Abstract
Background
Minimally invasive video-assisted thyroidectomy (MIVAT) advantages include a smaller incision, less extensive surgical dissection, improved visualization secondary to rigid fiberoptics, and decreased postoperative pain. The aims of our study were to report our experience using expanded indications of MIVAT.
Methods
A retrospective chart review of a single surgeon's initial experience was carried out at a tertiary academic cancer center.
Results
In all, 53 patients were identified, of whom 40 underwent total thyroidectomy and 13 underwent hemithyroidectomy. Thyroid volume, nodule size, incision length, and surgical time were all examined. Most common pathology was well-differentiated papillary thyroid cancer (69.8%): 42% of patients had evidence of thyroiditis found on pathology; 17% of patients had temporary vocal cord paralysis, with only 1 case of vocal cord paralysis persisting >6 months (1.9%). Six patients (11%) experienced temporary hypocalcemia, requiring postoperative calcium supplementation; no patients experienced permanent hypocalcemia.
Conclusions
The use of MIVAT with expanded indications shows complication rates comparable to those of traditional open thyroidectomy.
Keywords: thyroid, minimally invasive, thyroidectomy, thyroid neoplasm, video-assisted surgery
The incidence of well-differentiated thyroid cancer is increasing mainly as a result of the number of incidental thyroid nodules being detected by the increased use of imaging such as ultrasound, CT scan, MRI, and PET scans.1 As a result, surgeons are performing more thyroid surgery than ever before. Many of these thyroid operations are carried out on small volume thyroid glands with small nodules. Minimally invasive video-assisted thyroidectomy (MIVAT), first described by Miccoli et al2 in 1999, is an ideal technique for managing these types of patients with benefits that include a smaller scar, less extensive surgical dissection, and decreased postoperative pain.3 Patients often experience a shorter healing time, with some centers performing the surgery on an outpatient basis. In addition, improved voice and swallow outcomes have also been reported with MIVAT over conventional open thyroidectomy.4 Several high-volume thyroid surgical centers have now adopted MIVAT, and the safety of the procedure has been well reported.3,5 The early studies on MIVAT used limited indications for the surgery. Initial contraindications included large nodules (>25–30 mm), thyroiditis, an abnormal thyroid gland (>20 cm3), prior neck surgery, central compartment neck metastases, and large malignant tumors with extrathyroidal extension.5 With increasing experience it is now possible to carry out this technique with expanded indications. The objective of this retrospective study was to report the outcomes of patients undergoing MIVAT at a high-volume academic tertiary cancer center using expanded indications that include patients with prior neck surgery, larger thyroid glands, larger thyroid lesions, and the presence of thyroiditis.
Materials and Methods
After obtaining institutional review board approval for the study, we performed a retrospective review of patients who had undergone MIVAT for either hemithyroidectomy or total thyroidectomy at our institution, a tertiary academic cancer center. Patient data spanned from July 2008 to September 2009. Patient characteristics recorded included age, sex, body mass index (BMI), and prior neck surgery. Obesity was defined as a BMI > 30. Tumor characteristics recorded included size of the thyroid gland, size of the nodule, final pathology, and thyroid volume. Thyroid volume was determined using a formula described by Miccoli et al,6 which multiplies the ultrasound dimensions of the thyroid, width × height × depth, adding the left and right lobes, then multiplying by π/6. Vocal cord function for every patient was documented by preoperative and postoperative fiber-optic laryngoscopy. Treatment characteristics recorded included lobectomy or total thyroidectomy, length of incision, operation time, and hospital length of stay. Postoperative complications (infection, hematoma, recurrent laryngeal nerve [RLN] palsy, hypocalcemia) were recorded and compared with reported figures for traditional open surgery. Hypocalcemia was defined as any calcium level <7.8, when checked 6 hours after surgery and the following morning. Nerve monitoring was performed with the NIM (Nerve Integrity Monitoring) Response Monitor (Medtronic, Langhorne, PA), using hardware version 2.0 or 3.0.
Results
In all, 53 patients were identified, of whom 40 patients underwent total thyroidectomy and 13 patients underwent hemithyroidectomy. Forty-three patients (81%) were women, mostly white (91%), with a median age of 52 years (range, 20 to 87 years). Average BMI was 27, including 13 obese patients. Three patients (5.6%) had previous neck surgery, including 1 patient with prior neck dissection and 2 patients with prior anterior cervical discectomy. Average thyroid volume on preoperative ultrasound was 9.1 cm3 (range, 2.9–50.7 cm3) and on pathology was 24.4 cm3 (range, 4.8–134 cm3; median, 9.1 cm3) for total thyroidectomy and 24.8 cm3 (range, 4.8–80.5 cm3; median, 14.9 cm3) for hemithyroidectomy. Nodule size ranged from 0.9 to 5.4 cm, with a median nodule size of 3.2 cm. All patients were found to have bilateral vocal cord mobility of preoperative examination. Patient demographics are summarized in Table 1. All but 1 case were performed with laryngeal nerve monitoring. The nerve monitor could not be used in 1 case because of a technical failure. In all other cases, the recurrent laryngeal nerve was identified on both sides by visualization and was confirmed with nerve stimulation. The median incision length was 4 cm (range, 3–8 cm). Eight cases (15.1%) necessitated an increased surgical incision, but the MIVAT technique continued to be used in this setting. Surgical time averaged 113 minutes for hemithyroidectomy and 149 minutes for total thyroidectomy. Four patients (7.5%) had drains placed in the setting of large surgical dissection beds. The average hospital stay was 1.4 days; the average follow-up period was 3 months.
Table 1.
Patient demographics.
| Factor | No. (%)* |
|---|---|
| Total surgeries | 53 |
| Thyroidectomy | 40 (75) |
| Hemithyroidectomy | 13 (25) |
| Average age, y | 51 |
| Sex | |
| Female | 43 (81) |
| Male | 10 (19) |
| Race | |
| White | 48 (91) |
| Hispanic | 3 (6) |
| Asian | 1 (2) |
| Median nodule size, cm (range) | 3.2 (0.9–5.3) |
| Average thyroid lobe volume (by ultrasound) | 18.3 (2.9–50.7) |
Except as otherwise noted.
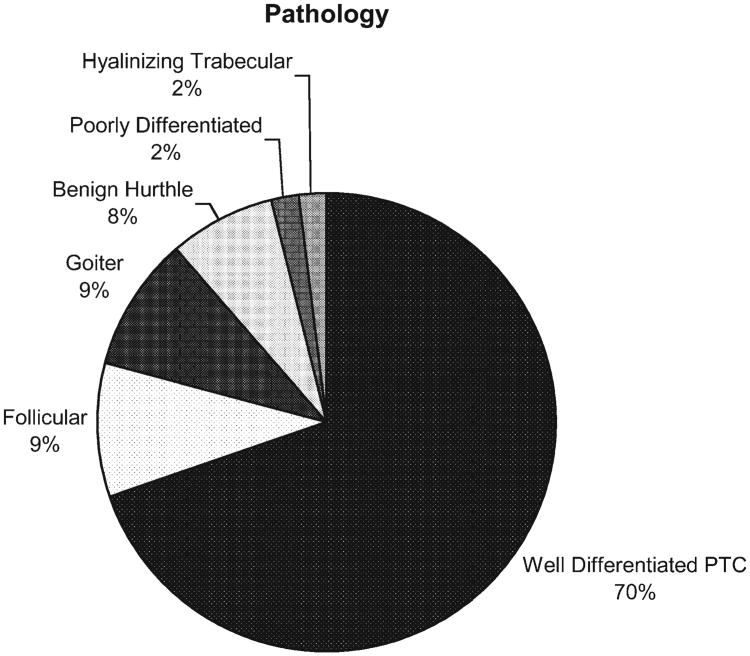
The most common finding on pathology was well-differentiated papillary thyroid cancer (69.8%) followed by follicular lesions (9.4%), goiter (9.4%), and benign Hürthle lesions (7.5%). There was 1 patient with poorly differentiated cancer (1.9%). Seventeen patients (32.1%) had evidence of resected parathyroid tissue on pathology review; 4 patients (7.5%) underwent parathyroid reimplantation; and 22 patients (42%) had evidence of thyroiditis on pathology. Pathology results are summarized in Figure 1.
Figure 1.
Thyroid pathology. The most common finding on pathology was well-differentiated papillary thyroid carcinoma (70%) followed by follicular lesions (9%), goiter (9%), and benign Hürthle lesions (8%). One patient had poorly differentiated cancer.
The most common complication was temporary vocal cord paralysis (17%), with 1 case of vocal cord paralysis persisting >6 months (1.9%). Both recurrent laryngeal nerves were identified and confirmed with the nerve monitor in this case. Six patients (11%) experienced temporary hypocalcemia requiring postoperative calcium supplementation, and no patients experienced permanent hypocalcemia. There were no instances of keloid formation at the incision site. One patient (1.9%) was treated with oral antibiotics for a wound infection, and there were no seromas or hematomas. One patient (1.9%) was treated for a hypertrophic scar. Eleven patients (21%) received postoperative radioactive iodine as part of the management for their thyroid malignancy. Four patients subsequently underwent completion thyroidectomy, which was not performed with minimally invasive technique. On limited follow-up (average of 3 months postoperatively), there were no cases of recurrence. Surgical complications are summarized in Table 2.
Table 2.
Thyroidectomy complications.
| Complication | No. (%) |
|---|---|
| Temporary vocal cord paralysis | 9 (17) |
| Vocal cord paralysis > 6 mo | 1 (1.9) |
| Temporary hypocalcemia | 6 (11.3) |
| Permanent hypocalcemia | 0 (0) |
| Hypertrophic scar | 1 (1.9) |
| Keloid | 0 (0) |
| Wound infection | 1 (1.9) |
| Seroma | 0 (0) |
| Hematoma | 0 (0) |
Discussion
The safety and efficacy of MIVAT used under limited conditions have been demonstrated in multiple studies in the literature. A recently published prospective review of >200 cases at multiple institutions reported no permanent vocal cord paralysis or permanent hypoparathyroidism. Concerns regarding adequacy of resection were addressed by Miccoli in a prospective randomized trial for papillary cancer, where postoperative thyroglobulin, radioactive iodine uptake levels, and complication rates were found to be equivalent to those of patients treated with conventional open thyroidectomy or MIVAT.5 The technique was initially described for limited indications; initial contraindications included large nodules (>2.5 to 3.0 cm), thyroiditis, an enlarged thyroid gland (>20 cm3), prior neck surgery, central compartment neck metastases, and large malignant tumors with extrathyroidal extension. Recently, Lai et al7 explored several cases using expanded indications for MIVAT, and demonstrated the oncologic completeness by evaluating postoperative radioiodine uptake.
In our study, we confirm the findings reported by Lai and colleagues by showing that MIVAT can be used for expanded indications. Although prior studies limited the technique to smaller nodules (2.5–3.0 cm), our study looked at nodules ranging from 0.9 to 5.4 cm, with a median nodule size of 3.2 cm. Previous studies limited resection to thyroid gland volumes that were ≤20 cm3 . The thyroid volumes on pathology in this study ranged from 4.8 to 80.5 cm3, with an average volume of 24.4 cm3 (median, 9.1 cm3). Lobectomy specimens ranged from 5.4 to 134 cm3, with an average volume of 24.8 cm3 (median, 14.9 cm3). Although patients with prior neck surgery were typically excluded, patients in this study included those with prior neck surgery (n = 3), such as anterior cervical discectomy and neck dissection. Prior studies using MIVAT included a patient population with a lower rate of malignant disease, 20% in some larger series.5 Our study had a malignant disease rate of 74%. In the past, thyroiditis was viewed as a contraindication to minimally invasive approach; in the current study, 42% (n = 22) of patients had evidence of thyroiditis on pathology.
A review of the complications of MIVAT compared with traditional open thyroidectomy show comparable rates of postoperative permanent hypocalcemia and vocal cord injury. Reported rates of temporary RLN paralysis with open thyroidectomy range from 0.5 to 8.9%.8,9 Rates of permanent RLN paralysis, or paralysis lasting >6 months, range from 1.2 to 5.2% of cases.10 Our study showed a high rate of temporary RLN paralysis (17%). The high incidence of temporary vocal cord dysfunction may be largely attributed to the immediate routine postoperative evaluation of all patients by flexible laryngoscopy. In part, it may arise from the adoption of this new surgical technique and this challenging patient population with increased temporary neuropraxia of the recurrent laryngeal nerve. With increased experience we anticipate a reduction in the incidence of temporary vocal cord dysfunction. However, our rate of permanent RLN paralysis (1.9%) was within the range reported for open thyroidectomy. Temporary hypocalcemia occurred in 11% of patients, within the reported averages of 3% to 25%.8,11,12 Many institutions that perform outpatient total thyroidectomy (open or MIVAT) routinely discharge patients on calcium replacement and vitamin D supplements, and this may obscure the real incidence of transient hypocalcemia. Permanent hypocalcemia, which can occur in 0.4% to 29% of open thyroidectomy cases, did not occur in this study.9,11,13 Overall, our rates of permanent hypocalcemia (0%) and permanent RLN paralysis (1.9%) are consistent with the reported literature.
The high rate of malignant disease in our series reflects the referral pattern of our institution, a tertiary academic cancer center. As noted previously, MIVAT has been shown to be as effective as open surgery, in terms of completeness of resection for low and intermediate risk well-differentiated thyroid disease.3 In addition to a 70% rate of papillary thyroid cancer in our series, 1 patient was noted with well-encapsulated poorly differentiated thyroid carcinoma that was diagnosed only on final pathology. We emphasize that MIVAT is still best suited for low- and intermediate-risk thyroid disease; any unusual or more aggressive pathologies should be managed appropriately, including additional surgery if needed.
The results of this study show the safety of MIVAT, carried out with expanded indications, and add further support for its safety and adaptability. On average, patients in this study undergoing MIVAT had larger thyroid volumes, larger nodules, and higher rates of malignant disease than those of patients in previously published studies using this technique. We experienced an increased rate of temporary vocal cord paralysis with this technique, compared with traditional open thyroidectomy. The incidence of complication rates for hematoma, wound infection, hypocalcemia, and permanent vocal cord paralysis were comparable. We establish the safety of the procedure with expanded indications, and add further support for the safety and adaptability of the procedure to other centers.
Conclusions
We establish the safety of MIVAT with expanded indications in our hands, and add further support for the safety and adaptability of the procedure to other centers. MIVAT can be applied to patients with expanded indications, with comparable rates of hematoma, wound infection, hypocalcemia, and permanent vocal cord paralysis.
Acknowledgments
The project described was supported by Award Number T32CA009685 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Footnotes
This work was presented at the Annual Meeting of the American Head and Neck Society, Las Vegas, Nevada, April 28–29, 2010.
References
- 1.Kent WD, Hall SF, Isotalo PA, Houlden RL, George RL, Groome PA. Increased incidence of differentiated thyroid carcinoma and detection of subclinical disease. CMAJ. 2007;177:1357–1361. doi: 10.1503/cmaj.061730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miccoli P, Berti P, Conte M, Bendinelli C, Marcocci C. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest. 1999;22:849–851. doi: 10.1007/BF03343657. [DOI] [PubMed] [Google Scholar]
- 3.Miccoli P, Pinchera A, Materazzi G, et al. Surgical treatment of low- and intermediate-risk papillary thyroid cancer with minimally invasive video-assisted thyroidectomy. J Clin Endocrinol Metab. 2009;94:1618–1622. doi: 10.1210/jc.2008-1418. [DOI] [PubMed] [Google Scholar]
- 4.Lombardi CP, Raffaelli M, D'Alatri L, et al. Video-assisted thyroidectomy significantly reduces the risk of early postthyroidectomy voice and swallowing symptoms. World J Surg. 2008;32:693–700. doi: 10.1007/s00268-007-9443-2. [DOI] [PubMed] [Google Scholar]
- 5.Terris DJ, Angelos P, Steward DL, Simental AA. Minimally invasive video-assisted thyroidectomy: a multi-institutional North American experience. Arch Otolaryngol Head Neck Surg. 2008;134:81–84. doi: 10.1001/archoto.2007.22. [DOI] [PubMed] [Google Scholar]
- 6.Miccoli P, Minuto MN, Orlandini C, Galleri D, Massi M, Berti P. Ultrasonography estimated thyroid volume: a prospective study about its reliability. Thyroid. 2006;16:37–39. doi: 10.1089/thy.2006.16.37. [DOI] [PubMed] [Google Scholar]
- 7.Lai SY, Walvekar RR, Ferris RL. Minimally invasive video-assisted thyroidectomy: expanded indications and oncologic completeness. Head Neck. 2008;30:1403–1407. doi: 10.1002/hed.20883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Runkel N, Riede E, Mann B, Buhr HJ. Surgical training and vocal-cord paralysis in benign thyroid disease. Langenbecks Arch Surg. 1998;383:240–242. doi: 10.1007/s004230050125. [DOI] [PubMed] [Google Scholar]
- 9.Shaha A, Jaffe BM. Complications of thyroid surgery performed by residents. Surgery. 1988;104:1109–1114. [PubMed] [Google Scholar]
- 10.Manolidis S, Takashima M, Kirby M, Scarlett M. Thyroid surgery: a comparison of outcomes between experts and surgeons in training. Otolaryngol Head Neck Surg. 2001;125:30–33. doi: 10.1067/mhn.2001.116790. [DOI] [PubMed] [Google Scholar]
- 11.Cummings CW, editor. Otolaryngology: head and neck surgery. 4th. St. Louis, MO: Mosby; 2005. [Google Scholar]
- 12.Foster RS., Jr Morbidity and mortality after thyroidectomy. Surg Gynecol Obstet. 1978;146:423–429. [PubMed] [Google Scholar]
- 13.Burge MR, Zeise TM, Johnsen MW, Conway MJ, Qualls CR. Risks of complication following thyroidectomy. J Gen Intern Med. 1998;13:24–31. doi: 10.1046/j.1525-1497.1998.00004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]