Abstract
Background
Little is known about what primary care physicians (PCPs) and patients would expect if patients were invited to read their doctors' office notes.
Objective
To explore attitudes toward potential benefits or harms if PCPs offered patients ready access to visit notes.
Design
The PCPs and patients completed surveys before joining a voluntary program that provided electronic links to doctors' notes.
Setting
Primary care practices in 3 U.S. states.
Participants
Participating and nonparticipating PCPs and adult patients at primary care practices in Massachusetts, Pennsylvania, and Washington.
Measurements
Doctors' and patients' attitudes toward and expectations of open visit notes, their ideas about the potential benefits and risks, and demographic characteristics.
Results
110 of 114 participating PCPs (96%), 63 of 140 nonparticipating PCPs (45%), and 37 856 of 90 826 patients (42%) completed surveys. Overall, 69% to 81% of participating PCPs across the 3 sites and 92% to 97% of patients thought open visit notes were a good idea, compared with 16% to 33% of nonparticipating PCPs. Similarly, participating PCPs and patients generally agreed with statements about potential benefits of open visit notes, whereas nonparticipating PCPs were less likely to agree. Among participating PCPs, 74% to 92% anticipated improved communication and patient education, in contrast to 45% to 67% of nonparticipating PCPs. More than one half of participating PCPs (50% to 58%) and most nonparticipating PCPs (88% to 92%) expected that open visit notes would result in greater worry among patients; far fewer patients concurred (12% to 16%). Thirty-six percent to 50% of participating PCPs and 83% to 84% of nonparticipating PCPs anticipated more patient questions between visits. Few PCPs (0% to 33%) anticipated increased risk for lawsuits. Patient enthusiasm extended across age, education, and health status, and 22% anticipated sharing visit notes with others, including other doctors.
Limitations
Access to electronic patient portals is not widespread, and participation was limited to patients using such portals. Response rates were higher among participating PCPs than nonparticipating PCPs; many participating PCPs had small patient panels.
Conclusion
Among PCPs, opinions about open visit notes varied widely in terms of predicting the effect on their practices and benefits for patients. In contrast, patients expressed considerable enthusiasm and few fears, anticipating both improved understanding and more involvement in care. Sharing visit notes has broad implications for quality of care, privacy, and shared accountability.
Information technologies offer new ways to engage patients in their health. Providers who have adopted electronic medical records are beginning to use secure Internet portals to offer patients online access to test results, medication lists, and other parts of those records (1–4). However, few portals offer access to notes generated in outpatient encounters, even though exploratory studies focusing on chronic illnesses suggest that such access may help patients and have little net effect on provider workflow (5– 8).
To gain further insight into such a shift in care, we designed and initiated OpenNotes, a research and demonstration project involving primary care physicians (PCPs) and their adult patients in urban and suburban Boston, rural Pennsylvania, and inner-city Seattle (9). We asked PCPs whether they would volunteer for 1 year, starting in summer 2010, to send their patients electronic invitations to read their outpatient visit notes online and to review these notes before the next scheduled encounter. We expected that PCPs would be wary of such a change in care, particularly those who had been in practice for many years and those who spend many hours in direct patient care. We hypothesized that patients would be generally positive about open visit notes, that highly educated and younger patients would be particularly enthusiastic, and that many would want to share their notes with others.
We surveyed eligible doctors and patients before the start of the voluntary program and report here on their attitudes and expectations toward electronic access to doctors' notes. Survey respondents included PCPs who volunteered to participate in OpenNotes, PCPs who declined to participate, and patients cared for by both groups of PCPs who were using the practices' online portals to access other information about their care (for example, test results).
METHODS
In summer 2010, patients were offered online access to ambulatory encounter notes written by the PCPs who volunteered to participate in OpenNotes. Before the doctors' notes were made available, we conducted online surveys of patients and PCPs from the 3 study sites: 1) practices offering primary care at Beth Israel Deaconess Medical Center (BIDMC), an urban academic health center in Boston, Massachusetts, and at associated community practices in and around Boston; 2) primary care sites at Geisinger Health System (GHS), a primarily rural integrated health system with 3 medical centers and 39 community practices in Pennsylvania; and 3) the adult medicine and HIV clinics at Harborview Medical Center (HMC), a county hospital in Seattle, Washington, that largely serves indigent patients. Beth Israel Deaconess Medical Center and GHS have well-established online patient portals (PatientSite and MyGeisinger, respectively), with approximately 50 000 and 163 000 registered patient-users. Before the start of the OpenNotes project, patients used these portals to access test results, medication lists, appointment schedules, prescriptions, referrals, secure electronic messaging with providers, and other information. Coincident with the start of our project, HMC deployed an online portal, UW Medicine e-care; previously, patients had not had online access to information about their care. Thus, patients at HMC who were enrolled in the intervention gained access to test results and PCP visit notes for the first time at the start of our study.
Participating PCPs were given the option of excluding patients who, in their clinical judgment, might be put at risk by reading their notes, and those who were excluded were not asked to complete surveys. At BIDMC, participating PCPs excluded 158 of 11 898 portal patients; at GHS, they excluded 139 of 10 825 portal patients. Because HMC cares for many patients with severe mental health and substance abuse issues, PCPs at that institution were reluctant to include many such patients in this initial test of the program; they excluded 1023 of 3186 eligible patients. Of the remaining eligible patients, 277 were registered for the HMC portal.
Questionnaire Design
To design surveys to assess the potential effects of open visit notes, we examined the literature on patient and doctor attitudes toward accessing medical records (8, 10, 11). For the PCP survey, we conducted 1 focus group at BIDMC and 1 at GHS, with a total of 14 PCPs. We recorded the sessions, and 3 of the study investigators reviewed transcripts and reached consensus on common themes. We transformed themes into survey questions addressing potential benefits, risks, and expectations about the impact of open visit notes on their practice (documentation, interactions with patients, liability, and effects on patient care). We added items about doctor and practice characteristics. We tested the survey in several iterations and revised it according to feedback. Using paper questionnaires, we solicited comments to ascertain face validity from 3 clinician-researchers at BIDMC. Finally, we pretested the online survey with 5 PCPs to assess content and potential technical issues.
We used parallel methods for the patient survey, beginning with 5 patient focus groups involving 41 patients at BIDMC and HMC. Investigators reached consensus about common themes and developed questions after 1 BIDMC focus group, and they then evaluated content and clarity by using paper questionnaires in 4 patient focus groups at HMC after the guided discussion. Subsequently, we obtained feedback for face validity, comprehension, flow, and completeness from 3 participants in BIDMC focus groups who volunteered to complete them online. Finally, we pretested the online survey with a pilot group of 829 participants at BIDMC and GHS to test technical processes and completeness. Their participation did not result in changes in the survey, and their responses are included in the results we document, except for those from 69 patients who were cared for by one of the study investigators.
To compare agreement between patients and PCPs, we used the same wording for both the PCP and patient surveys to address potential benefits and risks (response options were “disagree;” “somewhat disagree;” “somewhat agree;” “agree;” and, for patients only, “don't know”). In addition, we solicited patients' thoughts about privacy, sharing notes with others, and the effect on their doctors' work lives. We added validated questions addressing patient–doctor communication: the Perceived Efficacy of Patient–Doctor Interactions questionnaire measured self-confidence about communicating with doctors, and items from the Ambulatory Care Experiences Survey measured the quality of doctor–patient interactions (12, 13).
We also assessed patient sociodemographic characteristics, including race, education, employment, and overall health status; patient age and sex were obtained from administrative data. We asked all patients the same questions, but the introductory language differed slightly for patients of participating versus nonparticipating PCPs.
Surveys were conducted online by using SurveyGizmo, versions 2.0 and 3.0 (Widgix, Boulder, Colorado). Except for questions about demographic characteristics, free-text questions, and skip patterns, all items required a response. Respondents could not skip individual questions but could exit the survey at any point. Responses up to the point of exit were used in the data analysis. Surveys were designed to take less than 20 minutes to complete and are available upon request.
Conducting the Surveys
At BIDMC and GHS, we sent survey invitations electronically to all participating and nonparticipating PCPs and to their patients who were registered on the practice portals (approximately 36% of the PCP panels at BIDMC and 25% at GHS). We surveyed doctors first, then their patients. We sent up to 3 reminders to PCPs via their institutional e-mail addresses and to patients via the portals' secure messaging service. We asked participating PCPs to complete the survey at the time of enrollment in the study. Their patients were surveyed before notes were opened, and patients of participating PCPs could view their notes regardless of whether they responded to the survey. We gave invitees 4 to 6 weeks to complete the survey. All PCPs and most patients who responded completed the surveys before notes were made available to patients.
Because of scheduling constraints at GHS, the survey was online for a 12-day overlap when visit notes were initially made available. We estimate that less than 1% of GHS patients who responded to the survey may have viewed a visit note before completing the survey.
At HMC, which had no preexisting portal, we contacted PCPs via their institutional e-mail addresses. Because some patients at HMC did not own computers, we enrolled PCPs and HMC patients on a rolling basis over 4 months; inviting patients in the clinic, by mail, or by telephone to join the study; and then enrolling them in person. We required each HMC patient to complete a survey in order to join the study.
We offered survey incentives in line with site policies: BIDMC patients who completed surveys entered a raffle for $25 gift certificates, and each PCP who completed a survey received $50. Doctors at GHS who answered surveys received $30 gift cards, and HMC patients received $10 gift cards.
Statistical Analysis
In our descriptive analysis, we used means and SDs for continuous variables and percentages for categorical variables. Because sample size and patient characteristics differed greatly across the sites and there were potential un-measured confounders in the aggregated data, we did not use multivariable modeling to assess the independent effects of interest, such as sex, age, education, health status, and confidence in communication. We limit our inferences to our study sample alone and report only descriptive statistics summarizing our findings.
For statements evaluating attitudes, we first examined results across a 5-level agree–disagree response set. After determining empirically that the data were suitable for doing so, we combined the “agree” and “somewhat agree” categories and the “disagree” and “somewhat disagree” categories; “don't know” responses were retained as a separate category. Using data from each of the 3 sites, stratified according to whether the PCP was or was not a participant, we calculated sample proportions of PCPs who agreed with statements about perceived benefits, risks, and effect on their work. Similarly, we calculated the proportions of patients who agreed with statements about potential benefits, risks, and effect on the work lives of their PCPs by study sites, PCP participation, and patient characteristics. Patient responses of “don't know” were treated as nonmissing and were included in denominators. We performed all statistical analyses by using SAS software, version 9.2 (SAS Institute, Cary, North Carolina).
Beth Israel Deaconess Medical Center acted as the coordinating center for the project; its institutional review board approved the overall project. The institutional review boards at GHS and the University of Washington approved the implementation in their specific sites.
Role of the Funding Source
The study was funded by The Robert Wood Johnson Foundation's Pioneer Portfolio, the Drane Family Fund, and the Koplow Charitable Foundation. The funding sources had no role in designing or conducting the study; analyzing the data; preparing the manuscript; or deciding to submit the manuscript for publication.
Results
Of the 173 PCPs who responded to the survey, 64% volunteered to participate in OpenNotes (Table 1). Nearly all participating PCPs (96%) and 45% of those who declined to participate completed surveys. The PCP respondents were fairly distributed across the 3 sites (31% from BIDMC, 45% from GHS, and 24% from HMC); in contrast, 80% of patient respondents were from GHS, 19% from BIDMC, and less than 1% from HMC. All PCP surveys were complete, except for one with incomplete responses about doctor and practice characteristics. Among patients, the proportion of missing responses to most items was very low (0.01% to 2.65% across the 3 sites). For optional questions about demographic characteristics at the end of the patient survey, a few more responses were missing (2.68% to 4.55% across sites).
Table 1.
Survey Response Rates Among PCPs and Their Patients, According to Participation in OpenNotes
| Study Site | All PCPs, n | PCPs Who Submitted a Survey, n (%) | All Portal Patients, n | Patients Who Submitted a Survey, n (%) |
|---|---|---|---|---|
| BIDMC | ||||
| Participant | 42 | 42 (100) | 11 740 | 4545 (39) |
| Nonparticipant | 22 | 12 (55) | 6631 | 2633 (40) |
| GHS | ||||
| Participant | 27 | 26 (96) | 10 686 | 4226 (40) |
| Nonparticipant | 118 | 51 (43) | 61 492 | 26 180 (43) |
| HMC | ||||
| Participant | 45 | 42 (93) | – † | 272 |
| Nonparticipant* | – | – | – | – |
| Total | ||||
| Participant | 114 | 110 (96) | 22 703 | 9043 (40) |
| Nonparticipant | 140 | 63 (45) | 68 123 | 28 813 (42) |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
We did not survey nonparticipating PCPs or patients at HMC.
Of 2163 eligible patients at HMC who were not excluded by their PCP owing to concerns about risk resulting from reading their notes, 277 registered for the HMC portal (which was open only to study participants).
We observed demographic and practice differences among doctors according to study site and participation status (Table 2). In general, respondents at HMC were younger and worked fewer hours in direct care, whereas respondents at GHS who were not participating in OpenNotes worked the most hours in patient care. More than three quarters of GHS doctors and more than one half of BIDMC doctors communicated electronically with patients at least daily. At HMC, where access to electronic records was new for patients, e-mail communication with PCPs was infrequent.
Table 2.
Characteristics of PCPs Who Responded to the Survey, by Study Site
| Characteristic | BIDMC |
GHS |
HMC† |
||
|---|---|---|---|---|---|
| Participating PCPs (n = 42), % | Nonparticipating PCPs (n = 12), % | Participating PCPs (n = 26*), % | Nonparticipating PCPs (n = 51), % | Participating PCPs (n = 42), % | |
| Age | |||||
| 30–39 y | 26 | 0 | 23 | 26 | 45 |
| 40–49 y | 38 | 50 | 27 | 34 | 38 |
| 50–59 y | 26 | 42 | 46 | 32 | 17 |
| ≥60 y | 10 | 8 | 4 | 8 | 0 |
| Women | 50 | 42 | 23 | 42 | 62 |
| Direct care hours per week | |||||
| <115 | 43 | 42 | 8 | 2 | 73 |
| 15–35 | 45 | 42 | 46 | 26 | 19 |
| 36–62 | 12 | 17 | 46 | 72 | 7 |
| How often PCPs communicate with patients by e-mail | |||||
| Never | 4 | 0 | 0 | 4 | 17 |
| Less than once weekly | 7 | 8 | 4 | 10 | 60 |
| More than once weekly, but not daily | 36 | 25 | 15 | 10 | 19 |
| More than once daily | 52 | 67 | 81 | 76 | 5 |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Data were missing for 1 PCP survey respondent.
Only participating PCPs completed the survey at HMC.
Overall, patient respondents were more likely than nonrespondents to be women (63% vs. 59%, respectively) and were on average 5 years older (52 years vs. 47 years). Characteristics of patient respondents differed across the sites (Table 3). Compared with other sites, HMC patients were more likely to be nonwhite, male, unemployed, and in fair or poor health (72% of HMC study patients attend the HIV/AIDS clinic). In contrast, BIDMC patients were more highly educated and reported better self-rated health than those at other sites, and GHS patients were more often female, less educated, and white.
Table 3.
Characteristics of Patients Who Responded to the Survey, by Study Site
| Characteristic | BIDMC (n = 7178) | GHS (n = 30 406) | HMC (n = 272) |
|---|---|---|---|
| Age, y | |||
| Mean (SD) | 53 (13) | 52 (14) | 49 (11) |
| Median | 54 | 53 | 49 |
| Women, % | 60 | 64 | 24 |
| Race, % | |||
| White | 87 | 96 | 63 |
| Black or African American | 3 | 1 | 19 |
| Other or multiracial | 10 | 3 | 18 |
| Education, % | |||
| High school/GED or less | 5 | 33 | 27 |
| Some college | 17 | 32 | 41 |
| College graduate | 24 | 16 | 14 |
| Postcollege | 54 | 20 | 17 |
| Employed, % | 74 | 63 | 39 |
| Self-rated fair or poor health status, % | 10 | 17 | 27 |
| Ambulatory Care Experiences Survey score * | |||
| Mean (SD) | 5 (1) | 5 (1) | 5 (1) |
| Median | 5.4 | 5.4 | 5.6 |
| Perceived Efficacy of Patient–Doctor Interactions score † | |||
| Mean (SD) | 41 (7) | 40 (8) | 43 (7) |
| Median | 42 | 42 | 46 |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center.
Patient report of patient–doctor communication; range of 1 to 6, with a higher score indicating better communication.
Patient level of confidence about communicating with his or her physician; range of 5 to 50, with a higher score indicating more confidence.
Responding patients of participating PCPs were slightly more likely than those of nonparticipating PCPs to be men (GHS, 39% and 36%, respectively; BIDMC, 41% and 39%). At BIDMC, 86% of responding patients of participating PCPs were white, compared with 90% of patients of nonparticipating PCPs. We did not observe meaningful differences in other patient characteristics at BIDMC or GHS according to the participation status of their PCPs (data not shown). At HMC, 76% of participating patients were men, compared with 65% of eligible patients who did not participate in either OpenNotes or the survey.
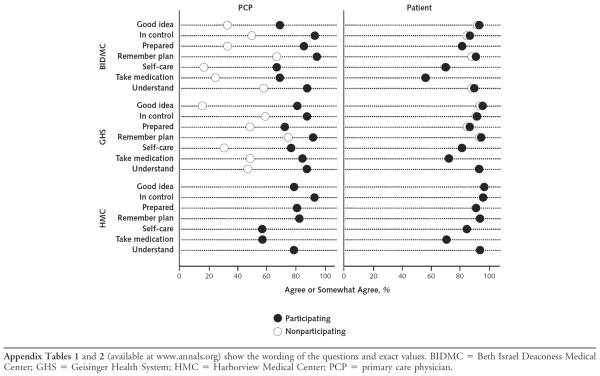
The PCP respondents who declined participation in the project were much more pessimistic about open visit notes in general than were participating PCPs (Figure 1 and Appendix Table 1, available at www.annals.org). Regardless of their PCPs' participation status, responding patients were highly positive about open visit notes. For example, only 16% of nonparticipating PCPs at GHS thought open visit notes were a good idea, compared with 81% of participating PCPs and more than 90% of patients (Figure 1). At BIDMC, 33% of nonparticipating PCPs agreed that open visit notes were a good idea, compared with 69% of participating PCPs and more than 90% of patients. Most participating PCPs at BIDMC and GHS agreed with statements about potential patient benefits; nonparticipating PCPs were far less likely to agree. At HMC, where all survey respondents were participating in OpenNotes, PCPs and patients were positive about these potential benefits (57% to 93% and 71% to 97%, respectively, agreed or somewhat agreed with each of the benefit statements). In contrast, 43% to 92% of PCPs across the study sites were far more likely to agree with statements about potential risks for worrying or confusing patients than were the patients themselves (7% to 16%) (Figure 2).
Figure 1.
Proportion of PCPs and patients who agreed or somewhat agreed with statements about the potential benefits of open visit notes for patients, by study site.
Figure 2.
Proportion of PCPs and patients who agreed or somewhat agreed with statements about the potential harms of open visit notes to patients, by study site.
Table 4 shows PCP expectations about the effect of open visit notes on their practices. Across the study sites, 71% to 77% of participating PCPs thought that patient satisfaction would improve, compared with 29% to 58% of nonparticipating PCPs. In addition, 36% to 62% of participating PCPs and 18% to 33% of nonparticipating PCPs thought that patient care would be safer. Somewhat less than one half of participating PCPs and more than 80% of nonparticipating PCPs anticipated spending more time addressing patient questions outside of visits; 27% to 40% of participating PCPs and 61% to 75% of nonparticipating PCPs believed that they would be less candid in documentation, whereas 33% to 50% of participating PCPs and 58% to 65% of nonparticipating PCPs predicted spending more time writing or editing their notes. Many nonparticipating PCPs believed that they would change the way they wrote about mental health (67% to 69%) and substance abuse (59% to 75%), compared with 27% to 55% and 31% to 43%, respectively, of participating PCPs.
Table 4.
PCP Survey Respondents' Expectations of the Impact of Open Visit Notes on Their Practice
| Expectation | BIDMC |
GHS |
HMC* |
||
|---|---|---|---|---|---|
| Participating PCPs (n = 42), % | Nonparticipating PCPs (n = 12), % | Participating PCPs (n = 26), % | Nonparticipating PCPs (n = 51), % | Participating PCPs (n = 42), % | |
| Visits will take significantly longer† | 26 | 58 | 27 | 71 | 24 |
| Will spend more time addressing patient questions outside of visits† | 50 | 83 | 46 | 84 | 36 |
| Patients who read their notes will be offended† | 33 | 58 | 8 | 45 | 29 |
| Will be less candid in documentation† | 36 | 75 | 27 | 61 | 40 |
| Will order more tests and/or referrals† | 0 | 8 | 4 | 20 | 2 |
| Will spend more time writing/dictating/editing my notes† | 50 | 58 | 35 | 65 | 33 |
| I will change the way I address these topics in my notes (yes response) | |||||
| Cancer/possibility of cancer | 36 | 58 | 15 | 49 | 29 |
| Mental health | 45 | 67 | 27 | 69 | 55 |
| Substance abuse | 43 | 75 | 31 | 59 | 43 |
| Overweight/obesity | 19 | 58 | 15 | 47 | 21 |
| Process measures of quality will improve (yes response) | 31 | 8 | 46 | 27 | 26 |
| Outcome measures of quality will improve (yes response) | 24 | 8 | 50 | 24 | 26 |
| Medical care will be delivered more efficiently (yes response) | 24 | 0 | 27 | 14 | 33 |
| Patient satisfaction will improve (yes response) | 71 | 58 | 77 | 29 | 76 |
| Patient care will be safer (yes response) | 62 | 33 | 58 | 18 | 36 |
| Risk for lawsuits will decrease | 7 | 0 | 12 | 4 | 10 |
| Risk for lawsuits will not change | 93 | 92 | 77 | 63 | 79 |
| Risk for lawsuits will increase | 0 | 8 | 12 | 33 | 12 |
| Notes can be useful for patient communication and education (agree or somewhat agree) | 74 | 67 | 92 | 45 | 79 |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Only participating PCPs completed surveys at HMC.
Percentage of PCPs responding that they were moderately or very concerned, or so concerned that they do not want open notes.
Older patients and those with less education were at least as likely as those who were younger and better educated to agree with statements about potential benefits (Appendix Table 2, available at www.annals.org). Overall, there were few differences among patients who responded to the survey in terms of demographic characteristics and self-reported health status.
Thirty-five percent of patients were concerned about their privacy, 22% anticipated sharing their notes with others, and 29% were undecided. Of those who foresaw sharing their notes, 93% anticipated doing so with a family member or relative, 36% with another doctor, 23% with a friend, and 23% with a nurse or other health professional. The findings regarding sharing notes derive from incomplete data; a random software error resulted in 13 007 GHS responses with missing information. However, we compared the characteristics of the GHS patients for whom data were missing with those of the 17 399 GHS patients for whom data were complete and found no material differences between the 2 groups.
Discussion
Although we observed striking differences between doctor and patient attitudes toward sharing visit notes, the doctors who participated in our project were more optimistic about the tangible benefits for patients than we postulated. They predicted improvements in both patient safety and satisfaction and believed that patients would be better prepared for visits, would feel more in control of their health care, and would take better care of themselves. However, many participating PCPs and most who declined participation anticipated lengthier visits and increased demands on their time between visits. Moreover, many doctors declining participation worried about frightening and confusing patients; recording their thoughts candidly; and writing about such issues as mental health, substance abuse, cancer, and obesity. Overall, PCPs who declined to participate predicted that open visit notes would lead to negative consequences for the way they practiced and would have little positive effect on their patients.
The enthusiasm of patients exceeded our expectations; most of them were overwhelmingly positive about the prospect of reading visit notes, regardless of demographic or health characteristics. In sharp contrast to the expectations of their PCPs, fewer than 1 in 6 patients was concerned about being worried or confused by reading their notes. Moreover, contrary to our hypotheses, we did not find that younger or more highly educated patients who responded to our survey were more likely to agree with the benefits than those who were older or had less education. It was also striking that many patients would consider sharing their notes with other people, including other doctors.
Our data suggest that almost all patients, including those who report poor health, anticipate that open visit notes may help them, a finding concordant with prior research using patient Web sites for collaborative long-term care (5–7, 14, 15). Whereas studies assessing Web site adoption suggest that patients with low to modest education have been less likely to use online services, patients with modest education in our study were just as likely as others to envision benefiting from open visit notes (16–18). Perhaps all patients would benefit from such an opportunity to review and understand information from the visit, using notes as an opportunity to grasp more thoroughly what the doctor recommends.
The finding that one half of the patients contemplated sharing their visit notes with others, including other doctors, could have many consequences. Confidentiality may be the hallmark of traditional doctor–patient interaction, but open visit notes put the patient in control of whether the note will remain private. Will sharing notes help patients engage families, friends, and caregivers more fully and effectively? If patients send notes to other health professionals, will that foster improved communication or act as a mechanism for seeking second or third opinions? How might that affect patients' trust in their PCP? The implications extend further: One third of the patients in our study worried about the effect of open visit notes on privacy. How would such fear interact with desire to share doctors' notes with others? As debate about “open disclosure” continues, how might transparent notes affect our litigious society? What information will land on social media sites (such as Facebook), and who will forward it to whom (19)?
The doctors in our survey, particularly those who declined to participate in OpenNotes, were far more worried about the downsides for patients than were the patients themselves. Are patients overly optimistic about how helpful the notes will be? Or do doctors underestimate their resourcefulness and resilience when they encounter arcane or worrisome language? OpenNotes has gone live since we collected these baseline data, and unanticipated consequences are emerging, with doctors and patients differing at times in assigning benefit or harm to specific byproducts of transparency. For example, as they learn what sort of information doctors write down, patients report withholding information that they would rather not have recorded. Patients may spot mistakes and help doctors avoid potential errors, but they may also question a doctor's competence or the veracity of what is documented. As language, shape, or content of notes shift, who will declare such change a benefit or liability?
Our study has limitations. First, all of the study sites have electronic medical records and patient portals, circumstances that differ from the average primary care practice and patient experience. Second, although the number of patient surveys is large, they were drawn from practices in only 3 regions and include only patients who had registered to use portals. Third, most of the survey questions were designed specifically for our project, and although these questions have face validity and were developed by drawing on literature, focus groups, individual interviews, and the experience of our study investigators, we did not perform psychometric testing to evaluate reliability or further validity. Fourth, because survey response rates were far lower among PCPs who declined to participate in OpenNotes than those who participated, our results may mis-represent the views of nonparticipating doctors. Fifth, many of the doctor respondents practice in academic settings and manage smaller patient panels than most practitioners. Sixth, patients who dislike or are indifferent to the concept of open visit notes may have been less likely to respond to the survey. Seventh, a larger proportion of patients at HMC were not surveyed owing to doctors' concerns about potential harm from reviewing their notes. Finally, expectations may differ from actual experience: We anticipate that reports from doctors and patients at the close of the 1-year study period will differ from their predictions.
Table 4 vividly demonstrates that doctors seemed remarkably divided in many of their expectations and the issues we highlight have important consequences for both their work life and quality of care. All U.S. patients have the right to review their visit notes if they so desire, and the spread of electronic records will inevitably ensure easier access. Whether open visit notes bring doctors and patients closer together, tend to drive them apart, or have little effect on the patient–doctor relationship remains to be seen. One might think of open visit notes as analogous to a new medicine: Its goal is to improve the process and outcome of care for those who use it, but as with every therapy, some may be harmed by it and some may choose not to use it.
The costs of instituting electronic medical records with patient portals are high. Nevertheless, electronic medical records, online portals that offer patients information about their care, and open visit notes will almost certainly proliferate, and as these features become more established, their price will decrease. Finally, as with new drug therapies, the “dose” and “formulation” of open notes will need to be determined over time. It will take considerable further analysis and experimentation to understand many of their implications and consequences.
From Beth Israel Deaconess Medical Center, Harvard Medical School, and College of Nursing and Health Sciences, University of Massachusetts, Boston, Massachusetts; Geisinger Health System, Danville, Pennsylvania; Harborview Medical Center, University of Washington School of Medicine, and Group Health Research Institute, Group Health Cooperative, Seattle, Washington; and University of Colorado Health Sciences Center, Aurora, Colorado.
Context
Electronic portals are beginning to provide patients with access to portions of their health records.
Contribution
In this survey, most physicians who planned to participate in a pilot program that provided patients with electronic access to their office notes anticipated benefits to their patients. Physicians who chose not to participate in the pilot program more often worried about potential harms to patients. Patients of both participating and nonparticipating physicians expected overall benefits more frequently than harms.
Caution
The survey was conducted among a selected group of physicians and patients at 3 institutions and does not reflect real-world experience.
Implication
Further study is needed to assess the benefits and harms of patients' access to their physicians' office notes.
—The Editors
Acknowledgments
Primary Funding Source: The Robert Wood Johnson Foundation's Pioneer Portfolio, Drane Family Fund, and Koplow Charitable Foundation.
Grant Support: By The Robert Wood Johnson Foundation's Pioneer Portfolio (grant 65921 to Ms. Walker and Dr. Delbanco), the Drane Family Fund, and the Koplow Charitable Foundation.
Appendix Table 1.
Proportion of PCPs Who Agreed or Somewhat Agreed With Statements About the Potential Benefits and Risks of Open Visit Notes, by Participation Status
| Statement | BIDMC |
GHS |
HMC* |
||
|---|---|---|---|---|---|
| Participating PCPs (n = 42), % | Nonparticipating PCPs (n = 12), % | Participating PCPs (n = 26), % | Nonparticipating PCPs (n = 51), % | Participating PCPs (n = 42), % | |
| Making notes available is a good idea | 69 | 33 | 81 | 16 | 79 |
| Among my patients who read their visit notes, a majority will: | |||||
| Feel more in control of their health care | 93 | 50 | 88 | 59 | 93 |
| Be better prepared for visits | 86 | 33 | 73 | 49 | 81 |
| Better remember the plan for their care | 95 | 67 | 92 | 75 | 83 |
| Take better care of themselves | 67 | 17 | 77 | 31 | 57 |
| Be more likely to take medications as prescribed | 69 | 25 | 85 | 49 | 57 |
| Better understand their health and medical conditions | 88 | 58 | 88 | 47 | 79 |
| Find the notes more confusing than helpful | 48 | 67 | 54 | 84 | 43 |
| Worry more | 50 | 92 | 58 | 88 | 45 |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Only participating PCPs completed surveys at HMC.
Appendix Table 2.
Proportion of Patients Who Agreed or Somewhat Agreed With Statements About the Potential Benefits and Risks of Open Visit Notes, by Study Site and Patient Characteristics
| Study Site or Patient Characteristic | Statement |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Making Visit Notes Available Is a Good Idea | I Would Take Better Care of Myself | I Would Better Understand My Health and Medical Conditions | I Would Better Remember the Plan for My Care | I Would Be More Likely to Take My Medications as Prescribed* | I Would Be Better Prepared for Visits | I Would Feel More in Control of My Health Care | The Notes Would Be More Confusing Than Helpful | I Would Worry More | I Would Be Concerned About My Privacy | It Could Make My Doctor's Job More Difficult | |
| Site, % | |||||||||||
| BIDMC | 93 | 70 | 89 | 90 | 56 | 82 | 86 | 9 | 13 | 38 | 29 |
| GHS | 94 | 82 | 93 | 93 | 73 | 85 | 91 | 11 | 15 | 34 | 27 |
| HMC | 97 | 85 | 94 | 94 | 71 | 91 | 96 | 14 | 13 | 35 | 16 |
| Age, % | |||||||||||
| 18–40 y | 95 | 77 | 92 | 93 | 66 | 83 | 91 | 11 | 15 | 30 | 31 |
| 41–55 y | 94 | 79 | 91 | 92 | 68 | 84 | 89 | 10 | 14 | 36 | 27 |
| 56–65 y | 94 | 82 | 93 | 93 | 71 | 85 | 90 | 10 | 15 | 37 | 25 |
| ≥66 y | 93 | 83 | 93 | 93 | 75 | 85 | 90 | 12 | 16 | 37 | 25 |
| Sex, % | |||||||||||
| Female | 94 | 79 | 92 | 93 | 70 | 84 | 90 | 11 | 16 | 36 | 28 |
| Male | 95 | 82 | 93 | 92 | 69 | 86 | 90 | 10 | 14 | 33 | 25 |
| Race, % | |||||||||||
| White | 94 | 80 | 92 | 93 | 70 | 84 | 90 | 10 | 15 | 35 | 27 |
| Black or African American | 96 | 84 | 93 | 92 | 75 | 85 | 91 | 13 | 15 | 45 | 18 |
| Other or multiracial | 93 | 79 | 89 | 90 | 70 | 84 | 88 | 11 | 16 | 40 | 24 |
| Education, % | |||||||||||
| High school/GED or less | 96 | 87 | 94 | 95 | 80 | 86 | 93 | 13 | 18 | 40 | 21 |
| Some college | 95 | 83 | 93 | 94 | 73 | 85 | 91 | 10 | 14 | 34 | 25 |
| College graduate | 95 | 76 | 91 | 92 | 64 | 83 | 89 | 9 | 14 | 33 | 31 |
| Postcollege | 92 | 73 | 89 | 89 | 59 | 82 | 87 | 9 | 14 | 33 | 34 |
| Employment, % | |||||||||||
| Not employed | 94 | 83 | 93 | 93 | 75 | 86 | 91 | 11 | 16 | 37 | 25 |
| Employed | 94 | 79 | 92 | 92 | 67 | 84 | 90 | 10 | 14 | 33 | 28 |
| Self-reported health, % | |||||||||||
| Fair or poor | 96 | 84 | 94 | 94 | 77 | 88 | 93 | 10 | 16 | 34 | 22 |
| Good or excellent | 94 | 79 | 92 | 92 | 68 | 84 | 89 | 11 | 15 | 35 | 28 |
| Ambulatory Care Experiences Survey score, %† | |||||||||||
| Never or usually | 93 | 80 | 91 | 92 | 70 | 83 | 88 | 10 | 14 | 32 | 26 |
| Almost always | 95 | 80 | 93 | 94 | 70 | 85 | 91 | 10 | 15 | 36 | 28 |
| Always | 95 | 81 | 94 | 94 | 71 | 87 | 92 | 11 | 16 | 39 | 27 |
| Perceived Efficacy of Patient–Doctor Interactions score, %‡ | |||||||||||
| Low | 95 | 81 | 93 | 94 | 72 | 86 | 92 | 12 | 17 | 39 | 27 |
| Moderate | 95 | 80 | 93 | 93 | 70 | 85 | 91 | 10 | 15 | 35 | 28 |
| High | 93 | 79 | 90 | 91 | 68 | 82 | 88 | 9 | 13 | 31 | 25 |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center.
Of patients taking medications.
Patient report of patient–doctor communication.
Patient level of confidence about communicating with his or her physician.
Footnotes
Potential Conflicts of Interest: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M11-0962.
Reproducible Research Statement: Study protocol, statistical code, and data set: Not available.
Current author addresses and author contributions are available at www.annals.org.
Author Contributions: Conception and design: J. Walker, S.G. Leveille, J.D. Darer, J.G. Elmore, H.J. Feldman, J.D. Ralston, S.E. Ross, T. Delbanco.
Analysis and interpretation of the data: J. Walker, S.G. Leveille, L. Ngo, J.G. Elmore, J.D. Ralston, S.E. Ross, T. Delbanco.
Drafting of the article: J. Walker, S.G. Leveille, L. Ngo, J.D. Ralston, S.E. Ross, T. Delbanco.
Critical revision of the article for important intellectual content: J. Walker, S.G. Leveille, L. Ngo, E. Vodicka, J.G. Elmore, J.D. Ralston, S.E. Ross, T. Delbanco.
Final approval of the article: J. Walker, S.G. Leveille, L. Ngo, E. Vodicka, J.D. Darer, S. Dhanireddy, J.G. Elmore, H.J. Feldman, M.J. Lichtenfeld, N. Oster, J.D. Ralston, S.E. Ross, T. Delbanco.
Provision of study materials or patients: J. Walker, S.G. Leveille, E. Vodicka, J.D. Darer, S. Dhanireddy, J.G. Elmore, M.J. Lichtenfeld, N. Oster, J.D. Ralston, S.E. Ross, T. Delbanco.
Statistical expertise: S.G. Leveille, L. Ngo.
Obtaining of funding: J. Walker, T. Delbanco.
Administrative, technical, or logistic support: E. Vodicka, H.J. Feldman, M.J. Lichtenfeld, N. Oster.
Collection and assembly of data: J. Walker, S.G. Leveille, E. Vodicka, H.J. Feldman, M.J. Lichtenfeld, N. Oster.
References
- 1.Reti SR, Feldman HJ, Ross SE, Safran C. Improving personal health records for patient-centered care. J Am Med Inform Assoc. 2010;17:192–5. doi: 10.1136/jamia.2009.000927. PMID: 20190063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ralston JD, Martin DP, Anderson ML, Fishman PA, Conrad DA, Larson EB, et al. Group Health Cooperative's transformation toward patient-centered access. Med Care Res Rev. 2009;66:703–24. doi: 10.1177/1077558709338486. PMID: 19549993. [DOI] [PubMed] [Google Scholar]
- 3.Pagliari C, Detmer D, Singleton P. Potential of electronic personal health records. BMJ. 2007;335:330–3. doi: 10.1136/bmj.39279.482963.AD. PMID: 17703042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NHS Connecting for Health [10 April 2011];Access to your summary care record. Accessed at www.nhscarerecords.nhs.uk/access/ on.
- 5.Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT. Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res. 2004;6:e12. doi: 10.2196/jmir.6.2.e12. PMID: 15249261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Earnest MA, Ross SE, Wittevrongel L, Moore LA, Lin CT. Use of a patient-accessible electronic medical record in a practice for congestive heart failure: patient and physician experiences. J Am Med Inform Assoc. 2004;11:410–7. doi: 10.1197/jamia.M1479. PMID: 15187074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;32:234–9. doi: 10.2337/dc08-1220. PMID: 19017773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ralston JD, Revere D, Robins LS, Goldberg HI. Patients' experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. BMJ. 2004;328:1159. doi: 10.1136/bmj.328.7449.1159. PMID: 15142919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delbanco T, Walker J, Darer JD, Elmore JG, Feldman HJ, Leveille SG, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153:121–5. doi: 10.7326/0003-4819-153-2-201007200-00008. PMID: 20643992. [DOI] [PubMed] [Google Scholar]
- 10.Ross SE, Todd J, Moore LA, Beaty BL, Wittevrongel L, Lin CT. Expectations of patients and physicians regarding patient-accessible medical records. J Med Internet Res. 2005;7:e13. doi: 10.2196/jmir.7.2.e13. PMID: 15914460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenhalgh T, Wood GW, Bratan T, Stramer K, Hinder S. Patients' attitudes to the summary care record and HealthSpace: qualitative study. BMJ. 2008;336:1290–5. doi: 10.1136/bmj.a114. PMID: 18511764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived efficacy in patient-physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc. 1998;46:889–94. doi: 10.1111/j.1532-5415.1998.tb02725.x. PMID: 9670878. [DOI] [PubMed] [Google Scholar]
- 13.Safran DG, Karp M, Coltin K, Chang H, Li A, Ogren J, et al. Measuring patients' experiences with individual primary care physicians. Results of a statewide demonstration project. J Gen Intern Med. 2006;21:13–21. doi: 10.1111/j.1525-1497.2005.00311.x. PMID: 16423118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–67. doi: 10.1001/jama.299.24.2857. PMID: 18577730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simon GE, Ralston JD, Savarino J, Pabiniak C, Wentzel C, Operskalski BH. Randomized trial of depression follow-up care by online messaging. J Gen Intern Med. 2011;26:698–704. doi: 10.1007/s11606-011-1679-8. PMID: 21384219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roblin DW, Houston TK, 2nd, Allison JJ, Joski PJ, Becker ER. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc. 2009;16:683–9. doi: 10.1197/jamia.M3169. PMID: 19567790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, López A, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18:318–21. doi: 10.1136/jamia.2010.006015. PMID: 21262921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weppner WG, Ralston JD, Koepsell TD, Grothaus LC, Reid RJ, Jordan L, et al. Use of a shared medical record with secure messaging by older patients with diabetes. Diabetes Care. 2010;33:2314–9. doi: 10.2337/dc10-1124. PMID: 20739686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mostaghimi A, Crotty BH. Professionalism in the digital age. Ann Intern Med. 2011;154:560–2. doi: 10.7326/0003-4819-154-8-201104190-00008. PMID: 21502653. [DOI] [PubMed] [Google Scholar]