Abstract
Sexually victimized women may make sexual decisions differently than non-victimized women. This study used an eroticized scenario and laboratory alcohol administration to investigate the roles of victimization history, intoxication, and relationship context in women’s perceptions of a male partner and their subsequent intentions for unprotected sex. A community sample of 436 women completed childhood sexual abuse (CSA) and adolescent/adult sexual assault (ASA) measures. After random assignment to an alcohol or control condition, participants read and projected themselves into a sexual scenario which depicted the male partner as having high or low potential for a lasting relationship. Participants rated their perceptions of his intoxication, STI risk level, and anticipated reactions to insistence on condom use. They then indicated their likelihood of allowing the partner to decide how far to go sexually (abdication) and engaging in unprotected sex. SEM analyses revealed that intoxication predicted greater unprotected sex likelihood indirectly via abdication. CSA and ASA predicted partner perceptions, which in turn predicted unprotected sex likelihood. These findings indicate that, compared to non-victimized counterparts, sexually victimized women may respond differently in sexual encounters partly as a function of their perceptions of partners’ STI risk and anticipated reactions to condom insistence.
Sexually transmitted infections (STIs), including HIV, pose serious threats to women’s health (CDC, 2011; CDC, 2012). Infection risk can be reduced through the use of male condoms. However, because women do not wear condoms themselves, their successful condom use often hinges on asking for and getting the cooperation of male partners; difficulty with either may make unprotected sex more likely. Little is currently known about how, in the moments preceding condom negotiation, a woman’s perceptions of her partner and his anticipated reactions to such a request might affect her approach to him and her ensuing risk taking. The present work addresses this knowledge gap by examining whether a woman’s perceptions of her male partner, specifically his STI risk, his level of intoxication, and his anticipated response to her insistence on condom use, affect her decision to have sex without a condom. In light of growing evidence suggesting that a woman’s background and situational context both influence her likelihood of having unprotected sex, we also examined sexual victimization history, acute alcohol intoxication, and the potential for a relationship with the partner.
Sexual Victimization History and Unprotected Sex
Data from both survey and experimental studies indicate that victimized women may perceive and respond to sexual situations differently than non-victimized women and may do so in ways that lead to riskier sexual decisions. Numerous survey studies have linked childhood sexual abuse (CSA) with both subsequent sexual risk behavior and revictimization in adulthood (see reviews by Lalor & McElvaney, 2010 and Malow, Devieux, & Lucenko, 2006). Messman-Moore and Long’s review (2003) found that women with a CSA history were between two and 11 times more likely than women without such a history to be sexually victimized in adulthood. Regardless of CSA history, population rates of adult and adolescent sexual assault (ASA) are substantial (Tjaden & Thoennes, 2006), and both CSA and ASA are associated with sexual risk behavior (Davis, Combs-Lane, and Jackson, 2002; Molitor, Ruiz, Klausner, and McFarland, 2000). One proposed explanation for the relationship between victimization history and sexual risk is that emotional reactions to abuse or assault, such as fear, can decrease self-protective behaviors such as assertive condom negotiation and result in unprotected sex (Quina, Morokoff, Harlow, and Zurbriggen, 2004). Another explanation focuses on changes in cognition after abuse or assault that result in victimized women perceiving less risk in unprotected sexual behavior than non-victimized women (Smith, Davis, and Fricker-Elhai, 2004). In sum, either child or adult sexual victimization, or the combination of the two, seem likely to act upon women’s perceptions, interactions, and decisions regarding sexual risk prevention and condom use.
Experimental data are increasingly available regarding how a sexual victimization background may combine with proximal situational factors, such as alcohol intoxication, to influence women’s sexual risk behavior. Experiments have assessed in-the-moment unprotected sex intentions with scenarios in which participants project themselves into an eroticized consensual encounter. Using this methodology, Schacht et al. (2010) found that women with CSA histories reported a lower likelihood of condom use than women with no victimization histories. Likewise, Stoner et al. (2008) found that ASA victimized women were less sexually assertive, resulting in less condom insistence and greater likelihood of unprotected sex.
Victimization history may also influence unprotected sex behavior through its associations with women’s partner perceptions. Quina and her colleagues found a strong correlation between women’s history of sexual victimization and their anticipation of negative responses to condom use requests (Quina, Harlow, Morokoff, Burkholder & Deiter, 2000; Quina et al., 2004). Women’s perception of a partner as more likely to react negatively was also associated with less assertive refusal of unsafe sex.
Alcohol Intoxication and Unprotected Sex
Comprehending alcohol’s impact on unprotected sex decisions may be a key element of understanding the role of victimization history in sexual risk behavior. Victimized women overall tend to drink differently than non-victimized women (e.g., Brener, McMahon, Warren & Douglass, 1999; Kendler et al., 2000), specifically consuming greater quantities of alcohol more frequently and being more likely to drink before sex. Ullman’s review of studies on links between alcohol and sexual assault (2003) proposes a theoretical framework explaining this relationship. It states that the association between sexual victimization and alcohol is most likely bidirectional. Victimization in childhood or early adulthood may lead to risky behavior such as drinking to cope or heavy drinking, and these behaviors in turn may increase likelihood of subsequent sexual assault (Ullman, 2003).
Studies of alcohol’s relationship with unprotected sex have produced mixed findings. Although alcohol appears to have a global association with unprotected sex, in that individuals who drink to intoxication use condoms less frequently overall than those who do not, event-level diary studies (e.g. Leigh et al., 2008) demonstrate that this relationship does not persist when individuals report on their intoxication and condom use during specific sexual events. However, recent theory-building longitudinal work by Cooper (2010) supports the idea that contextual factors, along with individual characteristics, affect the relationship between alcohol and unsafe sex. And experimental studies using in-the-moment scenarios (e.g., Hendershot & George, 2007) have established that in specific hypothetical contexts, alcohol increases sexual risk-taking intentions. This effect seems more pronounced at higher rather than at lower alcohol dosages (George et al., 2009).
Experimental findings suggest that a decreased ability to make or enforce sexual decisions while intoxicated may occur in both consensual and assaultive situations, and may be another factor affecting women’s unprotected sex likelihood. For example, alcohol administration experiments using filmed scenarios of consensual sexual situations indicate that intoxicated women express a higher likelihood of having unprotected sex than sober women (Maisto, Carey, Carey, Gordon, & Schum, 2004). Experimental studies also suggest that intoxicated women respond more passively in sexual assault situations than sober women (Davis, George & Norris, 2004; Norris et al., 2006; Stoner et al., 2007).
Along with her own intoxication, a woman’s perception of her partner’s intoxication also colors the situation when alcohol consumption is involved in the sexual encounter (Cooper, 2002; George & Stoner, 2000). Previous findings (e.g. George et al., 1997) suggest that a drinking man is perceived by women as being more sexual than a non-drinking man and that the more he drinks, the more this perception increases. Women who are moderate-to-heavy drinkers tend to believe that alcohol makes men both more sexual and easier to anger (Abbey et al., 1999). And experimental work with men indicates that intoxicated men report greater intentions to react negatively, including angrily, to a woman’s insistence on condom use than do sober men (Davis, 2010). Both beliefs about drinking men and personal experience of intoxicated men’s behavior could lead a woman who perceived her male partner as intoxicated to anticipate a negative response to her refusal of unprotected sex.
Findings from alcohol administration experiments contribute mixed evidence regarding intoxication, perceptions of partner STI risk, and unprotected sex decisions. Participants in one study watched a film depicting hypothetical partners at different risk levels (Abbey, Saenz, Buck, Parkhill, & Hayman, 2006). Although intoxicated men and women did not differentiate between high and low STI risk partners, sober individuals reported they would be more likely to date the low risk partner. In a scenario study that manipulated partner risk level, intoxicated women appraised partners at all risk levels as having higher sexual potential than did sober women (Purdie et al., 2011). Such appraisals in turn predicted impelling cognitions about sex, which predicted less assertive condom requests and higher unprotected sex intentions. On the other hand, Murphy, Monahan, and Miller (1998) found that intoxication did not decrease women’s ability to perceive a partner’s STI risk cues in an experimental video. Other factors, like relationship context, may play an important role in women’s perceptions of their partners’ STI risk level.
Relationship Factors and Unprotected Sex
Relationship factors, broadly defined, affect many aspects of women’s responses in sexual encounters. A desire for a long-term relationship (Regan & Dreyer, 1999) and investment in relationship longevity (Rosenthal, Gifford, & Moore, 1998) have both been associated with unsafe sex. Women who reported higher emotional attachment, a relationship-related construct, were more likely to refrain from asking a partner to use a condom and to downplay his HIV risk (e.g., Clark, Miller, Harrison, Kay, & Moore, 1996).
There is also evidence that the effect of relationship factors on unprotected sex decisions may be mediated in part through a woman’s perceptions of her partner. Survey research has established that casual partners are generally perceived as higher in STI risk than are committed partners (for a review, see Misovich, Fisher, & Fisher, 1997). For example, Conley and Peplau (2010) examined perceptions of STI-risk-related factors (e.g., condom use, monogamy, having ever had an STI) and found that women underestimated the sexual risk posed by their steady romantic partners. These women perceived their boyfriends as lower risk than the men reported themselves to be; they also saw them as lower risk than college students overall. Such misperceptions of a man’s STI risk could lead women to have unprotected sex in relationships that were steady and romantic or seemed to have the potential to become so.
Present Study
Taken together, this empirical literature suggests that victimization history, intoxication, and the relationship potential of male partners affect women’s unprotected sex behavior. These factors seem likely to influence a woman’s sexual decision making through perceptions of her male partner – his intoxication, his STI risk, and his likelihood of reacting negatively to her refusal of unprotected sex. However, while all of these factors occur together naturalistically, no study has yet examined them in combination. The present study did so, evaluating interconnections among these variables in an experiment. Women’s sexual risk taking was operationalized as self-reported likelihood of engaging in unprotected sex and was examined using an eroticized sexual scenario. Alcohol intoxication was manipulated in the laboratory, and relationship potential was manipulated in the scenario.
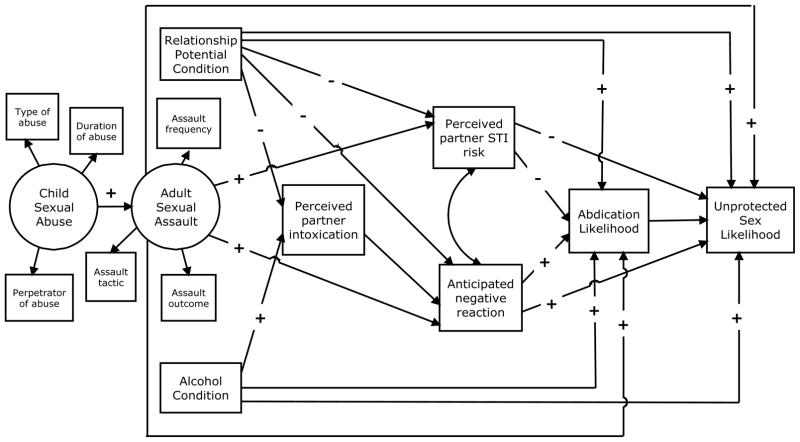
Based on previous research, we examined a model (Figure 1) testing whether previous victimization experiences, alcohol intoxication, and relationship potential would exert influences on women’s abdication of sexual decision-making and sexual risk-taking intentions and whether these influences would be mediated by their perceptions of the male scenario partner. The model included the empirically established path between CSA and ASA and tested three hypotheses: (1) ASA will predict greater likelihood of unprotected sex (a) directly, (b) indirectly via abdication (ceding the unprotected sex decision to the male partner), and (c) indirectly via partner perceptions; (2) acute alcohol intoxication will predict greater likelihood of unprotected sex (a) directly, (b) indirectly via abdication, and (c) indirectly via partner perceptions; (3) relationship potential will predict greater likelihood of unprotected sex (a) directly, such that a situation offering greater potential for a romantic relationship will foster a riskier sexual outcome, (b) indirectly via abdication, such that higher relationship potential will predict greater likelihood of ceding the unprotected sex decision to the male partner, and (c) indirectly via partner perceptions, such that higher relationship potential will predict lower perceptions of the partner’s intoxication, STI risk, and potential negative reaction to condom insistence.
Figure 1.
Hypothesized Model
Method
Data for this study were collected as part of a large-scale alcohol administration study that investigated multiple factors influencing women’s risky sex intentions. Other analyses drawing upon this dataset are reported elsewhere (author citation, under review).
Participants
Participants from an urban community were recruited with online and print advertisements seeking single female drinkers to participate in a research study on male-female social interactions. Eligible women were between the ages of 21 and 30 years and had at least one experience of heavy episodic drinking (4 or more drinks within two hours) and at least one instance of unprotected sex within the past year. Further eligibility criteria required at least one of the following HIV/STI risk factors: (a) new sex partner in the past year; (b) two or more sex partners in the past year; (c) having had an STI; or (d) knowing or suspecting that a past year sex partner had himself had a concurrent sexual relationship, an STI and/or HIV, a same-sex sexual encounter, ever used IV drugs, or been incarcerated in last 12 months. Exclusion criteria were based on the NIAAA’s guidelines for the ethical administration of alcohol to humans in research settings (2005). They included medical conditions or prescription medication use that contraindicated alcohol consumption and a history of problem drinking or negative reactions to alcohol, assessed during eligibility screening with the Brief Michigan Alcohol Screening Test (Pokorny, Miller, & Kaplan, 1972). Participants were paid $15 per hour; the range of compensation was approximately $45 to $150.
Four hundred forty-eight women participated in the study. Twelve women’s data were not included in the analysis sample: One participant’s data were lost due to a power outage, two received an experimental vignette that did not match their alcohol condition, four opted out of the study prior to receiving the experimental beverage, and five were excluded because they failed comprehension checks designed to assess the validity of the scenario. The final data set included 436 women; their demographic, victimization history, alcohol consumption, and sexual HIV-risk characteristics are presented in Table 1. Proportions of the sample belonging to each racial or ethnic group roughly matched those of the region in which the study was conducted.
Table 1.
Demographic, Victimization History, Alcohol Consumption, and Sexual HIV-risk Characteristics of Study Participants (n = 436)
| Demographic Characteristics
|
Proportion (n)
|
|---|---|
| Mean age | 24.8 (SD 2.6) |
| Race | |
| European American | 72.5 (313) |
| Multiracial/ Other | 14.8 (64) |
| African American | 5.8 (25) |
| Asian/ Pacific Islander | 6.0 (26) |
| Native American | 0.9 (4) |
| Hispanic/ Latina | 6.7 (29) |
| Employed full- or part-time | 58.6 (255) |
| Full- or part-time student | 34.4 (150) |
| Annual income < $40,999
|
73.7 (302) |
| Victimization History Characteristics
|
|
| No victimization | 15.6 (68) |
| Childhood sexual abuse (CSA) only | 3.9 (17) |
| Adult/ adolescent sexual assault (ASA) only | 52.3 (228) |
| CSA and ASA
|
28.2 (123) |
| Alcohol Consumption Characteristics
|
|
| Mean drinks per week | 14.0 (SD 8.0) |
| Binge drinking episode ≥1x/ month in past year
|
71.9 (316) |
| Sexual HIV-risk Characteristics
|
|
| Mean lifetime vaginal sex partners* | 14.8 (SD = 11.5) |
| Did not use condom at last intercourse | 59.6 (260) |
| Previous STI diagnosis | 35.6 (154) |
Note.
Capped at 50.
Procedures
When participants arrived at the laboratory, a trained female experimenter verified that their blood alcohol concentration (BAC) was 0.00% using a handheld breathalyzer (Alco-Sensor IV, Intoximeters, Inc.). Experimenters then reviewed an informed consent document – describing alcohol administration procedures, types of questions that would be asked, content of the scenario, and risks and benefits of participating – with each participant. Each participant was weighed to calculate her alcohol dose and took a urine test to ensure she was not pregnant. Participants completed computerized background questionnaires in a private room. These surveys included questions regarding sexual victimization in childhood and adulthood.
The computer calculated a code to assign participants to experimental conditions according to victimization history while keeping this information masked from the experimenter. Mutually exclusive groups were child sexual abuse only (CSA); adult sexual assault only (ASA); both (CSA-ASA); or no sexual victimization. For group assignment purposes, CSA was defined as having experienced any form of sexual contact before age 14. ASA was defined as having experienced sexual contact or attempted or completed oral, vaginal or anal penetration after turning 14 without her consent or when she was too intoxicated to stop what was happening. Finally, participants were block randomized into either the “high relationship potential” or “low relationship potential” experimental scenario condition, and to either a control (no alcohol, .00% BAC) or alcoholic (target peak BAC = .10%) beverage condition, to create a 2 x 2 (relationship potential by alcohol) design within each of the 4 victim groups (no victimization, n = 68 (15.6%); CSA only, n = 17 (3.9%); ASA only, n = 228 (52.3%); both CSA and ASA, n = 123(28.2%)).
Alcohol participants received a beverage consisting of cranberry juice and 190 proof grain alcohol in a 5 to 1 ratio, dosed at 1.0 ml per kg of body weight. Control participants drank an equivalent amount of cranberry juice. Participants in both groups were cognizant of whether they were receiving an alcoholic or non-alcoholic beverage. Beverages were divided into three equal portions and consumed over a period of 12 minutes. Breathalyzer tests occurred approximately every four minutes until a criterion BAC of .07 was reached. This procedure ensured that participants would be on the ascending limb of the blood alcohol curve for the presentation of the sexual scenario. To control for individual differences in speed of alcohol absorption, each control participant was yoked to an alcohol participant and provided the same number of breath samples over the same number of minutes before beginning the experimental scenario (Schacht, Stoner, George, & Norris, 2010). After reaching the criterion BAC (alcohol participants) or completing the yoked number of breathalyzers (controls), participants were left alone in the experiment room to read the experimental scenario.
The experimental sexual scenario was developed using data from focus groups on young women’s sexual relationship experiences, as well as the team’s previous research, and was pilot tested to ensure realism. Participants read the written scenario on a computer screen in a private room. The approximately 1600-word scenario was written in the second person (“you…”) to facilitate women’s projection into the storyline. For participants in alcohol condition, the protagonist drank alcohol; for those in the control condition, she drank soft drinks. The male character’s moderate drinking was constant across conditions.
The scenario established that the protagonist had previously had sex with the male character, Michael, that they had used a condom, and that she was on the pill (to eliminate pregnancy concerns associated with unprotected sex). Validity checks indicated that 97% of participants correctly perceived scenario condom use and 95%, scenario oral contraceptive use. She was very attracted to him, and her assessment of the relationship’s potential was varied according to experimental condition (e.g., in the low relationship potential condition “he may not really be your type” and “you’re uncertain whether there’s any future in this”, while in the high, he is “your type” and “you’re hopeful that there might be a future…”). Participants’ perception of the male partner’s relationship potential was assessed during the scenario; means in the low relationship potential condition were signficantly lower than those in the high relationship potential condition.
The characters went to dinner, then to Michael’s place where they began kissing and touching. Sexual activity became progressively more heated until both characters were undressed and approaching intercourse. Descriptions and dialogue were eroticized to increase the participant’s sexual arousal. Michael indicated that he would get a condom, but was unable to find one. The sexual activity continued. Finally, Michael said, “I really want to make love to you, but I’ll do whatever you want. Do we have to stop now?” Study participants rated the scenario as very realistic (M = 5.80, SD = 1.37; 1 “not at all realistic” to 7 “extremely realistic”).
Measures and Instruments
Childhood Sexual Abuse
Hulme’s Childhood Sexual Abuse (CSA) questionnaire is a retrospective behaviorally-specific measure of childhood sexual experiences (Hulme, 2007). Participants were provided with a list of 13 sexual acts and asked if any occurred when they were 13 years old or younger. Follow-up questions assessed specific details including relationship to the perpetrator and duration of abuse. We added an additional question: “How upsetting were these events for you at the time they occurred?” (1 = “not at all,” 7 = “extremely”). We also administered the Childhood Trauma Questionnaire (Bernstein et. al., 2003); two of its questions ask about being “sexually abused” and “molested” while growing up. The final definition of CSA includes childhood sexual experiences, prior to age 14, that involved a person 3 or more years older, or when involving a person of same age or only 1 or 2 years older, the participant reported (1) the use of coercion, threats, or force; (2) being upset at the time of the experience; (3) having been molested or sexually abused as a child; and (4) vaginal or anal penetration at an age prior to that identified by the participant as her age of first consensual sexual intercourse.
We modeled child sexual abuse as a latent variable in order to acknowledge the complexity of this phenomenon. Based on theoretical considerations and previous literature, we selected three indicators: type of abuse (no CSA = 1, contact = 2, or penetration = 3), duration of abuse (no CSA = 1, once = 2, less than 1 year = 3, one-to-two years = 4, two or more years = 5), and perpetrator of abuse (no CSA = 1, stranger/other = 2, acquaintance = 3, non-parent family member = 4, parent = 5).
Adolescent and Adult Sexual Assault Victimization
The revised Koss et al. (2007) Sexual Experiences Survey assesses unwanted and nonconsensual sexual experiences since age 14. Acts include sexual contact and oral, anal, and vaginal penetration by a penis or object. Tactics used to obtain each act include verbal coercion, incapacitation through alcohol or drugs, and physical force or threat of force. For each sexual act or attempted sexual act, participants reported the number of times they experienced each tactic with response options ranging from 0 “never” to 3 “3 or more times”. To acknowledge the complexity of sexual assault, we also modeled ASA as a latent variable. Indicators were 3 variables selected based on empirical and theoretical considerations: assault outcome (no ASA = 1, contact = 2, attempted rape = 3, completed rape = 4), assault tactic (no ASA = 1, coercion = 2, incapacitation = 3, force = 4), and penetrative assault frequency (number of completed penetrative assaults).
Partner Perceptions
We assessed women’s perceptions of the partner Michael’s level of intoxication, his STI risk, and his negative reaction to their refusal of sex without a condom. Perceived partner intoxication was measured with the item “how intoxicated do you think Michael is at this point?” asked after the couple had returned to his apartment, but prior to the commencement of sexual activity. Response options ranged from 1 “not at all intoxicated” to 7 “extremely intoxicated.” Perceived STI risk was operationalized as the mean of two correlated items (r = .39). The first item was “how much of the time do you think Michael uses a condom?” (1 = “never,” 2 = “almost never,” 3 = “less than half the time,” 4 = “about half the time,” 5 = “more than half the time,” 6 = “almost all the time,” 7 = “all of the time”), reversed scored such that a high score was equivalent to high perceived riskiness. The second item was “how likely is it that Michael has an STD?” with response options ranging from 1 “not at all likely” to 7 “extremely likely.” Women’s anticipation of a negative reaction to refusal of sex without a condom was measured with a 5-item scale with an alpha of .80 (adapted from Wingood & DiClemente, 1997). The stem for these items was “If you refuse to have sex without a condom, how likely is Michael to…” and they continued with “try to persuade you to have sex without a condom,” “lose interest in you,” “end the evening,” “become angry with you,” and “force you to have sex anyway.” Again, response options ranged from 1 “not at all likely” to 7 “extremely likely.” Both STI risk and anticipated negative reaction questions were asked at the end of the scenario before the abdication and likelihood of unprotected sex questions.
Abdication
Abdication of sexual decision-making was measured with one question at the end of the scenario, which asked “how likely are you to let Michael decide how far to go sexually?” Response options ranged from 1 “not at all likely” to 7 “extremely likely.”
Likelihood of Unprotected Sex
A likelihood of unprotected sex scale was created by taking the mean of three items, “How likely are you to: rub your clitoris against Michael’s penis,” “have vaginal sex without a condom,” and “let Michael put his penis inside of your vagina but only if he pulls out before ejaculating.” Both these items and the abdication item above have been used in previous research on sexual decision-making (e.g., George et al., 2009; Stoner et al., 2008). Response options ranged from 1 “not at all likely” to 7 “extremely likely.” These three items had an alpha of .89.
Analytic Approach
We used structural equation modeling (SEM) to test the theoretical model in Figure 1, which represents all of the hypothesized relationships among variables, using Mplus statistical modeling software for Windows, version 6 (Muthén & Muthén, 2010). Perceived partner STI risk and anticipated negative reaction were allowed to intercorrelate. We screened data for outliers, skewness, kurtosis, and missingness. Only ASA frequency deviated from normality; because the number of times women experienced unwanted completed penetrative acts was significantly skewed and kurtotic, we capped this variable at 9 to address distributional issues. Our estimation method was maximum likelihood with robust standard errors, and we employed full information maximum likelihood (FIML), standard with Mplus, to handle rare instances of missing data.
Results
Preliminary Analyses
Bivariate correlations among the variables in the model, as well as their means and standard deviations, appear in Table 2. Severity of CSA type, duration of CSA, and relationship to the perpetrator were all significantly associated with perceiving the scenario partner being at higher risk of STIs. Experiencing violent sexual assault in adolescence or adulthood was significantly associated both with increased perception of the scenario partner’s STI risk and with anticipation of a more negative reaction from him to refusal of sex without a condom. Number of adolescent or adult assaults was significantly associated with increased perception of the scenario partner’s STI risk. Scenario partner’s perceived STI risk was associated with both less abdication of sexual decision-making and lower likelihood of unprotected sex, and abdication and unprotected sex were positively associated.
Table 2.
Means, Standard Deviations, and Bivariate Correlations Among Model Variables (N = 436)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CSA type | — | .81** | .85** | .19** | .18** | .24** | .00 | −.03 | .05 | .13** | .04 | −.01 | .01 |
| 2. CSA duration | — | .83** | .17** | .17** | .19** | .02 | .01 | .07 | .16** | .06 | .00 | −.04 | |
| 3. CSA perpetrator | — | .16** | .17** | .15** | −.01 | −.02 | .07 | .19** | .07 | −.01 | −.03 | ||
| 4. ASA outcome | — | .83** | .61** | −.02 | .02 | .00 | .08 | .09 | .06 | .06 | |||
| 5. ASA tactic | — | .53** | .04 | .01 | .03 | .10* | .14** | .00 | .00 | ||||
| 6. ASA frequency | — | −.01 | .02 | −.01 | −.01 | .05 | .07 | .09 | |||||
| 7. Alcohol condition | — | .02 | .51** | .05 | .10* | .09 | .05 | ||||||
| 8. Relationship potential condition | — | −.08 | −.05 | −.09 | .06 | −.03 | |||||||
| 9. Perceived partner intoxication | — | .04 | .13** | .02 | −.01 | ||||||||
| 10. Perceived partner STI risk | — | .30** | −.22** | −.31** | |||||||||
| 11. Anticipated negative reaction | — | .10** | .03 | ||||||||||
| 12. Abdication likelihood | — | .61** | |||||||||||
| 13. Unprotected sex likelihood | — | ||||||||||||
|
| |||||||||||||
| Mean | 1.52 | 1.69 | 1.72 | 3.16 | 2.86 | 2.24 | n/a | n/a | 3.38 | 3.93 | 3.47 | 3.29 | 3.90 |
| SD | .80 | 1.27 | 1.19 | 1.20 | 1.09 | 2.56 | n/a | n/a | 1.38 | 1.08 | 1.24 | 1.78 | 1.93 |
Note.
p < .05.
p < .01.
Model Specification and Re-specification
The hypothesized model, including participant background variables and variables manipulated in the laboratory, is shown in Figure 1. This model fit the data acceptably (χ2 (49) = 65.51, p = .058; RMSEA (root mean square error of approximation) = .028; CFI (comparative fit index) = .992; SRMR (standardized root mean squared residual) = .034) and accounted for 41% of the variance in unprotected sex likelihood. Indicator variables’ loadings onto latent constructs were substantial, significant, and in the expected direction. However, inspection of the modification indices suggested that the effects of CSA on perception of partner STI risk were not fully mediated by ASA, and that adding a direct path between CSA and perception of partner STI risk would improve model fit. This re-specified model was a good fit (χ2 (50) = 57.10, p = .228; RMSEA = .018; CFI = .997; SRMR = .026) and continued to account for 41% of the observed variance in unprotected sex intention. A statistically non-significant chi-square difference test indicated that the fit of the two models was statistically equivalent, so we selected the re-specified model depicted in Figure 2 based on both fit and theoretical criteria.
Figure 2.
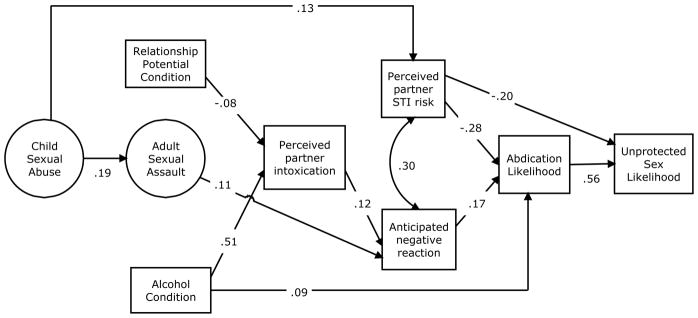
Final Model Depicting Significant Paths and Standardized Coefficients
Note. Only paths significantly different from zero (p < .05) are shown in the figure, however, all paths in the hypothesized model were retained in the final model.
Direct and Indirect Effects
Figure 2 depicts the final model and displays standardized coefficients for significant paths; standardized estimates for all paths modeled appear in Table 3. Women with a more severe history of childhood victimization viewed Michael as a high STI risk. Women with more severe histories of adult victimization anticipated stronger negative reactions from him to their refusal of unsafe sex. Intoxicated women perceived the scenario partner as more intoxicated, and they were also more likely to abdicate their decision and allow him to choose how far to go sexually. High relationship potential was associated with lower levels of perceived partner intoxication, and women who perceived Michael as less intoxicated were less likely to anticipate a negative reaction from him. The more strongly women anticipated a negative reaction from the scenario partner, the more likely they were to abdicate sexual decision-making. As women perceived the partner as being a higher risk for STIs, they were less likely both to abdicate and to intend to engage in unprotected sex. The largest relationship seen was between abdication and unprotected sex intention; women who expressed higher likelihood of letting the scenario partner decide how far to go sexually were much more likely to intend to have unprotected sex. We also tested the significance of specific and total indirect effects of CSA, ASA, alcohol, and relationship potential on unprotected sex likelihood; these results are summarized below.
Table 3.
Standardized Estimates of All Paths in Final Model
| Standardized estimate | SE | p-value | |
|---|---|---|---|
| Childhood Sexual Abuse by | |||
| Type | .946*** | .013 | .000 |
| Duration | .877*** | .016 | .000 |
| Perpetrator | .931*** | .015 | .000 |
| Adult/adolescent Sexual Assault by | |||
| Outcome | .965*** | .019 | .000 |
| Tactic | .855*** | .025 | .000 |
| Frequency | .629*** | .017 | .000 |
| CSA on ASA | .189*** | .046 | .000 |
| Perceived Partner Intoxication on | |||
| Alcohol Condition | .509*** | .035 | .000 |
| Relationship Potential Condition | −.084* | .041 | .040 |
| Perceived Partner STI Risk on | |||
| CSA | .127** | .050 | .010 |
| ASA | .071 | .052 | .170 |
| Relationship Potential Condition | −.044 | .048 | .352 |
| Anticipated Negative Partner Reaction on | |||
| ASA | .11* | .053 | .034 |
| Perceived Partner Intoxication | .115* | .048 | .016 |
| Relationship Potential Condition | −.080 | .047 | .089 |
| Perceived Partner STI Risk with | |||
| Anticipated Negative Partner Reaction | .296*** | .053 | .000 |
| Abdication Likelihood on | |||
| ASA | .054 | .047 | .254 |
| Alcohol Condition | .093* | .046 | .044 |
| Relationship Potential Condition | .051 | .046 | .270 |
| Perceived Partner STI Risk | −.282*** | .050 | .000 |
| Anticipated Negative Partner Reaction | .166** | .056 | .003 |
| Unprotected Sex Likelihood on | |||
| ASA | .031 | .037 | .394 |
| Alcohol Condition | .007 | .037 | .857 |
| Relationship Potential Condition | −.056 | .037 | .133 |
| Perceived Partner STI Risk | −.197*** | .046 | .000 |
| Anticipated Negative Partner Reaction | .027 | .048 | .571 |
| Abdication Likelihood | .563*** | .040 | .000 |
Note.
p < .05.
p < .01.
p < .001.
Victimization hypotheses
As has been established in previous research, CSA was associated with ASA. Furthermore, once the model was re-specified, we also saw a significant but non-hypothesized positive relationship between CSA and perceived partner STI risk. CSA was associated with lower likelihood of unprotected sex both via perceived partner STI risk (standardized estimate = −.025, SE .011, p = .020) and through a similar significant indirect path via perceived partner STI risk and abdication (standardized estimate = −.020, SE .009, p = .030).
Our hypothesis (1a) regarding ASA’s direct effects on unprotected sex was not supported. However, although this total indirect effect only approached significance, ASA had an indirect effect (standardized estimate = .010, SE .009, p = .080) on unprotected sex via anticipated negative reaction and abdication (hypotheses 1b and 1c).
Alcohol hypotheses
Our hypotheses that acute alcohol intoxication would predict greater sexual risk taking both directly (2a), and indirectly via the mediating effects of partner perceptions (2c), were not supported; the total indirect path from alcohol to unprotected sex intentions via perceived partner intoxication, anticipated negative response, and abdication was not significant. However, in accordance with hypothesis 2b, alcohol did predict unprotected sex likelihood indirectly via its effect on abdication (standardized estimate = .052, SE .026, p = .042).
Relationship potential hypotheses
Although relationship potential was associated with lower perceived partner intoxication, none of our hypotheses (3a, b, and c) about its direct and indirect effects on unprotected sex likelihood were supported.
Discussion
This study tested whether previous sexual victimization experiences, alcohol intoxication, and relationship potential would influence women’s abdication of sexual decision-making and their sexual risk-taking intentions, and whether these influences would be mediated by their perceptions of a male partner. Three key findings emerged. First, CSA predicted higher perception of partner STI risk, which in turn predicted lower unprotected sex likelihood. Second, ASA was associated with anticipating a negative partner reaction to condom insistence; and this anticipation was, in turn, associated with greater likelihood of unprotected sex indirectly via abdication (although the test of this total indirect effect only approached significance). Third, alcohol’s association with higher unprotected sex likelihood acted indirectly through abdication; intoxicated women were more likely than sober women to allow the male partner to decide how far to go sexually, and this abdication in turn was strongly associated with greater likelihood of unprotected sex. Generally, these findings advance as well as complicate our understanding of the associations between previous sexual victimization and unprotected sex, and they cohere with established experimental findings regarding the relationship between alcohol and unprotected sex.
Sexual Victimization Influences Women’s Perceptions of Male Partners
Our results indicate that a history of sexual victimization can change women’s responses in sexual situations. CSA was positively associated with women’s likelihood of perceiving a male partner as at higher risk of having an STI. This perception may originate in negative early experiences of men and sex that forge links in victimized women’s minds between male sex partners and danger, threat, or risk. If a child victim contracted an STI or experienced other genital discomfort as a result of abuse, she might be more likely to grow up into a woman prone to see male partners or sex itself as a source of distress or as “unclean.” The perception may also stem from women’s adult experiences. Since women with a history of CSA tend to have more lifetime sexual partners than non-victimized women (Lalor & McElvaney, 2010; Malow, Devieux, & Lucenko, 2006), they are more likely to have been exposed to an STI and to have had one themselves. Perception of a partner as a higher STI risk, whether based on trauma history or accurate in the present, was associated with a woman’s likelihood of having unprotected sex in two ways. It directly and negatively predicted her intention to have unprotected sex, and it also negatively predicted that she would allow her partner to decide how far to go sexually, which in turn predicted her intention to have unprotected sex.
The finding that CSA is associated with a decrease in unprotected sex intentions as a result of perceiving the male partner as at high STI risk is in contrast to previous work linking CSA with increased unprotected sex in adult life (Lalor & McElvaney, 2010; Malow, Devieux, & Lucenko, 2006), however, the direct path between CSA and unprotected sex was not tested in the current study. It suggests that a history of CSA may exert some protective influence in certain sexual situations, such that a woman with a CSA history may be likely to see a male partner as a high risk for STI transmission, and to rationally respond with a lower likelihood of having unprotected sex with him, at least in an experimental scenario. The novelty of this finding means that its implications should be considered with caution. However, whether women’s perception of a partner as high risk for STIs stems from a CSA history or not, this perception can shape their intended behavior. Thus, one non-controversial implication is that health care providers may be able to use accurate information about the STI transmission risk men can pose to women as a way to reduce women’s likelihood of unprotected sex.
Our second finding regarding victimization history, while necessarily tentative due to the marginal statistical significance of the total indirect path, was that sexual victimization in adulthood can increase a woman’s anticipation of a negative response from a partner to insistence on condom use, which increases her likelihood of abdicating sexual decision making and having unprotected sex. In this study’s experimental scenario, there was no suggestion that the male character would react to condom insistence or sexual refusal in an angry, violent, or otherwise negative way. He was portrayed as attractive and a “good guy.” Nonetheless, more severely ASA-victimized women were inclined to view a negative reaction as more likely and to leave the sexual decision up to the male scenario partner, which in turn increased their likelihood of endorsing unprotected sex with him. This finding coheres with past work documenting a connection between sexual assault history in adulthood and unprotected sex (Davis et al., 2002; Molitor et al., 2000). It suggests that one route from ASA to unprotected sex is fear of men’s negative reactions to condom insistence. If a woman’s sexual assertiveness has been met with male violence, coercion, or anger in the past, her current abdication makes sense as a way to protect herself from proximal aggressive consequences, even if she is well aware it makes her more likely to suffer distal consequences. In the moment, fear of being raped or coerced (or yelled at, shamed, or rejected) may be far more salient than the possibility of contracting an STI in the future.
Women who have experienced sexual assault have good reason to believe that their efforts to make and enforce decisions about sexual behavior will be met with male push-back. This opinion, while understandable, may persist even in situations where a male partner’s reaction is not yet known. It may lead to women eschewing insistence on condom use, or even making condom requests, at times when male partners would comply or could be persuaded. As such, women’s anticipation of negative partner responses could offer a useful intervention target. Focused feedback on the genuine interest some men have in safer sex, social and relational skills training to increase women’s chances of identifying such men and choosing them as sex partners, and support for communicating condom requests frankly without assuming all men will respond negatively, are messages these findings suggest might be effective.
Abdicating Sexual Decision-Making: Alcohol’s Role
Our third key finding was that abdication is a major gateway to sexual risk. All the variables in the model influenced unprotected sex intention through abdication. Our findings strongly suggest that if a woman cedes decision making in a sexual situation, she is more likely to proceed with unprotected sex. The connection between abdication and sexual risk-taking is particularly critical because most women live their lives in a social context that downplays their sexual agency and emphasizes men as sexual decision-makers (Gavey, 2005). Letting a male partner decide what to do in terms of going ahead with sex without a condom may seem quite natural and normal in this context. However, doing so also puts women at higher risk of all the negative consequences of unprotected sex.
Consistent with previous research (George et al., 2009; Schacht et al., 2010), alcohol intoxication acted to increase the likelihood of unprotected sex in the scenario, doing so in this case by increasing women’s abdication of sexual decision-making. Zawacki and her colleagues investigated interactions among women’s relationship motivation, familiarity with a male partner, and intoxication (Zawacki et al., 2009). In their model, the interaction of these three factors had a significant indirect effect on abdication, and abdication was associated with unprotected sex intention, as it was in the current study. However, by testing the specific path between alcohol condition and abdication likelihood rather than a complex interaction, our study clarifies the link between alcohol intoxication and abdication, and in turn, unprotected sex intention. Alcohol may make a woman more likely to leave decisions about unprotected sex up to her male partner in several ways. It may serve to focus a woman’s attention on immediate impelling cues such as her own sexual arousal and that of her partner, while reducing her attention to inhibitory cues such as the risk of STIs (alcohol myopia theory: Steele & Josephs, 1990; Taylor & Leonard, 1983).
Alcohol may also act on women’s sexual decision making through its expectancy effects (George & Stoner, 2000), specifically the belief that alcohol makes both men and women more sexual. Since mainstream sexual scripts assign men to more active and women to more passive sexual roles (Dworkin & O’Sullivan, 2005; Gagnon, 1990; Masters, Casey, Wells, & Morrison, 2012), many women may act upon alcohol-enhanced sexual focus by leaving the decision up to the man and allowing sex to happen.
These findings about the abdication of sexual decision making and alcohol’s role in making it more likely have implications for interventions to decrease unprotected sex. Existing programs that support assertive decision making and communication about sex, such as those aiming to increase women’s sexual assault resistance skills, may also be effective at increasing women’s sexual agency in consensual situations. Sexuality education, both formal in-school programs and informal family communications, could inculcate more gender equitable ideas about sexual decision making in young people of both sexes in order to counter the mainstream sexual script that contributes to women’s abdication likelihood. This evidence suggesting that alcohol intoxication makes abdication more likely, and that abdication in turn can lead to greater likelihood of unprotected sex, could be an important addition to both types of interventions.
Strengths and Limitations
The present study has both strengths and limitations. Strengths include modeling sexual victimization with latent variables, rigorous management of alcohol intoxication, a realistic and immersive experimental scenario, and a community sample. Characterizing both CSA and ASA with multiple indicators begins to represent the complexity of victimization severity more fully than doing so with single-item or dichotomous variables. Aspects of alcohol intoxication were controlled through procedures involving consistent BAC monitoring, specific BAC criterion starting points, and yoked controls. The erotic quality of the experimental scenario created an ambiance during the decision-making process that approximated a real-world sexual situation. Our sampling of predominantly urban community residents strengthened the study by diversifying the participants beyond clinical and college samples.
Limitations include aspects of the experimental scenario, general limitations of experimental procedures, the possibility of volunteer bias, and specific characteristics of our sample. Creating a realistic scenario for the experiment required specificity about details, such as how many times the couple had had sex before, but providing these details means that women’s reactions and decisions might be different outside this specific hypothetical context. Experimental procedures that use laboratory analogues of sexual situations can never capture all elements of real sexual situations. Volunteers for sexuality research tend to have more liberal sexual attitudes and more sexual experience than non-volunteers (Strassberg & Lowe, 1995). Although our community sample avoided the problems associated with college samples (e.g., under-representation of racial and ethnic minority participants), its characteristics limit the generalizability of our findings in several ways. Since the experiment involved alcohol administration, ethical concerns precluded the participation of abstainers, light drinkers, and problem drinkers. Only non-problem drinkers with fairly recent heavy episodic drinking experience were included. Because our alcohol administration paradigm required participants to be of legal drinking age (21 and over), current findings may not generalize to underage drinking women. Similarly, both the requirement that participants have some HIV/STI risk factors, and the high rates of sexual victimization among participants, limit generalizability. Summing up, because the alcohol consumption patterns, sexual risk indicators, and sexual victimization histories of this study’s sample are high relative to the general population, care must be taken when generalizing current findings to other groups of women. That noted, the participants in this study were recruited due to their elevated risk levels, and this vulnerability makes them an important focus of research on these topics.
Conclusion
This study’s combination of survey and experimental methods allowed us to integrate distal and proximal factors into our model to better understand their mutual influence on processes leading to sexual risk. Its findings suggest three potential ways to decrease women’s likelihood of unprotected sex. The first way is increasing women’s accurate perceptions of partners’ STI risk. The second way is increasing women’s confidence about condom insistence as well as their ability to react to realistic fear of a particular man’s potentially violent or coercive reaction to such insistence. The third way is enhancing their sexual agency in order to steer them away from abdication (under the influence of alcohol or otherwise) and toward making affirmative decisions in their own sexual self-interest.
Acknowledgments
Funding:
This research was supported by a grantfrom the National Institute on Alcohol Abuse and Alcoholism(R01 AA016281-01A2) to William H. George.
References
- Abbey A, McAuslan P, Ross LT, Zawacki T. Alcohol expectancies regarding sex, aggression, and sexual vulnerability: Reliability and validity assessment. Psychology of Addictive Behaviors. 1999;13(3):174–182. doi: 10.1037//0893-164X.13.3.174. [DOI] [Google Scholar]
- Abbey A, Saenz C, Buck PO, Parkhill MR, Hayman LW. The effects of acute alcohol consumption, cognitive reserve, partner risk, and gender on sexual decision making. Journal of Studies on Alcohol. 2006;67:113–121. doi: 10.15288/jsa.2006.67.113. Retrieved from http://www.jsad.com/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arriola KRJ, Louden T, Doldren MA, Fortenberry RM. A meta-analysis of the relationship of child sexual abuse to HIV risk behavior among women. Child Abuse and Neglect. 2005;29(6):725–746. doi: 10.1016/j.chiabu.2004.10.014. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Brener ND, McMahon PM, Warren CW, Douglas KA. Forced sexual intercourse and associated health risk behaviors among female college students in the United States. Journal of Consulting and Clinical Psychology. 1999;67:252–259. doi: 10.1037//0022-006x.67.2.252. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2010. Atlanta, GA: U.S. Department of Health and Human Services; 2011. Retrieved from http://www.cdc.gov/std/stats10/surv2010.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. HIV surveillance report, 2010. Vol. 22. Atlanta, GA: U.S. Department of Health and Human Services; 2012. Retrieved from http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/index.htm. [Google Scholar]
- Clark LF, Miller KS, Harrison JS, Kay KL, Moore J. The role of attraction in partner assessments and heterosexual risk for HIV. In: Oskamp S, Thompson SC, editors. Understanding and preventing HIV risk behavior: Safer sex and drug use. Thousand Oaks, CA: Sage Publications; 1996. pp. 80–99. [Google Scholar]
- Conley TD, Peplau LA. Gender and perceptions of romantic partners’ sexual risk. Journal of Sexual Medicine. 2010;7:794–802. doi: 10.1111/j.1743-6109.2009.01598.x. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol. 2002;14:101–117. doi: 10.15288/jsas.2002.s14.101. Retrieved from http://www.jsad.com/ [DOI] [PubMed] [Google Scholar]
- Cooper ML. Toward a person x situation model of sexual risk-taking behaviors: Illuminating the conditional effects of traits across sexual situations and relationship contexts. Journal of Personality and Social Psychology. 2010;98(2):319–341. doi: 10.1037/a0017785. [DOI] [PubMed] [Google Scholar]
- Davis KC. The influence of alcohol expectancies and intoxication on men’s aggressive unprotected sexual intentions. Experimental and Clinical Psychopharmacology. 2010;18(5):418–428. doi: 10.1037/a0020510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis KC, George WH, Norris J. Women’s responses to unwanted sexual advances: The role of alcohol and inhibition conflict. Psychology of Women Quarterly. 2004;28 (4):333–343. doi: 10.1111/j.1471-6402.2004.00150. [DOI] [Google Scholar]
- Davis JL, Combs-Lane AM, Jackson TL. Risky behaviors associated with interpersonal victimization. Journal of Interpersonal Violence. 2002;17(6):611–629. doi: 10.1177/0886260502017006002. [DOI] [Google Scholar]
- Dworkin SL, O’Sullivan L. Actual versus desired initiation patterns among a sample of college men: Tapping disjunctures within traditional male scripts. Journal of Sex Research. 2005;42(2):150–158. doi: 10.1080/00224490509552268. [DOI] [PubMed] [Google Scholar]
- Gagnon JH. The explicit and implicit use of the scripting perspective in sex research. Annual Review of Sex Research. 1990;1:1–43. [Google Scholar]
- Gavey N. Just sex? The cultural scaffolding of rape. New York, NY: Routledge; 2005. [Google Scholar]
- George WH, Davis KC, Norris J, Heiman JR, Stoner SA, Schacht RL, Kajumulo KF. Indirect effects of acute alcohol intoxication on sexual risk-taking: The roles of subjective and physiological sexual arousal. Archives of Sexual Behavior. 2009;38(4):498–513. doi: 10.1007/s10508-008-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George WH, Lehman GL, Cue KL, Martinez LJ, Lopez PA, Norris J. Postdrinking sexual inferences: Evidence for linear rather than curvilinear dosage effects. Journal of Applied Social Psychology. 1997;27(7):629–648. doi: 10.1111/j.1559-1816.1997.tb00652.x. [DOI] [Google Scholar]
- George WH, Stoner SA. Understanding acute alcohol effects on sexual behavior. Annual Review of Sexual Research. 2000;11:92–124. Retrieved from http://dionysus.psych.wisc.edu/lit/articles/GeorgeW2000a.pdf. [PubMed] [Google Scholar]
- Hendershot CS, George WH. Alcohol and sexuality research in the AIDS era: Trends in publication activity, target populations and research design. AIDS and Behavior. 2007;11(2):227–237. doi: 10.1007/s10461-006-9130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulme PA. Psychometric evaluation and comparison of three retrospective, multi-item measures of childhood sexual abuse. Journal of Child Abuse & Neglect. 2007;31(8):853–869. doi: 10.1016/j.chiabu.2007.03.016. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: An epidemiological and Cotwin control analysis. Archives of General Psychiatry. 2000;57(10):953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Koss MP, Abbey A, Campbell R, Cook S, Norris J, Testa M, White J. Revising the SES: A collaborative process to improve assessment of sexual aggression and victimization. Psychology of Women Quarterly. 2007;31(4):357–370. doi: 10.1111/j.1471-6402.2007.00385.x. [DOI] [Google Scholar]
- Lalor K, McElvaney R. Child sexual abuse, links to later sexual exploitation/high-risk sexual behavior, and prevention/treatment programs. Trauma, Violence, & Abuse. 2010;11:159–177. doi: 10.1177/1524838010378299. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Vanslyke JG, Hoppe MJ, Rainey DT, Morrison DM, Gillmore MR. Drinking and condom use: Results from an event-based daily diary. AIDS and Behavior. 2008;12:104–112. doi: 10.1007/s10461-007-9216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL. Effects of alcohol and expectancies on HIV-related risk perception and behavioral skills in heterosexual women. Experimental and Clinical Psychopharmacology. 2004;12(4):288–297. doi: 10.1037/1064-1297.12.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malow RM, Devieux JG, Lucenko B. History of childhood sexual abuse as a risk factor for HIV risk behavior. Journal of Trauma Practice. 2006;5(3):13–32. doi: 10.1300/J189v05n03_02. [DOI] [Google Scholar]
- Masters NT, Casey E, Wells EA, Morrison DM. Sexual scripts among young heterosexually active men and women: Continuity and change. Journal of Sex Research. 2012 doi: 10.1080/00224499.2012.661102. Early publication online at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore T, Long P. The role of childhood sexual abuse sequelae in the sexual revictimization of women: An empirical review and theoretical reformulation. Clinical Psychology Review. 2003;23(4):537–571. doi: 10.1016/S0272-7358(02)00203-9. [DOI] [PubMed] [Google Scholar]
- Misovich SJ, Fisher JD, Fisher WA. Close relationships and elevated HIV risk behavior: Evidence and possible underlying psychological processes. Review of General Psychology. 1997;1:72–107. doi: 10.1037//1089-2680.1.1.72. [DOI] [Google Scholar]
- Molitor F, Ruiz JD, Klausner JD, McFarland W. History of forced sex in association with drug use and sexual HIV risk behaviors, infection with STDs, and diagnostic medical care: Results from the Young Women Survey. Journal of Interpersonal Violence. 2000;15(3):262–278. doi: 10.1177/088626000015003003. [DOI] [Google Scholar]
- Murphy ST, Monahan JL, Miller LC. Inference under the influence: The impact of alcohol and inhibition conflict on women's sexual decision making. Personality and Social Psychology Bulletin. 1998;24(5):517–528. doi: 10.1177/0146167298245007. [DOI] [Google Scholar]
- Muthén LK, Muthén BO. Mplus Users Guide. Los Angeles, CA: Muthén & Muthén; 2010. Retrieved from http://www.statmodel.com/download/usersguide/Mplus%20Users%20Guide%20v6.pdf. [Google Scholar]
- National Advisory Council on Alcohol Abuse and Alcoholism. Recommended council guidelines on ethyl alcohol administration in human experimentation. 2005 Available on the National Institute on Alcohol Abuse and Alcoholism website at http://www.niaaa.nih.gov/research/guidelines-and-resources/administering-alcohol-human-studies.
- Norris J, George WH, Stoner SA, Masters NT, Zawacki T, Davis KC. Women's responses to sexual aggression: The effects of childhood trauma, alcohol, and prior relationship. Experimental and Clinical Psychopharmacology. 2006;14(3):402–411. doi: 10.1037/1064-1297.14.3.402. [DOI] [PubMed] [Google Scholar]
- Pokorny A, Miller B, Kaplan H. The brief MAST: A shortened version of the Michigan Alcoholism Screening Test. American Journal of Psychiatry. 1972;129(3):342–345. doi: 10.1176/ajp.129.3.342. Retrieved from http://ajp.psychiatryonline.org/ [DOI] [PubMed] [Google Scholar]
- Purdie MP, Norris J, Davis KC, Zawacki T, Morrison DM, George WH, Kiekel PA. The effects of acute alcohol intoxication, partner risk level, and general intention to have unprotected sex on women’s sexual decision making with a new partner. Experimental and Clinical Psychopharmacology. 2011;19(5):378–388. doi: 10.1037/a0024792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quina K, Harlow LL, Morokoff PJ, Burkholder G, Deiter PJ. Sexual communication in relationships: When words speak louder than actions. Sex Roles. 2000;42(7–8):523–549. doi: 10.1023/A:1007043205155. [DOI] [Google Scholar]
- Quina K, Morokoff PJ, Harlow LL, Zurbriggen EL. Cognitive and attitudinal paths from childhood trauma to adult HIV risk. In: Koenig L, Doll L, O’Leary A, Pequegnat W, editors. From child sexual abuse to adult sexual risk: Trauma, revictimization, and intervention. Washington, DC: American Psychological Association; 2004. pp. 117–134. [Google Scholar]
- Regan PC, Dreyer CS. Lust? Love? Status? Young adults’ motives for engaging in casual sex. Journal of Psychology & Human Sexuality. 1999;11:1–24. doi: 10.1300/J056v11n01_01. [DOI] [Google Scholar]
- Rosenthal D, Gifford S, Moore S. Safe sex or safe love: Competing discourses? AIDS Care. 1998;10:35–47. doi: 10.1080/09540129850124569. [DOI] [PubMed] [Google Scholar]
- Schacht RL, George WH, Davis KC, Heiman JR, Norris J, Stoner SA, Kajumulo KF. Sexual abuse history, alcohol intoxication, and women’s sexual risk behavior. Archives of Sexual Behavior. 2010;39(4):898–906. doi: 10.1007/s10508-009-9544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schacht RL, Stoner SA, George WH, Norris J. Idiographically-determined versus standard absorption periods in alcohol administration studies. Alcoholism: Clinical and Experimental Research. 2010;34(5):925–927. doi: 10.1111/j.1530-0277.2010.01165.x,10.1007/s10508-009-9544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DW, Davis JL, Fricker-Elhai AE. How does trauma beget trauma? Cognitions about risk in women with abuse histories. Child Maltreatment. 2004;9(3):292–303. doi: 10.1177/1077559504266524. [DOI] [PubMed] [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. American Psychologist. 1990;45(8):921–933. doi: 10.1037/0003-066X.45.8.921. [DOI] [PubMed] [Google Scholar]
- Stoner SA, Norris J, George WH, Davis KC, Masters NT, Hessler DM. Effects of alcohol intoxication and victimization history on women’s sexual assault resistance intentions: The role of secondary cognitive appraisals. Psychology of Women Quarterly. 2007;31(4):344–356. doi: 10.1111/j.1471-6402.2007.00384.x. [DOI] [Google Scholar]
- Stoner SA, Norris J, George WH, Morrison DM, Zawacki T, Davis KC, Hessler DM. Women’s condom use assertiveness and sexual risk-taking: Effects of alcohol intoxication and adult victimization. Addictive Behaviors. 2008;33(9):1167–1176. doi: 10.1016/j.addbeh.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strassberg DS, Lowe K. Volunteer bias in sexuality research. Archives of Sexual Behavior. 1995;24:369–382. doi: 10.1007/BF01541853. [DOI] [PubMed] [Google Scholar]
- Taylor SP, Leonard KE. Alcohol and human aggression. In: Geen RG, Donnerstein EI, editors. Aggression: Theoretical and Empirical Reviews. New York, NY: Academic Press; 1983. pp. 77–102. [Google Scholar]
- Tjaden P, Thoennes N. Extent, nature, and consequences of rape victimization: Findings from the National Violence Against Women Survey (NCJ 210346) Washington, DC: US Department of Justice; 2006. Jan, Retrieved from http://www.ncjrs.gov/pdffiles1/nij/210346.pdf. [Google Scholar]
- Wingood GM, DiClemente RJ. Child sexual abuse, HIV sexual risk, and gender relations of African-American women. American Journal of Preventive Medicine. 1997;13(5):380–384. Retrieved from http://www.ajpmonline.org/ [PubMed] [Google Scholar]
- Zawacki T, Norris J, Hessler DM, Morrison DM, Stoner SA, George WH, Abdallah DA. Effects of alcohol, partner familiarity, and relationship motivation on women's risky sexual decision making. Personality and Social Psychology Bulletin. 2009;35(6):723–736. doi: 10.1177/0146167209333043. [DOI] [PMC free article] [PubMed] [Google Scholar]