Abstract
Background Temporomandibular joint (TMJ) total replacement with alloplastic prostheses has been performed since 1960s. Research in these last two decades has achieved important improvement in the development of biomaterials, design, adaptation, and fixation of the prosthesis components.
Objective To evaluate total TMJ replacement with alloplastic prostheses.
Methods We studied 27 patients, between 19 and 73 years old, who had total TMJ uni- or bilateral replacement surgery with custom-made alloplastic prostheses manufactured by TMJ Concepts, Inc. (Ventura, CA) between 1996 and 2011. The general data and preoperative measurements were taken from medical records. Subjective data related to pain, diet consistency, and current quality of life were collected with a questionnaire answered by the patients; measures of maximum interincisal opening and lateral mandibular movements were obtained from direct examination.
Results We found significant difference (p < 0.05) comparing pre- to postoperative results about improvement in mouth opening, pain relief, and satisfaction with the surgery and diet consistency.
Conclusion The results of this study show that total alloplastic TMJ prostheses are an efficient, safe, and stable long-term solution for patients who need TMJ total replacement.
Keywords: temporomandibular joint (TMJ), TMJ replacement, alloplastic prosthesis
The 1990s changed the history of temporomandibular joint (TMJ) total replacement with alloplastic prostheses, thanks to the appearance of personalized prostheses and the evolution of their components, and the use of these implants stopped being a debatable topic with regard to the disadvantages that for decades had taken their forerunners out of the market. Current research is focused on the analysis of the longevity and the functional results of these prostheses, as well as the degree of customer satisfaction, with the goal of improving the long-term effects in this type of treatment, thus contributing to the understanding of pain etiology and management. A thorough evaluation of TMJ and associated structures is needed for optimum results; in addition, an objective diagnosis is needed to avoid overtreatment. Planning and carrying out ideal and individualized procedures for each patient are also essential.
The method of TMJ replacement remains controversial, and several techniques, autogenous as well as alloplastic, have been described. There are, however, some specific TMJ conditions and pathologies that require total replacements with alloplastic prostheses, some of which can be described as absolute: ankylosed or reankylosed joints, self-graft failure, severe polyarticular inflammatory disease, concomitant reconstruction of the temporal bone and the zygomatic arch root, and any other situation in which anatomical structures have been destroyed. There is also another group of relative indications, and among those we can mention condylar fracture sequels, avascular necrosis, benign or malignant neoplasias that require extensive bone resection, congenital disorders such as hemifacial microsomia, and concomitant correction of dentofacial anomalies.2,3,4,5,6,7,8,9
The personalized or custom-made prostheses used for the current study were produced by TMJ Concepts, Inc. (Ventura, CA). These reconstruction devices are designed by computer-aided systems, and the prostheses are manufactured following a stereolithographic model in all patients, which is produced through the patient's three-dimensional computed tomography. The fossa component has a part that is made of pure titanium, which is fixed onto the base of the cranium, and an articulating surface, which is made of ultra-high-molecular-weight polyethylene and is bonded to the titanium base. The mandibular component (ramus-condyle) is made of wrought titanium alloy (6A1/4V) and the condylar head is made of an alloy containing chrome (28%), cobalt (64%), and molybdenum (6%).10,11 These prostheses have been used for more than 20 years and have shown satisfactory long-term stability, without any evidence of foreign body reactions or other complications such as fracture or material failure (Fig. 1).10
Figure 1.
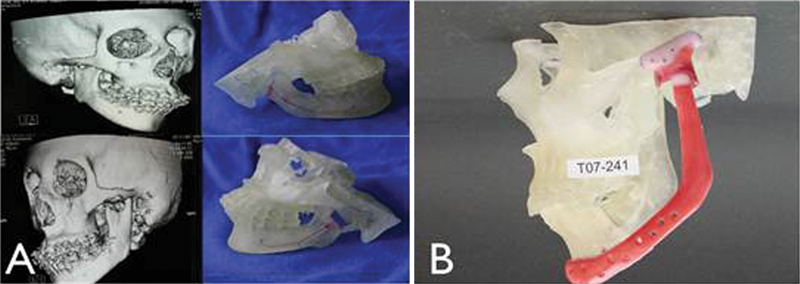
(A) Preoperative computed tomography and stereolithographic model. (B) Stereolithographic model and temporomandibular joint prosthesis template.
There are no 20-year longer-term reports as yet, however, that objectively evaluate interincisal opening and lateral movements, despite the diversity of surgeons managing significant sample cases, and this is also due to the fact that in Colombia there seem to be no reports of the results of total TMJ replacements with custom-made alloplastic prostheses.
The TMJ is a very complex structure that must withstand diverse forces to function properly, such as mastication, deglutition, phonation. To comply with these functions, the TMJ must carry out different mandibular movements, among which the following can be mentioned: opening, closing, lateral movement (right and left), protrusion, and retrusion (Fig. 2).12,13
Figure 2.
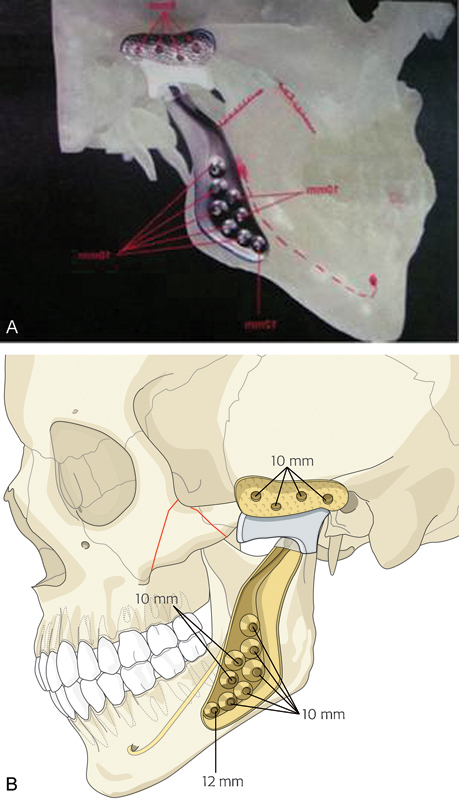
(A) Stereolithographic model with final custom temporomandibular joint prosthesis by TMJ Concepts, Inc. (Ventura, CA). (B) Final custom-made implant construction.
This study analyzes patients who have undergone total TMJ replacement surgeries with custom-made alloplastic prostheses, through an observational study of the results, by way of TMJ functionality description, and specifically interincisal opening and lateral movements, pain evolution, changes in diet consistency, and complications, all of which will enable discussion and research continuity, as well as allow characterization and comparison of results, to determine if these data correspond with results reported through the worldwide medical literature.
Materials and Methods
This is a descriptive observational study of 27 patients who underwent total TMJ replacement surgery with custom-made alloplastic prostheses between 1996 and 2011. Patients agreed to participate after signing written consents that were approved by the Ethics Committee of the Pontificia Universidad Javeriana. Patients additionally filled out a survey to assess subjective variables.
General preoperative data, such as age, race, gender, diagnosis, interincisal opening, and preoperative lateral movements, were taken from the patients' clinical records. Pain was evaluated by means of the visual analog scale (VAS). All the patients were given a survey with five questions to evaluate degree of satisfaction toward the surgery, facial changes, and changes in the diet. The mandibular function evaluated at the time the study was performed by measuring direct interincisal opening and lateral movement. The statistical information was analyzed by means of nonparametric tests for coupled samples (Wilcoxon test). Gender, race, age, and the different diagnoses that lead to total TMJ replacement as well as the incidence of complications (expressed in percentile values) were evaluated. Preoperative pain values, interincisal opening, and lateral movement ranges were compared with those of the current postoperative values to establish the results. All the data were processed using SPSS 18 software (IBM Corporation, New York, NY).
Results
There were 41 TMJ replacements with alloplastic prostheses in 27 patients (2 men and 25 women) between 1996 and 2011; of those 41 replacements, 14 were bilateral (28 TMJ) and 13 were unilateral (7 left and 6 right). The patients' ages were between 19 and 73 years, with an average of 42 years (standard deviation [SD] 11.331); the women were between 19 and 58 years, with an average of 41 years (SD 9.857), and the 2 men were 38 and 73 years, with an average of 55 years (SD 24.749). The predominant race in the cross section was Latino 59.3% (16), followed by Caucasian 40.7% (11).
Seven general diagnoses were identified, reporting the frequency and the age correlation. The TMJ mutilation diagnosis included patients with gunshot wounds and multiple previous surgeries that had failed (Table 1; Fig. 3).
Table 1. Frequency of diagnosis and patient ages with TMJ replacements using custom-made alloplastic prostheses.
| Diagnosis | Frequency | Age (y) | ||
|---|---|---|---|---|
| % | n | Median | SD | |
| Ankylosis | 18.5 | 5 | 45 | 8.044 |
| Polyarthritis | 18.5 | 5 | 45 | 8.044 |
| TMJ mutilation | 22.2 | 6 | 51 | 13.491 |
| Condylar fracture sequel | 14.8 | 4 | 38 | 4.123 |
| Idiopathic condylar resorption | 11.1 | 3 | 28 | 11.314 |
| Neoplasias | 7.4 | 2 | 23 | 6.364 |
| Condylar agenesia | 7.4 | 2 | 45 | 10.817 |
Abbreviations: SD, standard deviation; TMJ, temporomandibular joint.
Figure 3.
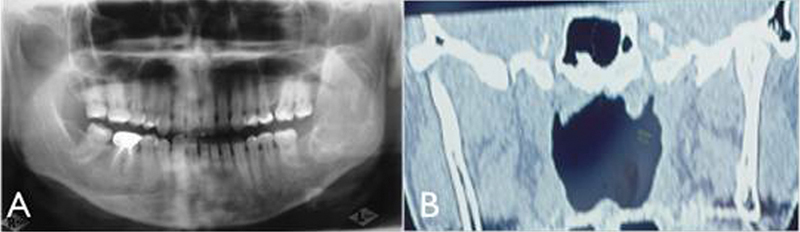
(A) Panoramic radiograph showing neoplasia in left mandibular body and ramus. (B) Axial computed tomography showing idiopathic condylar resorption of the right condyle.
The most frequent articular replacement surgery was bilateral, at 52.19% (14), followed by unilateral, at 48.1% (13), of which the most frequent were left-sided, at 53.8% (7), followed by right-sided, at 46.2% (6; Fig. 4).
Figure 4.
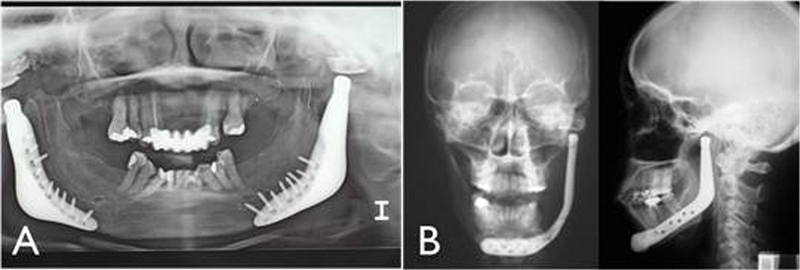
(A) Postoperative panoramic radiograph showing bilateral custom temporomandibular joint (TMJ) prosthesis by TMJ Concepts, Inc. (Ventura, CA). (B) Postoperative posteroanterior radiograph showing unilateral custom TMJ prosthesis by TMJ Concepts, Inc.
Preoperative measures of pain level, using the 0 to 10 VAS score, showed an average of 7 (SD 3.690). Postoperatively, patients expressed a level of pain between 0 and 10, with an average of 1.74 (SD 2.427; p = 0.005 by Wilcoxon test).
The general preoperative results for unilateral replacements, measuring a level of pain between 0 and10 using the VAS, showed an average of 5.92 (SD 4.071); postoperatively, the patients expressed an average level of pain of 1.38 (SD 0,1805; p = 0.008 by Wilcoxon test). Preoperative results with bilateral replacements using the VAS indicated an average of 8 (SD 3.113); postoperatively, the patients expressed a an average level of pain of 2.07 (SD 2.921; p = 0.003 by Wilcoxon test).
The general preoperative interincisal openings were between 0 and 49 mm, with an average of 22.41 (SD 14.885), and postoperatively were between 17 and 50 mm, with an average of 35.19 (SD 7.711).
The preoperative general interincisal openings for unilateral replacements were an average of 26.77 (SD 12.201), and postoperative average was 36.46 (SD 6.983; p = 0.012 by Wilcoxon test). The general preoperative openings for bilateral replacements were an average of 18.36 (SD 16.402), and postoperative average was 34.00 (SD 8.412; p = 0.015 by Wilcoxon tests).
Preoperative opposite lateral movement in unilateral replacements was an average of 3.85 mm (SD 1.951), and postoperative average was 2.77 mm (SD 2.488; p = 0.156 by Wilcoxon test). Preoperative left lateral movement for bilateral replacements was an average of 1.93 mm (SD 2.129), and the postoperative average was 0.71 mm (SD 0.914; p = 0.056 by Wilcoxon test). The preoperative right lateral movement for bilateral replacements was an average of 2.14 mm (SD 2.143), and the postoperative average was 0.93 mm (SD 01.141; p = 0.032 by Wilcoxon test; Fig. 5; Table 2).
Figure 5.

(A) Postoperative mouth opening after making total replacement of temporomandibular joint (TMJ) with custom prosthesis by TMJ Concepts, Inc. (Ventura, CA). (B) Intraoperative mandibular function after placement a custom TMJ prosthesis by TMJ Concepts, Inc.
Table 2. Pre- and postoperative functional comparison according to type of prosthesis.
| Unilateral (n = 13) | Bilateral(n = 14) | |||||
|---|---|---|---|---|---|---|
| Pre | Post | p | Pre | Post | p | |
| VAS | 5.92 (SD 4.071) | 1.38 (SD 1.805) | 0.008 | 8.00 (SD 3.113) | 2.07 (SD 2.921) | 0.003 |
| Interincisal opening | 26.77 (SD 12.201) | 0.012 | 18.36 (SD 16.402) | 34.00 (SD 8.412) | 0.005 | |
| Opposite lateral movement | 3.85 (SD 1.951) | 0.156 | ||||
| Right lateral movement | 2.14 (SD 2.143) | 0.93 (SD 1.141) | 0.032 | |||
| Left lateral movement | 1.93 (SD 2.129) | 0.71 (SD 0.914) | 0.056 | |||
Abbreviations: Pre, preoperative; Post, postoperative; SD, standard deviation; VAS, visual analog scale.
Similar statistical tests were conducted to compare functional measurements, according to the prostheses that were used, and they showed evidence of significant statistical differences in the average pre- and postoperative pain score for each type of prostheses (p = 0.005; unilateral, p = 0.008, and bilateral, p = 0.003). In the case of interincisal opening, the results were similar to those of unilateral opening (p = 0.012, and bilateral, p = 0.005). With regard to lateral movement, a decrease was identified in each of the prosthetic groups, with an important decrease after the surgeries, and there was statistically significant evidence only for the different averages between pre- and postoperative right lateral movement in the case of bilateral prostheses (p = 0.05 and a p = 0.032, respectively).
After receiving the implants, all patients were followed weekly for the first 2 months, then monthly for the next 4 months. Patients returned 6 months later, and then yearly thereafter. The data for all patients were collected in their last visit.
There were some complications in 25.9% (7) of the population studied, and the most frequent was transitory paresia of the temporal ramus of cranial nerve VII in 57.1% (4), followed by myofascial pain syndrome in 14.3% (1), permanent paresia of the temporal ramus of cranial nerve VII in 14.3% (1), and tumor relapse in 14.3% (1).
Postoperatively, patients were surveyed about their normal everyday activities related to their articulating prostheses (for example, capacity to chew their favorite foods, talking, yawning, among others). Patients indicated the following answers: significant improvement, 44.4% (12); improvement, 33.3% (9); no change, 18.5% (5); and significantly limited, 3.7% (1). When asked about the results of their TMJ replacement surgery, their answers were: excellent, 40.7% (11); good, 55.6% (15); fair 3.7% (3); and there were no answers mentioning bad results. With regard to a question about interincisal opening after their TMJ replacement surgery, they answered: significant improvement, 37.0% (10); improved, 44.4% (12); without any changes 11.1% (3); worsened, 3.7% (1); significantly worsened, 3.7% (1). Regarding their dietary habits, with respect to the consistency of the food consumed on a regular basis, after their TMJ replacement surgery they had the following answers: significant improvement, 29.6% (8); improved, 51.9% (14); and without any changes, 18.5% (5). With respect to the shape of their faces, after the TMJ replacement surgery, they answered: significant improvement, 7.4% (2); improved, 51.9% (14); without any changes, 37.0% (10); and worsened, 3.7% (1).
Discussion
This study proves that total TMJ replacement using personalized alloplastic prostheses is a treatment that offers functional and aesthetic advantages. The results that were reached indicate that most of the patients reported improved interincisal opening, significantly lessened pain, and improvements in dietary consistency, which not only satisfied the patients' aesthetic demands but also enabled greater adaptability of the prosthetic elements to the bone, which is an important factor that greatly helps achieve better long-term stability.
Currently, materials used to make prosthetic components have evolved and are biocompatible (ultra-high-molecular-weight polyethylene, titanium, chrome-cobalt-molybdenum), which has eradicated the disadvantages exhibited by prostheses made of other materials that were used decades before; these disadvantages included foreign body reactions, giant cell granuloma formations, and prosthesis loss due to these complications. In addition, the new materials are able to withstand masticatory efforts to which TMJ and associated structures are subject. The force exerted by the molars during mastication is estimated to be ∼265 N (60 pounds) and that of the incisors, 160 N (35 pounds).10,11 Due to the fact that the external and temporal pterygoid muscles are disinserted, the force that is exerted by these over the TMJ is lost, and as a consequence, the forces these prostheses are subject to decrease by 50%,10,11,13 which is why long-term prosthetic stability is observed without affecting healthy TMJ.
Regarding functions, one of the relevant disadvantages presented by TMJ replacement with alloplastic prostheses is the decrease or loss of contralateral lateral movement in patients with unilateral replacements, or loss of mandibular lateral movement in patients with bilateral replacements, due to the disinsertion of the external pterygoid muscle and the impossibility of reinserting it back inside the prosthetic component, thus enabling condylar rotation and limiting its translation.10,15,16,17,18 This is demonstrated with the results obtained, which indicate limited contralateral condylar excursion with respect to the prosthesis, and ipsilateral excursion is kept in those cases with total unilateral TMJ replacement, but in the case of bilateral replacements, lateral bilateral excursion is observed limited.
Another disadvantage is the cost of the prosthesis, but if cost-benefit is considered (and compared with other surgical alternatives), then it is worth using, due to its design, mainly because the anatomical structures to be replaced are morphologically recreated, which enables a greater adaptability and eliminates the need for a another surgical team to handle autografts, eliminates morbidity at the donors site, and reduces the time of hospitalization and patient disability.
In 2007, Mercuri performed a 14-year follow-up study of patients with total TMJ reconstruction with custom-made alloplastic prostheses made by TMJ Concepts, evaluating a total of 102 TMJs with an average 11.4-year follow-up; a significant 95% decrease in pain was reported over the follow-up, with mandibular function improving by 95% and interincisal opening significantly increasing by 95%, with an average annual increase of 0.4 mm.10 However, the mandibular function was not evaluated in an objective manner, using the VAS, and the only objective mandibular function measurement was that of the interincisal opening. Diet consistency and quality of life improved also, and these were subjectively evaluated by means of the VAS.
In the year 2003, Wolford performed a comparative study, evaluating two prosthetic systems: TMJ Concepts (22 patients) and TMJ Christensen (TMJ Implants, Inc., Golden, CO) (23 patients).5 Interincisal opening was measured, mandibular function was evaluated, and diet and pain were scored with a VAS. The average postoperative interincisal opening for Christensen's prostheses was 30.1 mm, and in the case of TMJ Concepts, it was 37.3 mm. The average pain in the case of Christensen's TMJ prostheses was 6.0, decreasing by 1.8, and for TMJ Concepts prostheses it was 4.1, with a decrease of 3.1. The measurement was performed by means of a survey where 0 = normal function and 10 = without function; with the diet, 0 = no restrictions and 10 = only liquids. Mandibular function and the diet improved in both cases, with an average of 5.0 and 3.9, respectively.
The current study reveals a postoperative improvement with regard to pain, interincisal opening, and a decrease or loss of lateral movements. One comparative advantage regarding previous studies is that, despite having a smaller population, the subjective results are similar to those contained in the literature, and in addition, objective analyses were performed, such as mandibular function, which was evaluated with interincisal opening and lateral movements, aided by a measuring tool, in millimeters.
Considering that mandibular function is limited not only to a simple hinge movement but also to the possibility of recreating all the movements in the three spatial planes, patients with alloplastic replacements lose part of their eccentric movements. This turns replaced joints into less complex systems than the natural joints, losing part of their function. Until there is an adequate method for muscular reinsertion in the prostheses, reconstruction with alloplastic prostheses will always bring about these sequels in patients, with their respective long-term complications, such as loss of reflexes protection, turning this group of patients into candidates who require the use of occlusal plates for dental protection, due to the imminent possibility of having dental fractures caused by direct trauma.
Pain continues to be a somewhat controversial topic; however, most patients experienced a significant decrease in postoperative pain: average preoperative pain was 5.92 and postoperative, 1.38. Despite this, we have to take into account that one of the existing complications in those patients is the occurrence of myofascial pain syndrome in the masticatory muscles; adequate preoperative patient analysis prevents mistaken diagnosis as a postoperative sequel and as the source of pain. Therefore, the source of the preoperative pain must be accurately identified before carrying out the replacement surgery, so as not to attribute the pain to a pathology that is not associated to the joint and to be able to objectively evaluate the control of the pain by using a prosthetic treatment.
After conducting an analysis about the results and despite having a high degree of success as evidenced by the literature, 2,3,4,5,8,9,10,11,12,13,14,15,16,17,18,19,20,21 we cannot set aside the small percentage of patients who expressed dissatisfaction with the treatment. We also have to consider that these results in the study might be attributed to advanced stages of uncontrolled severe inflammatory disease (polyarthritis), failed previous multiple surgeries where there is a decrease in the prognosis for pain amelioration, a high degree of stress on the part of the patient, lack of compliance by the patient with the therapies or postoperative controls or due to a lack of postoperative follow-up, and reinforcement on the part of the therapist in self-care techniques for this type of pathologies.
Nowadays, even restricted use of these prostheses in growing patients continues to be controversial. However, there is evidence of joint replacements with alloplastic prostheses in orthopedics in young patients, but there is not much literature regarding TMJ, which is why more studies should be performed about the indications and long-term stability in this type of patients.1,10,14
The replacements presented 25.9% of complications, and the most frequent of these was nerve injuries (paralysis of the temporal branch of the facial nerve), which is an inherent complication of the surgical approach but not of the prosthesis itself. Another complication exhibited after the surgery was tumor relapse, which is not connected with the prosthesis but is associated with the diagnosis that led to the replacement. Due to the size of the study, it cannot be concluded that the complications that were evidenced had a high percentage or that those setbacks were the only ones exhibited for this type of treatment. Mercuri and Anspach, in 2003, reported that there could be some neurologic complications, such as reflex sympathetic dystrophy, that cause extreme pain and are characterized by little improvement in the immediate postoperative period and slow recovery and rehabilitation, as well as cutaneous hypersensitivity.20 Neuromas are also mentioned in Mercuri and Anspach's study, as well as Frey syndrome and fatigue or muscular spasms that delay the progress of the recovery.20 World literature concerning total TMJ replacement with alloplastic prostheses does not report specific complications, so we cannot possibly compare them with the complications presented in this study. It cannot be assumed either that other authors have not reported complications, due to the fact there is no reference of this in the studies that have been published.
Other authors have reported some advantages of total TMJ replacements with personalized alloplastic prostheses, such as decreased morbidity at the donor site, surgical time, and hospitalization time; immediate function, avoiding the need of extending intermaxillary fixation, thus enabling immediate physical therapy and improving interincisal opening in a more rapid manner; capacity to maintain stable postoperative occlusion due to the minimal dimensional change of the prosthesis compared with its opposite (autologous graft with resorption capacity); the possibility of manipulating the prosthetic design, which more precisely recreates TMJ anatomy.1,2,3,4,5,10,11,14,15 This also makes concomitant reconstruction of temporal bone and attached structures possible, as well as the possibility of dentofacial deformity (DFD) correction and simultaneous replacement. Nonetheless, custom-made prostheses offer better adaptability and long-term stability, thus increasing their useful life, but there are no exact indicators about the life span of an alloplastic replacement. Despite this, prostheses that were evaluated over this current study remain stable and functional, without any reports of failure.
Conclusions
Total TMJ replacements with custom-made prostheses represent an efficient and safe treatment option for patients who require TMJ reconstruction. The current study reveals that 100% of the prostheses have remained stable through time. There is also evidence of improvement in interincisal opening, decreased pain and lateral movements, changes in the diet consistency of the studied population, due to the fact that the consistency of the group improved by exhibiting minimum complications that had no influence over the patients' level of satisfaction toward their TMJ replacement surgeries, which ranked 95%.
Despite the fact that the percentage of success of alloplastic prostheses has already been established, long-term studies must continue to help develop materials that will improve characteristics of the current prostheses, so as to minimize the disadvantages, such as limited mandibular excursive movements, along with their use in growing patients.
References
- 1.Saeed N R, Kent J N. A retrospective study of the costochondral graft in TMJ reconstruction. Int J Oral Maxillofac Surg. 2003;32:606–609. doi: 10.1054/ijom.2003.0418. [DOI] [PubMed] [Google Scholar]
- 2.Mercuri L G Total joint reconstruction—autologous or alloplastic Oral Maxillofac Surg Clin North Am 200618399–410., vii [DOI] [PubMed] [Google Scholar]
- 3.Fonseca R Oral and Maxillofacial Surgery Temporomandibular Disorders. Vol. 4. Asheville, NC: W. B. Saunders; 2000 [Google Scholar]
- 4.Voiner J, Yu J, Deitrich P, Chafin C, Giannakopoulos H. Analysis of mandibular motion following unilateral and bilateral alloplastic TMJ reconstruction. Int J Oral Maxillofac Surg. 2011;40:569–571. doi: 10.1016/j.ijom.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Wolford L M Dingwerth D J Talwar R M Pitta M C Comparison of 2 temporomandibular joint total joint prosthesis systems J Oral Maxillofac Surg 200361685–690., discussion 690 [DOI] [PubMed] [Google Scholar]
- 6.Westermark A, Koppel D, Leiggener C. Condylar replacement alone is not sufficient for prosthetic reconstruction of the temporomandibular joint. Int J Oral Maxillofac Surg. 2006;35:488–492. doi: 10.1016/j.ijom.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 7.Moore L J Evaluation of the patient for temporomandibular joint surgery Oral Maxillofac Surg Clin North Am 200618291–303., v [DOI] [PubMed] [Google Scholar]
- 8.Mercuri L. The use of alloplastic prostheses for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58:70-75. doi: 10.1016/s0278-2391(00)80020-8. [DOI] [PubMed] [Google Scholar]
- 9.Dela Coleta K E, Wolford L M, Gonçalves J R, Pinto A S, Pinto L P, Cassano D S. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part I—skeletal and dental stability. Int J Oral Maxillofac Surg. 2009;38:126–138. doi: 10.1016/j.ijom.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 10.Mercuri L G, Edibam N R, Giobbie-Hurder A. Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg. 2007;65:1140–1148. doi: 10.1016/j.joms.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Mercuri L. The TMJ Concepts patient-fitted total temporomandibular joint reconstruction prosthesis. Oral and Maxillof Surg Clinics. 2000;12:73–91. [Google Scholar]
- 12.Okeson J Management of Temporomandibular Disorders and Occlusion 6th ed. Lexington, KY: Elsevier Mosby; 2008 [Google Scholar]
- 13.Throckmorton G. Temporomandibular joint biomechanics. Oral and Maxillof Surg Clinics. 2000;12:27–42. [Google Scholar]
- 14.Mercuri L G, Swift J Q. Considerations for the use of alloplastic temporomandibular joint replacement in the growing patient. J Oral Maxillofac Surg. 2009;67:1979–1990. doi: 10.1016/j.joms.2009.05.430. [DOI] [PubMed] [Google Scholar]
- 15.Yoon H J, Baltali E, Zhao K D. et al. Kinematic study of the temporomandibular joint in normal subjects and patients following unilateral temporomandibular joint arthrotomy with metal fossa-eminence partial joint replacement. J Oral Maxillofac Surg. 2007;65:1569–1576. doi: 10.1016/j.joms.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Collins C P, Wilson K J, Collins P C. Lateral pterygoid myotomy with reattachment to the condylar neck: an adjunct to restore function after total joint reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:672–673. doi: 10.1067/moe.2003.153. [DOI] [PubMed] [Google Scholar]
- 17.Pinto L P, Wolford L M, Buschang P H, Bernardi F H, Gonçalves J R, Cassano D S. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part III—pain and dysfunction outcomes. Int J Oral Maxillofac Surg. 2009;38:326–331. doi: 10.1016/j.ijom.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 18.Guarda-Nardini L, Manfredini D, Ferronato G. Temporomandibular joint total replacement prosthesis: current knowledge and considerations for the future. Int J Oral Maxillofac Surg. 2008;37:103–110. doi: 10.1016/j.ijom.2007.09.175. [DOI] [PubMed] [Google Scholar]
- 19.Quinn P, Tomado de Fonseca R. Asheville, NC: Saunders; 2000. Oral and Maxillofacial Surgery. Temporomandibular Disorders; pp. 316–332. [Google Scholar]
- 20.Mercuri L G, Anspach W E III. Principles for the revision of total alloplastic TMJ prostheses. Int J Oral Maxillofac Surg. 2003;32:353–359. doi: 10.1054/ijom.2002.0447. [DOI] [PubMed] [Google Scholar]
- 21.Wolford L M, Pitta M C, Reiche-Fischel O, Franco P F. TMJ Concepts/Techmedica custom-made TMJ total joint prosthesis: 5-year follow-up study. Int J Oral Maxillofac Surg. 2003;32:268–274. doi: 10.1054/ijom.2002.0350. [DOI] [PubMed] [Google Scholar]