Abstract
Purpose
When barcode medication administration (BCMA) is implemented nurses are required to integrate not only a new set of procedures or artifacts into everyday work, but also an orientation to medication safety itself that is sometimes at odds with their own. This paper describes how the nurses’ orientation (the Practice Frame) can collide with the orientation that is represented by the technology and its implementation (the System Frame), resulting in adaptations at the individual and organization levels.
Methods
The paper draws on two qualitative research studies that examined the implementation of BCMA in inpatient settings using observation and ethnographic fieldwork, content analysis of email communications, and interviews with healthcare professionals.
Results
Two frames of reference are described: the System Frame and the Practice Frame. We found collisions of these frames that prompted adaptations at the individual and organization levels. The System Frame was less integrated and flexible than the Practice Frame, less able to account for all of the dimensions of everyday patient care to which medication administration is tied.
Conclusion
Collisions in frames during implementation of new technology result in adaptations at the individual and organization level that can have a variety of effects. We found adaptations to be a means of evolving both the work routines and the technology. Understanding the frames of clinical workers when new technology is being designed and implemented can inform changes to technology or organizational structure and policy that can preclude unproductive or unsafe adaptations.
Keywords: Barcode medication administration, adaptations, workarounds, unintended consequences, orienting frames
1.0 Introduction
The topics of health information technology (IT) design and implementation provide a canvas onto which engineers, clinicians, administrators and politicians paint a variety of idealized states of clinical practice and patient engagement. Health IT is said to have the potential to improve the safety and effectiveness of care (1-4). However, it is known that the implementation of health IT can introduce new risks into the environment of care as a result of design failures (5), implementation failures (6) and unintended consequences (7).
At the institutional level, management decisions to implement IT-based patient safety innovations are influenced by a variety of factors: financial considerations, marketing efforts of vendors, individual and shared experiences of leaders (e.g., clinical and/or management experience, education, and personal experiences with the health system), and subjective and shared ideas about what constitutes safe practice. Once the decision to implement the IT system has been made, various interest groups such as vendors, management, IT staff and users may have very different ideas about which safety-related problems need to be solved and the best strategies for solving them. The result is a myriad of software features, rollout decisions, infrastructure decisions, organizational structures, use practices and other factors converging to transform the sociotechnical system in ways that vary across clinical units.
Optimally, the convergence of these various perspectives, or frames of reference, can result in mutual learning and increased safety and effectiveness. In a less optimal scenario, there is a collision in priorities or understandings of practice that goes unresolved, leaving end-users, groups and organizations to adapt to fulfill individual goals (5, 8, 9). For example, when some hospitals’ new health IT systems collide unfavorably with pre-existing workflow, clinicians are known to adapt by persisting in the use of paper artifacts (10-13). These adaptations may improve or compromise quality and safety and, by virtue of being adaptations, constitute unintended consequences. With this paper, we use empirical research from 2 studies of the implementation of barcode medication administration (BCMA) to explore the collisions of the frame of reference for medication safety that was codified in the BCMA system with the frame held by practicing nurses. We examine adaptations used by individuals and organizations as a result of the collisions. With these analyses we aim to complement the sociotechnical frameworks that have been applied to health IT (14-21) by contributing insights into some fundamental reasons for adaptations and exploring the potential value of adaptations.
2.0 Background
2.1 Patient safety IT implementation research
Numerous health IT systems have been put forth as potentially valuable patient safety solutions, including BCMA, clinical decision support (CDS) and computerized provider order entry (CPOE). There is evidence of these systems alternately improving patient safety (22-27) and being the source of potential harm to patients (5, 6, 28, 29), suggesting that health IT outcomes depend on contextual issues such as implementation design (30-33). Research on unintended consequences has focused on patient safety IT, and has shown a lack of realistic representations of clinical work in tool design and implementation (7, 8, 39-41).
2.2 Frames
At the core of the problem revealed by unintended consequences is the existence of multiple frames of reference regarding clinical work. A technology developer may think of clinical work in terms that can be represented in a computer program. A manager may think about aspects of work that can be influenced by management practices, policies or the allocation of resources. A clinician or other health care worker may have a more “situated” (43) perspective on clinical work, where a myriad of factors such as the clinical environment, the patient and family, their training experiences, and surprises “in the moment” converge in the doing and describing of their work. These different perspectives have been characterized as frames (44), orienting frames (45), schema (46), and interpretive schemes (47). All of these constructs refer to shared conceptual resources that actors use to make sense of complex, ambiguous social and technical information. In contrast to the technological frames literature that examines frames of orientation to technological artifacts (48-50), we examine frames of orientation to the work of medication management and medication safety.
There are a variety of communities, or stakeholders, involved in the implementation of a BCMA system, ranging from vendors to clinical and technological management to bedside nurses. We use the term “System Frame” as a way of considering the system’s functionality and implementation as representative of the cumulative assumptions, decisions, priorities and perceived possibilities for problem-solving of the vendor, developers and implementation decision-makers. The “Practice Frame” is a similar aggregation of the bedside nurse’s perspective, as documented through observations and interviews. The practice frame may indirectly include the patient’s perspective via the nurse’s role as an advocate. In this paper we examine the conflicts or “collisions” between the System Frame and the Practice Frame and the resultant adaptations by both nurses and management.
2.3 Adaptations
In the context of health IT, adaptations are dynamic responses by human actors to the technology as well as the evolution and persistence of these responses over time. Adaptations include augmenting the technology and changing work practices to accommodate the technology (51, 52). Workarounds comprise a specific type of adaptation that is a widely-reported unintended consequence of health IT implementation (5, 28). In the case of workarounds, a new way of working is devised as a way to remove an impediment or problem (53). Studies have documented numerous workarounds related to BCMA use (53), including affixing patient identification barcodes to locations other than the patient in an effort to speed the scanning process (5, 28) or not scanning the medication or patient armband. Additionally, Koppel et al. (2008) identified causes of BCMA workarounds, including emergencies, wireless connectivity problems and malfunctioning technology (5). These findings suggest that gains in patient safety associated with BCMA may be eroded by risks introduced from workarounds, resulting in the need to alter the technology, the work process, or management policies related to medication management (10, 54). Adaptations can be observed at the individual level, in which a single user adapts work to accommodate the needs of the technology, or alternatively, avoids features of the technology in order to achieve work goals. Organizational adaptations also can be observed, as management decisions are implemented to either endorse the frame that the system imposes, or to soften or change the impact of the technology on work through explicit or implicit policies that reject aspects of the System Frame. We aim to add to the literature on technology implementation by describing adaptations that occur when frames of clinical work collide during sociotechnical transitions. Figure 1 is a graphical depiction of this conceptual model.
Figure 1.
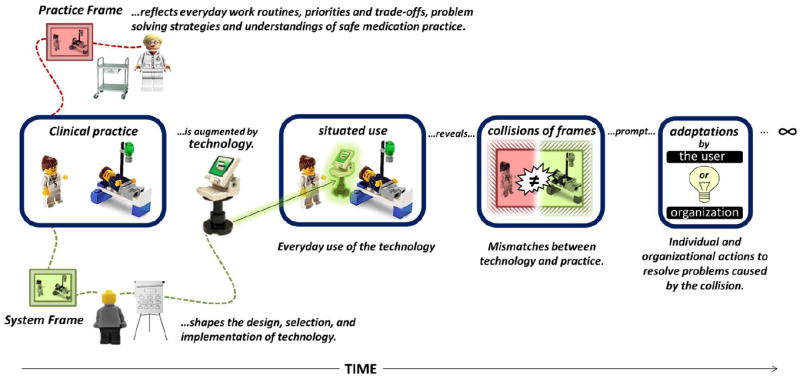
Collisions between the Practice Frame and the System Frame can result in adaptations by users and by the organization.
3.0 Methods
To depict multiple frames of reference for clinical work and the consequences of their collision for health IT implementation, we use illustrations from two qualitative BCMA studies. Both studies were conducted in inpatient settings. Methods are described in Table 1.
Table 1.
| Time Frame | Setting/ Focus | Data Sources | Primary Analysis | |
|---|---|---|---|---|
| Study A | 2007 – Phase 1 - observation of initial rollout of BCMA 2011 – Phase 2 observation and interviews |
Medication work of nurses on ten inpatient units in a tertiary adult hospital. |
|
Fieldnotes transcribed and analyzed with NVivo 9 Software. Phase 1 data coded by a one researcher, Phase 2 data coded by 3 researchers. Major themes included: 1) the five rights, 2) patient education, 3) verification, 4) dose timing, 5) coordination, 6) classification of medications |
| Study B | 2005 – pre- BCMA observations 2006 – initial rollout of BCMA 2007 – interviews 2008 – post-BCMA observations |
Medication work of nurses in a tertiary, free-standing pediatric hospital. |
|
Fieldnotes transcribed and annotated in Microsoft Word and Excel; flowcharts developed in MS Visio. Fieldnotes further assembled into bounded episodes of work and content-analyzed for problem-solving (i.e., adaptive) behavior by three researchers. Initial themes from 89 BCMA-specific episodes were: (1) BCMA facilitated novel problem-solving behavior; (2) BCMA blocked familiar problem-solving behavior; and (3) BCMA introduced new problems. |
For more detail on the methods used in Study A, see Novak et al (55), and for Study B see Holden et al (10).
The data for the two studies were initially analyzed independently. Investigators from each study then reanalyzed original study data to specifically identify instances of collisions of frames and any resultant adaptations. Collisions found across both studies were grouped under a progressively shrinking set of major themes evidenced by both studies. Examples from both studies were chosen to illustrate the themes and subthemes.
4.0 Results
Results are presented from analysis of both studies collectively. In each theme there is a collision between the System Frame (assumptions about medication administration and medication safety that are encoded in the design and implementation of the BCMA technology), and the Practice Frame (the way nurses enact or describe enacting medication administration). The collisions between the frames resulted in adaptations at both the individual and organizational levels.
4.1 Collision 1: The Role of the 5 Rights of Medication Administration
We found in both studies that the System Frame involved a rigid interpretation of the 5 Rights of medication administration that contrasted with nurses’ work, which involved 1) flexibility in the application of the 5 Rights and 2) important activities that went beyond the 5 Rights. The following section describes the System Frame, the Practice Frame, nurses’ adaptations observed in both studies, and the contrasting organizational adaptations seen in the two studies. These elements are summarized in Table 2.
Table 2.
Summary of frames and adaptations related to the role of the 5 Rights
|
Collision 1: Role of the “5 Rights” of medication administration
| ||
|---|---|---|
| System Frame | Practice Frame | Adaptations Observed |
|
| ||
| The 5 Rights are central to the design of BCMA systems. Barcoding is intended to ensure the right patient through barcoded wristbands, right drug, form and dose through barcoded labels and right time through the time of the scan. |
|
Individual adaptations were related to “Right Time” administrations and BCMA’s lack of accounting for other patient activities. Nurses inappropriately documented medications as “given” or “not given” in order to remove them from the active list. |
| Two approaches to organizational adaptation were observed in the two studies, with one organization making changes to the BCMA system to accommodate nurses’ needs and the other endorsing the System Frame through organizational policies. | ||
4.1.1 The System Frame
BCMA systems are designed to ensure the five rights of medication administration: right patient, right drug, right time, right dose and right way. A summary of the system definitions for the 5 Rights is included in Table 3.
Table 3.
Definitions of the 5 Rights in the System Frame
| Element | System Frame Definition |
|---|---|
| Right Patient | Barcode on scanned wristband must be patient to whom the nurse is assigned, for whom the subsequently scanned medications are prescribed. |
| Right Drug | Medication must appear in the orders for the patient. |
| Right Time | Must be within 1 hour before or 1 hour after the scheduled time for the dose. |
| Right Dose | Dose scanned must match dose ordered. Some systems allow accumulation (e.g. two 10mg tablets = 20mg), others give wrong dose error on first tablet scan that must be cleared. |
| Right Way | Form must match the form ordered (e.g. tablet, drops, patch, etc.). BCMA has little ability to assess the route through which the medication is actually administered. |
Several core functions observed in our studies are shared by most BCMA systems implemented in the United States (56). The barcoding technology includes handheld scanners that are either tethered or wirelessly connected to a computer, which is typically either wall-mounted or a laptop on a rolling cart. In some systems there is a handheld computer with a barcode scanner. The person administering the medication (usually a nurse) scans a barcode on the patient wristband and on the medication in various sequences, depending on the vendor. Medications have barcodes on unit-dose packages or may also come in packages assembled with barcode labels in the hospital pharmacy.
When the patient wristband and the medication are scanned, the system checks the patient’s orders to ensure that the scanned medication is ordered for the time scanned and in the dose indicated by the medication barcode. If these conditions are met, there is typically a process such as clicking a button whereby the nurse confirms that the medication was successfully administered to the patient. This action will document the dose as administered at the current time in the patient’s medical record. The documentation occurs in the electronic medication administration record (eMAR). The eMAR replaces the traditional paper MAR, which is a tabular, patient-specific document that lists each dose to be given to the patient over a specified period of time.
If the medication scanned does not match the eMAR for the patient scanned, various warnings or errors may appear, alerting the nurse that the medication is not found in the patient’s profile, or that the dose is wrong. BCMA systems diverge somewhat on the way these warnings appear and the way they need to be handled by the user. Medication administrations could also be documented without a scan through the eMAR, by selecting the dose to be administered and manually entering the time. This was “overriding” the scanning feature, and the system issued warnings and required a reason to be entered for all overrides. In entering a reason for overrides, the nurses select among the possible choices in a drop down list or documented in a free-text note.
BCMA technology is typically interoperable with other clinical and administrative applications such as CPOE, Pharmacy applications, billing and nursing documentation.
4.1.2 The Practice Frame
While the five rights were clearly important to patient safety, nurses described other categories of activities that they viewed as critical to medication safety, including 1) verifying others’ work, 2) educating the patient about the medication, its purpose, and proper administration, and 3) planning medication administrations to avoid conflicts and minimize patient distress.
4.1.2.1 Verifying others’ work
Nurses described checking multiple information sources to determine what medications were (or were not) administered on a previous unit, such as a procedural unit or the emergency department. In the quote below, a nurse describes a common strategy that involved checking one or more sources and then finally resorting to a phone call to confirm the details of previous administrations.
“…when a patient goes off the floor, sometimes we don’t know if they’ve been given a certain med, … if they came from the emergency room, we have to verify what they’re already received, … and if I can’t figure it out in the computer under the [Emergency Department] orders, I’ll just call down there so I can talk to the nurse because sometimes it’s still showing up in our [nursing system] to give it, but they may have already gotten it downstairs, ….”
Cardiology Nurse, 1 year experience
Verification also included researching orders that may have been incorrectly placed in the system or were old orders that had been superseded by a new order and had not been deleted. One nurse stated that reading orders and being able to discern which medications to actually give the patients was a skill gradually acquired through experience.
“…The doctor is putting the order in through [CPOE], and it goes through the computers…but it appears eventually [in BCMA] to give….But the doctor puts it [the new dose] in…and they forgot to take out the [old dose], stuff like that…my discernment has grown greatly just from the beginning.”
Cardiology Nurse, 1 year experience
The concept of verification also had a place in patient education. Nurses taught patients and families about the importance of verifying medication-related activities of others after the patient goes home. A pediatric nurse described a medication administration tracking tool that she encouraged families to use at home, because coordinating medication information may be new to some families:
“You know, Mom has to go to work while Dad is at home or the grandparents are there and that way you don’t mess up and two people give the same thing.”
Pediatric nurse, 12 years experience
4.1.2.2 Educating the patient about the medication, its purpose, and proper administration
Few nurses mentioned patient education in their initial response to the open-ended question of what medication safety meant to them. When questioned directly about it (due to the prominence of education activity during medication administrations in the observational data) the nurse below described patient education as an aspect of medication safety that is on equal footing with the 5 Rights:
“[Medication safety is] making sure that the person gets the right medication at the right time, the right dose, the right route and it also means making sure that the patient [is] familiar with the medications that they are getting so that when they go home…they’ll understand why they’re taking a particular medication and … be able to recognize it. And also, I am very careful about pronouncing medications.
Emergency medicine research nurse, 6 years experience
Another nurse also found patient education to be extremely important, not only for patient knowledge but also for patient adherence to prescribed therapy and prevention of medication errors.
“I think it [patient education] is extremely important…I think [patient understanding] leads to compliance and I think they should always question. … they can say ‘Well, I never take that medicine at night, I always take it during the morning,’ and you find out it’s the wrong patient or the wrong drug.”
Cardiology research nurse specialist, 9 years experience
4.1.2.3 Planning medication administration to avoid conflicts and minimize patient distress
The nurse quoted below describes his work in conforming medication administration actions to what makes the most sense for the patient and maximizes the patient’s comfort, even if that means compromising the Five Rights.
“… I had a patient, I had two antibiotics due, and she only had one IV line, and they’re both due at the same time…There’s definitely certain cases where you’d have to start another IV. In her case, it’s not really that inconvenient just to run one after the other; it’s less distress for her than to have another IV, so we just did that.”
Cardiology nurse, 4 years experience and graduate school
With two antibiotics due at the same time, the “right way” dictates that he is faced with the choice of administering them sequentially or starting another intravenous line. The nurse describes choosing to administer the drugs sequentially to minimize patient distress, partially because it is “not really that inconvenient” to do so. However, this choice may result in a late administration, and requires the nurse to remind himself to go back and administer the antibiotic to the patient after he has moved on to other tasks.
4.1.3 Adaptations resulting from Collision 1
This collision of the System Frame and the Practice Frame resulted from both 1) the rigid application of the 5 Rights in BCMA and nurses’ need for flexibility in practice, and 2) the many activities related to safe medication administration that fell outside the 5 Rights and were not addressed by BCMA functionality. Below we discuss adaptations made by nurses and by the organizations as a result of the collision.
4.1.3.1 Nurses’ Adaptations of Work to the System Frame
In both studies, we observed nurses adapting their work to the System Frame’s rigid interpretation of the 5 Rights. Of the 5 Rights, “right time” was the most flexibly interpreted in practice. A specific medication schedule is produced abstractly per single patient, without regard to other activities the patient may be engaged in. Each patient is busy with important activities such as tests and procedures, sleeping, and eating, among other things. This complexity is multiplied for the nurses, who are typically assigned to multiple patients. In order to organize their days, nurses often “batched” medication passes for individual patients to save time, e.g. giving all of the medications due during a 4 h period at one time. Other examples of collisions of system rigidity and practice flexibility include the following:
In the pediatric hospital of Study B, pharmacists entered important administration-related directions into BCMA that were previously written out on the paper MAR. These directions were located in BCMA on a screen that nurses rarely checked prior to administration. As a result, the directions would only come up at the time the medication was scanned. Thus, whereas information related to the five rights was highly accessible and visible in BCMA, additional important information such as pharmacy directions for administration, was “buried” in the system.
In both studies, nurses sometimes documented doses “Not Given” if the administrations were anticipated to be outside the on-time window, removing the chance that the doses would be classified in the system as “Late.” However, the opportunity to give these doses often arose later in the shift or on a subsequent shift, but a dose previously documented as “Not Given” is no longer available to administer. This resulted in the nurse selecting the next dose in the schedule, a practice referred to by study subjects as “borrowing” or “stealing” doses. This practice shifted the schedule, causing problems with downstream doses and future shifts.
In Study B, a pediatric ICU nurse was delayed in administering a scheduled medication because a) the previous dose of the medication had been administered later than scheduled due to a surgical procedure and b) an incompatible medication was presently being infused. Rather than give the appearance that the medication was “missed” or administered late, the nurse scanned the medication before the scheduled administration window had elapsed but half an hour before actually administering it.
Another example of the rigid interpretation of “right time” in the System Frame was the standard interval assigned to the timing of PRN (as needed) medications. We observed a pediatric ICU nurse who had determined that his patient required a PRN ointment. Because the four hour interval between PRN administrations had not elapsed, BCMA issued a warning against administering the medication. However, explaining that the 4 h interval was arbitrary and contradicted current clinical needs, the nurse overrode the warning and documented “time change” as the reason for doing so.
Finally, we observed the System Frame’s tenacity with respect to “right time” raising questions among nurses about the choices they made in practice. In one case, the nurse found that a number of scheduled medications had become classified as “past due” in the BCMA system, but that these medications were rightly being withheld in anticipation of a surgical procedure; even after documenting this, the medications remained labeled “past due,” leading the nurse to question whether she had done the right thing.
4.1.3.2 Organizational Adaptations
Our two studies presented contrasting images of organizational adaptations. In one study, management attempted to adapt the System Frame to the nurses’ work, apparently making it less rigid. Noting the problems caused by “stealing doses,” management took several actions to attempt to remove the stigma of late doses, including renaming a standard BCMA report from Overdue Medications Report to Outstanding Medications Report and launching a publicity campaign among the nurses to clarify that there were clinically acceptable reasons for a late medication.
In the other study, management strongly endorsed the System Frame by making nurses’ compliance with the BCMA system a part of performance measurement. If a medication was documented as given, but there was no associated scan of the patient and/or the medication, that administration was not considered compliant. Scanning compliance thresholds were set at 97% for patients and 90% for medications. If these thresholds were not met, the nurses, despite excellence in other areas of performance, could not achieve the top score on their annual evaluations. These scores were linked to nurses’ compensation levels.
4.2 Collision 2: Roles of human actors and the linearity of medication work
4.2.1 The System Frame
In both studies, BCMA encoded the roles of human actors in an inflexible, linear workflow: the physician ordered the medication and specified the frequency, dose and route; the pharmacist verified the dose and route and assigned the schedule, the pharmacy department filled and dispensed the medication and the nurse or therapist assigned to the patient administered the medication. With its focus on medication administration in the abstract, the System Frame assumed that medication administration tasks could be isolated from other nursing tasks unrelated to medications. In order to document their activities within BCMA-prescribed roles, nurses and other personnel with patient contact such as respiratory therapists and technical staff went through a process of “assignment” at the beginning of a shift to appoint themselves as a nurse or caregiver for the patients they had been assigned.
4.2.2 The Practice Frame
Prior to the implementation of BCMA, documenting medication administration on the paper MAR was a somewhat autonomous act for nurses. For example, nurses were observed writing notes to other nurses on the paper medication administration record (MAR). In both studies, this practice was used to communicate information about specific doses to others caring for the patient. If the nurse found she needed to give a medication outside the window of “on-time” administration, this could be done and the actual time of administration could be noted on the paper MAR. If an early or delayed dose affected the timing of downstream doses, nurses occasionally drafted a plan that they documented in the MAR to “stagger” the patient back onto the proper schedule through a series of appropriately timed doses. Nurses had the authority and ability to adapt the schedule as was clinically appropriate and within their scope of practice.
In contrast to BCMA’s focus on medication administration in the abstract, nurses described their work in holistic terms. They discussed managing medications amid numerous clinical and logistical dependencies, such as patients’ need for sleep, their trips off the unit for tests and procedures, and meals. The administration of many medications required prior blood pressure readings, blood glucose measurements or research as to how the drug can be administered safely with respect to the other medications and their timing for that patient. Medication administration was not an isolated task, but instead co-mingled with many activities that might seem unrelated.
4.2.3 Adaptations resulting from Collision 2
Adaptations that we observed related to Collision 2 are summarized in Table 4. With respect to the rigid interpretation of roles, we documented no organizational adaptations to technology or policy to either reject or endorse the System Frame, which suggests a tacit endorsement by the organizations in both studies. However, in Study A organizational leaders expressed concern about the system’s rigid interpretation of the medication schedule, and that to the extent that BCMA constrained the nurse’s ability to make minor adjustments constituted a threat to nurse’s ability to apply “critical thinking” to patient care issues. Organizational adaptations were observed to soften the impact of the linear workflow imposed by BCMA. For example, in Study A, paper MAR forms were re-introduced for use in emergency situations. Individual adaptations are described below.
Table 4.
Summary of frames and adaptations related to the roles of human actors
|
Collision 2: Roles of human actors in medication administration
| ||
|---|---|---|
| System Frame | Practice Frame | Adaptations Observed |
|
| ||
| Roles of actors related to medication administration were encoded into the system: Physician orders, Pharmacist verifies and assigns schedule, and Nurse or therapist administers the medication. |
|
Individual adaptations involved substantial communication among nurses and pharmacists to adjust schedules and accommodate special requirements (e.g. substituting two 10mg tablets for one 20mg tablet). |
| Organizational adaptations in our data were minimal, although organizational leaders discussed concern about the potential limitations being placed on nurses’ practice. | ||
|
| ||
| Linear workflow: BCMA accepts orders from the CPOE system that have been processed by the pharmacy. Administration of medications cannot occur until the medication becomes active in the BCMA medication list. | In addition to verbal orders for immediate administration of a medication, which precludes the full BCMA process, medication management is co-mingled with other activities for the patient. These activities and contingencies may simultaneously apply for all of the patients assigned to a given nurse. | Individual adaptations included parallel tracking systems for tasks. |
| Organizational adaptations included the development of paper MAR forms for documentation during emergencies. | ||
4.2.3.1 Patient assignments
In both studies, nurses who wished to assist fellow nurses with their assigned patients were required to go through the additional process of adding a patient to their list of assigned patients, completing the necessary clinical tasks, then removing the patient from the list.
4.2.3.2 Adjusting schedules and doses
In several cases, nurses were unable to adjust the timing of scheduled medications or the permissible interval between PRN (as needed) medications. Timing decisions and timing changes were instead made by pharmacists, sometimes with and sometimes without, consultation with the nurse. At times the nurse’s lack of control over timing led the nurse to request timing changes from pharmacy and at other times it resulted in medications being labeled as “missed doses” in the system or in nurses overriding BCMA. This illustrates how the BCMA encoded the frame that pharmacists make decisions about medication timing and nurses act on those decisions. Similarly, BCMA encoded the frame that physicians make dosing decisions and nurses must execute them as ordered. At times this was in conflict with the Practice Frame. The vignette presented in Box 1, previously reported in Holden et al (57), BCMA enforced a strict interpretation of the physician’s original order, despite the nurse’s ability to make a simple substitution between two clinically equivalent sets of doses (one 20mg vs. two 10mg).
Box 1. The rigid interpretation of roles in BCMA collides with more flexible interpretations in practice.
“… a physician ordered a 20mg dose of a blood pressure medication that would be scheduled starting with the first dose at 0900. Even though the medication was scheduled to be given right away, it would take some time for Pharmacist 1 (the first of two Pharmacists involved in the case) to prepare it. Prior to this 20mg dose order, the patient had a standing PRN order [to be administered as needed], for a 10mg dose of this medication. Thus, there were 2 available 10mg doses of the medication at bedside, in the nurse’s medication lockbox. However, when the resident placed a new order into CPOE for the 20mg dose, s/he also discontinued the 10mg PRN order. At this point, the BCMA system was “expecting” a single 20mg dose, and would not allow two 10mg doses to be scanned in as acceptable. Under these conditions, the available medication could not be administered according to the goals of the ordering physicians (and, likely, the goals of the nurse).
Pharmacist 2, recognizing this problem, instructed the nurse to administer two 10mg doses of the available medication, at once, to avoid delays. To allow this to happen within the restrictions of the BCMA software, Pharmacist 2 first reinstated the 10mg PRN order, so that the nurse could scan one of the 10mg doses and administer it as if it were a PRN. However, the BCMA system did not allow a second dose of PRN medication to be given so close to the first. In response, Pharmacist 2 created a new onetime order for a 10mg dose of the medication, in the BCMA system. The nurse was then able to administer the second available 10mg dose. Afterwards, Pharmacist 2 had to very quickly discontinue the new 10mg PRN medication so that it would no longer be available in the system. Pharmacist 2 also had to request that Pharmacist 1 change the scheduled 20mg order so that the first dose was now scheduled for 1500 as opposed to 0900, so that no extra dose would be given. During an interview, Pharmacist 2 remarked on this situation, “Sometimes you have to play games with the system to make it work.”
In some cases, particularly in the pediatric Intensive Care Unit, nurses were required by the rigid logic of BCMA to wait until an order was created in CPOE and transcribed by pharmacy into the BCMA system before they could administer the medication using the normative BCMA-based process. Prior to BCMA, however, ICU nurses could act on verbal orders and complete medication preparation, verification, and administration steps in parallel to physicians’ medication ordering and pharmacists’ transcription of the order.
4.2.3.3 Keeping track of other clinical tasks
While BCMA displayed the medication schedule, it did not allow for the display of other clinical tasks, even if they were directly related to medication administration. In this example from Study B, a nurse describes her strategy keeping track of tasks:
“… when I worked in the ICU for several shifts, one thing I learned from them is they would take a piece of tape every day and put on the counter and schedule out 8, 9, 10, 11, 12…They would write their shift down and say at 8:00, this patient needs this and this, at 9:00 they’re gonna need a repeat blood pressure, at 10:00…So they could go through their day and check it off to make sure they didn’t forget anything.”
The nurse is explaining that even though the nurses had BCMA in the ICU, they still put a long piece of masking tape on their workstation desk at the start of the shift. On that tape, they wrote down everything that had to be done for the patient and at what time. They did this because only medications could be tracked or monitored in BCMA; most of the nursing work could not. Thus, they created an artifact on which they could put not only meds, but also meal times, lab times, care tasks, consultation time, etc. In Study A, we observed nurses using a blank piece of paper or a printout of the patient’s orders for the day as a “cheat sheet” on which they wrote key information and tracked tasks.
4.2.3.4 Accommodating urgent situations
During urgent situations in which medications needed to be quickly administered, BCMA’s linear logic (physician order → pharmacy transcription → nurse administration → nurse documentation) conflicted with the exigencies of the situation, in which processes such as ordering, transcription, and administration might occur in parallel or out of sequence and documentation was of lower priority. As an adaptation at the organization level, the hospital in Study B attempted several solutions. One of the solutions was to use a blank MAR to document medications during urgent situations, bypassing the BCMA. However, using the blank MAR created confusion: in order to charge administered medications documented in the blank MAR, they had to be entered into the pharmacy information system, which resulted in a new order being transmitted to the BCMA. To remove this order, pharmacists then had to discontinue the medication immediately after entering it.
4.3 Collision 3: Classification of medications
4.3.1 The System Frame
In both studies, BCMA enabled classification of certain medications for which additional regulations applied. For example, the system included functionality for a second nurse to sign off on the administration of certain medications such as insulin, or in the case of wasting excess narcotics, where the risk of injury to the patient was high if an error in dosing occurred. However, there were no customizable classifications for a specific patient or for types of drugs based on administration characteristics. In general, medications were treated equally by the system. Table 5 summarizes the frames and adaptations related to the classification of medications.
Table 5.
Summary of frames and adaptations related to the classification of medications
| Collision 3: Classification of medications | ||
|---|---|---|
| System Frame | Practice Frame | Adaptations Observed |
| BCMA classified some medications (e.g. insulin, narcotics, and chemotherapeutic agents) as special, with constraints for administration designed into the system. All other medications were considered “equal” by BCMA. | Medication administration is context-dependent. Nurses’ priorities were patient safety and comfort. Nurses described making choices among patients, drugs and therapies. | Individual adaptations primarily involved workarounds to make administrations appear to be on-time in BMCA (e.g. scanning the medication substantially earlier than the actual administration takes place), and simply overriding administration times, accepting the “late” status of the administration. |
4.3.2 The Practice Frame
Nurses viewed medication administration decisions as context-dependent, and nurses sometimes delayed medications for which precise timing was not critical. In interviews, nurses discussed numerous situational strategies for prioritizing medication administrations: placing transplant patients at a high priority for on-time administrations, paying special attention to antibiotics and the need to occasionally draw peak and trough blood levels of the drugs, and paying special attention to blood-thinning agents especially when patients are scheduled for procedures. These decisions were made based on each patient’s schedule and often required nurse experience and additional communication with physicians to determine when medications could be held.
“There’s lots of times when [physicians] don’t want [medications] post-procedure, but nobody’s responsible because the patient’s transitioning from one unit to the other…and then it’s up to us [nurses] to try and figure out [if the medication should be administered].”
Cardiology Nurse, 5 years experience
Other medications were of lower priority, sometimes as a result of patient activity. For example, a dose of Tylenol might be delayed if the patient was sleeping or it could be combined with other medications in a subsequent administration. A nurse described the prioritization:
“… if someone has a med that’s due at nine o’clock that’s a multi-vitamin and someone has an antibiotic due, then you know which one’s going to get priority, so I just…you know, and prioritize things like pain and safety issues … prioritize according to keeping patients comfortable and keeping them safe.”
Cardiology nurse, 4 years experience
4.3.3 Adaptations resulting from Collision 3
After being trained on BCMA in Study A, nurses expressed concern about losing the flexibility in documentation. The nurses attempted to minimize the inevitable late doses that resulted from their situated priorities, but several nurses reported that over time, they became less concerned that doses were classified as late. One nurse viewed his lack of concern about late medications as “a personality trait,” while another saw it as an inevitable product of workload:
“…we give a lot meds early and a lot of meds late just so that you can get through the day. …it’s very common for me to be constantly overriding my meds, either too early or too late.”
Cardiology Nurse, 5 years experience
5.0 Discussion
The collisions and related adaptations we describe raise questions about the design and implementation of BCMA and about research on adaptations that may also apply to other clinical informatics applications and health IT tools:
5.1 BCMA design and implementation
5.1.1 What should the role of the 5 Rights of medication administration be in medication management IT?
The 5 Rights are essential, but not sufficient to ensure safe medication practice. The nurses in the two studies engaged in other work beyond the 5 Rights to ensure medication safety. Some tasks were easily recognizable as clinical work that could be linked to medications with some ease (e.g. obtaining blood pressure values prior to certain administrations). Others, such as patient education, have little or no functionality in BCMA but are crucial to ensuring medication safety within and beyond the scope of the hospital. Nurses described and were observed teaching the patients and families the names and clinical actions of the medications, discussing strategies for home medication management, and reinforcing the need to adhere to the prescribed regimen. BCMA systems contain a substantial amount of data that could be contributed to patient education efforts during the inpatient stay; for example, helping patients understand the schedule they will go home with, and reinforcing the names and descriptions of the medications could potentially improve patient compliance with self-administered medications. The effects of patient education can potentially improve the quality of subsequent health care encounters, when patients aware of their own medication regimens can act as another source of information for both physicians and nurses unfamiliar with their medical history.
The details of the tasks and knowledge that constitute medication administration safety vary among patient populations and clinical settings. Exploring the clinician and patient perspective of how medication safety is achieved can provide insight into the functionality that needs to be present in medication safety IT tools.
5.1.2 Why are so many adaptations related to the timing of doses?
The design and implementation of BCMA encoded explicit and implicit assumptions about temporal aspects of medication-related work. Examples of these assumptions include a) the classification of administrations as on-time, early or late, even when clinical documentation was entered to justify early or late administrations and, b) arbitrary and inflexible intervals assigned to PRN medications without consideration of patient or nurse availability. The effect of this ossification of temporal categories is the overstatement of the importance, in some cases, of an on-time dose. Certainly there are situations in which the medications must be given at a specific time, but critical temporal relationships in medication administration are often relative to other events, such as eating, an invasive procedure, or the administration of other conflicting medications. In our studies, BCMA offered little functionality for the management of these complex temporal relationships (58), leading to adaptations around the system that could possibly increase medication error.
5.1.3 If the System Frame represents the correct policy, shouldn’t the Practice Frame be forced to adapt?
The System Frame formalized the roles of physicians, pharmacists, nurses and other clinicians with respect to medication management. This formalization was based on both legal and traditional structures of clinical authority and responsibility. However, qualitative research demonstrates that real-world clinical work, referred to here as the Practice Frame, often does not adhere to formalizations (14, 59). Design accommodations in BCMA may bring the two frames into better alignment. For example, the patient assignment function created a one-to-one relationship between nurses and patients that had to be established each time a colleague assisted in administering medications. Perhaps if the System Frame more accurately reflected the Practice Frame, nurses would see primarily the clinical status and information for their assigned patients, but also be authorized to assist in caring for others on the same unit. Similarly, the authority within BCMA to make changes in the medication schedule, within limits, would more accurately reflect the Practice Frame when medication administration is secondary to patients’ schedules. Such adjustments to medication schedules would also provide more significance to time-related warnings, potentially making the system more effective. With the implementation of BCMA, increased formalization of the work system and reallocation of authority over schedules and patient assignments can be interpreted as a loss of control or autonomy for the nurses. The loss of nursing autonomy that results from management endorsement of an inflexible work system must be weighed against potential improvements in safety that can be achieved by the implementation of patient safety IT. Even as we suggest potential repairs to BCMA, we observe that research exploring collisions between the way system designers think people work and the way people actually work serves another purpose: calling policies, traditions and classifications into question. The linearity of medication management tasks was an aspect of the System Frame that collided with the way nurses experience their work. Due to time pressures created by urgent clinical situations, overall complexity, or volume of work, work processes that may have seemed linear (or ideally have been linear given institutional and legal interpretations of clinical roles) were carried out in non-linear ways. For example, tasks were compressed such that interrelated tasks were carried out in parallel or out of sequence, and steps were sometimes paused and continued later. Clinical roles in health care are changing so that relations are increasingly less hierarchical, and new competencies are beginning to be reflected in legal and institutional structures (60, 61). Therapeutic interventions are also dynamic. Nurses administer drugs ranging from pain medications to stool softeners to antihistamines, all under the same role and responsibility structure. We do not advocate that the Practice Frame be considered a “gold standard” by which clinical IT systems should be infinitely customized. Instead, we believe that ongoing dialogue on the relationship between competency and therapy at the institutional and policy levels should inform the development of clinical IT.
5.2 Adaptations
5.2.1 Why study adaptations?
Berg (62) argues that a common myth about health IT implementation is that it is “the technical realization of a planned system in an organization.” Instead, as this study shows, implementation is an ongoing, mutual transformation of the organization and the health IT. Adaptations at the individual and organization levels are two mechanisms behind this mutual transformation. We argued here that at least some adaptations occur when health IT is designed or implemented in a way that conflicts with how clinicians perceive (or frame) their work; this is the reality that debunks the “field of dreams fallacy” that “if you provide [health IT] to clinicians, they will gladly use it, and use it as the designer intended” (41) p. 619. Other studies are beginning to identify ways in which nurses adapt when BCMA is introduced (10, 52) and the literature on unintended consequences, workarounds, and paper persistence in particular has identified specific adaptations related to CPOE (9, 11-13). However, adaptations remain understudied and, without being better understood, risk being labeled as undesirable side-effects perpetrated by “resistors” or “bad apples” (41). In fact, adaptations may be inevitable; necessary to accomplish work goals; can be learned from as new “best practices”; and consequently may need to be fostered and facilitated (10). However, further discourse on adaptations must proceed on a stronger research base than currently exists. Future research questions include: How do adaptations evolve? What classes of adaptations are found following technology implementation? What are their ultimate effects? Notably, in our analysis of adaptations related to collisions of the System Frame and the Practice Frame, we identified numerous adaptations at the individual level but few at the organizational level. This may be because there are few organizational adaptations. Indeed, there are few accounts of these types of adaptations in the literature, although exceptions include Campbell’s et al discussion of constant software upgrades and fixes or “never-ending demands for system changes” (9) p. 550, Goorman and Berg’s (63) example of CPOE being modified to accommodate nurse note writing, and the work of Novak et al on organizations hiring mediators to advocate for the practice frame and assist nurses with integration of technology into everyday work during BCMA implementation (31). Another possibility is that the two studies reported here were not designed to or could not adequately capture organization-level adaptations. Future research may benefit from targeting such adaptations by capturing in detail the history of health IT implementation and use, interviewing the organization’s or unit’s decision makers, and asking in what ways organizational entities endorse, facilitate, and invent adaptations.
5.2.2 What should organizations do about adaptations related to health IT?
Adaptations, especially at the individual level, can be seen as problematic or pragmatic. It is probable that there are adaptations of both types. Therefore, rather than seeking to eliminate adaptations, careful internal analyses should identify which adaptations should be supported, for example through organizational alliances between clinical and technical staff, leadership endorsement and involvement, or empowerment of staff in mediating roles (30). However, adaptations are not without their faults. They may be necessary or unnecessary, effective or ineffective, useful or counterproductive, proactive or reactive, safe or unsafe, etc. Further, as Holden et al argue, “adaptive problem-solving behavior is a double-edged sword: it precludes failures not prevented through design but also obscures those design flaws” (10). Again, more research will be needed to truly understand the nature of adaptations related to health IT.
5.2.3 What is the value added by using “frames” to describe adaptations?
Research on adaptations of any kind should proceed on the assumption that adaptations are a rational response, given the social and technological conditions presented to the actor. When patterns in adaptations are observed, actors are carrying out an implied structure, in other words a set of unspoken “rules”, that may at times conflict with institutionally sanctioned policy and procedure. Research on frames attempts to reveal these rules or structures. Hazlehurst and McMullen conducted ethnographic research among ICU nurses and identified several “orienting frames” that they defined as “conceptual resources that help actors to organize, prioritize, conduct and evaluate their work” (45) p. S130. Using frames to understand how nurses enact medication safety (e.g. their priorities, the activities they engage in, and problem solving strategies) can produce information that technology designers and implementers can use to improve the fit between the technology and the work.
In this paper we reported two frames: System and Practice. The System Frame is a composite of the assumptions embedded in BCMA design, technological and organizational implementation decisions and related organizational policies. Our research foregrounds the nurses’ experience and highlights that nurses are not just integrating a new set of procedures or artifacts into everyday work, but an orientation to medication safety itself that is sometimes at odds with their own. Given the designs of our studies, we were able to specify the Practice Frame more completely than the System Frame. Future work must strike better balance between understanding work and safety from the worker’s perspective and from the perspective of the designer and implementer. This will allow for a more complete picture of the factors and relationships that constitute sociotechnical systems.
6.0 Conclusion
We found that the System Frame was less integrated and flexible than the Practice Frame, less able to acknowledge all of the dimensions of patient care to which medication administration is tied. In our studies, nurses viewed medication safety holistically, as emerging from all aspects of their nursing work. They worried about forgetting or not being able to keep track of the myriad of tasks required for their patients in addition to medication administration. BCMA is focused on medication administration, specifically, the 5 Rights, as opposed to other aspects of nursing. Future research should attempt to explicate further the frames of orientation that influence the actions of clinicians, patients, managers, vendors and other stakeholders in the medication management enterprise. This will result in a body of evidence regarding the work of medication management and how it fits into everyday routines that can be used to support institutionally sanctioned adaptations of work, technology and organizational policies and structures.
Summary Points.
What was already known
Health IT can improve patient safety and also introduce new risks to patient care.
Research on unintended consequences in health IT has shown a lack of realistic representations of clinical work in tool design and implementation.
Adaptations include augmenting the technology and changing work practices to accommodate the technology.
What this study adds
At the core of the problem revealed by adaptations is the collision of multiple frames of reference regarding clinical work.
Adaptations are not universally negative, but instead sometimes result in productive changes to workflow, organizational policy and/or informatics tools.
Using frames to understand how nurses enact medication safety can produce information that technology designers and implementers can use to improve the fit between the technology and the work.
Highlights.
Health IT system designers and implementers may have frames of orientation regarding medical work that differ from the frames held by practitioners.
Collisions in system frames and practitioner frames can result in adaptations by individuals and organizations.
Adaptations are not universally negative, but instead sometimes result in productive changes to workflow, organizational policy and/or informatics tools.
Acknowledgments
This paper is dedicated to Professor Bentzi Karsh, a leader in sociotechnical research in health care. Bentzi contributed significantly to the first version of the manuscript by challenging assumptions of the other authors and providing his unique insights and edits on the text. Sadly, he passed away on August 18, 2012. This paper reflects his evolving thinking on sociotechnical approaches to understanding technology and organizations.
The authors wish to thank the anonymous reviewers for their insights. Dr. Novak was supported by funding from National Library of Medicine grants 1 K99 LM 010038 and 4 R00 LM010038, and Dr. Holden was supported by National Center for Advancing Translational Sciences (NCATS) grant 2KL2TR000446-06 through the Vanderbilt Institute for Clinical and Translational Research (VICTR).
Footnotes
Author contributions
Laurie L. Novak: conception and design of the study, acquisition of data, analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be submitted.
Richard J. Holden: conception and design of the study, acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Shilo H. Anders: conception and design of the study, acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Jennifer Y. Hong: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Ben-Tzion Karsh: conception and design of the study, acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content.
The authors have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Laurie Lovett Novak, Department of Biomedical Informatics, Implementation Sciences Laboratory, Center for Research and Innovation in Systems Safety, Vanderbilt University School of Medicine.
Richard J Holden, Departments of Medicine and Biomedical Informatics, Center for Research and Innovation in Systems Safety, Vanderbilt University School of Medicine.
Shilo H Anders, Department of Anesthesiology, Center for Research and Innovation in Systems Safety, Vanderbilt University School of Medicine.
Jennifer Y Hong, Department of Biomedical Informatics, Summer Research Internship, Vanderbilt University School of Medicine.
Ben-Tzion Karsh, Department of Industrial and Systems Engineering, University of Wisconsin Madison.
References
- 1.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma’Luf N, et al. The Impact of Computerized Physician Order Entry on Medication Error Prevention. Journal of the American Medical Informatics Association. 1999 Jul;6(4):313–21. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Devine EB, Hansen RN, Wilson-Norton JL, Lawless NM, Fisk AW, Blough DK, et al. The impact of computerized provider order entry on medication errors in a multispecialty group practice. Journal of the American Medical Informatics Association. 2010 Jan;17(1):78–84. doi: 10.1197/jamia.M3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sakowski J, Leonard T, Colburn D, Michaelson B, Schiro T, Schneider J, et al. Using a bar-coded medication administration system to prevent medication errors in a community hospital network. American Journal of Health-System Pharmacy. 2005;62:2619–25. doi: 10.2146/ajhp050138. [DOI] [PubMed] [Google Scholar]
- 4.Johnson C, Carlson R, Tucker C, Willette C. Using BCMA software to improve patient safety in Veterans Administration Medical Centers. Journal of Healthcare Information Management. 2002;16(1):46–51. [PubMed] [Google Scholar]
- 5.Koppel R, Wetterneck T, Telles JL, Karsh B-T. Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. Journal of the American Medical Informatics Association. 2008;15(4):408–23. doi: 10.1197/jamia.M2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han YY, Carcillo JA, Venkataraman ST, Clark RS, Watson RS, Nguyen TC, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005 Dec;116(6):1506–12. doi: 10.1542/peds.2005-1287. [DOI] [PubMed] [Google Scholar]
- 7.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. Journal of the American Medical Informatics Association. 2004 Mar-Apr;11(2):104–12. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ash JS, Sittig DF, Dykstra RH, Guappone K, Carpenter JD, Seshadri V. Categorizing the unintended sociotechnical consequences of computerized provider order entry. Int J Med Inform. 2007;76(Supplement 1):S21–S7. doi: 10.1016/j.ijmedinf.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 9.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006 Sep-Oct;13(5):547–56. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holden R, Rivera-Rodriguez A, Faye H, Scanlon M, Karsh B. Automation and adaptation: Nurses’ problem-solving behavior following the implementation of bar coded medication administration technology. Cognition, Technology and Work. 2012 doi: 10.1007/s10111-012-0229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holden RJ. Physicians’ beliefs about using EMR and CPOE: in pursuit of a contextualized understanding of health IT use behavior. Int J Med Inform. 2010 Feb;79(2):71–80. doi: 10.1016/j.ijmedinf.2009.12.003. Epub 2010/01/15. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saleem JJ, Russ AL, Justice CF, Hagg H, Ebright PR, Woodbridge PA, et al. Exploring the persistence of paper with the electronic health record. Int J Med Inform. 2009 Sep;78(9):618–28. doi: 10.1016/j.ijmedinf.2009.04.001. Epub 2009/05/26. eng. [DOI] [PubMed] [Google Scholar]
- 13.Saleem JJ, Russ AL, Neddo A, Blades PT, Doebbeling BN, Foresman BH. Paper persistence, workarounds, and communication breakdowns in computerized consultation management. Int J Med Inform. 2011 Jul;80(7):466–79. doi: 10.1016/j.ijmedinf.2011.03.016. Epub 2011/05/03. eng. [DOI] [PubMed] [Google Scholar]
- 14.Aarts J, Gorman P. IT in Health Care: Sociotechnical Approaches “To Err is System”. Int J Med Inform. 2007 Jun;76(Suppl 1):1–3. doi: 10.1016/S1386-5056(07)00078-0. [DOI] [PubMed] [Google Scholar]
- 15.Berg M, Aarts J, van der Lei J. ICT in health care: sociotechnical approaches. Methods of information in medicine. 2003;42(4):297–301. [PubMed] [Google Scholar]
- 16.Harrison MI, Koppel R, Bar-Lev S. Unintended Consequences of Information Technologies in Health Care An Interactive Sociotechnical Analysis. Journal of the American Medical Informatics Association. 2007 Sep 1;14(5):542–9. doi: 10.1197/jamia.M2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holden RJ. Cognitive performance-altering effects of electronic medical records: An application of the human factors paradigm for patient safety. Cogn Technol Work. 2011 Mar;13(1):11–29. doi: 10.1007/s10111-010-0141-8. Epub 2011/04/12. Eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holden RJ, Brown RL, Alper SJ, Scanlon MC, Patel NR, Karsh BT. That’s nice, but what does IT do? Evaluating the impact of bar coded medication administration by measuring changes in the process of care. International journal of industrial ergonomics. 2011 Jul 1;41(4):370–9. doi: 10.1016/j.ergon.2011.02.007. Epub 2011/06/21. Eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holden R, Karsh B-T. A theoretical model of health information technology usage behaviour with implications for patient safety. Behaviour & Information Technology. 2009;28(1):21–38. [Google Scholar]
- 20.Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform. 1999 Aug;55(2):87–101. doi: 10.1016/s1386-5056(99)00011-8. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan B. Evaluating informatics applications--some alternative approaches: theory, social interactionism, and call for methodological pluralism. Int J Med Inform. 2001 Nov;64(1):39–56. doi: 10.1016/s1386-5056(01)00184-8. [DOI] [PubMed] [Google Scholar]
- 22.Potts AL, Barr FE, Gregory DF, Wright L, Patel NR. Computerized Physician Order Entry and Medication Errors in a Pediatric Critical Care Unit. Pediatrics. 2004;113(1):59–63. doi: 10.1542/peds.113.1.59. [DOI] [PubMed] [Google Scholar]
- 23.Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Archives of internal medicine. 2003 Jun 23;163(12):1409–16. doi: 10.1001/archinte.163.12.1409. Epub 2003/06/26. eng. [DOI] [PubMed] [Google Scholar]
- 24.King WJ, Paice N, Rangrej J, Forestell GJ, Swartz R. The effect of computerized physician order entry on medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003 Sep;112(3 Pt 1):506–9. doi: 10.1542/peds.112.3.506. Epub 2003/09/02. eng. [DOI] [PubMed] [Google Scholar]
- 25.Kuperman GJ, Gibson RF. Computer physician order entry: benefits, costs, and issues. Annals of internal medicine. 2003 Jul 1;139(1):31–9. doi: 10.7326/0003-4819-139-1-200307010-00010. [DOI] [PubMed] [Google Scholar]
- 26.Mekhjian HS, Kumar RR, Kuehn L, Bentley TD, Teater P, Thomas A, et al. Immediate benefits realized following implementation of physician order entry at an academic medical center. J Am Med Inform Assoc. 2002 Sep-Oct;9(5):529–39. doi: 10.1197/jamia.M1038. Epub 2002/09/12. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996 Nov-Dec;3(6):399–409. doi: 10.1136/jamia.1996.97084513. Epub 1996/11/01. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patterson ES, Cook RI, Render ML. Improving patient safety by identifying side effects from introducing bar coding in medication administration. J Am Med Inform Assoc. 2002 Sep-Oct;9(5):540–53. doi: 10.1197/jamia.M1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aarts J, Ash J, Berg M. Extending the understanding of computerized physician order entry: Implications for professional collaboration, workflow and quality of care. Int J Med Inform. 2006 Jun 22; doi: 10.1016/j.ijmedinf.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 30.Novak LL, Anders SH, Gadd CS, Lorenzi NM. Mediation of Adoption and Use: A Key Strategy for Mitigating Unintended Consequences of Health IT Implementation. Journal of the American Medical Informatics Association. 2012 May 26; doi: 10.1136/amiajnl-2011-000575. Online First. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Novak LL, Brooks J, Anders S, Lorenzi N, Gadd CS. Mediating the intersections of organizational routines during the introduction of health IT systems. European Journal of Information Systems. 2012;21:552–69. doi: 10.1057/ejis.2012.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aarts J, Berg M. Same systems, different outcomes--comparing the implementation of computerized physician order entry in two Dutch hospitals. Methods of information in medicine. 2006;45(1):53–61. [PubMed] [Google Scholar]
- 33.Aarts J, Peel V, Wright G. Organizational issues in health informatics: a model approach. Int J Med Inform. 1998 Oct-Dec;52(1-3):235–42. doi: 10.1016/s1386-5056(98)00142-7. [DOI] [PubMed] [Google Scholar]
- 34.Campion TR, Jr, Waitman LR, Lorenzi NM, May AK, Gadd CS. Barriers and facilitators to the use of computer-based intensive insulin therapy. Int J Med Inform. 2011;80(12):863–71. doi: 10.1016/j.ijmedinf.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ash JS, Sittig DF, Seshadri V, Dykstra RH, Carpenter JD, Stavri PZ. Adding insight: a qualitative cross-site study of physician order entry. Int J Med Inform. 2005 Aug;74(7-8):623–8. doi: 10.1016/j.ijmedinf.2005.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Unertl KM, Johnson KB, Lorenzi NM. Health information exchange technology on the front lines of healthcare: workflow factors and patterns of use. Journal of the American Medical Informatics Association. 2011 Oct 14; doi: 10.1136/amiajnl-2011-000432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carayon P, Karsh BT, Cartmill R. Incorporating health information technology into workflow redesign - Summary report. Rockville, MD: Prepared by the Center for Quality and Productivity Improvement, University of Wisconsin-Madison, under Contract No. HHSA 290-2008-10036C, 2010 Contract No.: AHRQ Publication No. 10-0098-EF; [Google Scholar]
- 38.Niazkhani Z, Pirnejad H, van der Sijs H, Aarts J. Evaluating the medication process in the context of CPOE use: the significance of working around the system. Int J Med Inform. 2011 Jul;80(7):490–506. doi: 10.1016/j.ijmedinf.2011.03.009. Epub 2011/05/11. eng. [DOI] [PubMed] [Google Scholar]
- 39.Aarts J, Doorewaard H, Berg M. Understanding implementation: the case of a computerized physician order entry system in a large Dutch university medical center. J Am Med Inform Assoc. 2004 May-Jun;11(3):207–16. doi: 10.1197/jamia.M1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berg M, Langenberg C, vd Berg I, Kwakkernaat J. Considerations for sociotechnical design: experiences with an electronic patient record in a clinical context. Int J Med Inform. 1998 Oct-Dec;52(1-3):243–51. doi: 10.1016/s1386-5056(98)00143-9. [DOI] [PubMed] [Google Scholar]
- 41.Karsh BT, Weinger MB, Abbott PA, Wears RL. Health information technology: fallacies and sober realities. J Am Med Inform Assoc. 2010 Nov-Dec;17(6):617–23. doi: 10.1136/jamia.2010.005637. Epub 2010/10/22. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ash JS, Stavri PZ, Dykstra R, Fournier L. Implementing computerized physician order entry: the importance of special people. Int J Med Inform. 2003 Mar;69(2-3):235–50. doi: 10.1016/s1386-5056(02)00107-7. [DOI] [PubMed] [Google Scholar]
- 43.Suchman L. Human-Machine Configurations: Plans and Situated Actions. Second Edition. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- 44.Goffman E. Frame Analysis: An Essay on the Organization of Experience. Cambridge, MA: Harvard University Press; 1974. [Google Scholar]
- 45.Hazlehurst B, McMullen C. Orienting frames and private routines: The role of cultural process in critical care safety. Int J Med Inform. 2007 Jun;76(Suppl 1):129–35. doi: 10.1016/j.ijmedinf.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 46.Gioia DA, Poole PP. Scripts in organizational behavior. The Academy of Management Review. 1984;9(3):449–59. [Google Scholar]
- 47.Giddens A. The Constitution of Society. Berkeley: University of California Press; 1984. [Google Scholar]
- 48.Karsten H, Laine A. User interpretations of future information system use: a snapshot with technological frames. Int J Med Inform. 2006;76S:S136–40. doi: 10.1016/j.ijmedinf.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 49.Orlikowski WJ, Gash DC. Technological Frames - Making Sense of Information Technology in Organizations. Acm T Inform Syst. 1994 Apr;12(2):174–207. English. [Google Scholar]
- 50.Davidson EJ. Technology frames and framing: a socio-cognitive investigation of requirements determination. MIS Q. 2002;26(4):329–58. [Google Scholar]
- 51.Gasser L. The integration of computing and routine work. ACM Trans Inf Syst. 1986;4(3):205–25. [Google Scholar]
- 52.Yang Z, Ng B-Y, Kankanhalli A, Yip J. Workarounds in the use of IS in healthcare: A case study of an electronic medication administration system. Int J Hum-Comput St. 2012;70:43–65. [Google Scholar]
- 53.Halbesleben JRB, Savage GT, Wakefield DS, Wakefield BJ. Rework and workarounds in nurse medication administration process: Implications for work processes and patient safety. Health Care Management Review. 2010;35(2):124–33. doi: 10.1097/HMR.0b013e3181d116c2. [DOI] [PubMed] [Google Scholar]
- 54.Patterson ES, Rogers ML, Chapman RJ, Render ML. Compliance With Intended Use of Bar Code Medication Administration in Acute and Long-Term Care: An Observational Study. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2006 Spring;48(1):15–22. doi: 10.1518/001872006776412234. [DOI] [PubMed] [Google Scholar]
- 55.Novak LL, Anders S, Gadd CS, Lorenzi NM. Mediation of adoption and use: a key strategy for mitigating unintended consequences of health IT implementation. Journal of the American Medical Informatics Association. 2012 doi: 10.1136/amiajnl-2011-000575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Karsh BT, Wetterneck T, Holden RJ, Rivera AJ, Faye H, Scanlon M, et al. Bar coding in medication administration. In: Yih Y, editor. Handbook of Healthcare Delivery Systems. Boca Raton, FL: CRC Press; 2011. [Google Scholar]
- 57.Holden RJ, Alper SJ, Scanlon MC, Murkowski K, Rivera AJ, Karsh BT. Challenges and problem-solving strategies during medication management: A study of a pediatric hospital before and after barcoding. 2nd International Conference on Healthcare Systems Ergonomics and Patient Safety; Strasbourg France. 2008. [Google Scholar]
- 58.Reddy M, Dourish P, Pratt W. Temporality in Medical Work: Time also Matters. Computer Supported Cooperative Work. 2006;15:29–53. [Google Scholar]
- 59.Berg M. Considerations for sociotechnical design: experiences with an electronic patient record in a clinical context. Int J Med Inform. 1998;52:243–51. doi: 10.1016/s1386-5056(98)00143-9. [DOI] [PubMed] [Google Scholar]
- 60.Banning M. Nurse prescribing, nurse education and related research in the United Kingdom: a review of the literature. Nurse Education Today. 2004;24(6):420–7. doi: 10.1016/j.nedt.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 61.Ritter A, Hansen-Turton T. The primary care paradigm shift: an overview of the state-level legal framework governing nurse practitioner practice. The Health Lawyer. 2008;20(4):21–8. [Google Scholar]
- 62.Berg M. Implementing information systems in health care organizations: myths and challenges. Int J Med Inform. 2001 Dec;64(2-3):143–56. doi: 10.1016/s1386-5056(01)00200-3. [DOI] [PubMed] [Google Scholar]
- 63.Goorman E, Berg M. Modelling nursing activities: electronic patient records and their discontents. Nurs Inq. 2000 Mar;7(1):3–9. doi: 10.1046/j.1440-1800.2000.00053.x. Epub 2000/10/07. eng. [DOI] [PubMed] [Google Scholar]


