none, a little, moderate, extreme, or unable to do) in the following: reading ordinary newsprint; doing work or hobbies that require seeing well up close; going down steps, stairs, or curbs in dim light or at night; noticing objects off to the side while walking; finding objects on a crowded shelf; and daytime driving in familiar places. Responses to these individual items were dichotomized (presence or absence), and 2 derived measures were coded to represent overall visual function loss based on cumulative responses to the following items: number of visual function problems (ranging from 0 to 6) and the presence of any visual function loss.
VISUAL ACUITY
The physical examination in the Medical Examination Center included a vision examination. With the use of a Nidek ARK-760 autorefractor containing built-in visual acuity charts, presenting distance visual acuity was measured in each eye with whichever form of correction (eg, glasses or contact lenses), if any, that the participant was wearing at the time of the examination. For eyes with presenting acuity of 20/30 or worse, distance visual acuity was reassessed after an objective autorefraction. Persons who were completely blind (ie, unable to see in both eyes) or who had a severe infection in at least 1 eye were excluded from the vision examination (n=17).
Presenting visual acuity impairment was defined as a presenting visual acuity of worse than 20/40 in the better-seeing eye. Uncorrectable visual acuity impairment was defined as a visual acuity of worse than 20/40 in the better-seeing eye after the autorefractor provided optical correction. Correctable visual acuity impairment (ie, impairment due to refractive error) was defined as a presenting visual acuity of worse than 20/40 in the better-seeing eye that improved to 20/40 or greater after objective autorefraction.
DEPRESSION MEASURE
The 9-item Patient Health Questionnaire (PHQ-9) depression scale was used to measure depression. The PHQ, which is widely used in both clinical and research settings, is a self-administered version of the Primary Care Evaluation of Mental Disorders.18 The validity and reliability of the PHQ and its 9-item depression module to establish depressive diagnosis and grade severity have been widely documented.19–22 The PHQ-9 has also been used to assess depression among those with visual impairment in other studies.3,6,23 A PHQ-9 score of 10 or greater is recommended as a cut point for screening purposes, yields 88% sensitivity and 88% specificity for identifying major depression,18 and was used in our study to identify cases of depression.
OTHER MEASUREMENTS
We considered factors that have been reported in the literature as being associated with both vision loss and depression as possible covariates.4 All participants were asked about age (20–39, 40–64, or ≥65 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, or those who selected multiple races or other racial/ethnic groups), educational attainment (less than a high school diploma, high school graduate, or education beyond high school), household income (poverty income ratio [PIR] < 1,1≤PIR<3, or PIR≥3), marital status (yes or no), living alone (yes or no), employed (yes or no), health insurance status (yes or no), smoking status (current, former, or never), binge drinking (defined as having ever consumed ≥5 drinks of any kind of alcoholic beverage almost every day; yes or no), and history of cardiovascular diseases (yes or no). A history of cardiovascular diseases was ascertained by self-report of coronary heart disease, angina, myocardial infarction, stroke, or congestive heart failure. A prior self-reported history of cancer was included. Diabetes was defined as a self-report of a previous diagnosis of the disease by a health care provider (excluding gestational diabetes mellitus) or a hemoglobin A1c level of 6.5% or greater (which is the American Diabetes Association’s diagnostic criterion for diabetes [to convert to proportion of total hemoglobin, multiply by 0.01]).24 Hypertension was defined as antihypertensive medication use or a reported blood pressure of 140/90 mm Hg or higher. The participants were also asked how much of the time they worried about their eyesight (none, a little, some, most, or all of the time). Height and weight were measured in the Medical Examination Center, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. We divided respondents into 3 BMI groups: normal weight or underweight (BMI < 25), overweight (BMI = 25 to <30), and obese (BMI ≥ 30).
STATISTICAL METHODS
Statistical analyses were conducted using SAS, version 9.2 (SAS Institute Inc), and SUDAAN, version 10.1 (Research Triangle Institute), to calculate national estimates and their standard errors, accounting for the survey’s complex sampling design. Taylor series linearization was used for variance estimation.25 Missing values were imputed to avoid bias associated with listwise deletion of participants with missing values from the analysis. We used multiple imputation by chained equations, a technique using regression based on all variables in the model, to attribute missing data.26,27 Five imputations per missing observation were performed and analyzed. Characteristics of the study population are described using mean values for continuous variables and percentages for categorical variables. The t test was used for continuous variables, and the χ2 test was used for categorical variables. We estimated the crude prevalence of depression (PHQ-9 score of ≥10) by sociodemographic characteristics in the adult US population. In addition, we provided specific estimates of depressive symptoms by severity using 3 categories: mild (PHQ-9 score of 5–9), moderate (PHQ-9 score of 10–14), and moderate severe to severe (PHQ-9 score of 15–27). Logistic regression was used to assess the associations between visual function loss and depression and between visual acuity impairment and depression after adjusting for other covariates. Odds ratios (ORs) and associated 95% CIs were calculated. Associations were considered to be statistically significant if the P value was less than .05.
RESULTS
The NHANES sample for this analysis included 10 480 participants whose mean age was 47 years (Table 1). Fifty-two percent of participants were female, 71% were non-Hispanic whites, 11% were non-Hispanic blacks, and 8% were Mexican Americans. Overall, 23% were current smokers, 15% were binge drinkers, and many had chronic health conditions such as hypertension (33%), diabetes (11%), cardiovascular disease (7%), and cancer (9%).
Table 1.
Selected Characteristics of 10 480 US Adults 20 Years of Age or Older, NHANES 2005–2008
| Characteristic | Weighted % (95% CI) |
|---|---|
| Age group, y | |
| 20–39 | 37.8 (35.8–39.7) |
| 40–64 | 38.9 (37.2–40.6) |
| ≥65 | 23.3 (21.3–25.5) |
| Age, mean, y | 46.7 (45.8–47.5) |
| Male sex | 48.1 (47.3–48.9) |
| Race/ethnicity | |
| Non-Hispanic white | 70.6 (65.7–75.1) |
| Non-Hispanic black | 11.4 (8.9–14.4) |
| Mexican American | 8.2 (6.5–10.2) |
| Other | 9.8 (7.9–12.2) |
| <High school | 19.2 (17.1–21.4) |
| PIR | |
| PIR <1 | 12.8 (11.4–14.2) |
| 1 ≤ PIR <3 | 36.5 (34.0–39.1) |
| PIR ≥3 | 50.8 (47.4–54.1) |
| Currently working | 65.7 (63.4–67.9) |
| Married or living with partner | 64.8 (62.5–67.0) |
| Living alone | 13.6 (12.5–14.7) |
| Uninsured | 19.2 (17.2–21.4) |
| BMIa | |
| Normal weight or underweight | 32.4 (30.8–34.0) |
| Overweight | 33.6 (32.5–34.8) |
| Obese | 34.0 (32.2–35.9) |
| Smoking status | |
| Current smoker | 23.4 (21.6–25.2) |
| Former smoker | 24.5 (23.2–25.8) |
| Never smoked | 52.2 (50.0–54.3) |
| Binge drinkerb | 15.1 (14.0–16.3) |
| Self-rated fair or poor health | 17.6 (16.2–19.1) |
| Hypertensionc | 33.0 (31.4–34.6) |
| Diabetesd | 10.5 (9.5–11.6) |
| History of CVDs | 7.0 (6.1–7.9) |
| History of cancer | 8.6 (7.9–9.3) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CVDs, cardiovascular diseases; NHANES, National Health and Nutrition Examination Survey; PIR, poverty to income ratio.
The BMI was divided into 3 groups: normal weight or underweight (BMI <25), overweight (BMI = 25 to <30), and obese (BMI ≥ 30).
Defined as having ever consumed 5 drinks or more of any kind of alcoholic beverage almost every day.
Defined as antihypertensive medication use or a reported blood pressure of 140/90 mm Hg or higher.
Defined as self-reported diabetes diagnosed by a health professional (all adults) or a hemoglobin A1c level of 6.5% or greater (to convert to proportion of total hemoglobin, multiply by 0.01) (nonpregnant adults only).
The estimated (weighted) crude prevalence of depression (PHQ-9 score of ≥ 10) in the 2005–2008 sample was 11.3% (95% CI, 9.7%–13.2%) among those with visual function loss and 4.8% (95% CI, 4.0%–5.7%) among those without (Table 2). Across age groups, adults with visual function loss were more likely to report depression than their counterparts (13.0% vs 4.7% for those 20–39 years of age, 11.5% vs 6.0% for those 40–59 years, and 9.6% vs 3.0% for those ≥60 years) (eTable, jamaophth.com). In addition, 20.1% (95% CI, 18.5%–21.8%) of adults with visual function loss had some mild depressive symptoms (PHQ-9 score of 5–9) compared with 12.1% (95% CI, 11.0%–13.2%) of those without impaired visual function.
Table 2.
Crude Prevalence of Depression by Visual Function Status and Depression Severity in US Adults 20 Years of Age or Older, NHANES 2005–2008a
| Status | Participants, No. |
Prevalence of Depression, Weighted % (95% CI) |
|||
|---|---|---|---|---|---|
| Moderate to Severe (PHQ-9 Score of ≥10) |
Mild (PHQ-9 Score of 5–9) |
Moderate (PHQ-9 Score of 10–14) |
Moderately Severe to Severe (PHQ-9 Score of ≥15) |
||
| Difficulty reading ordinary newsprintb |
|||||
| No | 8046 | 5.3 (4.5–6.3) | 13.3 (12.3–14.5) | 3.5 (3.0–4.1) | 1.7 (1.3–2.3) |
| Yes | 2419 | 13.4 (11.0–16.2) | 20.6 (18.4–23.0) | 8.5 (6.7–10.8) | 4.6 (3.5–6.2) |
| Difficulty seeing up close when doing work or hobbies |
|||||
| No | 8527 | 5.6 (4.8–6.5) | 13.8 (12.7–14.9) | 3.8 (3.3–4.5) | 1.7 (1.3–2.2) |
| Yes | 1938 | 12.9 (10.6–15.7) | 19.6 (17.3–22.1) | 7.7 (6.0–9.8) | 5.1 (3.8–6.8) |
| Difficulty seeing steps or curbs in dim light |
|||||
| No | 8510 | 5.3 (4.5–6.1) | 13.0 (11.9–14.2) | 3.5 (3.0–4.1) | 1.7 (1.3–2.2) |
| Yes | 1954 | 15.9 (13.0–19.2) | 24.4 (22.1–26.8) | 9.9 (7.8–12.4) | 5.9 (4.6–7.5) |
| Difficulty noticing objects off to the side |
|||||
| No | 9328 | 5.8 (5.0–6.7) | 14.0 (13.0–15.1) | 3.9 (3.3–4.6) | 1.8 (1.4–2.2) |
| Yes | 1140 | 19.7 (16.0–24.0) | 23.8 (20.1–27.9) | 11.2 (8.5–14.5) | 8.4 (6.4–10.9) |
| Difficulty finding object on a crowded shelf |
|||||
| No | 9119 | 5.6 (4.8–6.6) | 13.9 (13.0–14.9) | 3.8 (3.2–4.5) | 1.7 (1.3–2.3) |
| Yes | 1347 | 18.4 (15.1–22.3) | 22.8 (19.9–26.1) | 10.9 (8.3–14.2) | 7.4 (5.5–9.8) |
| Difficulty driving in the daytime in a familiar place |
|||||
| No | 9798 | 6.1 (5.2–7.2) | 14.6 (13.6–15.6) | 4.1 (3.4–4.8) | 2.0 (1.6–2.5) |
| Yes | 655 | 25.0 (20.0–30.7) | 20.2 (15.8–25.3) | 15.1 (11.2–20.1) | 9.7 (6.2–14.9) |
| Impaired visual functionc | |||||
| No | 6609 | 4.8 (4.0–5.7) | 12.1 (11.0–13.2) | 3.2 (2.7–3.8) | 1.5 (1.1–2.0) |
| Yes | 3871 | 11.3 (9.7–13.2) | 20.1 (18.5–21.8) | 7.1 (5.9–8.6) | 4.0 (3.2–5.1) |
Abbreviations: NHANES, National Health and Nutrition Examination Survey; PHQ-9, 9-item Patient Health Questionnaire.
Defined as a PHQ-9 score of 10 or greater.
Moderate, extreme, or unable to do.
Defined as any of the impaired visual functions listed.
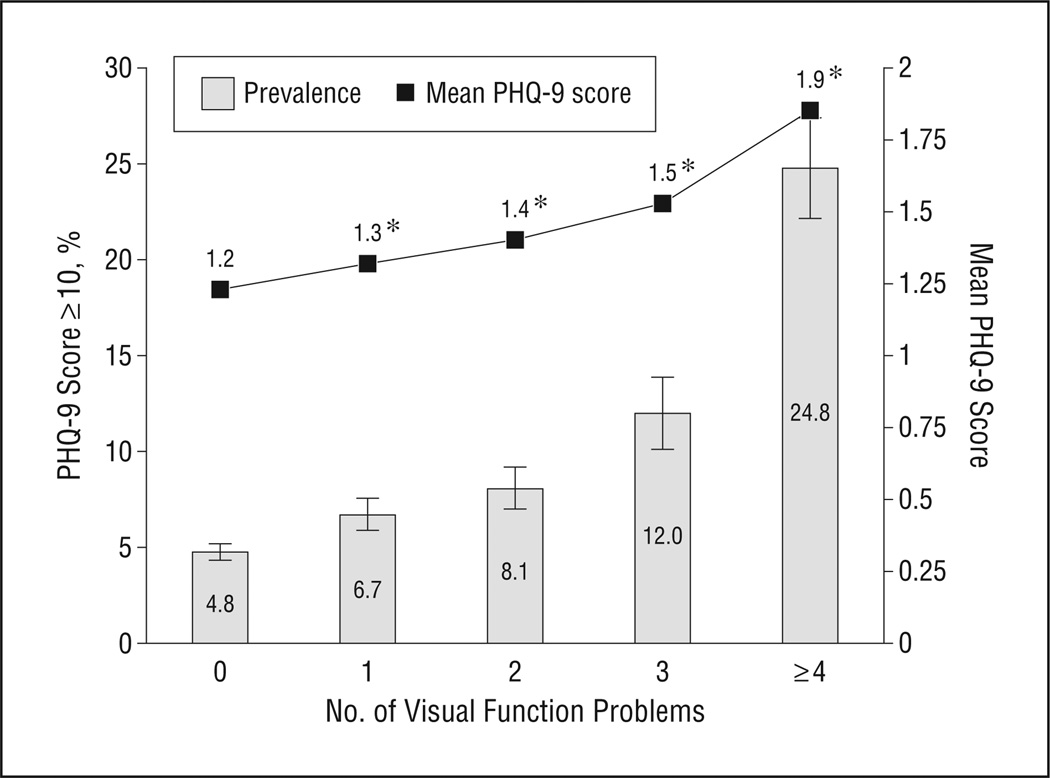
The findings for overall depression and depression severity by each specific visual function activity all showed a similar pattern (Table 2). Among persons with difficulty reading ordinary newsprint, approximately 13.4% (95% CI, 11.0%–16.2%) had depression compared with 5.3% (95% CI, 4.5%–6.3%) of those without difficulty reading. Approximately 12.9% (95% CI, 10.6%–15.7%) of those with difficulty seeing up close when doing work or hobbies had depression, whereas 5.6% (95% CI, 4.8%–6.5%) of those without difficulty seeing up close had depression. The prevalence of depression was also higher among those with difficulty seeing steps, noticing objects off to the side, those with difficulty finding objects on a crowded shelf, and those with difficulty driving in daytime compared with those without such difficulties (15.9% vs 5.3%, 19.7% vs 5.8%, 18.4% vs 5.6%, and 25.0% vs 6.1%, respectively). Moreover, as the number of visual function problems increased among the participants, the prevalence and the severity of depression also increased (Figure).
Figure.
Crude prevalence (weighted percentages are presented) of depression (defined as a PHQ-9 score of ≥10) from the National Health and Nutrition Examination Survey 2005–2008. *P < .01 for comparison with mean PHQ-9 score by number of visual function problems (reference: mean PHQ-9 score for those reporting no visual function problems). PHQ-9 indicates 9-item Patient Health Questionnaire.
In contrast, the estimated (weighted) crude prevalence of depression was 10.7% (95% CI, 8.0%–14.3%) among those with presenting visual acuity impairment and 6.8% (95% CI, 5.8%–7.8%) among persons without presenting visual acuity impairment (Table 3). Among those with presenting visual acuity impairment, approximately 6.8% (95% CI, 5.9%–7.8%) of those with correctable visual acuity impairment and 10.9% (95% CI, 7.7%–15.2%) of those with uncorrectable visual acuity impairment had depression.
Table 3.
Crude Prevalence of Depression by Visual Impairment Status in US Adults 20 Years of Age or Older, NHANES 2005–2008a
| Status | Participants, No. |
Prevalence of Depression, Weighted % (95% CI) |
|||
|---|---|---|---|---|---|
| Moderate to Severe (PHQ-9 Score of ≥10) |
Mild (PHQ-9 Score of 5–9) |
Moderate (PHQ-9 Score of 10–14) |
Moderately Severe to Severe (PHQ-9 Score of ≥15) |
||
| Presenting visual acuity impairmentb |
|||||
| No | 9541 | 6.8 (5.8–7.8) | 14.7 (13.8–15.7) | 4.3 (3.7–5.0) | 2.3 (1.9–2.8) |
| Yes | 939 | 10.7 (8.0–14.3) | 16.6 (13.9–19.6) | 8.0 (5.6–11.2) | 2.7 (1.6–4.6) |
| Among those with presenting visual acuity impairment |
|||||
| Correctable | 252 | 6.8 (5.9–7.8) | 14.8 (13.8–15.8) | 4.3 (3.7–5.0) | 2.3 (1.9–2.8) |
| Uncorrectable | 687 | 10.9 (7.7–15.2) | 16.2 (13.0–19.9) | 8.3 (5.7–12.0) | 2.6 (1.2–5.2) |
Abbreviations: NHANES, National Health and Nutrition Examination Survey; PHQ-9, 9-item Patient Health Questionnaire.
Defined as a PHQ-9 score of 10 or greater.
Defined as presenting visual acuity worse than 20/40 in the better-seeing eye. Uncorrectable visual acuity impairment was defined as visual acuity worse than 20/40 in the better-seeing eye after the autorefractor provided optical correction. Correctable visual acuity impairment (ie, impairment due to refractive error) was defined as presenting visual acuity worse than 20/40 in the better-seeing eye before an objective autorefraction test that eventually improved visual acuity (≥20/40) after objective autorefraction.
Table 4 shows the associations of depression with visual function loss and visual acuity impairment among US adults. In multivariate analysis, overall visual function loss was associated with increased odds (OR, 2.6 [95% CI, 2.2–3.1]) of depression after adjusting for age, sex, and race/ ethnicity (Table 4, model I). The ORs slightly decreased (OR, 2.4 [95% CI, 2.0–2.9]) after further adjustment for socioeconomic characteristics (model II: model I plus marriage, living alone, education, income, employment status, and health insurance). The odds of depression were significantly higher among those with any visual function difficulty (OR, 1.9 [95% CI, 1.6–2.3]), even after controlling for all other factors, including unhealthy behavior (eg, smoking and binge drinking), self-reported health, BMI, and other chronic conditions (model III: model II plus BMI, smoking, binge drinking, self-reported health, worry about eyesight, diabetes, hypertension, cardiovascular disease, and cancer). Across all models, each measure of visual function loss was consistently significantly associated with depression. After controlling for age, sex, and race/ethnicity (model I), adults with presenting visual acuity impairment had higher odds of depression than their counterparts (OR, 1.6 [95% CI, 1.1–2.2]). However, there was no statistically significant association between depression and visual acuity impairment (presenting, correctable, and uncorrectable) in any models after controlling for other additional factors (models II and III).
Table 4.
Multivariate Analysis for Depression Associated With Visual Function Loss and Visual Impairment, Each Modeled Separately in US Adults 20 Years of Age or Older, NHANES 2005–2008a
| Odds Ratio (95% CI) |
|||
|---|---|---|---|
| Status | Model Ib | Model IIc | Model IIId |
| Visual function loss | |||
| No difficulty | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Difficulty reading ordinary newsprinte | 2.7 (2.1–3.6) | 2.4 (1.9–3.2) | 1.9 (1.5–2.6) |
| Difficulty seeing up close when doing work or chores | 2.6 (2.1–3.2) | 2.5 (2.0–3.1) | 2.0 (1.6–2.5) |
| Difficulty seeing steps or curbs in dim light | 3.4 (2.7–4.3) | 2.8 (2.2–3.5) | 2.0 (1.6–2.6) |
| Difficulty noticing objects off to the side | 3.8 (3.0–4.9) | 3.1 (2.5–4.0) | 2.4 (1.8–3.1) |
| Difficulty finding object on crowded shelf | 3.8 (3.0–4.9) | 3.1 (2.4–4.0) | 2.4 (1.8–3.2) |
| Difficulty driving in the daytime in a familiar place | 4.9 (3.5–6.8) | 3.4 (2.4–4.7) | 2.7 (1.8–3.9) |
| Impaired visual functionf | 2.6 (2.2–3.1) | 2.4 (2.0–2.9) | 1.9 (1.6–2.3) |
| Visual impairment | |||
| No impairment | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Presenting | 1.6 (1.1–2.2) | 1.1 (0.8–1.6) | 1.1 (0.8–1.5) |
| Correctable | 1.6 (1.1–2.3) | 1.2 (0.8–1.8) | 1.2 (0.8–1.8) |
| Uncorrectable | 1.4 (0.7–2.9) | 0.9 (0.4–1.8) | 0.8 (0.4–1.7) |
Abbreviation: NHANES, National Health and Nutrition Examination Survey.
Defined as a 9-item Patient Health Questionnaire score of 10 or greater.
Controlling for age, sex, and race/ethnicity.
Model I plus marriage, living alone, education, income, employment status, and health insurance.
Model II plus body mass index, smoking, binge drinking, self-reported health, worry about eyesight, diabetes, hypertension, cardiovascular disease, and cancer.
Moderate or extreme difficulty or unable to do.
Defined as any of the impaired visual functions listed.
COMMENT
One in 10 US adults reporting loss of visual function meets criteria for clinically significant depressive disorder, and an additional 1 in 5 exhibits mild depressive symptoms (PHQ-9 score of 5–9). These rates of depression are comparable to rates of depression in persons with other chronic conditions.28 Blindness was ranked as the fourth most feared health condition, after AIDS, cancer, and Alzheimer disease.29 People with any kind of visual function loss are more likely than those with none to report depression, especially in key activities of daily living such as driving. Even after considering possible confounding factors, adults with visual function loss are at least 90% more likely to have depression than those without visual function loss.
To the best of our knowledge, this is the first study to assess, in a national sample, depressive symptoms in conjunction with visual function and visual acuity loss. Previous studies have used the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition),30 the Center for Epidemiologic Studies–Depression scale,7 the Geriatric Depression Scale,30 the Beck Depression Inventory,31 the Hamilton Rating Scale for Depression,32 the 12- or 36-item Short Form Health Survey,4 and the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes33,34 to assess depression and depressive symptomology. Although previous studies35–37 have suggested an association between vision loss and depression among the older population, our study provides further evidence to generalize this relationship to adults across the age spectrum.
VISION LOSS AND DEPRESSION
Self-reported visual functioning reflects a person’s perception of his or her ability to perform vision-related daily activities. The association between visual function loss and depression is complicated. Depression and disability may exist in a bidirectional relationship in which depression leads to disability and in which disability causes depression.38 Although it is not possible from this cross-sectional analysis to determine whether depression is a cause or an effect of visual function loss, it may be that people with depressive symptoms have actual physical limitations or perceived limitations. Individuals whose lifestyles have been influenced by a real or perceived reduced ability to perform instrumental activities of daily living (such as reading a medication label, recognizing a face, writing a check, or driving a vehicle) have been shown to be at higher risk for depression.39 Studies40,41 have reported that the presence of major age-related eye diseases (such as age-related macular degeneration [AMD] and glaucoma) are associated with an increased risk of depression. People with impaired vision often report that they feel unhappy, lonely, or even hopeless.42 In the English Longitudinal Study of Aging (Waves 1 and 2),7 self-reported vision loss was a consistent predictor of both onset and persistence of depression after adjusting for other covariates. Findings from the present study are consistent with this published literature. Moreover, a large population-based study5 from 10 European countries found that persons with self-reported impaired vision were more likely to report concentration problems; losing interest and enjoyment; feeling fatigued, irritable, sad, and tearful; having less hope for the future; and, in some cases, wishing for death.
People who are depressed may not seek out eye care when experiencing visual difficulties. They also may not realize, unless asked, that they even have difficulties with their vision. For those with diagnosed eye conditions, depression may cause poor adherence to treatment, which may, in turn, hasten the progression of vision loss. As a result, the association between visual function and depression could be further complicated because a depressive mood might adversely affect a person’s self-reported visual function.2,30 Such an inverse association has also been found in other diseases.31,43–45 One study46 found that depressive symptoms explained 40% to 50% of the variance of participation in daily activities and social roles. Another study3 suggested that vision-specific distress was the strongest unique predictor of depressive symptoms; the emotional consequence of vision loss thus plays a critical role that is separate from the severity and duration of visual acuity impairment and functional loss. A study by Ishii et al47 found that cataract surgery, which improves a patient’s eyesight significantly, improved the vision-related quality of life and depressive mental status of elderly patients. Owsley at al48 reported that nursing home residents with uncorrected refractive error improved their quality of life and decreased their depressive symptoms after undergoing refractive correction.
Visual acuity and contrast sensitivity are 2 major predictors of visual function loss.1,49–51 Visual acuity is important for activities involving good resolution and adaptation to changing light conditions, whereas contrast sensitivity is associated with activities involving distance judgments, night driving, and mobility.49 There is a substantial literature reporting the effect of loss of visual acuity on a decrease in quality of life and an increase in depression among people with AMD.2,30,52–59 Among persons 65 years of age or older with glaucoma, those with vision loss (identified using ICD-9 codes) were more likely to develop depression (OR, 1.63 [95% CI, 1.54–1.73]) than those without vision loss.33 A recent population-based, retrospective cohort study34 in an older population in Quebec, Canada, found that clinically diagnosed vision impairment independently increased the risk of depression (hazard ratio, 1.35 [95% CI, 1.10–1.66] for severe cases; hazard ratio, 1.35 [95% CI, 1.09–1.69] for moderate visual impairment). Other studies2,37,41,60 also found that visual acuity loss and depressive symptoms were independently associated with visual function status in people 65 years of age or older.
In this analysis, the significance level of the association between visual function loss and depression was lower after we controlled for socioeconomic factors, and it was further reduced after we controlled for other confounding behavior and health condition factors. However, we did not find a statistically significant association between impairment of visual acuity (presenting, correctable, and uncorrectable) and depression after controlling for all potential confounders. Bookwala and Lawson,61 using data from National Social Life, Health, and Aging Project, also found that objective vision (visual acuity) contributed significantly to functional limitations but was unrelated to depressive symptoms. Likely, the association between vision loss and depression could be related to other factors in addition to reduced visual acuity, particularly the disability that vision loss causes in a person’s life. People with uncorrectable visual acuity impairment may have adjusted to their physical limitation or may have implemented compensatory strategies and do not have strong depressive feelings. However, failing to reject the null hypothesis does not imply that the null hypothesis is true, only that the effect, if present, was too weak to detect with our sample. In addition, self-reported visual function loss represents a person’s actual health condition and its effect on his or her daily activities. Their perceptions may reflect the overall function of vision, including not only the effect of loss of visual acuity but also other effects due to impairment (such as contrast sensitivity) of optical organs.
PUBLIC HEALTH IMPLICATIONS
The high prevalence of depression among people with visual function loss, especially among the older population, suggests that eye care providers and primary care providers should be aware of the increased risk of depression among those with vision loss. Depression alone is a major cause of disability independent of vision loss.62,63 Moreover, people with vision loss are more likely than those without to have other comorbid chronic conditions, disability, lack of social networking, worse overall health, and reduced access to health care.64,65 The capability to perform daily tasks of persons with both vision loss and depression is even more compromised.66 In particular, difficulty may be experienced when driving to a clinic and communicating with health care professionals owing to the combined effects of vision loss and depression. These circumstances limit these persons’ ability to seek needed care. Several studies67,68 have indicated that receipt of rehabilitation services and the use of assistive devices are useful in addressing the issue of depression. A randomized, controlled trial53 of a self-management program involving cognitive and behavioral interventions for persons with AMD reported a significantly, clinically meaningful reduction in depressive symptoms after a 6-month follow-up. Improvements in mood and function were significantly greater for those with depression than for those without depression.69 Another study70 also found that interventions that teach patients problem-solving skills and that teach patients to identify practical solutions could prevent depressive disorders in patients with AMD.
Our findings suggest that eye care professionals should consider patients’ psychological conditions and provide referrals to those exhibiting depressive symptoms. Early diagnosis and prompt treatment could offer real benefit. For those at higher risk for depression, a potential screening tool might be useful. For example, eye care professionals and primary care providers may use PHQ-9 in clinical settings to screen patients with depressive symptoms and refer them for further evaluation if needed. Moreover, it is important for health care professionals to be aware of the prevalence of such conditions because they are often the first to interact with these patients on a consistent basis. Brody et al30 found that, among 151 adults with advanced AMD who were 60 years of age or older, almost one-third had a depressive disorder. Shmuely-Dulitzki et al63 found that 38.6% of people entering a low-vision clinic met the criteria for major depression according to the Diagnostic and Statistical Manual of Mental Disorders (Third Edition Revised) criteria, and yet only a very few received treatment. Another study71 found that fewer than 1 in 3 eye care providers attempt to identify depressive symptoms as a regular component of patient care. Effective training of eye care professionals of vision loss and depression might allow them to better prepare patients and their families to identify and manage depressive symptoms, especially among older persons whose activities of daily living have already been compromised by other chronic conditions.
The strengths of our study include its population-based national sample, its inclusion of persons with measured visual acuity impairment, and its effective detection of depressive symptoms using a short, easy-to-administer, and well-validated instrument, the PHQ-9. Survey participants who had no light perception or who had a severe infection in 1 or both eyes were excluded; this might bias the prevalence estimates toward the null, although the number of individuals excluded for these reasons were few. Because of data limitations, we were unable to assess the association of glare or contrast sensitivity with depression. Owing to limitations inherent with the NHANES sampling frame, we were unable to estimate the prevalence among racial/ethnic groups other than non-Hispanic whites, non-Hispanic blacks, and Mexican Americans. Finally, our data’s cross-sectional nature makes it difficult to make causal inference. However, our findings are consistent with the existing literature and highlight the emerging public health need to address depression among people reporting loss of visual function.
In conclusion, our study provides nationally representative estimates on the prevalence of depression among persons with visual function loss and impairment in visual acuity. We found strong associations between loss of visual function (rather than loss of visual acuity) and the presence of depressive symptoms among US adults. Better recognition of depression among people reporting reduced ability to perform routine activities of daily living due to vision loss is warranted. Improved access to screening, diagnosis, and treatment of depression by eye care professionals and primary care providers may help to reduce the burden of depression-related excess disability and improve the quality of life among people with vision loss.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by the National Center for Health Statistics of the CDC. Funding for the NHANES retinal component was provided by intraagency agreement 05FED47304 from the Division of Diabetes Translation of the CDC. Funding for the vision component was provided by Intramural Research Program award ZIAEY000402 from the National Eye Institute/National Institutes of Health.
Role of the Sponsors: The National Center for Health Statistics was involved in the design and conduct of the NHANES and in data collection, but it was not involved in the analysis or interpretation of the study results or in the preparation of the manuscript. The Division of Diabetes Translation provided funding support for the retinal component and was involved in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, and approval of this article before submission.
Footnotes
Author Contributions: Drs Zhang and Bullard had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest Disclosure: None reported.
Disclaimer: The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the National Institutes of Health or the CDC.
Online-Only Material: The eTable is available at jamaophth.com.
Additional Contributions: We thank the NHANES participants without whom this study would not be possible.
REFERENCES
- 1.Rubin GS, Bandeen-Roche K, Huang GH, et al. The association of multiple visual impairments with self-reported visual disability: SEE project. Invest Ophthalmol Vis Sci. 2001;42(1):64–72. [PubMed] [Google Scholar]
- 2.Rovner BW, Casten RJ, Tasman WS. Effect of depression on vision function in age-related macular degeneration. Arch Ophthalmol. 2002;120(8):1041–1044. doi: 10.1001/archopht.120.8.1041. [DOI] [PubMed] [Google Scholar]
- 3.Rees G, Tee HW, Marella M, Fenwick E, Dirani M, Lamoureux EL. Vision-specific distress and depressive symptoms in people with vision impairment. Invest Ophthalmol Vis Sci. 2010;51(6):2891–2896. doi: 10.1167/iovs.09-5080. [DOI] [PubMed] [Google Scholar]
- 4.Paz SH, Globe DR, Wu J, Azen SP, Varma R Los Angeles Latino Eye Study. Relationship between self-reported depression and self-reported visual function in Latinos. Arch Ophthalmol. 2003;121(7):1021–1027. doi: 10.1001/archopht.121.7.1021. [DOI] [PubMed] [Google Scholar]
- 5.Mojon-Azzi SM, Sousa-Poza A, Mojon DS. Impact of low vision on well-being in 10 European countries. Ophthalmologica. 2008;222(3):205–212. doi: 10.1159/000126085. [DOI] [PubMed] [Google Scholar]
- 6.Lamoureux EL, Fenwick E, Moore K, Klaic M, Borschmann K, Hill K. Impact of the severity of distance and near-vision impairment on depression and vision-specific quality of life in older people living in residential care. Invest Ophthalmol Vis Sci. 2009;50(9):4103–4109. doi: 10.1167/iovs.08-3294. [DOI] [PubMed] [Google Scholar]
- 7.Chou KL. Combined effect of vision and hearing impairment on depression in older adults: evidence from the English Longitudinal Study of Ageing. J Affect Disord. 2008;106(1–2):191–196. doi: 10.1016/j.jad.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 8.Capella-McDonnall ME. The effects of single and dual sensory loss on symptoms of depression in the elderly. Int J Geriatr Psychiatry. 2005;20(9):855–861. doi: 10.1002/gps.1368. [DOI] [PubMed] [Google Scholar]
- 9.Huang CQ, Dong BR, Lu ZC, Yue JR, Liu QX. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res Rev. 2010;9(2):131–141. doi: 10.1016/j.arr.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 10.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 11.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317(7160):703–713. [PMC free article] [PubMed] [Google Scholar]
- 12.Thase ME, Denko T. Pharmacotherapy of mood disorders. Annu Rev Clin Psychol. 2008;4:53–91. doi: 10.1146/annurev.clinpsy.2.022305.095301. [DOI] [PubMed] [Google Scholar]
- 13.DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62(4):409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- 14.Pignone MP, Gaynes BN, Rushton JL, et al. Screening for depression in adults: a summary of the evidence for the U.S Preventive Services Task Force. Ann Intern Med. 2002;136(10):765–776. doi: 10.7326/0003-4819-136-10-200205210-00013. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey. [Accessed November 19, 2008];Survey Questionnaires, Examination Components and Laboratory Components 2003–2004. CDC website. http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/questexam03_04.htm. [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) National Health and Nutrition Examination Survey. [Accessed February 22, 2010];NHANES Response Rates and CPS Population Totals. CDC website. http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm. [Google Scholar]
- 17.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD National Eye Institute Visual Function Questionnaire Field Test Investigators. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. [Accessed January 8, 2013];Psychiatr Ann. 2002 32(9):509–515. http://www.lphi.org/LPHIadmin/uploads/.PHQ-9-Review-Kroenke-63754.PDF. [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JB Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders: Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183(3):759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 23.Lamoureux EL, Tee HW, Pesudovs K, Pallant JF, Keeffe JE, Rees G. Can clinicians use the PHQ-9 to assess depression in people with vision loss? Optom Vis Sci. 2009;86(2):139–145. doi: 10.1097/OPX.0b013e318194eb47. [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association. Diagnosis and classification of diabetes mellitus [published correction appears in Diabetes Care. 2010;33(4):e57] Diabetes Care. 2010;33(suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Korn EL, Graubard BI. Analysis of Health Surveys. New York, NY: Wiley; 1999. [Google Scholar]
- 26.Ambler G, Omar RZ, Royston P. A comparison of imputation techniques for handling missing predictor values in a risk model with a binary outcome. Stat Methods Med Res. 2007;16(3):277–298. doi: 10.1177/0962280206074466. [DOI] [PubMed] [Google Scholar]
- 27.Sterne JA, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Charney DS, Reynolds CF, III, Lewis L, et al. Depression and Bipolar Support Alliance. Depression and Bipolar Support Alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch Gen Psychiatry. 2003;60(7):664–672. doi: 10.1001/archpsyc.60.7.664. [DOI] [PubMed] [Google Scholar]
- 29.Faye EE, Stuen CS, editors. The Aging Eye and Low Vision: A Study Guide for Physicians. New York, NY: The Lighthouse Inc; 1992. [Google Scholar]
- 30.Brody BL, Gamst AC, Williams RA, et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology. 2001;108(10):1893–1900. doi: 10.1016/s0161-6420(01)00754-0. discussion 1900–1901. [DOI] [PubMed] [Google Scholar]
- 31.Schrag A, Jahanshahi M, Quinn NP. What contributes to depression in Parkinson’s disease? Psychol Med. 2001;31(1):65–73. doi: 10.1017/s0033291799003141. [DOI] [PubMed] [Google Scholar]
- 32.Cubo E, Bernard B, Leurgans S, Raman R. Cognitive and motor function in patients with Parkinson’s disease with and without depression. Clin Neuropharmacol. 2000;23(6):331–334. doi: 10.1097/00002826-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Bramley T, Peeples P, Walt JG, Juhasz M, Hansen JE. Impact of vision loss on costs and outcomes in Medicare beneficiaries with glaucoma. Arch Ophthalmol. 2008;126(6):849–856. doi: 10.1001/archopht.126.6.849. [DOI] [PubMed] [Google Scholar]
- 34.Tournier M, Moride Y, Ducruet T, Moshyk A, Rochon S. Depression and mortality in the visually-impaired, community-dwelling, elderly population of Quebec. Acta Ophthalmol. 2008;86(2):196–201. doi: 10.1111/j.1600-0420.2007.01024.x. [DOI] [PubMed] [Google Scholar]
- 35.Iliffe S, Kharicha K, Harari D, Swift C, Gillmann G, Stuck A. Self-reported visual function in healthy older people in Britain: an exploratory study of associations with age, sex, depression, education and income. Fam Pract. 2005;22(6):585–590. doi: 10.1093/fampra/cmi067. [DOI] [PubMed] [Google Scholar]
- 36.McDonnall MC. The effects of developing a dual sensory loss on depression in older adults: a longitudinal study. J Aging Health. 2009;21(8):1179–1199. doi: 10.1177/0898264309350077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rovner BW, Zisselman PM, Shmuely-Dulitzki Y. Depression and disability in older people with impaired vision: a follow-up study. J Am Geriatr Soc. 1996;44(2):181–184. doi: 10.1111/j.1532-5415.1996.tb02436.x. [DOI] [PubMed] [Google Scholar]
- 38.Rovner BW, Casten RJ. Activity loss and depression in age-related macular degeneration. Am J Geriatr Psychiatry. 2002;10(3):305–310. [PubMed] [Google Scholar]
- 39.Tolman J, Hill RD, Kleinschmidt JJ, Gregg CH. Psychosocial adaptation to visual impairment and its relationship to depressive affect in older adults with age-related macular degeneration. Gerontologist. 2005;45(6):747–753. doi: 10.1093/geront/45.6.747. [DOI] [PubMed] [Google Scholar]
- 40.Casten RJ, Rovner BW, Tasman W. Age-related macular degeneration and depression: a review of recent research. Curr Opin Ophthalmol. 2004;15(3):181–183. doi: 10.1097/01.icu.0000120710.35941.3f. [DOI] [PubMed] [Google Scholar]
- 41.Skalicky S, Goldberg I. Depression and quality of life in patients with glaucoma: a cross-sectional analysis using the Geriatric Depression Scale-15, assessment of function related to vision, and the Glaucoma Quality of Life-15. J Glaucoma. 2008;17(7):546–551. doi: 10.1097/IJG.0b013e318163bdd1. [DOI] [PubMed] [Google Scholar]
- 42.Globe DR, Wu J, Azen SP, Varma R Los Angeles Latino Eye Study Group. The impact of visual impairment on self-reported visual functioning in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111(6):1141–1149. doi: 10.1016/j.ophtha.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 43.Beck CA, Joseph L, Bélisle P, Pilote L QOLAMI Investigators (Quality of life in acute myocardial infarction) Predictors of quality of life 6 months and 1 year after acute myocardial infarction. Am Heart J. 2001;142(2):271–279. doi: 10.1067/mhj.2001.116758. [DOI] [PubMed] [Google Scholar]
- 44.Gold DT, Burchett BM, Shipp KM, Pieper CF, Lyles KW. Factors associated with self-rated health in patients with Paget’s disease of bone. J Bone Miner Res. 1999;14(suppl 2):99–102. doi: 10.1002/jbmr.5650140221. [DOI] [PubMed] [Google Scholar]
- 45.Nash IS, Curtis LH, Rubin H. Predictors of patient-reported physical and mental health 6 months after percutaneous coronary revascularization. Am Heart J. 1999;138(3, pt 1):422–429. doi: 10.1016/s0002-8703(99)70142-0. [DOI] [PubMed] [Google Scholar]
- 46.Desrosiers J, Wanet-Defalque MC, Témisjian K, et al. Participation in daily activities and social roles of older adults with visual impairment. Disabil Rehabil. 2009;31(15):1227–1234. doi: 10.1080/09638280802532456. [DOI] [PubMed] [Google Scholar]
- 47.Ishii K, Kabata T, Oshika T. The impact of cataract surgery on cognitive impairment and depressive mental status in elderly patients. Am J Ophthalmol. 2008;146(3):404–409. doi: 10.1016/j.ajo.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 48.Owsley C, McGwin G, Jr, Scilley K, Meek GC, Seker D, Dyer A. Effect of refractive error correction on health-related quality of life and depression in older nursing home residents. Arch Ophthalmol. 2007;125(11):1471–1477. doi: 10.1001/archopht.125.11.1471. [DOI] [PubMed] [Google Scholar]
- 49.Rubin GS, Roche KB, Prasada-Rao P, Fried LP. Visual impairment and disability in older adults. Optom Vis Sci. 1994;71(12):750–760. doi: 10.1097/00006324-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 50.Ivers RQ, Cumming RG, Mitchell P, Attebo K. Visual impairment and falls in older adults: the Blue Mountains Eye Study. J Am Geriatr Soc. 1998;46(1):58–64. doi: 10.1111/j.1532-5415.1998.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 51.Crews JE, Jones GC, Kim JH. Double jeopardy: The effects of comorbid conditions among older people with vision loss. [Accessed January 9, 2013];J Vis Impair Blind. 2006 100:824–848. http://www.afb.org/jvib/jvib001307.asp. [Google Scholar]
- 52.Lotery A, Xu X, Zlatava G, Loftus J. Burden of illness, visual impairment and health resource utilisation of patients with neovascular age-related macular degeneration: results from the UK cohort of a five-country cross-sectional study. Br J Ophthalmol. 2007;91(10):1303–1307. doi: 10.1136/bjo.2007.116939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brody BL, Roch-Levecq AC, Kaplan RM, Moutier CY, Brown SI. Age-related macular degeneration: self-management and reduction of depressive symptoms in a randomized, controlled study. J Am Geriatr Soc. 2006;54(10):1557–1562. doi: 10.1111/j.1532-5415.2006.00881.x. [DOI] [PubMed] [Google Scholar]
- 54.Hassell JB, Lamoureux EL, Keeffe JE. Impact of age related macular degeneration on quality of life. Br J Ophthalmol. 2006;90(5):593–596. doi: 10.1136/bjo.2005.086595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mitchell J, Bradley C. Quality of life in age-related macular degeneration: a review of the literature. Health Qual Life Outcomes. 2006;4:97. doi: 10.1186/1477-7525-4-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pauleikhoff D, Scheider A, Wiedmann P, et al. Neovascular age-related macular degeneration in Germany: encroachment on the quality of life and the financial implications [in German] Ophthalmologe. 2009;106(3):242–251. doi: 10.1007/s00347-008-1797-9. [DOI] [PubMed] [Google Scholar]
- 57.Rovner BW, Casten RJ. Preventing late-life depression in age-related macular degeneration. Am J Geriatr Psychiatry. 2008;16(6):454–459. doi: 10.1097/JGP.0b013e31816b7342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rovner BW, Casten RJ, Hegel MT, Hauck WW, Tasman WS. Dissatisfaction with performance of valued activities predicts depression in age-related macular degeneration. Int J Geriatr Psychiatry. 2007;22(8):789–793. doi: 10.1002/gps.1742. [DOI] [PubMed] [Google Scholar]
- 59.Wysong A, Lee PP, Sloan FA. Longitudinal incidence of adverse outcomes of age-related macular degeneration. Arch Ophthalmol. 2009;127(3):320–327. doi: 10.1001/archophthalmol.2008.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hidalgo JL, Martínez IP, Bravo BN, Pretel FA, Ferrer AV, Verdejo MA. Visual function versus visual acuity in older people. Ophthalmic Epidemiol. 2009;16(4):262–268. doi: 10.3109/09286580902999397. [DOI] [PubMed] [Google Scholar]
- 61.Bookwala J, Lawson B. Poor vision, functioning, and depressive symptoms: a test of the activity restriction model. Gerontologist. 2011;51(6):798–808. doi: 10.1093/geront/gnr051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am J Public Health. 1999;89(9):1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shmuely-Dulitzki Y, Rovner BW, Zisselman P. The impact of depression on functioning in elderly patients with low vision. Am J Geriatr Psychiatry. 1995;3(4):325–329. doi: 10.1097/00019442-199503040-00007. [DOI] [PubMed] [Google Scholar]
- 64.Jones GC, Crews JE, Danielson ML. Health risk profile for older adults with blindness: an application of the International Classification of Functioning, Disability, and Health framework. Ophthalmic Epidemiol. 2010;17(6):400–410. doi: 10.3109/09286586.2010.528137. [DOI] [PubMed] [Google Scholar]
- 65.Spencer C, Frick K, Gower EW, Kempen JH, Wolff JL. Disparities in access to medical care for individuals with vision impairment. Ophthalmic Epidemiol. 2009;16(5):281–288. [PubMed] [Google Scholar]
- 66.Jones GC, Rovner BW, Crews JE, Danielson ML. Effects of depressive symptoms on health behavior practices among older adults with vision loss. Rehabil Psychol. 2009;54(2):164–172. doi: 10.1037/a0015910. [DOI] [PubMed] [Google Scholar]
- 67.McDonnall MC. Risk factors for depression among older adults with dual sensory loss. Aging Ment Health. 2009;13(4):569–576. doi: 10.1080/13607860902774410. [DOI] [PubMed] [Google Scholar]
- 68.Horowitz A, Reinhardt JP, Boerner K. The effect of rehabilitation on depression among visually disabled older adults. Aging Ment Health. 2005;9(6):563–570. doi: 10.1080/13607860500193500. [DOI] [PubMed] [Google Scholar]
- 69.Brody BL, Roch-Levecq AC, Gamst AC, Maclean K, Kaplan RM, Brown SI. Self-management of age-related macular degeneration and quality of life: a randomized controlled trial. Arch Ophthalmol. 2002;120(11):1477–1483. doi: 10.1001/archopht.120.11.1477. [DOI] [PubMed] [Google Scholar]
- 70.Rovner BW, Casten RJ, Hegel MT, Leiby BE, Tasman WS. Preventing depression in age-related macular degeneration. Arch Gen Psychiatry. 2007;64(8):886–892. doi: 10.1001/archpsyc.64.8.886. [DOI] [PubMed] [Google Scholar]
- 71.Rees G, Fenwick EK, Keeffe JE, Mellor D, Lamoureux EL. Detection of depression in patients with low vision. Optom Vis Sci. 2009;86(12):1328–1336. doi: 10.1097/OPX.0b013e3181c07a55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.