Abstract
Background and aim
The sex of the physician performing the endoscopic procedure is one of the parameters influencing patient satisfaction. Our aim was to characterize patients’ preferences according to their sex, socioeconomic status, and religious beliefs and according to procedure-related variables.
Methods
All patients undergoing an endoscopic procedure at Sheba Hospital between April 2012 and September 2012 were asked to complete a questionnaire regarding their sex, ethnic background, socioeconomic status, religious practice, and preference for an endoscopist of a specific sex. Questionnaires were included for analysis only when more than 95% of the items were addressed.
Results
A total of 1,009 patients agreed to complete the questionnaires; of these 946 (94% [59% male]) were eligible for inclusion. Most patients (675 [70%]) expressed no preference for sex of the endoscopist, while 234 patients (25%) preferred a same-sex endoscopist, and only 55 (6%) preferred an other-sex endoscopist. Stepwise logistic regression analysis showed that in female patients, lower education (odds ratio [OR] = 1.28), non-Jewish religion (OR = 4.86), orthodox religious practice (OR = 2.28), African or Asian ethnic origin (OR = 2.44), scheduled for colonoscopy (OR = 1.90), and no previous endoscopy experience (OR = 1.88) were all associated with a preference for a same-sex endoscopist.
Conclusion
One-quarter of patients preferred the physician performing their examination to be of particular sex. Most of these patients preferred a same-sex endoscopist. Education level, intensity of religious practice, ethnic origin, and type of endoscopic examination were associated with a preference for a same-sex endoscopist. Addressing patients’ preferences may improve the atmosphere in the clinical environment, reduce stress, and facilitate better treatment and adherence to endoscopic surveillance programs.
Keywords: endoscopy, patients’ satisfaction, compliance, patient’s preference
Introduction
Patient satisfaction is becoming an increasingly important outcome measure in health care provision. In line with these developments, attention has been directed recently towards patients’ preferences and satisfaction while undergoing endoscopic procedures.1,2 Colonoscopy is perceived by many patients to be an uncomfortable and invasive procedure,3 and one of the issues that seems to concern patients anticipating endoscopic procedures is the sex of the endoscopist.4,5 Previous studies have shown that female patients attribute more importance to their endoscopists’ sex than do male patients and that they are more prone to postpone the examination in order to wait for a female endoscopist.4 In an attempt to characterize the social characteristics of female patients who preferred a female endoscopist, a recent Korean study found that these patients were younger, better educated, more often employed, and single compared with female patients without sex preference.5
However, these findings are valid to the Korean population. We postulated that different patient populations may give rise to or reveal other factors that play a role in patients’ sex preference.
Our hospital is a tertiary referral center located in the center of Israel. We admit a large and heterogeneous patient population assembled from immigrants from all over the world and various religious groups. We postulated that the patients’ preference for an endoscopist of specific sex might be determined mainly by their ethnocultural origin and the intensity of their religious practice and that also, the type of procedure and personal experience could be significant. Therefore, our aim was to characterize patient preferences according to their sex, socioeconomic status, religious beliefs, the type of procedure they are scheduled for, and the extent of their personal experience in endoscopic procedures. Since we believed the sex of the endoscopist might be important in female as well as male patients, we included both sexes in our study.
Patients and methods
Study design and participants
All patients scheduled for an endoscopy between April 2012 and September 2012 at the Sheba Medical Center, Tel Hashomer, Israel were asked, by the outpatient clinic receptionists, to complete an anonymous questionnaire (Figure S1). Patients were informed that participation in the questionnaire was voluntary and that their answers would not affect the identity or sex of the endoscopist performing the procedure they were about to undergo. The questionnaires were collected by the receptionists before endoscopy. While completing the questionnaire, the patients were ignorant of the sex of the endoscopist performing their examination. The procedures were performed by the entire staff of our department, which includes 15 male and two female endoscopists.
This study was approved by the Sheba Medical Center ethics committee.
Ethnic and religious background
Israel is a multicultural country that accommodates immigrants from all over the world. The latest statistical data show that 75.4% of its population is Jewish, while the remaining 20.5% are Muslim and Christian, mostly of Arabic origin. The remaining 4.1% comprises several minorities (such as Armenians and Druze. Within these broad religious categories, patients range from secular nonbelievers to very orthodox believers, and this spectrum of intensity of religious practice proves highly relevant to our study.
Questionnaire
The questionnaire completed by the patients contained information about age, sex, marital status, number of children, education, religion and the intensity of religious practice, place of birth of the patient and of his/her parents, the endoscopic procedure, and previous endoscopic examinations (Figure S1).
Ethnic origin was determined by the patients’ own self-categorization and his/her parents’ places of birth. Intensity of religious practice was also determined by patients themselves and consisted of three main categories: secular, conservative, and orthodox. Questionnaires were included for analysis only when more than 95% of the items were addressed.
Statistical analysis
The chi-square test was used to assess the relation between categorical responses for each variable. Logistic regression was used to model the association between the dependent variable (sex preference) and the independent variables that were significantly associated in univariate analysis (P < 0.05). In the logistic regression models, P-values < 0.05 were considered significant; the results were presented as odds ratios (OR) with 95% confidence intervals (CI).
Results
A total of 1,009 out of 1,212 patients agreed to complete a questionnaire, of whom 946 (59% male, 41% female) were eligible for inclusion.
The patients’ baseline characteristics are shown in Table 1. The majority of patients (657 [70%]) expressed no preference for an endoscopist of a specific sex, while 234 patients (25%) preferred a same-sex endoscopist, and only 55 (6%) preferred an other-sex endoscopist.
Table 1.
Baseline characteristics of included patients
| Male† n (%) | Female‡ n (%) | P-value n (%) | |
|---|---|---|---|
| Mean age (SD) | 57.1 ± 0.6 | 55.3 ± 0.7 | 0.19 |
| Lower education* | 265 (50) | 212 (44) | 0.02 |
| Non-Jewish faith | 17 (3) | 15 (4) | 0.59 |
| Non-Western background | 79 (15) | 39 (11) | 0.07 |
| Orthodox religious practice | 201 (38) | 152 (40) | 0.53 |
| Colonoscopy vs gastroscopy | 369 (70) | 223 (60) | <0.01 |
| No previous endoscopy | 320 (63) | 211 (58) | 0.14 |
Notes:
N = 553 (59%).
N = 393 (41%).
Data on education level were only available for 508 patients; lower education: ≤8 years of formal education (elementary school).
Abbreviation: SD, standard deviation; vs, versus.
One hundred and forty female patients (36%) compared with 149 (27%) of male patients expressed a sex preference (OR 1.50; 95% CI 1.14–1.98). If a sex preference was stated at all, it was almost always for a same sex endoscopist: 103 (74%) of women and 131 of the men (88%) (OR 0.37; 95% CI 0.20–0.69). But 9% of the female patients preferred a male endoscopist, as compared with 3% of males who preferred a female endoscopist (OR 3.09; 95% CI 1.73–5.51) (Figure 1). The most frequent reason mentioned for this preference was higher trust in the opposite-sex endoscopist.
Figure 1.
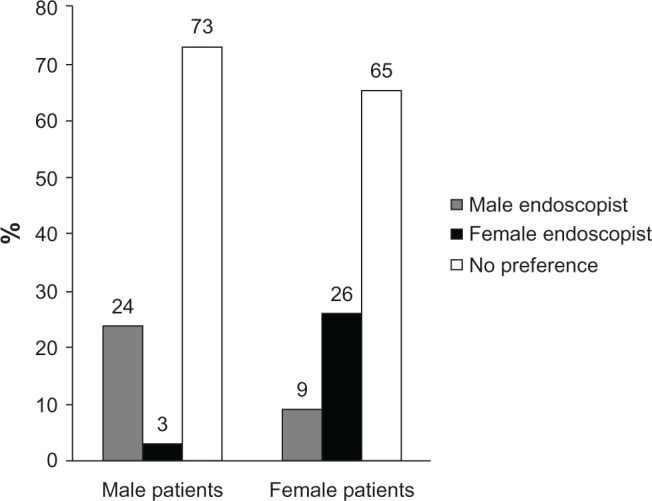
Male endoscopist/female endoscopist preference in male and female patients.
Stepwise logistic regression analysis showed that female sex, lower education (primary school education), orthodox religious practice, African or Asian ethnic origin, colonoscopy, and no previous endoscopy were all associated with a preference for a same-sex endoscopist. The results are shown in Table 2.
Table 2.
Factors influencing same sex preference
| No sex preference N (%) | Same-sex preference N (%) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Age | 56.6 ± 15.0 | 55 ± 16.0 | 0.99 (0.99–1.05) | 0.99 (0.98–1.01) |
| Female sex | 290 (40) | 103 (44) | 1.14 (0.85–1.54) | 1.25 (0.86–1.83) |
| Lower education | 336 (49) | 141 (65) | 1.90 (1.38–2.61) | 1.59 (1.09–2.32) |
| Non-Jewish faith | 18 (3) | 14 (6) | 2.46 (1.21–5.04) | 3.75 (1.52–9.26) |
| Non-Western background | 74 (11) | 44 (21) | 2.06 (1.37–3.11) | 2.03 (1.23–3.34) |
| Orthodox religious practice | 228 (33) | 125 (57) | 2.68 (1.97–3.66) | 2.31 (1.27–2.92) |
| Colonoscopy vs gastroscopy | 432 (63) | 160 (72) | 1.56 (1.11–2.17) | 1.90 (1.27–2.92) |
| No previous endoscopy | 233 (36) | 110 (50) | 1.85 (1.36–2.52) | 1.66 (1.15–2.39) |
Abbreviations: CI, confidence interval; OR, odds ratio; vs, versus.
Demographic variables
As mentioned above, we found that a preference for an endoscopist of specific sex is contingent upon religion, intensity of religious practice, and patient ethnic origin.
We found that a lower level of education was associated with a same-sex preference. Although most of our patients were Jewish (901 [95%]), our study also included some non-Jewish patients, mostly Muslims (19 [2%]) and Christians (10 [1%]), and for 13 patients, the religious background was unknown. The intensity of religious practice was divided into three major categories: secular, conservative, and orthodox. We found that 52 (46%) of the orthodox religious patients had a same-sex preference as compared with 73 (30%) of the conservative patients and 94 (17%) of the secular patients. As well, 76 (89%) of patients who chose religious considerations as the reason for sex preference had a same-sex preference as compared with the 63 patients (51%) who had other considerations.
Patients whose ethnical origin was Asian or African expressed significantly more often a same-sex preference, than patients from other origins. Sex preference was not affected by age and marital status of patients.
Procedure-related variables
Type of examination
The sex of the endoscopist was statistically more important to patients undergoing colonoscopy (194 patients [33%]) compared with patients undergoing gastroscopy (74 patients [25.%]) (OR 1.44; 95% CI 1.06–1.96).
A same-sex preference was expressed by 160 (27%) patients undergoing colonoscopy as compared with 60 (19.%) patients undergoing gastroscopy (OR 1.56; 95% CI 1.11–2.17).
Previous endoscopic procedure
Patients who had never undergone an endoscopy were significantly more likely to have a sex preference than patients who had experienced an endoscopic examination in the past. Among those who had undergone endoscopy in the past, significantly more patients who reported having had a same-sex endoscopist preferred to have a same-sex endoscopist again than did patients who reported having had an endoscopy by an other-sex endoscopist (31% versus 11%, respectively) (OR 4.11; 95% CI 2.36–7.16).
Factors influencing same sex preference in males versus females
We further tried to assess the reason for same-sex preferences in men versus women. The results are shown in Table 3.
Table 3.
Factors influencing same sex preference in males versus females
| Adjusted OR (95% CI)
|
||
|---|---|---|
| Males | Females | |
| Age | 1.01 (0.99–1.03) | 0.97 (0.94–1.99) |
| Lower education | 1.37 (0.84–2.24) | 1.84 (0.99–3.40) |
| Non-Jewish faith | 1.29 (0.24–6.92) | 5.59 (1.42–21.95) |
| Non-Western background | 1.96 (1.05–3.65) | 2.22 (0.91–5.42) |
| Orthodox religious practice | 2.98 (1.81–4.90) | 1.60 (0.87–2.91) |
| Colonoscopy vs gastroscopy | 1.65 (0.94–2.91) | 2.83 (1.49–5.40) |
| No previous endoscopy | 0.83 (0.50–1.39) | 4.00 (2.21–7.25) |
Abbreviations: CI, confidence interval; OR, odds ratio.
Interestingly, we found that the most important factor affecting men’s same-sex preference was an orthodox religious practice (OR 2.98; 95% CI 1.81–4.9) and that this influence was far more important than in women (OR 1.60; 95% CI 0.87–2.91). As for women, there were various factors affecting a same-sex preference: non-Jewish faith and first-time examination were far more common among women as the reason for same-sex preference ([OR 5.59; 95% CI 1.42–21.95] and [OR 4.00; 95% CI 2.21–7.25], respectively) than they were for men ([OR 1.29; 95% CI 0.24–6.92] and [OR 0.83; 95% CI 0.5–1.39], respectively); to a lesser extent, the type of examination (colonoscopy vs gastroscopy) and nonwestern background ([OR 2.83; 95% CI 1.49–5.4] and [OR 2.22; 95% CI 0.91–5.42], respectively) were also more important for women than they were for men ([OR 1.65; 95% CI 0.94–2.91] and [OR 1.96; 95% CI 1.05–3.65], respectively). Education level affected both sexes almost equally as a reason for same sex preference (OR 1.37; 95% CI 0.84–2.24, in men vs OR 1.84; 95% CI 0.99–3.4, in women).
Discussion
The sex of their health care provider is relevant for up to one-third of patients, according to the literature.6–8 We found that sex preference was influenced by sex, level of education, religious practice, and ethnic background as well as by procedure-related variables.
Approximately one-quarter of patients from both sexes expressed a same-sex endoscopist preference. More women than men stated a sex preference but unlike men, not always for a same-sex endoscopist. Our finding that 26% of women preferred a female endoscopist is more or less within the range reported by other studies in the literature, which has shown a female preference for women endoscopists of 30%–48%.3,9,10,11,12 A recent study conducted by Menees et al11 found, not only that 43% of women preferred a female endoscopist, but that 87% of these women were willing to wait more than 30 days for a female endoscopist. An interesting finding in our study was that women, more often than men, preferred an other-sex (ie, male) endoscopist. These patients stated a higher trust in male endoscopists, possibly reflecting traditional perceptions. Hopefully, with the increasing number of female physicians in the field, this perception will change.
Not unexpectedly, patients undergoing colonoscopy attached more importance to the sex of the endoscopist than did patients undergoing gastroscopy. Although the questionnaire did not address the underlying reasons, we speculate that colonoscopy, which involves exposure of intimate organs, is considered more embarrassing by the patients than gastroscopy. In the literature, a sex preference is stronger when intimate procedures are required. Thus, 34% of female patients preferred a female obstetrician,13 and 30% preferred a female breast surgeon.9 Although men are usually considered to have less sex preferences, it was shown by Kerssens et al that 64% of male patients preferred a male physician for anal or genital examination.6
Current guidelines support colonoscopy every 10 years, as the preferred screening option in average-risk individuals aged >50 years.15,16
In almost all European countries, colorectal cancer screening is mainly fecal occult blood test (FOBT)-based, followed by colonoscopy, if positive.17 A joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology makes no clear recommendation about whether to use FOBT or colonoscopy as the primary screening tool. However, it supports both methods for primary screening.18
According to the Health Belief Model,17 individuals who perceive the screening procedure to be embarrassing, uncomfortable, inconvenient, or costly are less likely to participate in the procedure.18–26 In a recent study conducted by Harewood et al, 30% of patients mentioned “embarrassed by the procedure” as a reason for not wanting to undergo screening colonoscopy.3 When patients were asked about methods to improve screening compliance, 21% chose “being able to choose the sex of the endoscopist.” Again, the sex of the endoscopist was ranked as important by more women (29%) than men (18%). One of the conclusions of this study was that the stress of a lower gastrointestinal endoscopy may be minimized by offering the choice of a female endoscopist to female patients and that this may especially improve the compliance of female patients with the procedure.
Contrary to the findings in a Korean study5 and in agreement with the findings of a recent study conducted in the Hispanic population in the United States,10 we found that the less educated patient had a stronger sex preference, as well as patients who had orthodox religious beliefs. The more traditional the religious beliefs, the greater importance patients from both sexes attached to the sex of the endoscopist. Orthodox Jews evidenced particular sensitivity to body parts exposure, as demonstrated by their dressing codes; this sensitivity is even more pronounced when intimate organs are involved. Interestingly, religion influenced same-sex preference in men much more than in women. In fact, this was the main reason for same-sex preference in men, while women stated a variety of reasons.
As for education level, we do not have specific data, but we believe higher education may widen one’s horizons, so that sex issues seem less important. Patients from Asian or African ethnic origins were more likely to have a sex preference than patients from European origin. We believe that this finding is explained by the fact that patients from non-Western origins tend to attach more importance to tradition and therefore, to modest behavior, which includes the prohibition of body exposure.27
The small group of non-Jewish women, mainly of Muslim origin, who took part in this study showed a strong same-sex preference. Eighty-three percent of Muslim women in our study preferred a female endoscopist. However, due to the small number of patients, no firm conclusions can be drawn.
We found that patients who had already undergone an endoscopy were significantly less likely to have a sex preference than were patients who had never experienced endoscopic examinations. We believe this finding can be explained by experience – patients who had undergone the examination in the past knew what to expect and were less concerned by it and by potential embarrassment during the procedure. These findings are in concert with the study by Zapatier et al,10 which showed a stronger sex preference among patients who had not previously undergone a colonoscopy. Also, Sheikh et al14 reported a strong preference for colonoscopy as a screening method in patients who had previously undergone a colonoscopy. On the other hand, Harewood et al3 found that endoscopist’s sex was more important in the group of previously screened patients (30% vs 21%). The reason for this inconsistency is not clear.
It should be noted that our study design has a few limitations. First, the fact that patients completed the questionnaires just before entering the endoscopy room may have caused a bias, since before the examination, patients tend to be under stress, which may have influenced their responses. Second, since in our center, patients cannot choose their endoscopist, patients who attribute importance to the sex of the endoscopist might have chosen beforehand to undergo the examination in a center where they could have the option of choice. Furthermore, we have no data on patients who were referred to colonoscopy by their physician but who refused because of the physical embarrassment involved. All these limitations may have caused an underestimation of the percentage of patients with a preference for an endoscopist of specific sex. However, as far as we know, this is the largest study assessing sex preference among endoscopy patients conducted so far.
Another limitation is the specific patient population composition in our study. This reflects the diverse population in Israel, but few conclusions can be drawn regarding other populations from different cultural backgrounds.
In conclusion, approximately one-third of patients, men as well as women, expressed a preference for an endoscopist of specific sex. Most of these patients preferred a same-sex endoscopist. Lower level of education, orthodox religious believes, ethnic origin, and colonoscopy (vs gastroscopy) are all associated with a sex preference in our group of patients. Since 26% of female patients showed a preference for a female endoscopist, it is important to offer these patients that choice. Hopefully, addressing patients’ preference will advance better adherence to endoscopic surveillance programs.
Supplementary figure
The study questionnaire.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Yacavone RF, Locke GR, Gostout CJ, Rockwood TH, Thieling S, Zinsmeister AR. Factors influencing patient satisfaction with GI endoscopy. Gastrointest Endosc. 2001;53(7):703–710. doi: 10.1067/mge.2001.115337. [DOI] [PubMed] [Google Scholar]
- 2.Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc. 2009;69(4):883–891. doi: 10.1016/j.gie.2008.06.024. [DOI] [PubMed] [Google Scholar]
- 3.Harewood GC, Wiersema MJ, Melton LJ. A prospective, controlled assessment of factors influencing acceptance of screening colonoscopy. Am J Gastroenterol. 2002;97(12):3186–3194. doi: 10.1111/j.1572-0241.2002.07129.x. [DOI] [PubMed] [Google Scholar]
- 4.Varadarajulu S, Petruff C, Ramsey WH. Patient preferences for gender of endoscopists. Gastrointest Endosc. 2002;56(2):170–173. doi: 10.1016/s0016-5107(02)70173-9. [DOI] [PubMed] [Google Scholar]
- 5.Lee SY, Yu SK, Kim JH, et al. Link between a preference for women colonoscopists and social status in Korean women. Gastrointest Endosc. 2008;67(2):273–277. doi: 10.1016/j.gie.2007.06.039. [DOI] [PubMed] [Google Scholar]
- 6.Kerssens JJ, Bensing JM, Andela MG. Patient preference for genders of health professionals. Soc Sci Med. 1997;44(10):1531–1540. doi: 10.1016/s0277-9536(96)00272-9. [DOI] [PubMed] [Google Scholar]
- 7.Fennema K, Meyer DL, Owen N. Sex of physician: patients’ preferences and stereotypes. J Fam Pract. 1990;30(4):441–446. [PubMed] [Google Scholar]
- 8.Weyrauch KF, Boiko PE, Alvin B. Patient sex role and preference for a male or female physician. J Fam Pract. 1990;30(5):559–562. [PubMed] [Google Scholar]
- 9.Reid I. Patients’ preference for male or female breast surgeons: questionnaire study. BMJ. 1998;317:1051. doi: 10.1136/bmj.317.7165.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zapatier JA, Kumar AR, Perez A, Guevara R, Schneider A. Preferences for ethnicity and sex of endoscopists in a Hispanic population in the United States. Gastrointest Endosc. 2011;73(1):89–97. doi: 10.1016/j.gie.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 11.Menees SB, Inadomi JM, Korsnes S, Elta GH. Women patients’ preference for women physicians is a barrier to colon cancer screening. Gastrointest Endosc. 2005;62(2):219–223. doi: 10.1016/s0016-5107(05)00540-7. [DOI] [PubMed] [Google Scholar]
- 12.Fidler H, Hartnett A, Cheng Man K, Derbyshire I, Sheil M. Sex and familiarity of colonoscopists: patient preferences. Endoscopy. 2000;32(6):481–482. doi: 10.1055/s-2000-645. [DOI] [PubMed] [Google Scholar]
- 13.Howell EA, Gardiner B, Concato J. Do women prefer female obstetricians? Obstet Gynecol. 2002;99(6):1031–1035. doi: 10.1016/s0029-7844(02)01980-4. [DOI] [PubMed] [Google Scholar]
- 14.Sheikh RA, Kapre S, Calof OM, Ward C, Raina A. Screening preferences for colorectal cancer: a patient demographic study. South Med J. 2004;97(3):224–230. doi: 10.1097/01.SMJ.0000078619.39604.3D. [DOI] [PubMed] [Google Scholar]
- 15.Smith RA, Cokkinides V, Brooks D, Saslow D, Brawley OW. Cancer screening in the United States, 2010: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2010;60(2):99–119. doi: 10.3322/caac.20063. [DOI] [PubMed] [Google Scholar]
- 16.Allison JE, Lawson M. Screening tests for colorectal cancer: a menu of options remains relevant. Curr Oncol Rep. 2006;8(6):492–498. doi: 10.1007/s11912-006-0079-4. [DOI] [PubMed] [Google Scholar]
- 17.Becker M. Understanding Attitudes and Predicting behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- 18.Macrae FA, Hill DJ, St John DJ, Ambikapathy A, Garner JF. Predicting colon cancer screening behavior from health beliefs. Prev Med. 1984;13(1):115–126. doi: 10.1016/0091-7435(84)90044-6. [DOI] [PubMed] [Google Scholar]
- 19.Spector MH, Applegate WB, Olmstead SJ, DiVasto PV, Skipper B. Assessment of attitudes toward mass screening for colorectal cancer and polyps. Prev Med. 1981;10(1):105–109. doi: 10.1016/0091-7435(81)90011-6. [DOI] [PubMed] [Google Scholar]
- 20.Price JH. Perceptions of colorectal cancer in a socioeconomically disadvantaged population. J Community Health. 1993;18(6):347–362. doi: 10.1007/BF01323966. [DOI] [PubMed] [Google Scholar]
- 21.Kelly RB, Shank JC. Adherence to screening flexible sigmoidoscopy in asymptomatic patients. Med Care. 1992;30(11):1029–1042. doi: 10.1097/00005650-199211000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Neale AV, Demers RY, Herman S. Compliance with colorectal cancer screening in a high-risk occupational group. J Occup Med. 1989;31(12):1007–1012. doi: 10.1097/00043764-198912000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Olynyk JK, Aquilia S, Fletcher DR, Dickinson JA. Flexible sigmoidoscopy screening for colorectal cancer in average-risk subjects: a community-based pilot project. Med J Aust. 1996;165(2):74–76. doi: 10.5694/j.1326-5377.1996.tb124851.x. [DOI] [PubMed] [Google Scholar]
- 24.Vernon SW, Acquavella JF, Yarborough CM, Hughes JI, Thar WE. Reasons for participation and nonparticipation in a colorectal cancer screening program for a cohort of high risk polypropylene workers. J Occup Med. 1990;32(1):46–51. doi: 10.1097/00043764-199001000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Bejes C, Marvel MK. Attempting the improbable: offering colorectal cancer screening to all appropriate patients. Fam Pract Res J. 1992;12(1):83–90. [PubMed] [Google Scholar]
- 26.Farrands PA, Hardcastle JD, Chamberlain J, Moss S. Factors affecting compliance with screening for colorectal cancer. Community Med. 1984;6(1):12–19. [PubMed] [Google Scholar]
- 27.Rabin C, editor. Being Different in Israel – Ethnical Origin, Gender and Treatment. Tel Aviv: Ramot Publishing; 1999. Hebrew. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The study questionnaire.


